Abstract
OBJECTIVE:
To determine if race/ethnicity-based differences exist in the management of pediatric abdominal pain in emergency departments (EDs).
METHODS:
Secondary analysis of data from the 2006–2009 National Hospital Ambulatory Medical Care Survey regarding 2298 visits by patients ≤21 years old who presented to EDs with abdominal pain. Main outcomes were documentation of pain score and receipt of any analgesics, analgesics for severe pain (defined as ≥7 on a 10-point scale), and narcotic analgesics. Secondary outcomes included diagnostic tests obtained, length of stay (LOS), 72-hour return visits, and admission.
RESULTS:
Of patient visits, 70.1% were female, 52.6% were from non-Hispanic white, 23.5% were from non-Hispanic black, 20.6% were from Hispanic, and 3.3% were from “other” racial/ethnic groups; patients’ mean age was 14.5 years. Multivariate logistic regression models adjusting for confounders revealed that non-Hispanic black patients were less likely to receive any analgesic (odds ratio [OR]: 0.61; 95% confidence interval [CI]: 0.43–0.87) or a narcotic analgesic (OR: 0.38; 95% CI: 0.18–0.81) than non-Hispanic white patients (referent group). This finding was also true for non-Hispanic black and “other” race/ethnicity patients with severe pain (ORs [95% CI]: 0.43 [0.22–0.87] and 0.02 [0.00–0.19], respectively). Non-Hispanic black and Hispanic patients were more likely to have a prolonged LOS than non-Hispanic white patients (ORs [95% CI]: 1.68 [1.13–2.51] and 1.64 [1.09–2.47], respectively). No significant race/ethnicity-based disparities were identified in documentation of pain score, use of diagnostic procedures, 72-hour return visits, or hospital admissions.
CONCLUSIONS:
Race/ethnicity-based disparities exist in ED analgesic use and LOS for pediatric abdominal pain. Recognizing these disparities may help investigators eliminate inequalities in care.
Keywords: abdominal pain, disparities, emergency department, racial difference
What’s Known on This Subject:
Racial/ethnic differences in care for adult and pediatric patients in the emergency department have been documented.
What This Study Adds:
This study reveals racial/ethnic differences in analgesic administration and prolonged length of stay for pediatric emergency department visits for abdominal pain. Documenting such disparities is an important first step needed to improve the equity of care for this and other conditions.
Emergency departments (EDs) are a health care safety net for underserved patients, regardless of their insurance status, ability to pay, and race/ethnicity. However, there are race/ethnicity-based differences in pediatric ED care. For example, white children are more likely than other children to undergo diagnostic procedures (eg, blood tests, electrocardiograms, and chest radiographs) for chest pain.1 White children with intermediate or low-risk injury-severity head trauma are also more likely to undergo head computed tomography (CT) than similarly injured black and Hispanic children.2 Black female teenagers with abdominal pain or genitourinary symptoms are more likely than whites to be tested for sexually transmitted diseases, even when reporting no sexual activity (Holland C, et al., unpublished data presented at Pediatric Academic Societies Meeting, Section of Emergency Medicine, April 2011).3 Black and Hispanic infants with traumatic brain injury are more likely than white infants to have a skeletal survey to evaluate for child abuse.4 Similarly, black children with fractures are more likely than whites to be reported for suspected child abuse.5,6 Black and Hispanic children also have longer ED wait times compared with white children.6,7 Findings of race/ethnicity-based differences in ED care are concerning because minority children are less likely to have a usual source of care8 and more likely to visit EDs for common complaints.9
No study to date has examined race/ethnicity-based differences in the management of pediatric abdominal pain, a common complaint. For children presenting to EDs with abdominal pain, we hypothesized that compared with non-Hispanic white patients, minority patients would be less likely to have a pain score documented, receive analgesics for their pain (both narcotic and nonnarcotic), undergo diagnostic testing, or be admitted to the hospital and more likely to have a prolonged ED length of stay (LOS) or return visit for the same complaint. To test our hypotheses, we performed a secondary analysis of data reported in the National Hospital Ambulatory Medical Care Survey (NHAMCS) from 2006 to 2009 for ED visits by patients ≤21 years old with abdominal pain.
Methods
Data Source
With the University of Pittsburgh’s Institutional Review Board approval, we used data from NHAMCS, an annual nationwide survey designed to collect ED service data. Details of recruitment, sampling methods, and study procedures are available from the Centers for Disease Control and Prevention.10 Briefly, the NHAMCS uses a national probability sampling design that produces unbiased estimates when weighting procedures are applied. Hospital staff, trained by census representatives, review charts for a systematic random sample of patient visits during a 4-week reporting period. Standardized patient record forms are used to abstract and record data.
Study Population
During the 2006–2009 study period, the NHAMCS surveyed 140 415 visits, representing a national sample of 495 827 143 visits. We examined data from 2298 ED visits by pediatric patients (defined by the American Academy of Pediatrics as ≤21 years old11) whose primary reason for visit was documented as either “stomach pain,” “abdominal pain,” “abdominal cramps,” or “abdominal spasms.”
