Abstract
BACKGROUND AND OBJECTIVE:
Active smoking and secondhand smoke (SHS) are known risk factors for kidney disease in adults. We evaluated the association between exposure to active smoking or SHS and kidney function in US adolescents.
METHODS:
This is a cross-sectional study in 7516 adolescents aged 12–17 who participated in NHANES 1999–2010 and had serum creatinine and cotinine measures. Active smoking was defined as self-reported smoking or serum cotinine concentrations >10 ng/mL. SHS was defined as nonactive smokers who self-reported living with ≥1 smokers or serum cotinine concentrations ≥ 0.05 ng/mL. Kidney function was determined by using the chronic kidney disease in children estimated glomerular filtration rate (eGFR) equation.
RESULTS:
Median (interquartile range) eGFR and serum cotinine concentrations were 96.8 (85.4–109.0) mL/minute per 1.73 m2 and 0.07 (0.03–0.59) ng/mL, respectively. After multivariable adjustment, eGFR decreased 1.1 mL/minute per 1.73 m2 (95% confidence interval [CI]: −1.8 to −0.3) per interquartile range increase in serum cotinine concentrations. The mean (95%CI) difference in eGFR for serum cotinine tertiles 1, 2, and 3 among children exposed to SHS compared to unexposed were −0.4 (−1.9 to 1.2), −0.9 (−2.7 to 0.9), and −2.2 (−4.0 to −0.4) mL/minute per 1.73 m2, respectively (P = .03). The corresponding values among tertiles of active smokers compared to unexposed were 0.2 (−2.2 to 2.6), −1.9 (−3.8 to 0.0), and −2.6 (−4.6 to −0.6) mL/minute per 1.73 m2 (P = .01).
CONCLUSIONS:
Tobacco smoke exposure was associated with decreased eGFR in US adolescents, supporting the possibility that tobacco smoke effects on kidney function begin in childhood.
Keywords: adolescents, cotinine, creatinine, secondhand smoke, smoking, tobacco smoke pollution
What’s Known on This Subject:
Active smoking and secondhand smoke are associated with chronic kidney disease in adults. No data are available for children.
What This Study Adds:
Secondhand smoke and active smoking were associated with decreased estimated glomerular filtration rate in US adolescents. These findings support that tobacco smoke effects on kidney function begin in childhood.
Tobacco use and exposure to secondhand tobacco smoke are major health problems for adolescents, resulting in short-term and long-term adverse health effects.1,2 In the United States, more than 600 000 middle school students and 3 million high school students smoke cigarettes.1,3 Approximately 15% of nonsmoking adolescents self-report exposure to secondhand smoke at home.4 In adolescents, active smoking has been associated with increased asthma risk,5,6 reduced lung function and growth,7–9 early atherosclerotic lesions,10–13 and increased cancer risk and premature mortality in adulthood.14,15 Furthermore, tobacco use during adolescence increases the risk of heavier smoking in adulthood because of early nicotine addiction.1 Secondhand smoke exposure at a young age has been associated with increased risk of asthma,16 reduced lung function,9 endothelial dysfunction,17,18 and neurocognitive deficits,19 and increased probability of smoking during adolescence and early adulthood.1
Evidence from adult populations supports that active smoking is a risk factor for chronic kidney disease (CKD).20–27 Some studies also support the association between secondhand tobacco smoke and CKD in adults.20,22,26 No studies have evaluated these associations in children. Children and adolescents may be a more ideal population in which to examine the association between tobacco smoke and kidney function as they have a very low prevalence of CKD and are much less likely to be affected by common, and potentially confounding, CKD risk factors such as diabetes and hypertension.28 The objective of this study was to examine the relationship of active smoking and secondhand smoke exposure with glomerular filtration rate (eGFR) estimated by the creatinine-based bedside Chronic Kidney Disease in Children (CKiD) equation in US adolescents 12 to 17 years of age.
Methods
Study Population
Between 1999 and 2010, the National Health and Nutrition Examination Survey (NHANES) examined a nationally representative sample of ∼5000 persons each year by using a complex multistage sample design.29 The NHANES protocol was reviewed and approved by the National Center for Health Statistics Institutional Review Board. For participants < 18 years, informed consent was provided by the participants and their guardians. The participation rate for children 12 to 17 years old completing the questionnaires and physical examinations during the NHANES 1999–2010 was 85.8%.30
For this study, we selected 9155 adolescents 12 to 17 years of age who participated in the NHANES 2009–2010. We then excluded participants having missing values of serum creatinine or serum cotinine (N = 1236), as well as those without information on BMI or parental education (N =354). We also excluded 49 adolescents who were pregnant, leaving 7516 participants for these analyses. Participants included in this analysis were similar with respect to age, gender, and race/ethnicity compared with the original sample of adolescent in the NHANES 2009–2010 (data not shown).
Exposure Assessment
Tobacco use and exposure to secondhand smoke were assessed by using self-reported data from the home questionnaire and serum cotinine, a specific biomarker of tobacco exposure.31,32 Participants self-reporting having smoked “at least one day” in the last month (NHANES 1999–2010) or “at least one cigarette” in the last month (NHANES 2005–2010), or those who had serum cotinine concentrations over 10 ng/mL regardless of their self-reported information, were classified as active smokers (N = 927).33,34 Secondhand smoke exposure was defined as nonactive smokers who self-reported living with at least 1 person who smoked (independent of their cotinine levels), or who had cotinine levels ≥ 0.05 ng/mL but ≤10 ng/mL even if they reported not living with a smoker (N = 3692). Participants with serum cotinine levels below 0.05 ng/mL, not living with a smoker, and not smoking in the last month were classified as unexposed to tobacco (N = 2897).
