Abstract
OBJECTIVE:
Studies suggest that young adults have worse health care access, use less primary care, and visit emergency departments more frequently than adolescents. We examined whether these differences existed between older adolescents and young adults with asthma.
METHODS:
Using nationally representative data from the 1999 to 2009 Medical Expenditure Panel Survey, we performed cross-sectional comparisons of access and utilization between older adolescents (ages 14–17) and young adults (ages 19–25) with asthma. In longitudinal analyses, we assessed whether changes in health insurance coverage, schooling, and adult presence at home predicted changes in access and utilization.
RESULTS:
Young adults with asthma were less likely to have a usual source of care (–13.7 percentage points; P < .001) or primary care visit within the past year (–13.9 percentage points; P = .006). They were less likely to fill a short-acting beta-agonist prescription (–10.6 percentage points; P = .02) and more likely to visit the emergency department within the past year (+9.7 percentage points; P = .01). Adjusting for differences in insurance coverage reduced differences in usual source of care and primary care use by 32.4% to 38.0% but reduced the difference in emergency department use by only 10.3%. Among participants aged 16 to 19 in the first survey year, becoming uninsured strongly predicted losing a usual source of care (change relative to no coverage loss: –25.2 percentage points; P = .003).
CONCLUSIONS:
Compared with older adolescents with asthma, young adults with asthma have worse health care access and may use care less optimally. These differences were associated with but were not completely explained by differences in insurance coverage.
Keywords: adolescents, asthma, health care utilization, health insurance, young adult
What's Known on This Subject:
Studies suggest that young adults have worse access to health care, use less primary care, and visit emergency departments more frequently than adolescents. Whether these differences are present between adolescents and young adults with asthma is unknown.
What This Study Adds:
Young adults with asthma were less likely to have a usual source of care and use primary care. In contrast, they were more likely to use the emergency department. Adjusting for insurance coverage reduced these differences partially but not completely.
As adolescents transition to young adulthood, they often experience changes that could affect their health care utilization including discontinuation of schooling and transitions to independent living.1,2 Many young adults also lose health insurance coverage. Medicaid and the Children’s Health Insurance Program cover individuals aged 18 and younger in low-income families but generally do not cover individuals aged 19 and older unless they are pregnant, are disabled, or have children.3 Furthermore, before a recently implemented provision of the Affordable Care Act (ACA), private insurance policies in most states did not cover dependents older than age 18 unless they were full-time students.3 Consequently, individuals aged 19 to 25 had the highest uninsurance rate of any age group in 2010.4
Previous research suggests that the health care access and utilization patterns of young adults may be suboptimal.5,6 Compared with adolescents, young adults use less primary care and rely more heavily on emergency departments (EDs) for care.7 Whether these differences exist between adolescents and young adults with chronic diseases is unknown.
Using nationally representative survey data, we assessed differences in access and utilization between older adolescents and young adults with asthma. Asthma is highly prevalent in these age groups,8,9 and exacerbations may lead to emergent care when asthma is not appropriately managed or when ambulatory care cannot be accessed.10,11 We hypothesized that young adults with asthma are less likely than older adolescents with asthma to have a usual source of care, less likely to use primary and preventive care, less likely to fill prescriptions for asthma medications, and more likely to use the ED. We also explored potential mediators of these differences, focusing on insurance coverage, a factor targeted by recent legislation.
Methods
Data Source
We analyzed data from the 1999–2009 Medical Expenditure Panel Survey (MEPS), a nationally representative panel survey that examines access and utilization in the US civilian noninstitutionalized population. Households are interviewed 5 times during the 2-year survey period; 1 respondent answers for the entire household. A parent or adult relative usually provides proxy reports for adolescents and young adults living at home. In contrast, young adults living independently or away at college self-report information.12
Study Design
In cross-sectional analyses, we compared several measures of access and utilization between older adolescents and young adults with asthma. In longitudinal analyses, we tested whether changes in insurance coverage, schooling, or adult presence at home predicted changes in these measures among individuals with asthma transitioning from adolescence to young adulthood.
Cross-sectional Analysis
Study Population
We included participants for whom a current diagnosis of asthma, an asthma-related utilization event, or an asthma-related disability day was reported. Using age on July 1, we classified participants aged 14 to 17 as older adolescents and participants aged 19 to 25 as young adults. We excluded participants aged 18 because age 18 is a transitional year during which changes in insurance coverage, schooling, and living situations often occur. Our aim was to compare outcomes before and after the bulk of these transitions occurred.