Independent Variables
Our main independent variable was race/ethnicity. Unless it was the individual hospital’s policy to obtain self-reported race/ethnicity, hospital staff reported patient race/ethnicity on the basis of observation. The NHAMCS used 5 race categories: (1) white, (2) black, (3) Asian, (4) Native Hawaiian or other Pacific Islander, and (5) American Indian or Alaskan Native. A dichotomous variable was used to report ethnicity if the patient was Hispanic. Because of the small number of patients in the third, fourth, and fifth categories, we collapsed race/ethnicity into 4 categories for our analyses: non-Hispanic white, non-Hispanic black, Hispanic, and other. For patient visits with missing race/ethnicity, the NHAMCS used hot deck imputation, randomly assigning a value from another patient record with similar characteristics.
Dependent Variables
Our main dependent variables were related to pain management. Analgesics for severe pain (defined as ≥7 on a 10-point scale) was chosen as the primary pain management variable because we believed this variable met an “appropriateness” threshold on the basis of proposed performance measures for pediatric emergency care.12 Analgesic use included nonnarcotics (eg, acetaminophen, ibuprofen, and ketorolac) and narcotics (eg, morphine and oxycodone), which were identified by using the National Drug Code Directory. Additional pain management outcomes included documentation of pain score, receipt of any analgesics overall, and receipt of narcotic analgesics specifically.
Secondary outcome variables, chosen from proposed performance measures for pediatric emergency care,12 were the use of diagnostic tests (blood test, urinalysis, pregnancy test, or radiographic imaging), ED LOS (categorized as prolonged if >6 hours), 72-hour return visit rate for the same condition, and hospital admission rate.
Covariates
We examined patient biological (age and gender), clinical (pain and triage level at presentation), system-level (type of hospital ownership and geographic region), and socioeconomic (income and insurance status) factors as potential confounders.
Age (categorized as <2, 2–5, 6–11, 12–14, 15–18, and 19–21 years) and gender are biological factors that affect the differential diagnosis of abdominal pain and can influence management. Young age (<2 years) and female gender are also linked with ED oligoanalgesia, and therefore were adjusted for in our models.13,14
Patients’ pain and triage level at presentation are clinical factors that can influence diagnostic test ordering and administration of analgesics.15,16 Pain was measured on a 10-point scale and grouped into 4 categories: none (0), mild (1–3), moderate (4–6), and severe (7–10). Triage level is the level of urgency of the visit, determined by focused assessment of the patient’s acuity on the basis of vital sign stability, likelihood of an immediate life-threatening condition, and expected resources needed during the visit (eg, laboratory testing, intravenous therapy, consultations, or other procedures). Triage level was used as a proxy for illness severity, defined as follows: level 1, immediate care; level 2, emergent care (<15 minutes); level 3, urgent care (15–59 minutes); level 4, semiurgent care (1–2 hours); and level 5, nonurgent care (>2 hours).17 For our analyses, we collapsed triage level into 3 groups: immediate or emergent, urgent, and semiurgent or nonurgent.
System-level factors, such as variation in available resources and management practices between different hospitals, are known contributors to differences in care.18–20 For example, adult minorities are more likely to receive care in poorer performing institutions than whites, and these between-facility variations in quality contribute to disparities.19,20 Also, children seen in EDs in the South and West are more likely to receive opioid analgesics than in the Northeast.21 We adjusted for type of hospital (categorized as voluntary/nonprofit, government/nonfederal, or proprietary) and geographic region (Northeast, Midwest, South, or West) in our analyses.
Socioeconomic factors are also associated with differences in care.18,22–24 Patient zip codes and census data were used to determine the percentage of the area population living below the federal poverty line as a proxy for income.22,23 Insurance status, determined by expected source of payment documented, was categorized into 5 groups: private insurance, Medicaid or the Children’s Health Insurance Program, self-pay, other (eg, no charge/charity, worker’s compensation), and unknown.
Statistical Analyses
We used descriptive statistics to summarize patient and hospital characteristics, stratified by race/ethnicity. We used prescribed weighting procedures to generate national estimates.
To determine the association between race/ethnicity and outcome variables, we used logistic regression for dichotomous variables and linear regression for continuous variables. If variables showed a strong association (P < .10) with race/ethnicity in our bivariate models, we included them in our multivariate models. To assess the association of race/ethnicity with each outcome variable, we used hierarchical multivariate logistic regression models that adjusted for age, gender, pain level, triage level, type of hospital ownership, geographic region, income, and insurance status. We used non-Hispanic white patients as the referent group.
For all analyses, we used Stata version 11 (StataCorp, College Station, TX) and considered a P value <0.05 to be significant. We reported results as odds ratios (ORs) and 95% confidence intervals (CIs).
Results
Our sample consisted of 2298 pediatric ED visits for abdominal pain, representing 8 137 774 visits nationally during the 4-year study period. Patients’ mean age was 14.5 years (Table 1). Of the patients, 70.1% were female, 52.6% were non-Hispanic white, 23.5% were non-Hispanic black, 20.6% were Hispanic, and 3.3% were from other racial/ethnic groups. Whereas 17.9% had an unknown or undocumented pain score, there was no significant difference between these patients and those with a documented score.
TABLE 1.