Serum cotinine was measured by an isotope dilution-high performance liquid chromatography/atmospheric pressure chemical ionization tandem mass spectrometry.35 The limit of detection (LOD) for serum cotinine was 0.05 ng/mL for the NHANES 1999–2000 and the first phase of the NHANES 2001–2002, and 0.015 ng/mL for the second phase of the NHANES 2001–2002 and thereafter. In the study sample, serum cotinine levels were undetectable for 24% of the participants. Serum cotinine concentrations below the LOD were replaced by the LOD divided by the square root of 2. The interassay coefficients of variation for serum cotinine ranged from 1.1% to 9.0%.36,37
Outcome Assessment
Serum creatinine was measured by the modified kinetic Jaffé reaction. The interassay coefficients of variation ranged from 0.1% to 4.4%.38,39 To standardize serum creatinine measurements to a “gold standard” reference method as recommended by the National Kidney Disease Education Program,40 the NHANES also analyzed serum creatinine in a subset of participants by using a coupled enzymatic assay with calibrators traceable to an isotope dilution mass spectrometric method for serum creatinine (gold standard). Because a significant difference existed between creatinine determined by the modified Jaffé reaction and the enzymatic method in the NHANES 1999–2000 and the NHANES 2005–2006, the NHANES recommended the following corrections:
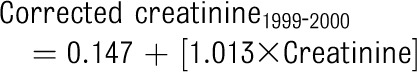 |
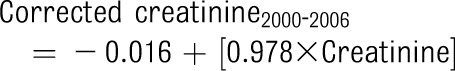 |
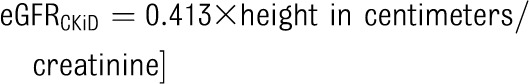
Several creatinine-based equations can be used to estimate kidney function in adolescents.41 We performed all analyses by using the original Schwartz42 and the novel bedside CKiD equations43:
 |
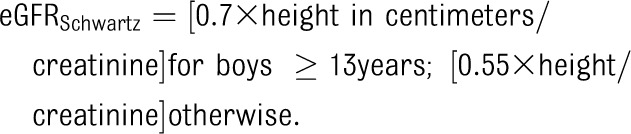 |
The findings were the same using both equations, and we present the results based on the novel bedside CKiD equation because it was also derived by using creatinine measurements that are traceable to a gold standard method.
Other Variables
Questionnaire information included gender, age, education of the household reference person (less than high school, high school, and more than high school), and race/ethnicity (non-Hispanic white, non-Hispanic black, Mexican-American, other). Measured height and weight were obtained during the physical examination. BMI percentiles were calculated based on the Centers for Disease Control and Prevention’s BMI for age and gender specific growth charts, and categorized as normal, overweight, and obese if BMI percentiles were ≤84, 85–94, and ≥95, respectively. Blood pressure measurements were obtained by manual auscultation with a mercury-gravity manometer by using a standardized protocol,44 and systolic and diastolic blood pressure percentiles were calculated by using established methods.45
Statistical Analyses
Statistical analyses were performed in STATA version 11.0 statistical software (Stata Corp, College Station, TX) by using the survey (svy) command to account for the complex sampling design and weights in the NHANES.
The distribution of eGFR was determined for participants in each of the tobacco exposure categories (unexposed, secondhand smoke, and active smokers). To evaluate the association of tobacco exposure with eGFR, first we estimated the mean difference in eGFR levels by serum cotinine concentrations by using linear regression models. Cotinine concentrations were modeled as (1) tertiles among secondhand smoke exposed participants and active smokers, respectively, compared with unexposed participants; (2) interquartile range (IQR) increase; and (3) restricted cubic spline models with knots at 10th, 50th, and 90th percentiles in all participants. We evaluated crude models, models adjusted for age and gender, and models further adjusted for parental education status, race/ethnicity, BMI, and survey year. We further adjusted for household income, systolic blood pressure percentile, and birth weight in the subsample of participants with this information available (N = 4578). Also, because the bedside CKiD equation accounts for the relationship between creatinine production and muscle mass by using height as a surrogate, we adjusted for potential differences in lean body mass in the subset of participants with dual-energy radiograph absorptiometry data in the NHANES 1999–2004.46 The results were similar after adjustment for lean body mass (data not shown).