Study Variables
Based on respondent reports of access and utilization over the previous 12 months, we constructed 8 dichotomous dependent variables for having (1) a usual source of care; (2) ≥1 primary care visit; (3) ≥1 preventive visit; (4) ≥1 fill of a short-acting beta-agonist (SABA) prescription; (5) ≥1 fill of a controller medication prescription; (6) ≥1 ED visit; (7) a cost or coverage-related problem accessing medical care; and (8) a cost or coverage-related problem accessing medications. For primary care visits, preventive visits, and cost or coverage-related access problems, we analyzed data from 2002 to 2009 because these items were not available before 2002.
We defined a usual source of care as a non-ED facility that participants usually visited when they were sick or needed health advice. We defined a primary care visit as an office visit to a physician whose specialty was family practice, general practice, internal medicine, osteopathy, or pediatrics. We defined a preventive visit as a primary care visit that respondents classified as a “general checkup.”13 Information on prescription fills was collected from respondent reports and pharmacies.14 Controller medications included inhaled corticosteroids, leukotriene modifiers, and combinations of inhaled corticosteroids/long-acting β agonists. We defined a cost or coverage-related access problem as a delay or inability to receive care because of unaffordability, denial of coverage by an insurance company, or refusal of insurance by a physician.12
Statistical Analysis
To provide readily interpretable estimates in terms of absolute percentage differences, we fitted linear models predicting each dichotomous dependent variable as a function of age group (young adults versus older adolescents), age in months (to adjust for trends preceding and continuing in young adulthood), race/ethnicity, gender, and survey year. To adjust for geographic variations in health care access and utilization, we included geographic identifiers at the level of metropolitan areas for densely populated areas and states or Census regions for less-populated areas (based on strata of the MEPS survey design).
In separate models, we added the percentage of months spent uninsured in each survey year as a covariate to determine the degree to which differences in coverage explained differences in access and utilization between age groups.
Sensitivity Analyses
We conducted 3 sensitivity analyses. First, because respondents were not asked if household members had a current diagnosis of asthma until 2003, we conducted an analysis that restricted our sample to participants classified as having asthma from reports of asthma-related utilization events or disability days. Second, we used logistic instead of linear regression models. Finally, to test whether differences between age groups were driven by inconsistencies between proxy and self-reports, we excluded participants who self-reported information the entire survey year.
Longitudinal Analysis
Study Sample
For longitudinal analyses examining participants transitioning from adolescence to young adulthood, we restricted the sample to participants with asthma who were aged 16 to 19 at the beginning of survey participation and who provided data in both survey years.
Study Variables
Because the small cohort size limited statistical power, we analyzed only 5 dichotomous dependent variables: reports of having a usual source of care and reports of having ≥1 primary care visit, preventive visit, fill of a SABA prescription, and fill of a controller medication prescription in the previous 12 months.
For our main predictors of interest, we created 3 variables describing changes in insurance coverage, schooling, and adult presence at home (defined as living with a parent or adult relative ≥35) between the first and second years of survey participation. To assess insurance loss, we subtracted the percentage of months insured in year 2 from the percentage of months insured in year 1 and truncated negative differences (because of the few who gained coverage) to 0. Thus, a unit increase in this variable indicated a change from continuous insurance coverage in year 1 to continuous uninsurance in year 2. To assess discontinued schooling, we constructed a similar variable from student status information reported during each interview. A unit increase in this variable indicated a change from continuous full-time schooling in year 1 to no schooling in year 2. To assess loss of adult presence at home, we created a similar variable from household structure information reported during each interview. A unit increase in this variable indicated a change from continuous adult presence at home in year 1 to continuous independent living in year 2. Student status is not determined for MEPS participants younger than 17, but we assumed that adolescents aged 16 were full-time students because ∼98% of the national population is enrolled in school at this age.15
Statistical Analysis
We fitted linear regression models predicting access and utilization as a function of survey participation year (first versus second), changes in insurance coverage, and the interaction between these terms (see Appendix for model specification). The interactions estimated the differential changes in outcomes associated with coverage losses, relative to participants who experienced no coverage loss. To control for changes in schooling and adult presence at home, as well as to assess whether these social factors predicted access and utilization we similarly included these changes and their interactions with survey participation year. Covariates included age at the beginning of year 1, race/ethnicity, gender, data year (MEPS panel), Census region, and, within each region, whether participants resided in a metropolitan area or not.
We performed analyses using SAS version 9.2 (SAS Institute, Inc, Cary, NC). We adjusted for the complex survey design of the MEPS by using sampling weights and using robust design-based variance estimators.16 We considered 2-sided P values <.05 to indicate statistical significance. The Committee on Human Studies at Harvard Medical School deemed this study exempt from review.
Results
Cross-sectional Analyses
After excluding 18-year-olds, 2485 participants met inclusion criteria for analyses of 1999–2009 data, providing 3469 person-years of data; 2173 participants met inclusion criteria for analyses of 2002–2009 data, providing 2958 person-years of data. For analyses of usual source of care and cost or coverage-related access problems, we excluded 0.5% to 1.5% of observations because of missing data.