Characteristics of Pediatric Patients Who Presented With Abdominal Pain to EDs, Stratified by Race/Ethnicity
| Characteristic | Total (N = 8 137 774) | Non-Hispanic White Children (n = 4 283 045) | Non-Hispanic Black Children (n = 1 908 755) | Hispanic Children (n = 1 676 632) | Other Children (n = 269 342) |
|---|---|---|---|---|---|
| Race/ethnicity, % | 100 | 52.6 (48.9–56.3) | 23.5 (19.7–27.7) | 20.6 (16.7–25.1) | 3.3 (2.4–4.6) |
| Mean age, y | 14.5 (14.2–14.9) | 14.8 (14.3–15.2) | 15.7 (15.1–16.3) | 13.0 (12.3–13.7) | 12.1 (10.5–13.6) |
| Age category, % | |||||
| <2 years | 1.4 (0.8–1.9) | 1.5 (0.8–2.7) | 0.8 (0.3–2.2) | 1.3 (0.6–2.9) | 4.5 (1.5–12.4) |
| 2–5 years | 8.6 (6.9–10.4) | 6.6 (5.0–8.6) | 7.7 (5.4–10.8) | 13.4 (9.4–18.7) | 19.3 (11.3–31.1) |
| 6–11 years | 20.0 (17.2–22.8) | 19.3 (16.2–22.8) | 13.3 (9.5–18.3) | 29.0 (22.5–36.4) | 23.6 (15.3–34.7) |
| 12–14 years | 8.5 (7.2–9.9) | 10.6 (8.7–12.8) | 6.1 (3.8–9.7) | 6.6 (4.1–10.6) | 5.8 (2.4–13.5) |
| 15–18 years | 27.8 (25.2–30.1) | 29.4 (25.8–33.3) | 28.2 (23.5–33.3) | 23.2 (18.8–28.2) | 24.1 (14.9–36.6) |
| 19–21 years | 33.8 (30.9–36.6) | 32.8 (29.2–36.6) | 44.0 (38.7–49.3) | 26.6 (21.4–32.5) | 22.7 (12.8–37.0) |
| Female gender, % | 70.1 (67.8–72.3) | 69.2 (66.3–72.1) | 76.8 (72.5–81.0) | 66.4 (61.6–71.2) | 58.6 (46.3–70.9) |
| Presenting level of pain, % | |||||
| None | 5.3 (4.0–6.6) | 4.4 (2.9–6.7) | 7.5 (4.9–11.4) | 5.6 (3.2–9.6) | 2.5 (0.9–6.7) |
| Mild | 10.8 (9.2–12.4) | 10.4 (8.6–12.5) | 10.2 (7.3–14.2) | 11.9 (8.2–16.8) | 15.3 (8.4–26.3) |
| Moderate | 32.5 (29.9–35.2) | 32.7 (29.2–36.5) | 28.2 (23.1–33.9) | 35.3 (29.3–41.8) | 43.6 (33.1–54.7) |
| Severe | 33.4 (30.1–36.7) | 36.5 (32.0–41.0) | 34.1 (29.2–39.3) | 27.3 (20.7–35.1) | 18.1 (10.4–29.5) |
| Unknown | 17.9 (15.0–20.9) | 16.1 (12.9–19.9) | 19.9 (15.7–25.0) | 20.0 (14.9–26.3) | 20.5 (10.9–35.3) |
| Triage level, % | |||||
| Immediate or emergent | 7.9 (6.1–9.7) | 7.6 (5.7–10.1) | 8.3 (5.6–12.3) | 8.4 (5.3–13.0) | 6.3 (2.8–13.5) |
| Urgent | 54.0 (50.2–57.7) | 55.8 (50.6–60.8) | 53.3 (46.6–59.9) | 50.0 (43.5–56.5) | 55.4 (39.5–70.2) |
| Semiurgent, nonurgent, or no triage performed | 38.1 (34.3–42.0) | 36.6 (31.6–41.9) | 38.4 (32.5–44.5) | 41.7 (34.9–48.7) | 38.3 (24.5–54.2) |
| Hospital ownership, % | |||||
| Voluntary/nonprofit | 74.9 (69.8–79.9) | 78.2 (72.3–84.1) | 78.5 (71.1–85.9) | 62.3 (54.3–70.3) | 74.7 (62.0–87.4) |
| Government/nonfederal | 13.1 (9.8–16.4) | 10.9 (7.4–14.5) | 13.4 (7.6–19.3) | 17.2 (9.9–24.4) | 18.6 (7.3–29.8) |
| Proprietary | 12.1 (8.1–16.0) | 10.8 (6.0–15.6) | 8.1 (3.9–12.3) | 20.5 (12.7–28.3) | 6.7 (0.0–13.3) |
| Region, % | |||||
| Northeast | 17.3 (14.3–20.4) | 19.0 (14.9–23.2) | 13.0 (8.3–17.8) | 17.4 (11.3–23.5) | 20.7 (8.8–32.6) |