To evaluate the consistency of our findings, we conducted the following sensitivity analyses. First, we estimated the mean eGFR levels by IQR increase in log-transformed serum cotinine in models stratified by gender, age, parental education, race/ethnicity, BMI, and birth weight. This was an exploratory analysis because we had no a priori hypothesis for potential effect modification between smoking and the variables evaluated. Second, we repeated all the analyses estimating GFR by using the Schwartz equation instead of the CKiD equation. Third, we evaluated the association between serum cotinine concentrations and log-transformed urinary albumin-to-creatinine ratio (ACR) in the subsample of 2009–2010 NHANES participants with a first-morning urine sample available (N = 858).47
Results
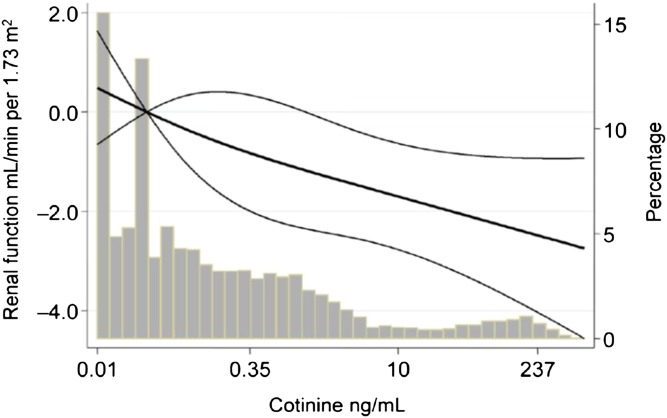
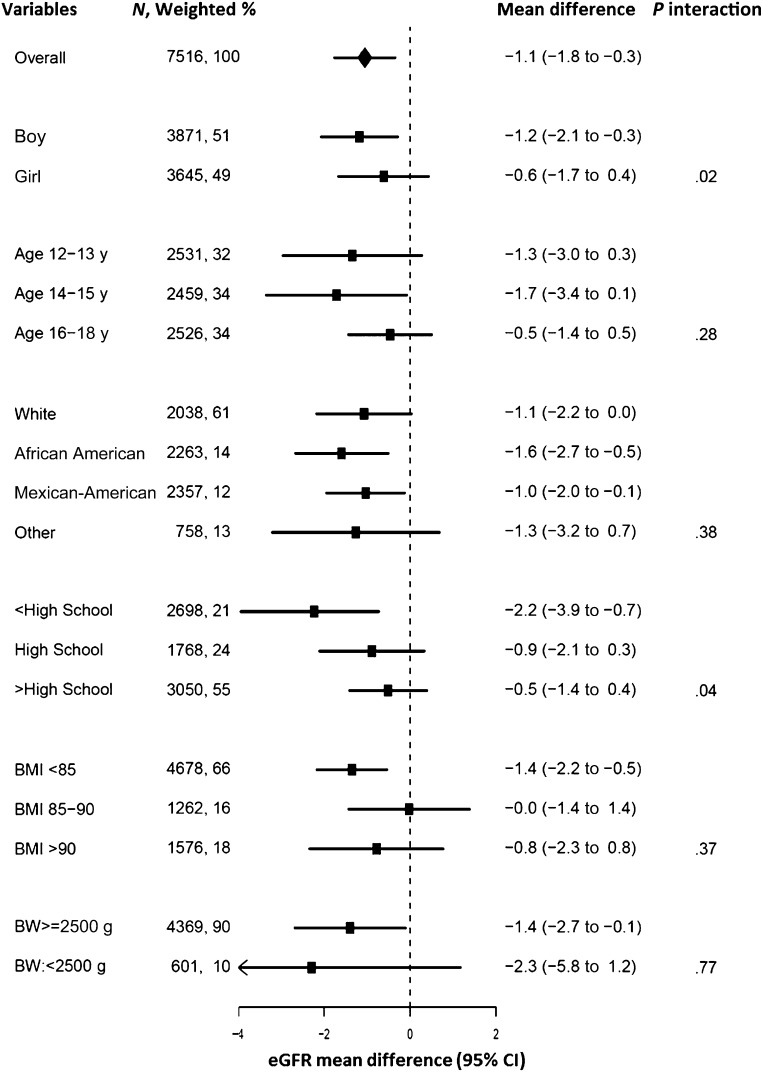
Median (IQR) eGFR in participants unexposed to tobacco was 99.1 (88.1–111.0) mL/minute per 1.73 m2 compared with 96.8 (85.0–109.0) mL/minute per 1.73 m2 among participants exposed to secondhand smoke and 90.1 (81.3–100.9) mL/minute per 1.73 m2 among active smokers. Older adolescents, boys, Mexican-American, and African American participants, and participants with lower parental education and higher BMI were more likely to smoke (Table1). Secondhand smoke exposure was more common in boys, younger adolescents, adolescents with lower parental education, and those who were obese. After multivariate adjustment, the mean (95% confidence interval [CI]) difference in eGFR for serum cotinine tertiles 1, 2, and 3 among children exposed to secondhand smoke compared with unexposed were −0.4 (−1.9 to 1.2), −0.9 (−2.7 to 0.9), and −2.2 (−4.0 to −0.4) mL/minute per 1.73 m2, respectively (P = .03) (Table 2). The corresponding mean (95% CI) difference in eGFR for serum cotinine tertiles 1, 2, and 3 among active smokers compared with unexposed were 0.2 (−2.2 to 2.6), −1.9 (−3.8 to −0.0), and −2.6 (−4.6 to −0.6) mL/minute per 1.73 m2, respectively (P = .01). In a flexible analysis of the dose-response relationship using restricted cubic splines, eGFR levels decreased progressively with increasing serum cotinine concentrations and with no evidence of a threshold (Fig 1). After multivariable adjustment, an IQR increase in serum cotinine concentrations was associated with a mean difference in eGFR of −1.1 (95% CI: −1.8 to −0.3) mL/minute per 1.73 m2 (Fig 2). After further adjustment for birth weight, blood pressure, and household income in the subsample of participants with information available (N = 4578), an IQR increase in serum cotinine concentrations was associated with a mean difference in eGFR of −1.5 (95% CI: −2.4 to −0.6) mL/minute per 1.73 m2. Adjustment by lean body mass in the subsample of participants with body composition data available (N = 3780) revealed similar results, with a mean decrease of −0.9 (95% CI: −1.8 to −0.0) mL/minute per 1.73 m2 for an IQR increase in serum cotinine concentrations.
TABLE 1.
Median (IQR) Serum Cotinine (ng/mL), Median (SD) eGFR (mL/min per 1.73 m2), and Tobacco Smoke Exposure Status by Participant Characteristics in US Adolescents 12 to 17 Years of Age
| Overall (N = 7516) | Unexposed (N = 2897) | SHS (N = 3692) | Active Smoking (N = 927) | ||
|---|---|---|---|---|---|
| Median eGFR (IQR) | Median Serum Cotinine (IQR) | Weighted % | Weighted % | Weighted % | |
| Overall | 96.8 (85.4–109.0) | 0.07 (0.03–0.59) | |||
| Gender | |||||
| Boy | 92.9 (81.8–105.4) | 0.09 (0.03–0.72) | 37.1 | 48.1 | 14.8 |
| Girl | 99.9 (90.0–112.0) | 0.06 (0.02–0.49) | 43.4 | 43.0 | 13.6 |
| Age, y | |||||
| 12–13 | 106.7 (96.3–119.4) | 0.05 (0.02–0.33) | 43.4 | 53.0 | 13.6 |
| 14–15 | 96.2 (86.4–106.4) | 0.07 (0.02–0.51) | 42.9 | 44.2 | 12.9 |
| 16–17 | 88.23 (78.9–99.1) | 0.11 (0.03–1.58) | 34.0 | 40.2 | 25.8 |
| Ethnicity | |||||
| White | 96.3 (85.6–107.7) | 0.08 (0.02–1.14) | 56.2 | 34.7 | 1.0 |
| African American | 92.3 (81.4–104.4) | 0.23 (0.05–1.03) | 45.8 | 40.2 | 14.0 |
| Mexican | 102.1 (89.7–116.4) | 0.04 (0.02–0.13) | 40.5 | 42.8 | 16.7 |
| Other | 99.1 (86.4–112.8) | 0.05 (0.02–0.37) | 22.3 | 68.2 | 9.5 |
| Education | |||||
| <High school | 98.1 (85.5–111.2) | 0.02 (0.04–0.21) | 31.5 | 52.0 | 16.5 |
| High school | 96.9 (84.9–109.0) | 0.04 (0.19–1.24) | 26.4 | 55.8 | 17.8 |
| >High school | 96.2 (85.7–108.1) | 0.14 (0.04–0.98) | 49.6 | 38.7 | 11.7 |
| BMI (percentile) | |||||
| Normal weight (≤84) | 96.1 (85.0–108.5) | 0.05 (0.02–0.45) | 43.1 | 42.7 | 14.2 |
| Overweight (85–94) | 97.1 (85.8–108.3) | 0.06 (0.02–0.57) | 35.2 | 49.0 | 15.8 |
| Obese (≥95) | 97.4 (85.7–110.0) | 0.08 (0.03–0.65) | 33.9 | 53.4 | 12.7 |
| Birth weight | |||||
| Normal weight (≥2500 g) | 101.5 (90.5–112.8) | 0.05 (0.22–0.37) | 44.0 | 48.0 | 8.0 |
| Underweight (<2500 g) | 99.2 (88.5–112.0) | 0.10 (0.03–0.67) | 38.3 | 53.6 | 8.1 |
SHS, secondhand smoke.