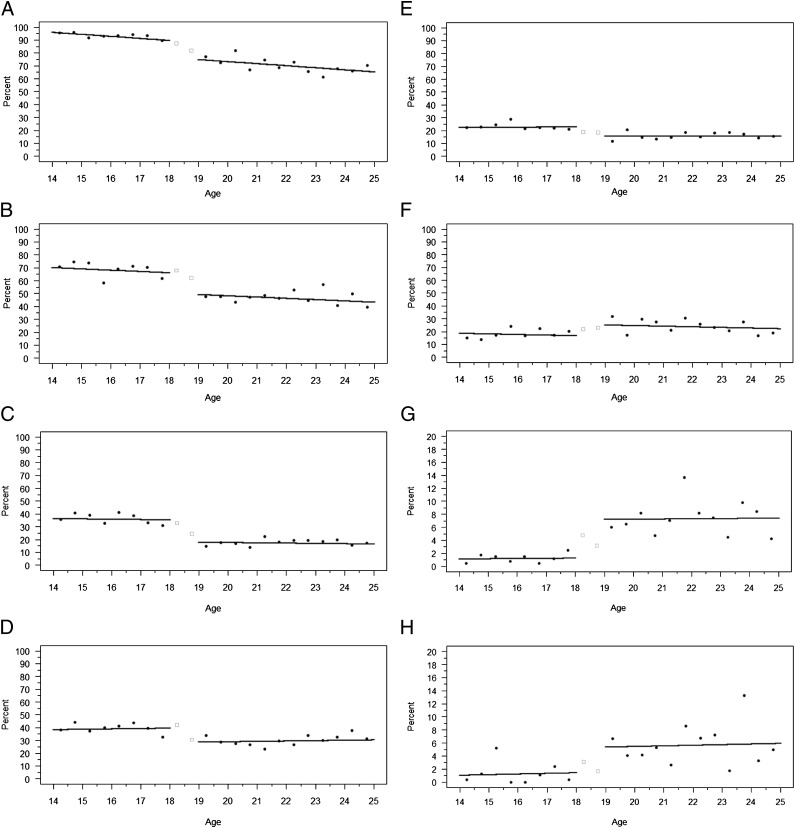
Older adolescents and young adults with asthma differed significantly by race/ethnicity, gender, and insurance coverage (Table 1). Figure 1 displays adjusted age-specific means and fitted regression lines for the 8 outcomes. Young adults with asthma were less likely to have a usual source of care than older adolescents with asthma (adjusted means: 65.5% vs 79.2%; difference: –13.7 percentage points; P < .001). In the previous 12 months, young adults were less likely to have ≥1 primary care visit (44.4% vs 58.3%; difference: –13.9 percentage points; P = .006) and ≥1 preventive visit (16.6% vs 33.7%; difference: –17.1 percentage points; P < .001). Young adults were also less likely to fill a SABA prescription at least once in the previous 12 months (34.7% vs 45.3%; difference: –10.6 percentage points; P = .02) but not significantly less likely to fill a controller medication prescription at least once in the previous 12 months.
TABLE 1.
Demographic Characteristics of Study Sample, MEPS 1999–2009
| Older Adolescents (n = 1871) | Young Adults (n = 1598) | P Value | |
|---|---|---|---|
| Race | <.001a | ||
| Asian/no other race/not Hispanic | 2.1% | 3.1% | |
| Black/no other race/not Hispanic | 25.1% | 22.3% | |
| Hispanic | 24.5% | 20.5% | |
| Other race/not Hispanic | 48.4% | 54.1% | |
| Gender | <.001b | ||
| Female | 47.0% | 61.6% | |
| Insurance coverage | <.001b | ||
| Percent of months uninsured | 10.6% | 33.5% |
P value is derived from a χ2 test.
P value is derived from a 2-sample t test assuming unequal variance.
FIGURE 1.
Health care access and utilization among older adolescents and young adults with asthma. Panels A to H display age-specific means and fitted regression lines for each of the 8 dependent variables in cross-sectional comparisons: A, Usual source of care; B, ≥1 primary care visit in the previous 12 months; C, ≥1 preventive visit in the previous 12 months; D, ≥1 fill of a short-acting beta-agonist prescription in the previous 12 months; E, ≥1 fill of a controller medication prescription in the previous 12 months; F, ≥1 ED visit in the previous 12 months; G, cost or coverage-related problem accessing medical care in the previous 12 months; H, cost or coverage-related problem accessing medications in the previous 12 months. The square data points represent excluded data for participants aged 18.