| Midwest | 22.5 (17.0–28.0) | 25.3 (19.1–31.6) | 23.8 (15.0–32.6) | 14.1 (6.5–21.8) | 20.4 (6.2–34.6) |
| South | 41.0 (34.8–47.2) | 38.8 (31.9–45.7) | 56.0 (45.7–66.3) | 33.6 (20.8–46.5) | 14.5 (5.0–24.0) |
| West | 19.2 (12.7–25.7) | 16.8 (9.6–24.1) | 7.2 (3.5–10.9) | 34.8 (23.4–46.2) | 44.4 (25.9–62.9) |
| Area population living below the federal poverty line, % | |||||
| <5% of population | 13.3 (10.7–15.8) | 19.1 (15.7–23.1) | 5.6 (3.5–8.8) | 8.2 (5.3–12.3) | 6.6 (2.7–15.2) |
| 5%–9.99% of population | 25.9 (22.9–29.0) | 31.0 (27.0–35.2) | 14.4 (10.3–19.9) | 25.1 (20.2–30.8) | 32.6 (22.8–44.3) |
| 10%–19.99% of population | 32.9 (29.4–36.3) | 33.6 (29.4–38.0) | 31.7 (26.6–37.2) | 34.2 (26.9–42.3) | 22.0 (13.0–34.7) |
| ≥20% of population | 21.7 (18.5–24.9) | 9.8 (7.4–13.0) | 42.6 (35.4–50.1) | 27.5 (20.8–35.4) | 27.5 (15.7–43.4) |
| Unknown | 6.2 (4.1–8.2) | 6.5 (4.3–9.8) | 5.8 (3.4–9.8) | 5.0 (2.9–8.6) | 11.3 (5.2–22.8) |
| Insurance status, % | |||||
| Private insurance | 38.8 (35.7–42.0) | 51.0 (46.7–55.3) | 22.6 (18.0–27.2) | 25.7 (19.1–32.2) | 42.8 (30.8–54.7) |
| Medicaid or CHIP | 32.5 (29.5–35.4) | 23.4 (20.0–26.9) | 44.5 (38.9–50.1) | 41.7 (34.9–48.5) | 32.5 (21.4–43.7) |
| Self-pay | 17.4 (14.7–20.0) | 15.6 (11.6–19.5) | 21.6 (16.6–26.6) | 18.1 (13.2–23.0) | 11.5 (3.9–19.0) |
| Other | 4.5 (3.2–5.8) | 3.6 (2.3–5.0) | 5.0 (2.3–7.6) | 6.8 (3.0–10.6) | 1.9 (0.0–4.1) |
| Unknown | 6.8 (4.0–9.7) | 6.3 (2.9–9.8) | 6.3 (3.4–9.2) | 7.8 (2.7–12.8) | 11.4 (0.0–23.5) |
Data are national estimates based on information reported in the 2006–2009 NHAMCS and represent means or percentages (95% CI), as indicated. Unless it was the individual hospital’s policy to obtain self-reported race/ethnicity, the hospital staff reported a patient’s race/ethnicity on the basis of observation. Because of rounding, percentages may not total 100%. CHIP, Children’s Health Insurance Program.
Overall, non-Hispanic white patients were more likely to receive analgesics (23.7%) than non-Hispanic black (16%), Hispanic (19%), and other race (17.9%) children. Similarly, among children with severe pain (≥7 of 10 points), non-Hispanic white children were more likely to receive analgesics (27.1%) than non-Hispanic black (15.8%), Hispanic (18.9%), and other race (7.1%) children. Narcotic analgesics were also administered more frequently to non-Hispanic white patients (12.3%) than non-Hispanic black (5%), Hispanic (8.1%), or other race (4.3%) children.
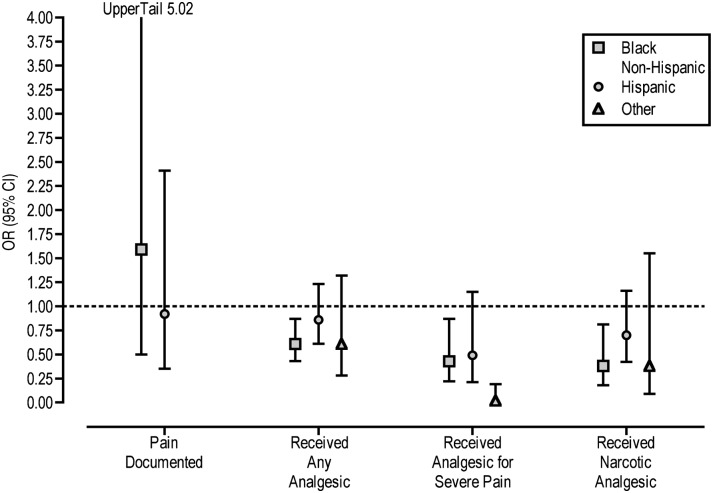
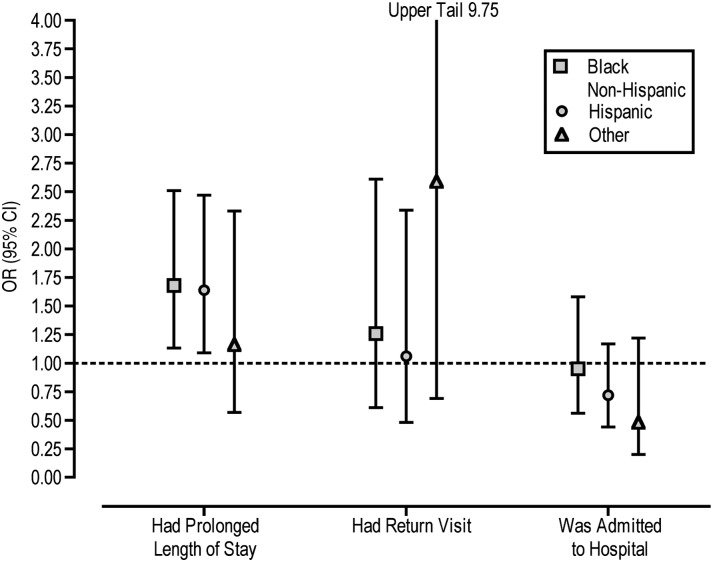
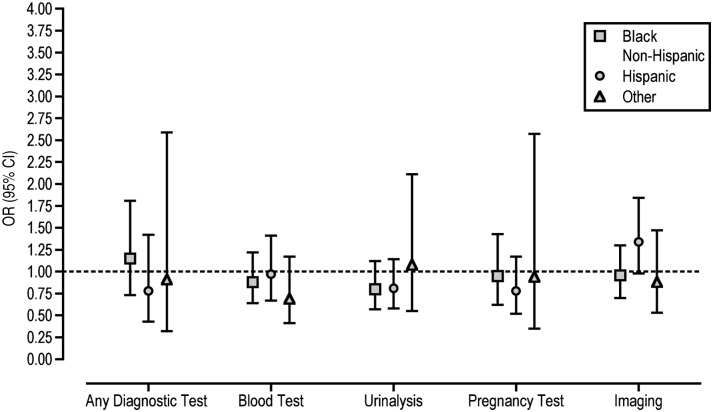
Findings from multivariate logistic regression models that adjusted for age, gender, pain level, triage level, hospital ownership, geographic region, income, and insurance status, and used non-Hispanic white patients as the referent group, are shown in Figs 1–3.