TABLE 2.
Mean Difference (95% CI) of eGFR by Serum Cotinine Concentrations in US Adolescents 12 to 17 Years of Age
| Exposure Categorya (Cotinine Levels) | N | Model 1 | Model 2 | Model 3 |
|---|---|---|---|---|
| Unexposed <0.05 ng/mL | 2897 | 0.0 (reference) | 0.0 (reference) | 0.0 (reference) |
| Secondhand smoke | ||||
| 0.05–0.10 ng/mL | 1182 | −1.7 (−3.5 to 0.1) | −1.0 (−2.7 to 0.7) | −0.4 (−1.9 to 1.2) |
| 0.10–0.54 | 1326 | −2.8 (−4.9 to −0.6) | −2.3 (−4.2 to −0.4) | −0.9 (−2.7 to 0.9) |
| 0.55–10 | 1184 | −3.5 (−5.8 to −1.3) | −3.7 (−5.7 to −1.6) | −2.2 (−4.0 to −0.4) |
| P trendb | <.001 | <.001 | .03 | |
| Active smoking | ||||
| 0.05–12 ng/mL | 335 | −4.3 (−7.1 to −1.6) | 0.09 (−2.4 to 2.6) | 0.2 (−2.2 to 2.6) |
| 12–103 | 319 | −9.8 (−12 to −7.7) | −2.5 (−4.5 to −0.5) | −1.9 (−3.8 to −0.0) |
| ≥104 | 273 | −11.7 (−14.0 to −9.4) | −3.5 (−5.8 to −1.3) | −2.6 (−4.6 to −0.6) |
| P trendb | <.001 | <.001 | <.01 | |
| Per IQR increase in serum cotinine | 7516 | −3.9 (−4.6 to −3.2) | −1.38 (−2.1 to −0.6) | −1.1 (−1.8 to −0.3) |
Model 1, crude; model 2, adjusted for age and gender; model 3, further adjusted for BMI, parental educational level, race/ethnicity, and NHANES year.
Secondhand smoke and active smoking categories were divided into tertiles according to serum cotinine concentrations within each category.
P values for trend were obtained separately for participants exposed to secondhand smoke and for active smoking.
FIGURE 1.
eGFR by serum cotinine concentrations. Mean eGFR difference (thick line) and 95% CIs (thin lines) by serum cotinine concentrations modeled by using restricted cubic splines for log-cotinine concentrations with knots at the 10th, 50th, and 90th percentile. The reference value is set at the 30th percentile of the cotinine distribution. Mean eGFR differences were adjusted for gender, age, race/ethnicity, parental educational level, BMI, and survey year. Vertical bars represented the histogram of the serum cotinine distribution. The first and fourth bars in the histogram correspond to participants who were below the LOD in the NHANES 1999–2000 (0.05 ng/mL) and the NHANES 2001–2010 (0.015 ng/mL). Participants below the LOD were replaced by the LOD divided by the square root of 2.
FIGURE 2.
Mean (95% CI) eGFR difference per IQR increase in serum cotinine concentrations by participant characteristics. Mean differences were adjusted for gender, age, race/ethnicity, parental educational level, BMI, and survey year. Dots represent the mean difference and horizontal lines the CIs. The P value indicates the level of significance for interaction for each participant subgroup and was estimated by using the Wald test.
Stratified analyses by participant characteristics revealed decreased eGFR associated with increased serum cotinine concentrations across all subgroups evaluated (Fig 2). Effect modification was statistically significant by gender and parental education. Mean difference in eGFR levels for an IQR increase in serum cotinine concentrations was stronger for boys (−1.2 [95% CI: −2.1 to −0.3] mL/minute per 1.73 m2) compared with girls (−0.6 [95% CI: −1.7 to −0.4] mL/minute per 1.73 m2). By parental education, mean eGFR levels for an IQR increase in serum cotinine concentrations was stronger among adolescents whose parents had less than high school education (−2.2 [−3.9 to −0.7] mL/minute per 1.73 m2). To evaluate if gender differences were related to a higher tobacco dose among boys (Table 1), we matched 2300 boys and 2300 girls on age and serum cotinine concentrations. In this subsample, the difference in eGFR levels for an IQR increase in serum cotinine concentrations were −3.1 (−4.4 to −1.9) ng/mL for boys and −2.6 (−4.0 to −1.3) ng/mL for girls.
When using the Schwartz equation instead of the CKiD equation, the mean difference in eGFR levels for an IQR increase in serum cotinine concentrations was −2.0 (95% CI: −3.0 to −1.0) mL/minute per 1.73 m2. Finally, in the 858 NHANES 1999–2010 participants with urine albumin measured on a first-morning urine sample (median ACR, 8.1; IQR, 4.8–15.0), the geometric mean of ACR was 3.4 times (95% CI: 3.2–3.6) higher for an IQR increase in serum cotinine concentrations.