Young adults with asthma were more likely to have ≥1 ED visit in the previous 12 months (28.5% vs 18.5%; difference: +9.7 percentage points; P = .01). They were also more likely to experience cost or coverage-related problems accessing medical care (8.1% vs 3.3%; difference: +4.9 percentage points; P = .01) and medications (5.4% vs 1.9%; difference: +3.6 percentage points; P = .04). Adjusting for differences in insurance coverage reduced differences in access and utilization by up to 61.1%, although the difference for ED visits did not change substantially (Table 2).
TABLE 2.
Differences in Access and Utilization Between Older Adolescents and Young Adults With Asthma, Before and After Adjustment for Insurance Coverage
| Absolute Difference Between Age Groups, Not Adjusting for Insurance Coverage, Percentage Points | P Value | Absolute Difference Between Age Groups, Adjusting for Insurance Coverage, Percentage Points | P Value | Percent Change in Absolute Difference Between Age Groups After Adjusting for Insurance Coverage, % | |
|---|---|---|---|---|---|
| Usual source of care | −13.7 | <.001 | −8.5 | .02 | 38.0 |
| ≥1 primary care visit | −13.9 | .006 | −9.4 | .07 | 32.4 |
| ≥1 preventive visit | −17.1 | <.001 | −15.0 | .001 | 12.3 |
| ≥1 fill of a short-acting beta-agonist prescription | −10.6 | .02 | −9.0 | .05 | 15.1 |
| ≥1 fill of a controller medication prescription | −5.3 | .19 | −3.7 | .37 | 30.2 |
| ≥1 emergency department visit | 9.7 | .01 | 8.7 | .03 | 10.3 |
| Cost or coverage-related problem accessing medical care | 4.9 | .01 | 2.6 | .14 | 46.9 |
| Cost or coverage-related problem accessing medications | 3.6 | .04 | 1.4 | .42 | 61.1 |
In sensitivity analyses, results of cross-sectional comparisons were not substantively changed by restricting the sample to participants for whom an asthma-related utilization event or disability day was reported, by using logistic instead of linear regression, or by excluding participants who self-reported information the entire survey year (see Appendix and Appendix Fig 1 for additional analyses regarding potential response bias).
Longitudinal Analyses
For longitudinal analyses of 1999–2009 data, 740 participants met inclusion criteria, yielding 1480 person-years of data. We excluded at most 3.8% of observations due to missing data. For analyses of 2002–2009 data, 608 participants met inclusion criteria, yielding 1216 person-years of data. We excluded 2.3% of observations due to missing data.
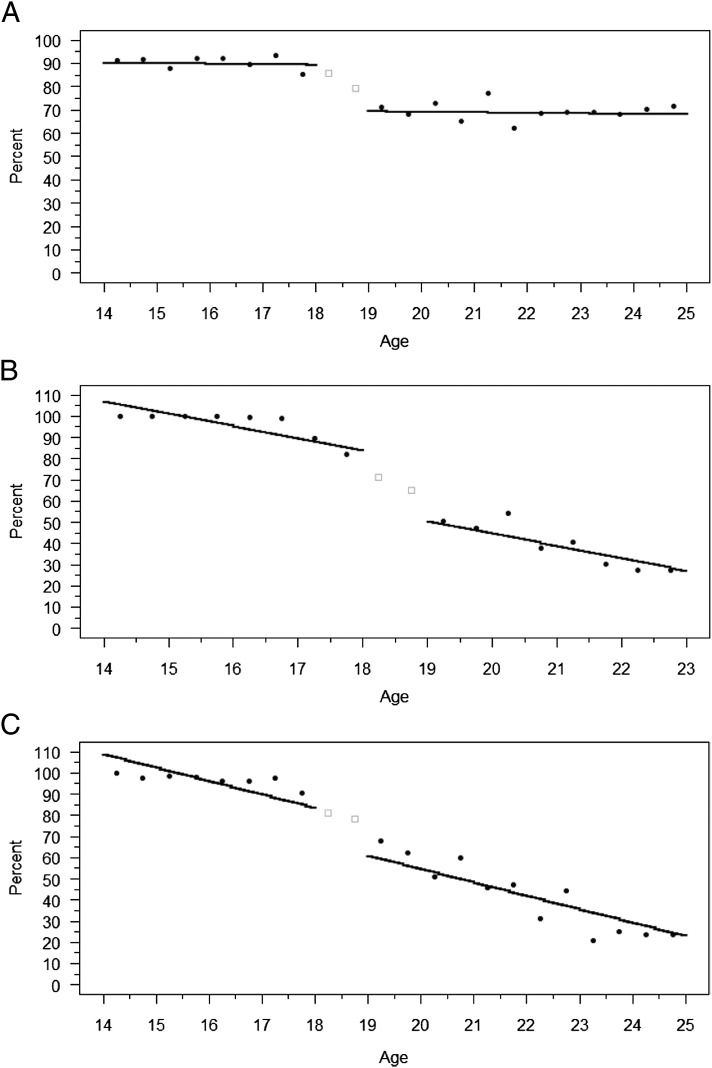
There were substantial differences between age groups in insurance coverage, schooling, and adult presence at home (Appendix Fig 2). Transitioning from continuous insurance coverage in year 1 to continuous uninsurance in year 2 was associated with a significant decrease in having a usual source of care in year 2 (change relative to no coverage loss: –25.2 percentage points; P = .003). Transitioning from continuous full-time schooling in year 1 to no schooling in year 2 was associated with significant reductions in reports of ≥1 primary care visit (change relative to no change in schooling: –21.1 percentage points; P = .03) and ≥1 preventive care visit (change relative to no change in schooling: –21.4 percentage points; P = .02). Transitioning from continuous adult presence at home in year 1 to continuous independent living in year 2 was associated with a significant increase in reports of filling a SABA prescription at least once (change relative to no loss of adult presence at home: +20.9 percentage points; P = .001) (Table 3).