FIGURE 1.
Management of pain in children who presented with abdominal pain to EDs. Findings are from multivariate logistic regression models that adjusted for confounders (age, gender, pain level, triage level, type of hospital ownership, geographic region, income, and insurance status) and used non-Hispanic white patients as the referent group. Severe pain was defined as a score of ≥7 on a 10-point scale. Values that do not cross 1 (dotted line) were considered statistically significant.
FIGURE 3.
Hospital-related processes for children who presented with abdominal pain to EDs. Findings are from multivariate logistic regression models that adjusted for confounders (age, gender, pain level, triage level, type of hospital ownership, geographic region, income, and insurance status) and used non-Hispanic white patients as the referent group. Prolonged LOS was defined as >6 hours, and return visit defined as return within 72 hours. Values that do not cross 1 (dotted line) were considered statistically significant.
Results for pain management variables (Fig 1) showed that non-Hispanic black patients were less likely than non-Hispanic white patients to receive any analgesic (OR: 0.61; 95% CI: 0.43–0.87) or a narcotic analgesic (OR: 0.38; 95% CI: 0.18–0.81). Among patients with severe pain (≥7 of 10 points), non-Hispanic black patients and patients from other racial/ethnic categories were less likely to receive analgesia than non-Hispanic white patients (ORs [95% CI]: 0.43 [0.22–0.87] and 0.02 [0.00–0.19], respectively). Among patients in the 2 most severe triage categories, non-Hispanic black patients and patients from other racial/ethnic categories were less likely to receive analgesia than non-Hispanic white patients (ORs [95% CI]: 0.60 [0.38–0.92] and 0.41 [0.18–0.90], respectively).
Results for any diagnostic test, blood tests, urinalyses, pregnancy tests, and imaging (Fig 2) revealed no significant differences associated with race/ethnicity.
FIGURE 2.
Diagnostic tests ordered for children who presented with abdominal pain to EDs. Findings are from multivariate logistic regression models that adjusted for confounders (age, gender, pain level, triage level, type of hospital ownership, geographic region, income, and insurance status) and used non-Hispanic white patients as the referent group. Values that do not cross 1 (dotted line) were considered statistically significant.
Results for other process of care measures (Fig 3) revealed that non-Hispanic black and Hispanic patients were more likely to have a prolonged ED LOS (>6 hours) than non-Hispanic white patients (ORs [95% CI]: 1.68 [1.13–2.51] and 1.64 [1.09–2.47], respectively). There were no significant differences in 72-hour return visit or admission rates.
Discussion
In our analyses of nationally representative data for children ≤21 years who presented to EDs with abdominal pain, we found that non-Hispanic black patients were less likely than non-Hispanic white patients to receive any analgesics or narcotic analgesics for pain, even when pain was reported as severe. We also found that non-Hispanic black and Hispanic patients were more likely than non-Hispanic white patients to have a prolonged LOS. We identified no significant race/ethnicity-based differences in diagnostic testing, return visits, or admission rates.
Our findings are consistent with studies in adult ED patients. For example, in a 4-year retrospective review of 20 125 adults with abdominal or back pain in 2 urban EDs, Mills et al24 found that white patients were more likely than nonwhite patients to receive any analgesics and opiates. In a study in 139 ED patients in Los Angeles over a 2-year period with isolated bone fractures, Todd et al25 found that non-Hispanic white patients were more likely than Hispanic patients to receive analgesics. Similarly, Todd et al26 also found that among 217 Atlanta, Georgia, ED patients with long-bone fractures, white patients were more likely than black patients to receive analgesics. In an analysis of 1997–1999 NHAMCS data that examined analgesic administration to adults, Tamayo-Sarver et al27 found that physicians were more likely to prescribe opioids to white patients than black patients with migraines and back pain. Finally, an analysis of NHAMCS data for pain-related visits to US EDs from 1993 to 2005 found that white patients were more likely to be prescribed opioids than black, Hispanic, or other race patients. These findings held for all types of pain visits (including nephrolithiasis and long-bone fractures) and were detected among adults and children.28
Our results differ from a study that used 1992–1998 NHAMCS data and found no race/ethnicity-based differences in analgesic administration to children under 19 years old with long-bone fractures.21 One possible explanation for the differences in results is that abdominal pain has more heterogeneous causes and fewer clinical and diagnostic findings than do long-bone fractures. Another possible explanation is health care providers’ concern about masking a surgical abdominal condition despite several studies showing that analgesics do not interfere with diagnosis.29–32 Furthermore, this concern would not explain findings of race/ethnicity-based disparities in analgesic administration.