Discussion
Despite important progress in tobacco control in the United States in recent decades, a large number of adolescents continue to smoke and remain exposed to secondhand tobacco smoke.1–3 Although previous evidence supports that tobacco smoke can affect kidney function in adult populations, the detrimental effect of tobacco smoke on kidney function in adolescents has not been evaluated before. In this nationally representative sample of US adolescents, exposure to tobacco, including secondhand smoke and active smoking, was associated with a lower eGFR. eGFR decreased linearly with increasing serum cotinine concentrations after adjustment for sociodemographic characteristics, BMI, and parental education with no evidence of a threshold. Our findings were robust to different sensitivity analyses. We also found a modest but positive association between serum cotinine concentrations and first morning ACR, further supporting that tobacco smoke may damage the kidneys.
Evidence from studies in adult populations suggest that smoking, particularly heavy smoking and cumulative smoking exposure, is an independent risk factor for CKD in both genders, as shown in large, prospective observational studies.48 Data from a community-based prospective cohort study conducted among 23 534 men and women from Washington County, Maryland, revealed a positive association between smoking and the risk of CKD after 20 years of follow-up.23 Similarly, during a 10-year follow-up study of adults 40 years and older who received community-based annual examinations in Japan, baseline smoking was associated with CKD stages III or higher.26 In adults over 18 years of age who participated in the NHANES III, current smokers were also more likely to have albuminuria than never smokers, and participants with hypertension were at an increased risk of albuminuria when exposed to secondhand smoke.20 However, evidence on secondhand smoke and CKD is inconclusive.2 In children, no population-based studies have evaluated the association between tobacco and kidney function.
Several mechanisms may explain tobacco smoke effects on the kidneys. Nicotine-induced mesangial cell proliferation is well established in cell culture models,49–51 and this histopathological change has also been observed in kidney biopsies of active smokers.52 Tobacco smoke could promote local oxidative stress and increases in the production of angiotensin II.53–55 Evidence from animal models and some evidence from epidemiologic studies support that angiotensin-converting enzyme inhibition protects against smoking-induced kidney function decline.56,57 Additionally, tobacco represents a major source of exposure to cadmium and lead, established nephrotoxicants at relatively low levels of exposure.28,58,59
The association between serum cotinine and eGFR was stronger in children whose parents had lower education levels, and also in boys. These are posthoc findings and need to be interpreted with caution. The association with lower education could be related to several factors: (1) adult smokers with lower education may expose their children more intensively to secondhand smoke60; (2) children whose parents had lower education levels were more likely to be active smokers; (3) lower parental education may be associated with coexposure to other environmental toxicants that could adversely affect the kidneys28; and (4) lower parental education could also be a marker for other factors that could affect kidney function such as low birth weight, diet, and health care access. Regarding differences observed by gender, some studies have described stronger kidney effects related to tobacco smoke exposure in men,21,61 with some authors suggesting that women’s kidney function may be protected by the effects of estrogens.62 However, it is also possible that differences in tobacco dose (higher dose in males versus females as suggested in our study, see Table 1) could also play a role. In our posthoc matched analysis, the association between serum cotinine concentrations and eGFR levels were largely similar for boys and girls. Larger community-based studies, moreover, have shown similar risks in men and women.23,25,26
Strengths of this study include its sample size, the national representativeness of the study sample, the high quality study protocol and laboratory methods, and the consistency of the various sensitivity analyses that have been conducted. Importantly, the availability of serum cotinine, a specific biomarker of tobacco smoke exposure, reduces the possibility of exposure misclassification.63
Limitations of this cross-sectional study must also be considered, including the lack of prospective data. Although we adjusted for relevant potential confounders including age, gender, race/ethnicity, parental education, household income, systolic blood pressure percentile, BMI, birth weight, and lean body mass, there is always the possibility of residual confounding by unmeasured factors such as exposure to other nephrotoxicants, and differences in health care access and nutritional status. Finally, the equations used to estimate GFR have limitations. First, creatinine is an imperfect surrogate to estimate GFR, as it varies by muscle mass and dietary composition.64 Second, eGFR equations in children, including the bedside CKiD equation, were developed by using data from children with CKD, and therefore GFR may be underestimated when applied to children without CKD.41 In a previous study in the NHANES 1999–2002, the median (IQR) GFR estimated by the bedside CKiD equation among adolescents 12 to 17 years of age was 97 (84–109) mL/minute per 1.73 m2, and participants in the lower range of eGFR did not have an increased prevalence of comorbidities commonly associated with CKD.41 Given this finding and the low prevalence of CKD in the pediatric population, bias of pediatric estimating equations is possible, as it has been reported with GFR estimating equations in adults at higher levels of GFR.65–67 This source of bias, however, should be nondifferential and underestimate potential associations with tobacco smoke exposure. Third, it is unknown if the CKiD equation can be generalized to populations beyond the population for which it was derived. The CKiD equation, however, was estimated in a sample of 349 children across the United States and Canada including children who were 69% white, 15% black, and 16% of other race/ethnicities with the goal of developing a formula that could be applied to generate eGFR in clinical laboratories by using endogenous serum markers.43 The CKiD equation has been used in other populations beyond the original study, with findings supporting that it can be used in other populations.68,69
As the burden of kidney disease continues to increase worldwide, identification of modifiable CKD risk factors remains a priority.70 Our findings from the NHANES support that tobacco smoke may affect kidney function early in life, and prospective studies are needed to establish causality. Although the association was modest, and the implications at the individual level uncertain, small changes in the distribution of eGFR levels in the population could have a substantial impact in kidney related illness, as it is well known for small changes in blood pressure levels and hypertension related disease.71 Tobacco as a CKD risk factor is of great concern given the high prevalence of use and the chronicity that most often accompanies this exposure. Protecting young people from active smoking is essential because nearly 80% of adults who smoke began smoking by 18 years of age.1,54 Evaluating potential secondhand smoke exposure and providing recommendations to minimize exposure should continue to be incorporated as part of children’s routine medical care, which may be beneficial in the prevention of kidney disease in addition to the many other known health risks of tobacco smoke exposure.