TABLE 3.
Changes in Health Care Access and Utilization Associated With Changes in Insurance Coverage, Schooling, and Adult Presence at Home, Among Participants With Asthma Transitioning to Young Adulthood
| Year 2–Year 1 Absolute Change in Access or Utilization Measure | Access or Utilization Measure, Percentage Points | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Usual Source of Care | ≥1 Primary Care Visit | ≥1 Preventive Visit | ≥1 Fill of a Short-Acting beta-Agonist Prescription | ≥1 Fill of a Controller Medication Prescription | ||||||
| Estimate | P Value | Estimate | P Value | Estimate | P Value | Estimate | P Value | Estimate | P Value | |
| A. Participants with no change in insurance coverage, schooling, or adult presence at home | 0.7 | .76 | –5.1 | .12 | 3.4 | .41 | –7.0 | .006 | –2.2 | .29 |
| B. Differential change for participants losing insurance coverage (versus A) (transition from continuous insurance to continuous uninsurance) | –25.2 | .003 | –9.0 | .30 | –3.7 | .67 | –2.3 | .78 | –1.1 | .83 |
| C. Differential change for participants discontinuing schooling (versus A) (transition from continuous schooling to no schooling) | 1.0 | .89 | –21.1 | .03 | –21.4 | .02 | –10.2 | .16 | –10.2 | .07 |
| D. Differential change for participants losing adult presence at home (versus A) (transition from continuous adult presence at home to continuous independent living) | 2.8 | .72 | –2.1 | .83 | –10.4 | .35 | 20.9 | .001 | 4.0 | .42 |
Discussion
In this nationally representative study, young adults with asthma were less likely than older adolescents with asthma to have a usual source of care and less likely to use primary or preventive care. These findings suggest that young adults with asthma have worse health care access and receive suboptimal care, as national guidelines recommend that young adults with asthma be seen at least every 6 months to monitor control.11 Young adults with asthma were also less likely to fill SABA prescriptions and more likely to experience cost and coverage-related access problems. Most of these differences were reduced substantially after adjusting for differences in insurance coverage.
In addition, young adults with asthma were more likely to visit EDs, consistent with previous research demonstrating that young adults in general rely on EDs for care more than adolescents.8 Our findings suggest a possible substitution of ED care for primary care by young adults with asthma. Such a substitution would be economically inefficient because ED care is more expensive than office-based care for similar conditions,17 as well as clinically important if the substitution resulted from poor disease control or led to poorly coordinated care.
Differences in insurance coverage between age groups did not explain the higher ED use by young adults with asthma. This finding suggests that other factors were involved or that insurance coverage has offsetting effects on nonemergent and emergent ED use in this population. Previous research examining the role of insurance coverage in ED use has produced mixed results.18 In 1 quasi-experimental study, coverage losses at age 19 were associated with decreased overall ED use among young adults.19 In another study, however, individuals who gained Medicaid coverage through a lottery in Oregon did not significantly increase their ED use.20 The effects of insurance coverage on emergent and nonemergent ED use by young adults are unclear.
In longitudinal analyses of participants with asthma transitioning from adolescence to young adulthood, becoming uninsured strongly predicted losing a usual source of care. This finding is consistent with a previous cross-sectional study demonstrating that uninsured young adults are less likely to have a usual source of care than their insured counterparts.21 Becoming uninsured was also associated with a large decrease in primary care visits, although this change was not statistically significant.