Compared with non-Hispanic white patients, non-Hispanic black and Hispanic patients were more likely to have a prolonged ED LOS. Our findings are consistent with NHAMCS data from 1997–2000 suggesting that ED wait times vary according to race/ethnicity.6 In our study, prolonged LOS does not seem to be related to diagnostic evaluation because no racial/ethnic differences in testing were identified. For Hispanic patients, LOS may be related to language barriers and use of interpreter services, although we could not examine the effect of language in our study. For non-Hispanic black patients, LOS may be partially explained by longer median wait times to see a physician for those triaged as semiurgent or nonurgent or with no documented triage score.
Racial/ethnic differences in diagnostic testing were found in our unadjusted analysis, but not after controlling for confounders. Differences in adjusted and unadjusted analyses suggest that factors other than patient race/ethnicity may explain differences in testing. In some scenarios, receiving less testing may result in delayed or misdiagnosis, reflecting poor-quality care. In other cases, receiving more testing may be harmful, such as exposing a child to radiation by performing a potentially unnecessary CT scan. To improve the quality and equity of care for all children, it is important for physicians to be mindful of and address differences in both directions.
Several study limitations deserve mention. First, the sample size was limited for certain variables. There were few cases in which patients from minority groups had severe pain and were given any analgesic or a narcotic analgesic, few cases in which Hispanic patients were given any analgesic, few cases in which patients from minority groups had 72-hour return visits, and few cases in which patients from the “other” category of race/ethnicity had a prolonged LOS or were admitted to the hospital. These small cell sizes result in unstable national estimates, limiting the accuracy of our results. However, when we grouped the patients into white and nonwhite categories to create larger cell sizes, we observed patterns similar to the ones reported in our results.
Second, whereas some hospitals obtained self-reported data on race/ethnicity, often considered the gold standard,33–35 others relied on hospital staff to assign race/ethnicity. Because our study is concerned with management on the basis of health care providers’ perceptions of race/ethnicity, hospital staff designations may more accurately reflect these perceptions. However, lack of consistent self-report for patient race/ethnicity may have contributed to misclassification bias.
Third, the majority of diagnoses codes were generic, with “other symptoms involving abdomen and pelvis” the most commonly listed discharge diagnosis for all children in the sample. Given the lack of specificity, we were unable to determine how specific diagnoses contributed to our findings. However, when we adjusted for age, gender, presenting pain level, and triage level, and looked specifically at analgesia administration in the 2 most severe triage categories, our findings persisted. Our adjusted results suggests that race/ethnicity-based differences in analgesic administration and LOS were independent of severity of illnesses and the clinical factors controlled for. However, other factors, such as diagnosis and comorbid illnesses, can influence management, which we were unable to control for.
Finally, we adjusted for triage category in our model; however, there may have been race/ethnicity-related bias among triage staff. A 10-year analysis of 78 million adult ED visits using NHAMCS found that black and Hispanic patients with chest pain were less likely than whites to be triaged emergently.36 Therefore, it is possible that in our study, white patients who were less ill may have been assigned a more urgent score and minority patients who were more ill could have been assigned a less urgent score. If this situation occurred, we would expect our results to underestimate the association between race/ethnicity and abdominal pain management.
The Institute of Medicine defines health care disparities as “observed differences in quality of healthcare by race/ethnicity that are not due to access to care, clinical needs, patient preferences, or appropriateness of the intervention.”18 We adjusted for confounders in our analysis, including biological, clinical, system-level, and socioeconomic factors, and found that race/ethnicity-based differences persisted for analgesic use and LOS. Additional research is needed to better understand other patient-, parent-, provider-, and system-level factors that may contribute to these differences. Future studies should explore factors that influence when (early or delayed), where (ED or primary medical provider’s office), and how (ambulance or private vehicle) parents access care for abdominal pain and other common conditions. Parental preference influences race/ethnicity-based differences in performing CT scans in children with head trauma.2 The role of parents’ treatment preferences, medical mistrust, and health beliefs warrants further analyses involving mixed qualitative and quantitative research methods.
EDs are settings conducive to stress and fatigue among health care providers. The stressful ED setting may foster providers’ use of mental shortcuts or heuristics,37 including racial/ethnic profiling and stereotyping. Studies in adult populations suggest that providers are more likely to be influenced by stereotypes and bias when making decisions in the setting of time pressure and limited available information.38 The subjective nature of abdominal pain, combined with lack of an established patient-provider relationship in EDs, may enhance the use of heuristic methods for evaluating and managing children. Additional research is needed to explore the role of bias and other provider-level factors that may contribute to pediatric health care disparities. System-level factors should also be explored, including the availability of primary care providers, interpreter services, consulting subspecialists, and pediatric formulations of analgesics.