Glossary
- ACR
albumin-to-creatinine ratio
- CI
confidence interval
- CKD
chronic kidney disease
- CKiD
chronic kidney disease in children
- eGFR
estimated glomerular filtration rate
- IQR
interquartile range
- LOD
limit of detection
- NHANES
National Health and Nutrition Examination Survey
Footnotes
Dr García-Esquinas conceptualized and designed the study, conducted statistical analyses, interpreted the data, drafted the initial article, and approved the final article as submitted. Dr Lauren Loeffler conceptualized and designed the study, conducted statistical analyses, interpreted the data, reviewed and revised the article, and approved the final article as submitted. Dr Virginia Weaver conceptualized and designed the study, interpreted the data, reviewed and revised the article, and approved the final article as submitted. Dr Jeffrey Fadrowski conceptualized and designed the study, interpreted the data, reviewed and revised the article, and approved the final article as submitted. Dr Ana Navas-Acien conceptualized and designed the study, provided statistical support, interpreted the data, drafted the initial article, reviewed and revised the article, and approved the final article as submitted.
FINANCIAL DISCLOSURE: The authors have indicated they have no financial relationships relevant to this article to disclose.
FUNDING: Dr Navas-Acien was supported by grants from the Flight Attendant Medical Research Institute, the Bloomberg Initiative to Reduce Tobacco Use, and from the US National Cancer Institute (R03CA153959). Dr García-Esquinas was supported by a Río Hortega Research Fellowship from the Instituto de Salud Carlos III, Spain (CM10/00332).
References
- 1.Surgeon General. Preventing Tobacco Use Among Youth and Young Adults. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention; 2012 [PubMed]
- 2.Surgeon General The Health Consequences of Involuntary Exposure to Tobacco Smoke. Atlanta, GA: Department of Health and Human Services, Centers for Disease Control and Prevention; 2006 [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention Tobacco use among middle and high school students–United States, 2000–2009. MMWR Morb Mortal Wkly Rep. 2010;59(33):1063–1068 [PubMed] [Google Scholar]
- 4.Max W, Sung HY, Shi Y. Who is exposed to secondhand smoke? Self-reported and serum cotinine measured exposure in the U.S., 1999-2006. Int J Environ Res Public Health. 2009;6(5):1633–1648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gilliland FD, Islam T, Berhane K, et al. Regular smoking and asthma incidence in adolescents. Am J Respir Crit Care Med. 2006;174(10):1094–1100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mak KK, Ho RC, Day JR. The associations of asthma symptoms with active and passive smoking in Hong Kong adolescents. Respir Care. 2012;57(9):1398–1404 [DOI] [PubMed] [Google Scholar]
- 7.Gold DR, Wang X, Wypij D, Speizer FE, Ware JH, Dockery DW. Effects of cigarette smoking on lung function in adolescent boys and girls. N Engl J Med. 1996;335(13):931–937 [DOI] [PubMed] [Google Scholar]
- 8.Wang X, Mensinga TT, Schouten JP, Rijcken B, Weiss ST. Determinants of maximally attained level of pulmonary function. Am J Respir Crit Care Med. 2004;169(8):941–949 [DOI] [PubMed] [Google Scholar]
- 9.Bono R, Nebiolo F, Bugiani M, et al. Effects of tobacco smoke exposure on lung growth in adolescents. J Expo Anal Environ Epidemiol. 1998;8(3):335–345 [PubMed] [Google Scholar]
- 10.Zieske AW, McMahan CA, McGill HC, Jr, et al. Smoking is associated with advanced coronary atherosclerosis in youth. Atherosclerosis. 2005;180(1):87–92 [DOI] [PubMed] [Google Scholar]
- 11.Kádár A, Mózes G, Illyés G, et al. World Health organization (WHO) and the World Heart Federation (WHF) pathobiological determinants of atherosclerosis in youth study (WHO/WHF PBDAY Study) 1986-1996. Histomorphometry and histochemistry of atherosclerotic lesions in coronary arteries and the aorta in a young population. Nutr Metab Cardiovasc Dis. 1999;9(5):220–227 [PubMed] [Google Scholar]
- 12.Loria CM, Liu K, Lewis CE, et al. Early adult risk factor levels and subsequent coronary artery calcification: the CARDIA Study. J Am Coll Cardiol. 2007;49(20):2013–2020 [DOI] [PubMed] [Google Scholar]
- 13.Berenson GS, Srinivasan SR, Bao W, Newman WP, III, Tracy RE, Wattigney WA. Association between multiple cardiovascular risk factors and atherosclerosis in children and young adults. The Bogalusa Heart Study. N Engl J Med. 1998;338(23):1650–1656 [DOI] [PubMed] [Google Scholar]
- 14.Hozawa A, Houston T, Steffes MW, et al. The association of cigarette smoking with self-reported disease before middle age: the Coronary Artery Risk Development in Young Adults (CARDIA) study. Prev Med. 2006;42(3):193–199 [DOI] [PubMed] [Google Scholar]
- 15.Iribarren C, Jacobs DR, Kiefe CI, et al. Causes and demographic, medical, lifestyle and psychosocial predictors of premature mortality: the CARDIA study. Soc Sci Med. 2005;60(3):471–482 [DOI] [PubMed] [Google Scholar]
- 16.Wang TN, Ko YC, Chao YY, Huang CC, Lin RS. Association between indoor and outdoor air pollution and adolescent asthma from 1995 to 1996 in Taiwan. Environ Res. 1999;81(3):239–247 [DOI] [PubMed] [Google Scholar]
- 17.Juonala M, Magnussen CG, Venn A, et al. Parental smoking in childhood and brachial artery flow-mediated dilatation in young adults: the Cardiovascular Risk in Young Finns study and the Childhood Determinants of Adult Health study. Arterioscler Thromb Vasc Biol. 2012;32(4):1024–1031 [DOI] [PubMed] [Google Scholar]
- 18.Kallio K, Jokinen E, Saarinen M, et al. Arterial intima-media thickness, endothelial function, and apolipoproteins in adolescents frequently exposed to tobacco smoke. Circ Cardiovasc Qual Outcomes. 2010;3(2):196–203 [DOI] [PubMed] [Google Scholar]