Discontinuing schooling was associated with decreased use of primary and preventive care, whereas transitioning to independent living was associated with greater fills of SABA prescriptions. There are several potential explanations for these findings. Nonstudents may face greater time costs when accessing primary and preventive care than full-time students, who are more likely to have convenient access to student health services.22 Previous research suggests that familial support improves asthma control in adolescents.23 As such, it is possible that individuals with asthma develop worse disease control after moving away from their families, leading to greater SABA inhaler use. Because of a lack of data on such mediators, however, we could not empirically test these potential explanations.
Our study has several other limitations. First, we could not examine ED visits for asthma exacerbations or otherwise measure asthma control. Second, we excluded participants aged 18 from cross-sectional analyses because many transitions in insurance, schooling, and living situations occur at this age. However, these transitions could have occurred earlier or later for any given participant. Third, inconsistencies between proxy and self-reports may have contributed to reported differences in access and utilization between age groups. However, our cross-sectional results did not substantively change when we excluded older participants who consistently self-reported information because they no longer lived with their families. Thus, any reporting bias was likely small, consistent with previous studies demonstrating high concordance between parent and adolescent reports of asthma-related office visits, ED visits, and medication use.24,25
Finally, we did not adjust our comparisons for socioeconomic status because of inconsistencies in the meaning of household income information across age groups. Specifically, for participants living with their parents and unmarried college students living away from home, household income information collected by the survey usually refers to parental income. For young adults living independently, however, this information represents the young adult’s income.
Our findings have important clinical implications. Many adolescents with asthma may experience disruptions in care as they become young adults, with potentially deleterious clinical consequences. Disruptions may be particularly pronounced for adolescents with asthma who lose insurance coverage, discontinue schooling, and move away from home. For these patients, pediatric clinicians could implement comprehensive plans to facilitate smooth transitions to adult care.26
Our findings also have important policy implications. The ACA allows dependent children to remain on private family policies until age 26 and will expand Medicaid eligibility to childless adults with incomes up to 133% of the federal poverty level starting in 2014.3 Thus, as the ACA is implemented, the number of uninsured young adults will likely fall dramatically. Our study suggests that these coverage expansions may substantially improve access to care for young adults with asthma. Indeed, implementation of the ACA dependent coverage provision in 2010 has already been associated with modest reductions in uninsurance among young adults,4,27 and similar state laws in 2005–2006 were associated with improved access among young adults.28 Our study also suggests that expanding coverage may improve care for young adults with asthma. Adjusting for differences in insurance coverage in this population explained 32% of their lower use of primary care and 47% to 61% of their greater problems accessing medical care or medications because of cost or coverage issues.
Differences in insurance coverage, however, did not fully explain differences in access or use of recommended care between adolescents and young adults with asthma. We identified other social factors that may contribute to differences in primary and preventive care use. In addition, differences in coverage did not substantially explain the higher ED use among young adults with asthma. These findings suggest that coverage expansions supported by the ACA might not fully address suboptimal utilization patterns among young adults with asthma.
Conclusions
Compared with older adolescents with asthma, young adults with asthma have worse health care access and may use care less optimally. Although losing insurance coverage may contribute to these differences, other social factors may also play important roles.
Glossary
- ACA
Affordable Care Act
- ED
emergency department
- MEPS
Medical Expenditure Panel Survey
- SABA
short-acting beta-agonist
Appendix
Specification and Interpretation of Linear Regression Models Used for Longitudinal Comparisons
In our longitudinal analyses, we fitted the following linear regression model: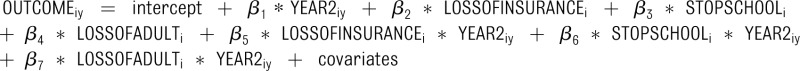
In this model, OUTCOMEiy is the outcome for individual i in year y (1 or 2) and YEAR2iy is a dummy variable that indicates whether the data for individual i comes from year y (1 or 2). LOSSOFINSURANCEi, STOPSCHOOLi, and LOSSOFADULTi are the predictor variables describing changes in insurance coverage, schooling, and adult presence at home between year 1 and year 2 for individual i. Covariates include age dummies representing age in years at the beginning of MEPS participation, gender, race, region in year 1, residence in a Metropolitan Statistical Area in year 1, and data year (MEPS panel). The following describes the interpretation of the coefficients of interest:
β1: The change in outcome between year 1 and year 2, in the absence of changes in insurance coverage, schooling, or adult presence at home from year 1 to year 2.
β5: The additional/differential change in outcome in year 2 (relative to β1) that is associated with transitioning from continuous insurance coverage in year 1 to continuous uninsurance in year 2, controlling for changes in schooling and adult presence at home.
β6: The additional/differential change in outcome in year 2 (relative to β1) that is associated with transitioning from continuous full-time schooling in year 1 to no schooling in year 2, controlling for changes in insurance coverage and adult presence at home.