Conclusions
Equity is an important component of health care quality, and efforts to identify and address race/ethnicity-based inequities are critical. By documenting inequities in analgesia and LOS for abdominal pain in a nationally representative sample of ED visits, our study contributes to the growing body of evidence showing disparities in pediatric health care. These data can be used to develop and test interventions that seek to eliminate race/ethnicity-based differences in the management of abdominal pain and other common pediatric complaints in EDs. Until such interventions are developed, clinicians caring for children in EDs should be aware of inequities in analgesic administration and make efforts to address pain control that may be suboptimal among minority children.
Glossary
- CI
confidence interval
- CT
computed tomography
- ED
emergency department
- LOS
length of stay
- NHAMCS
National Hospital Ambulatory Medical Care Survey
- OR
odds ratio
Footnotes
Dr Johnson conceptualized and designed the study, participated in data analysis and interpretation, drafted the initial manuscript, and made revisions to the manuscript; Mr Weaver was responsible for acquisition, statistical analysis, and interpretation of the data and made critical revisions to the manuscript; Drs Borrero, Davis, Myaskovsky, and Zuckerbraun contributed to the design of the study and made critical revisions to the manuscript; Dr Kraemer contributed to the design of the study, obtained funding, and made critical revisions to the manuscript; and all authors approved the final manuscript as submitted.
The Agency for Healthcare Research and Quality had no role in the study design; collection, management, analysis, and interpretation of the data; or manuscript preparation. This article’s content is solely the responsibility of the authors and does not necessarily represent the views of the Agency for Healthcare Research and Quality.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Supported by grant T32HS017587 from the Agency for Healthcare Research and Quality to Drs Johnson and Kraemer.
POTENTIAL CONFLICT OF INTEREST: The authors have indicated they have no potential conflicts of interest to disclose.
References
- 1.Hambrook JT, Kimball TR, Khoury P, Cnota J. Disparities exist in the emergency department evaluation of pediatric chest pain. Congenit Heart Dis. 2010;5(3):285–291 [DOI] [PubMed] [Google Scholar]
- 2.Natale JE, Joseph JG, Rogers AJ, et al. PECARN (Pediatric Emergency Care Applied Research Network) . Cranial computed tomography use among children with minor blunt head trauma: association with race/ethnicity. Arch Pediatr Adolesc Med. 2012;166(8):732–737 [DOI] [PubMed] [Google Scholar]
- 3.Goyal MK, Hayes KL, Mollen CJ. Racial disparities in testing for sexually transmitted infections in the emergency department. Acad Emerg Med. 2012;19(5):604–607 [DOI] [PubMed] [Google Scholar]
- 4.Wood JN, Hall M, Schilling S, Keren R, Mitra N, Rubin DM. Disparities in the evaluation and diagnosis of abuse among infants with traumatic brain injury. Pediatrics. 2010;126(3):408–414 [DOI] [PubMed] [Google Scholar]
- 5.Lane WG, Rubin DM, Monteith R, Christian CW. Racial differences in the evaluation of pediatric fractures for physical abuse. JAMA. 2002;288(13):1603–1609 [DOI] [PubMed] [Google Scholar]
- 6.James CA, Bourgeois FT, Shannon MW. Association of race/ethnicity with emergency department wait times. Pediatrics. 2005;115(3). Available at: www.pediatrics.org/cgi/content/full/115/3/e310 [DOI] [PubMed] [Google Scholar]
- 7.Park CY, Lee MA, Epstein AJ. Variation in emergency department wait times for children by race/ethnicity and payment source. Health Serv Res. 2009;44(6):2022–2039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shi L, Stevens GD. Disparities in access to care and satisfaction among U.S. children: the roles of race/ethnicity and poverty status. Public Health Rep. 2005;120(4):431–441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Flores G, Committee on Pediatric Research . Technical report—racial and ethnic disparities in the health and health care of children. Pediatrics. 2010;125(4). Available at: www.pediatrics.org/cgi/content/full/125/4/e979 [DOI] [PubMed] [Google Scholar]
- 10.Centers for Disease Control and Prevention. Ambulatory health data: about NAMCS/NHAMCS. Available at: www.cdc.gov/nchs/ahcd.htm. Accessed Aug 14, 2012
- 11.American Academy of Pediatrics Council on Child and Adolescent Health . Age limits of pediatrics. Pediatrics. 1988;81(5):736. [PubMed] [Google Scholar]
- 12.Alessandrini E, Varadarajan K, Alpern ER, et al. Pediatric Emergency Care Applied Research Network . Emergency department quality: an analysis of existing pediatric measures. Acad Emerg Med. 2011;18(5):519–526 [DOI] [PubMed] [Google Scholar]
- 13.Alexander J, Manno M. Underuse of analgesia in very young pediatric patients with isolated painful injuries. Ann Emerg Med. 2003;41(5):617–622 [DOI] [PubMed] [Google Scholar]