- 19.Yolton K, Dietrich K, Auinger P, Lanphear BP, Hornung R. Exposure to environmental tobacco smoke and cognitive abilities among U.S. children and adolescents. Environ Health Perspect. 2005;113(1):98–103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hogan SL, Vupputuri S, Guo X, et al. Association of cigarette smoking with albuminuria in the United States: the third National Health and Nutrition Examination Survey. Ren Fail. 2007;29(2):133–142 [DOI] [PubMed] [Google Scholar]
- 21.Briganti EM, Branley P, Chadban SJ, et al. Smoking is associated with renal impairment and proteinuria in the normal population: the AusDiab kidney study. Australian Diabetes, Obesity and Lifestyle Study. Am J Kidney Dis. 2002;40(4):704–712 [DOI] [PubMed] [Google Scholar]
- 22.Dülger H, Dönder A, Sekeroğlu MR, Erkoç R, Ozbay B. Investigation of the relationship between serum levels of cotinine and the renal function in active and passive smokers. Ren Fail. 2011;33(5):475–479 [DOI] [PubMed] [Google Scholar]
- 23.Haroun MK, Jaar BG, Hoffman SC, Comstock GW, Klag MJ, Coresh J. Risk factors for chronic kidney disease: a prospective study of 23,534 men and women in Washington County, Maryland. J Am Soc Nephrol. 2003;14(11):2934–2941 [DOI] [PubMed] [Google Scholar]
- 24.Klag MJ, Whelton PK, Randall BL, et al. Blood pressure and end-stage renal disease in men. N Engl J Med. 1996;334(1):13–18 [DOI] [PubMed] [Google Scholar]
- 25.Bleyer AJ, Shemanski LR, Burke GL, Hansen KJ, Appel RG. Tobacco, hypertension, and vascular disease: risk factors for renal functional decline in an older population. Kidney Int. 2000;57(5):2072–2079 [DOI] [PubMed] [Google Scholar]
- 26.Yamagata K, Ishida K, Sairenchi T, et al. Risk factors for chronic kidney disease in a community-based population: a 10-year follow-up study. Kidney Int. 2007;71(2):159–166 [DOI] [PubMed] [Google Scholar]
- 27.Nagasawa Y, Yamamoto R, Rakugi H, Isaka Y. Cigarette smoking and chronic kidney diseases. Hypertens Res. 2012;35(3):261–265 [DOI] [PubMed] [Google Scholar]
- 28.Fadrowski JJ, Navas-Acien A, Tellez-Plaza M, Guallar E, Weaver VM, Furth SL. Blood lead level and kidney function in US adolescents: The Third National Health and Nutrition Examination Survey. Arch Intern Med. 2010;170(1):75–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey. Available at: http://www.cdc.gov/nchs/nhanes/about_nhanes.htm. Accessed February 4, 2013
- 30.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) response rates and CPS totals. Available at: http://www.cdc.gov/nchs/nhanes/response_rates_CPS.htm. Accessed February 4, 2013
- 31.Benowitz NL. Cotinine as a biomarker of environmental tobacco smoke exposure. Epidemiol Rev. 1996;18(2):188–204 [DOI] [PubMed] [Google Scholar]
- 32.Caraballo RS, Giovino GA, Pechacek TF, Mowery PD. Factors associated with discrepancies between self-reports on cigarette smoking and measured serum cotinine levels among persons aged 17 years or older: Third National Health and Nutrition Examination Survey, 1988-1994. Am J Epidemiol. 2001;153(8):807–814 [DOI] [PubMed] [Google Scholar]
- 33.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84(7):1086–1093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Etzel RA. A review of the use of saliva cotinine as a marker of tobacco smoke exposure. Prev Med. 1990;19(2):190–197 [DOI] [PubMed] [Google Scholar]
- 35.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) laboratory procedure manual. Cotinine. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_99_00/lab06_met_cotinine.pdf. Accessed February 4, 2013
- 36.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) laboratory procedure manual. Cotinine. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_07_08/COT_E_met.pdf. Accessed February 4, 2013
- 37.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) laboratory procedure manual. Cotinine. http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/l06_c_met_cotinine.pdf. Accessed February 4, 2013
- 38.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) laboratory procedure manual. Creatinine. Available at: http://www.cdc.gov/NCHS/data/nhanes/nhanes_09_10/BIOPRO_F_met_creatinine.pdf. Accessed February 4, 2013
- 39.Centers for Disease Control and Prevention. National Health and Nutrition Examination Survey (NHANES) laboratory procedure manual. Creatinine. Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_03_04/l16_c_met_creatinine.pdf. Accessed February 4, 2013
- 40.Myers GL, Miller WG, Coresh J, et al. National Kidney Disease Education Program Laboratory Working Group . Recommendations for improving serum creatinine measurement: a report from the Laboratory Working Group of the National Kidney Disease Education Program. Clin Chem. 2006;52(1):5–18 [DOI] [PubMed] [Google Scholar]
- 41.Fadrowski JJ, Neu AM, Schwartz GJ, Furth SL. Pediatric GFR estimating equations applied to adolescents in the general population. Clin J Am Soc Nephrol. 2011;6(6):1427–1435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Schwartz GJ, Haycock GB, Edelmann CM, Jr, Spitzer A. A simple estimate of glomerular filtration rate in children derived from body length and plasma creatinine. Pediatrics. 1976;58(2):259–263 [PubMed] [Google Scholar]
- 43.Schwartz GJ, Muñoz A, Schneider MF, et al. New equations to estimate GFR in children with CKD. J Am Soc Nephrol. 2009;20(3):629–637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Centers for Disease Control and Prevention. Blood pressure section of the physician’s examination (BPX_B). Available at: http://www.cdc.gov/nchs/data/nhanes/nhanes_01_02/bpx_b_doc.pdf. Accessed May 20, 2010
- 45.National High Blood Pressure Education Program Working Group on High Blood Pressure in Children and Adolescents The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004;114(suppl 2, 4th Report):555–576 [PubMed] [Google Scholar]