β7: The additional/differential change in outcome in year 2 (relative to β1) that is associated with transitioning from continuous adult presence at home in year 1 to continuous independent living in year 2, controlling for changes in insurance coverage and schooling.
Additional Analyses Addressing Potential Response Bias
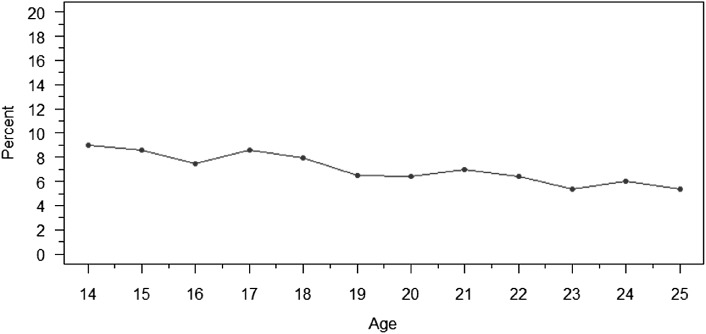
One potential threat to our study is sample selection bias introduced by age-related differences in responses to asthma-related questions, thereby leading to compositional differences between age groups in asthma severity and other unobserved factors. However, the results of our cross-sectional analyses were consistent with the results of our longitudinal analyses, in which there was no age-related compositional change in the sample by definition. Thus, age-related compositional changes in our sample are unlikely to explain our findings. In addition, we examined the age profile of asthma prevalence, using the definition of asthma from the cross-sectional analyses. If there were differential entry into the sample because young adults with asthma were more or less likely to report asthma-related health care utilization or a current diagnosis of asthma, one would expect an abrupt change in asthma prevalence around age 18. However, as shown in the graph of age-specific asthma prevalence in Appendix Figure 1, there is no evidence of such a change.
APPENDIX FIGURE 1.
Age-specific asthma prevalence in cross-sectional sample, MEPS 1999–2009.
APPENDIX FIGURE 2.
Changes in health insurance coverage, schooling, and adult presence at home among participants aged 14 to 25 with asthma, MEPS 1999–2009. A, Percentage of months with health insurance coverage; B, percentage of participants who were full-time students for all or most of the year; C, percentage of participants who had a continuous adult presence at home for all or most of the year. Student status information was collected only from participants aged 17 to 23 in the MEPS. To construct the graph of changes in schooling, we assumed that all participants aged 14 to 16 were full-time students and excluded data from participants aged 24 to 25. Using data from MEPS rounds 1 to 3 or 3 to 5, we classified participants as full-time students for all or most of the year if they were full-time students at the end of at least 2 of the 3 rounds. We applied similar criteria to identify participants with continuous adult presence at home for all or most of the year. To classify the small number of participants with missing data for schooling or adult presence at home, we used the rounds for which data were available for these individuals. The square data points represent excluded data for participants aged 18.
Footnotes
Dr Chua performed all analyses and drafted the initial manuscript; Drs Schuster and McWilliams assisted with interpretation and refinement of analyses and assisted with drafting the manuscript; and all authors conceptualized and designed the study and approved the final manuscript as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Chua was supported by the Harvard Pediatric Health Services Research Fellowship (AHRQ NRSA 5T32HS00063-17). Dr McWilliams was supported by grants from the Beeson Career Development Award Program (National Institute on Aging K08 AG038354 and the American Federation for Aging Research) and Doris Duke Charitable Foundation (Clinical Scientist Development Award #2010053).