- 14.Chen EH, Shofer FS, Dean AJ, et al. Gender disparity in analgesic treatment of emergency department patients with acute abdominal pain. Acad Emerg Med. 2008;15(5):414–418 [DOI] [PubMed] [Google Scholar]
- 15.Ducharme J, Tanabe P, Homel P, et al. Pain and Emergency Medicine Initiative Study Group . The influence of triage systems and triage scores on timeliness of ED analgesic administration. Am J Emerg Med. 2008;26(8):867–873 [DOI] [PubMed] [Google Scholar]
- 16.Silka PA, Roth MM, Moreno G, Merrill L, Geiderman JM. Pain scores improve analgesic administration patterns for trauma patients in the emergency department. Acad Emerg Med. 2004;11(3):264–270 [DOI] [PubMed] [Google Scholar]
- 17.Gilboy N, Tanabe P, Travers DA, Rosenau AM, Eitel DR. Emergency Severity Index, Version 4: Implementation Handbook. Rockville, MD: Agency for Healthcare Research and Quality; 2011. AHRQ Publication 12-0014 [Google Scholar]
- 18.Smedley B, Stith AY, Nelson A, eds. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002 [PubMed] [Google Scholar]
- 19.Hasnain-Wynia R, Kang R, Landrum MB, Vogeli C, Baker DW, Weissman JS. Racial and ethnic disparities within and between hospitals for inpatient quality of care: an examination of patient-level Hospital Quality Alliance measures. J Health Care Poor Underserved. 2010;21(2):629–648 [DOI] [PubMed] [Google Scholar]
- 20.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg. 2012;147(1):63–70 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yen K, Kim M, Stremski ES, Gorelick MH. Effect of ethnicity and race on the use of pain medications in children with long bone fractures in the emergency department. Ann Emerg Med. 2003;42(1):41–47 [DOI] [PubMed] [Google Scholar]
- 22.Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994;331(7):444–449 [DOI] [PubMed] [Google Scholar]
- 23.Hofer TP, Wolfe RA, Tedeschi PJ, McMahon LF, Griffith JR. Use of community versus individual socioeconomic data in predicting variation in hospital use. Health Serv Res. 1998;33(2 pt 1):243–259 [PMC free article] [PubMed] [Google Scholar]
- 24.Mills AM, Shofer FS, Boulis AK, Holena DN, Abbuhl SB. Racial disparity in analgesic treatment for ED patients with abdominal or back pain. Am J Emerg Med. 2011;29(7):752–756 [DOI] [PubMed] [Google Scholar]
- 25.Todd KH, Samaroo N, Hoffman JR. Ethnicity as a risk factor for inadequate emergency department analgesia. JAMA. 1993;269(12):1537–1539 [PubMed] [Google Scholar]
- 26.Todd KH, Deaton C, D’Adamo AP, Goe L. Ethnicity and analgesic practice. Ann Emerg Med. 2000;35(1):11–16 [DOI] [PubMed] [Google Scholar]
- 27.Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in emergency department analgesic prescription. Am J Public Health. 2003;93(12):2067–2073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA. 2008;299(1):70–78 [DOI] [PubMed] [Google Scholar]
- 29.Bailey B, Bergeron S, Gravel J, Bussières JF, Bensoussan A. Efficacy and impact of intravenous morphine before surgical consultation in children with right lower quadrant pain suggestive of appendicitis: a randomized controlled trial. Ann Emerg Med. 2007;50(4):371–378 [DOI] [PubMed] [Google Scholar]
- 30.Kim MK, Strait RT, Sato TT, Hennes HM. A randomized clinical trial of analgesia in children with acute abdominal pain. Acad Emerg Med. 2002;9(4):281–287 [DOI] [PubMed] [Google Scholar]
- 31.Kokki H, Lintula H, Vanamo K, Heiskanen M, Eskelinen M. Oxycodone vs placebo in children with undifferentiated abdominal pain: a randomized, double-blind clinical trial of the effect of analgesia on diagnostic accuracy. Arch Pediatr Adolesc Med. 2005;159(4):320–325 [DOI] [PubMed] [Google Scholar]
- 32.Green R, Bulloch B, Kabani A, Hancock BJ, Tenenbein M. Early analgesia for children with acute abdominal pain. Pediatrics. 2005;116(4):978–983 [DOI] [PubMed] [Google Scholar]
- 33.McAlpine DD, Beebe TJ, Davern M, Call KT. Agreement between self-reported and administrative race and ethnicity data among Medicaid enrollees in Minnesota. Health Serv Res. 2007;42(6 pt 2):2373–2388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Friedman DJ, Cohen BB, Averbach AR, Norton JM. Race/ethnicity and OMB directive 15: implications for state public health practice. Am J Public Health. 2000;90(11):1714–1719 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mays VM, Ponce NA, Washington DL, Cochran SD. Classification of race and ethnicity: implications for public health. Annu Rev Public Health. 2003;24:83–110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.López L, Wilper AP, Cervantes MC, Betancourt JR, Green AR. Racial and sex differences in emergency department triage assessment and test ordering for chest pain, 1997-2006. Acad Emerg Med. 2010;17(8):801–808 [DOI] [PubMed] [Google Scholar]
- 37.Croskerry P. Achieving quality in clinical decision making: cognitive strategies and detection of bias. Acad Emerg Med. 2002;9(11):1184–1204 [DOI] [PubMed] [Google Scholar]
- 38.van Ryn M. Research on the provider contribution to race/ethnicity disparities in medical care. Med Care. 2002;40(1 suppl):I140–I151 [DOI] [PubMed] [Google Scholar]