- 46.Centers for Disease Control and Prevention. The 1999–2004 dual energy x-ray absorptiometry multiple imputation data files and technical documentation. Available at: http://www.cdc.gov/nchs/nhanes/dxx/dxa.htm. Accessed February 4, 2013
- 47.American Society of Pediatric Nephrology. The National Kidney Foundation - Kidney Disease Outcomes Quality Initiative (NKF K/DOQI) clinical practice guidelines. Available at: http://aspneph.com/clinicalaffairs/clinical%20practice%20guidelines%20updated%20nov07.pdf. Accessed February 4, 2013
- 48.Orth SR, Hallan SI. Smoking: a risk factor for progression of chronic kidney disease and for cardiovascular morbidity and mortality in renal patients—absence of evidence or evidence of absence? Clin J Am Soc Nephrol. 2008;3(1):226–236 [DOI] [PubMed] [Google Scholar]
- 49.Dasgupta P, Chellappan SP. Nicotine-mediated cell proliferation and angiogenesis: new twists to an old story. Cell Cycle. 2006;5(20):2324–2328 [DOI] [PubMed] [Google Scholar]
- 50.Jaimes EA, Tian RX, Joshi MS, Raij L. Nicotine augments glomerular injury in a rat model of acute nephritis. Am J Nephrol. 2009;29(4):319–326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Jaimes EA, Tian RX, Raij L. Nicotine: the link between cigarette smoking and the progression of renal injury? Am J Physiol Heart Circ Physiol. 2007;292(1):H76–H82 [DOI] [PubMed] [Google Scholar]
- 52.Baggio B, Budakovic A, Dalla Vestra M, Saller A, Bruseghin M, Fioretto P. Effects of cigarette smoking on glomerular structure and function in type 2 diabetic patients. J Am Soc Nephrol. 2002;13(11):2730–2736 [DOI] [PubMed] [Google Scholar]
- 53.Odoni G, Ogata H, Viedt C, Amann K, Ritz E, Orth SR. Cigarette smoke condensate aggravates renal injury in the renal ablation model. Kidney Int. 2002;61(6):2090–2098 [DOI] [PubMed] [Google Scholar]
- 54.Mur C, Clària J, Rodela S, et al. Cigarette smoke concentrate increases 8-epi-PGF2alpha and TGFbeta1 secretion in rat mesangial cells. Life Sci. 2004;75(5):611–621 [DOI] [PubMed] [Google Scholar]
- 55.Ozbek E. Induction of oxidative stress in kidney [published online ahead of print April 17, 2012]. Int J Nephrol. 10.1155/2012/465897 [DOI] [PMC free article] [PubMed]
- 56.Chalon S, Moreno H, Jr, Hoffman BB, Blaschke TF. Angiotensin-converting enzyme inhibition improves venous endothelial dysfunction in chronic smokers. Clin Pharmacol Ther. 1999;65(3):295–303 [DOI] [PubMed] [Google Scholar]
- 57.Orth SR. Smoking and the kidney. J Am Soc Nephrol. 2002;13(6):1663–1672 [DOI] [PubMed] [Google Scholar]
- 58.Hwangbo Y, Weaver VM, Tellez-Plaza M, Guallar E, Lee BK, Navas-Acien A. Blood cadmium and estimated glomerular filtration rate in Korean adults. Environ Health Perspect. 2011;119(12):1800–1805 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Navas-Acien A, Tellez-Plaza M, Guallar E, et al. Blood cadmium and lead and chronic kidney disease in US adults: a joint analysis. Am J Epidemiol. 2009;170(9):1156–1164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang X, Martinez-Donate AP, Kuo D, Jones NR, Palmersheim KA. Trends in home smoking bans in the U.S.A., 1995-2007: prevalence, discrepancies and disparities. Tob Control. 2012;21(3):330–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Tozawa M, Iseki K, Iseki C, Oshiro S, Ikemiya Y, Takishita S. Influence of smoking and obesity on the development of proteinuria. Kidney Int. 2002;62(3):956–962 [DOI] [PubMed] [Google Scholar]
- 62.Sabolić I, Asif AR, Budach WE, Wanke C, Bahn A, Burckhardt G. Gender differences in kidney function. Pflugers Arch. 2007;455(3):397–429 [DOI] [PubMed] [Google Scholar]
- 63.Florescu A, Ferrence R, Einarson T, Selby P, Soldin O, Koren G. Methods for quantification of exposure to cigarette smoking and environmental tobacco smoke: focus on developmental toxicology. Ther Drug Monit. 2009;31(1):14–30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Stevens LA, Coresh J, Greene T, Levey AS. Assessing kidney function—measured and estimated glomerular filtration rate. N Engl J Med. 2006;354(23):2473–2483 [DOI] [PubMed] [Google Scholar]
- 65.Poggio ED, Wang X, Greene T, Van Lente F, Hall PM. Performance of the modification of diet in renal disease and Cockcroft-Gault equations in the estimation of GFR in health and in chronic kidney disease. J Am Soc Nephrol. 2005;16(2):459–466 [DOI] [PubMed] [Google Scholar]
- 66.Rule AD, Larson TS, Bergstralh EJ, Slezak JM, Jacobsen SJ, Cosio FG. Using serum creatinine to estimate glomerular filtration rate: accuracy in good health and in chronic kidney disease. Ann Intern Med. 2004;141(12):929–937 [DOI] [PubMed] [Google Scholar]
- 67.Stevens LA, Coresh J, Feldman HI, et al. Evaluation of the modification of diet in renal disease study equation in a large diverse population. J Am Soc Nephrol. 2007;18(10):2749–2757 [DOI] [PubMed] [Google Scholar]
- 68.Dodson JL, Jerry-Fluker JV, Ng DK, et al. Urological disorders in chronic kidney disease in children cohort: clinical characteristics and estimation of glomerular filtration rate. J Urol. 2011;186(4):1460–1466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Lee CK, Swinford RD, Cerda RD, Portman RJ, Hwang W, Furth SL. Evaluation of serum creatinine concentration-based glomerular filtration rate equations in pediatric patients with chronic kidney disease. Pharmacotherapy. 2012;32(7):642–648 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Coresh J, Selvin E, Stevens LA, et al. Prevalence of chronic kidney disease in the United States. JAMA. 2007;298(17):2038–2047 [DOI] [PubMed] [Google Scholar]
- 71.Whelton PK, He J, Appel LJ, et al. National High Blood Pressure Education Program Coordinating Committee . Primary prevention of hypertension: clinical and public health advisory from The National High Blood Pressure Education Program. JAMA. 2002;288(15):1882–1888 [DOI] [PubMed] [Google Scholar]