References
- 1.Aud S, Hussar W, Johnson F, et al. The Condition of Education 2012 (NCES 2012-045). Washington, DC: US Department of Education, National Center for Education Statistics; 2012 [Google Scholar]
- 2.Parker K. The Boomerang Generation. Washington, DC: Pew Research Center; 2012 [Google Scholar]
- 3.Collins S, Nicholson J. Rite of Passage: Young Adults and the Affordable Care Act of 2010. Washington, DC: Commonwealth Fund; 2010 [PubMed] [Google Scholar]
- 4.DeNavas-Walt C, Proctor B, Smith J. Income, Poverty, and Health Insurance Coverage in the United States: 2011. Washington, DC: US Census Bureau; 2012 [Google Scholar]
- 5.Fortuna RJ, Robbins BW, Mani N, Halterman JS. Dependence on emergency care among young adults in the United States. J Gen Intern Med. 2010;25(7):663–669 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Fortuna RJ, Robbins BW, Halterman JS. Ambulatory care among young adults in the United States. Ann Intern Med. 2009;151(6):379–385 [DOI] [PubMed] [Google Scholar]
- 7.Callahan ST, Cooper WO. Changes in ambulatory health care use during the transition to young adulthood. J Adolesc Health. 2010;46(5):407–413 [DOI] [PubMed] [Google Scholar]
- 8.Centers for Disease Control and Prevention. 2010 Adult Asthma Data: Prevalence Tables and Maps. September 26, 2011. Available at: www.cdc.gov/asthma/brfss/2010/current/tableC3.htm. Accessed August 10, 2012
- 9.Akinbami L, Moorman J, Liu X. Asthma Prevalence, Health Care Use, and Mortality: United States, 2005–2009. National Center for Health Statistics; No. 32. Hyattsville, MD: National Center for Health Statistics, 2011. [PubMed] [Google Scholar]
- 10.National Health, Lung, and Blood Institute Expert Panel Report 3: Guidelines for the Diagnosis and Management of Asthma. Bethesda, MD: National Institutes of Health; 2007 [Google Scholar]
- 11.Agency for Healthcare Research and Quality. Prevention quality indicators overview. February 2006. Available at: www.qualityindicators.ahrq.gov/Modules/pqi_overview.aspx. Accessed August 10, 2012
- 12.Agency for Healthcare Research and Quality. MEPS HC-129: 2009 full year consolidated data file. November 2011. Available at: http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h129/h129doc.pdf. Accessed August 10, 2012
- 13.Agency for Healthcare Research and Quality. MEPS HC-126G: 2009 office-based medical provider visits. November 2011. Available at: http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h126g/h126gdoc.pdf. Accessed August 10, 2012
- 14.Agency for Health Care Research and Quality. MEPS HC-126A: 2009 prescribed medicines. September 2011. Available at: http://meps.ahrq.gov/mepsweb/data_stats/download_data/pufs/h126a/h126adoc.pdf. Accessed August 10, 2012
- 15.Chapman C, Laird J, Ifill N, KewalRamani A. Trends in High School Dropout and Completion Rates in the United States: 1972-2009 (NCES 2012-006). Washington, DC: US Department of Education, National Center for Education Statistics; 2011 [Google Scholar]
- 16.Binder D. On the variances of asymptotically normal estimators from complex surveys. Int Stat Rev. 1983;57:279–292 [Google Scholar]
- 17.Mehrotra A, Liu H, Adams JL, et al. Comparing costs and quality of care at retail clinics with that of other medical settings for 3 common illnesses. Ann Intern Med. 2009;151(5):321–328 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Newton MF, Keirns CC, Cunningham R, Hayward RA, Stanley R. Uninsured adults presenting to US emergency departments: assumptions vs data. JAMA. 2008;300(16):1914–1924 [DOI] [PubMed] [Google Scholar]
- 19.Anderson M, Dobkin C, Gross T. The effect of health insurance coverage on the use of medical services. American Economic Journal: Economic Policy. 2012;4(1):1–27 [Google Scholar]
- 20.Finkelstein A, Taubman S, Wright B, et al. The Oregon Health Insurance Experiment: Evidence from the First Year. National Bureau of Economic Research Working Paper 17190. Cambridge, MA: National Bureau of Economic Research; 2011
- 21.Callahan ST, Cooper WO. Uninsurance and health care access among young adults in the United States. Pediatrics. 2005;116(1):88–95 [DOI] [PubMed] [Google Scholar]
- 22.McBride D, Van Orman S, Wera C, Leino V. ACHA Benchmarking Committee Report: 2010 Survey on the Utilization of Student Health Services. Hanover, MD: American College Health Association; 2010 [Google Scholar]
- 23.Rhee H, Belyea MJ, Brasch J. Family support and asthma outcomes in adolescents: barriers to adherence as a mediator. J Adolesc Health. 2010;47(5):472–478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ungar WJ, Davidson-Grimwood SR, Cousins M. Parents were accurate proxy reporters of urgent pediatric asthma health services: a retrospective agreement analysis. J Clin Epidemiol. 2007;60(11):1176–1183 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hedman L, Bjerg A, Perznowski M, Ronmark E. Good agreement between parental and self-completed questionnaires about allergic disease and environmental factors in teenagers. J Clin Epidemiol. 2010;63(7):783–789 [DOI] [PubMed] [Google Scholar]
- 26.American Academy of Pediatrics. American Academy of Family Physicians. American College of Physicians–American Society of Internal Medicine . A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 pt 2):1304–1306 [PubMed] [Google Scholar]
- 27.Sommers BD, Kronick R. The Affordable Care Act and insurance coverage for young adults. JAMA. 2012;307(9):913–914 [DOI] [PubMed] [Google Scholar]
- 28.Blum AB, Kleinman LC, Starfield B, Ross JS. Impact of state laws that extend eligibility for parents’ health insurance coverage to young adults. Pediatrics. 2012;129(3):426–432 [DOI] [PMC free article] [PubMed] [Google Scholar]