Abstract
Background:
Prescription is the written order of the physician which is conveyed to the patient. Rational prescription writing is a skill which should be mastered at the earliest. Internship is the period where undergraduate medical education can be consolidated through continued learning under the direct supervision of teachers. The attitude of interns toward rational drug use is of utmost importance. The present study aimed to explore the prescribing pattern of interns in a primary health center in India.
Materials and Methods:
A cross-sectional study was conducted for a period of 2 months (June 1 2010-July 30 2010) in a primary health center attached to a medical college in India. The main outcome measure was to assess rationality of prescribing pattern of interns was measured as per World Health Organization enlisted prescribing indicators. Data analysis was done by using descriptive and inferential statistical methods: Frequencies, percentage, and mean standard deviation.
Results:
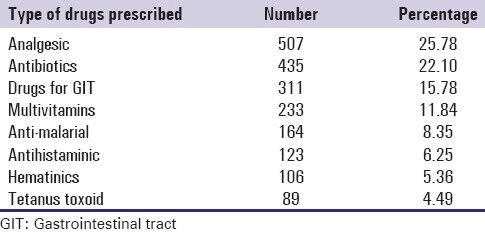
A total of 1968 drugs were prescribed in 760 prescriptions analyzed with an average of 2.58 drugs per prescription. Analgesic was the most commonly prescribed drug (25.78%) followed by antibiotics (22.1%), drugs used for gastrointestinal symptom (15.78%), multivitamins (11.84%), anti-malarials (8.35%), antihistaminics (6.25%), and hematinics (5.36%). Regarding prescribing indicators, in 435 prescriptions (22.4%), antibiotics were advised. A total of 688 (34.97%) drugs were prescribed by generic name, while the percentage of drugs prescribed from essential drug list of India was 58.47%. Injectables were prescribed in 89 prescriptions (4.49%).
Conclusion:
The present study shows that irrational prescribing practices are common among interns of the institute. The art of rational prescribing should be taught to them by medical teachers who are adequately trained in rational drug use.
Keywords: Intern, prescribing pattern, primary health center
Introduction
Prescription is the written order of the physician which is directly conveyed to the patient. It contains information pertaining to dose of the drug, route of administration, frequency of administration. Prescribing appropriate drugs in right doses is an integral part by which a physician can influence the patient's health and well-being. Drug plays an intrinsic role in maintaining and restoring health as well as to combat diseases. However, irrational use of drugs can lead to adverse drug reaction and negative socio-economic impact. To promote rational use of drugs, international agencies like the World Health organization (WHO) and the International Network for the rational use of drugs, have emphasized treatment of diseases by the use of essential drugs, prescribed by their generic names.[1]
Internship is the period where students after passing final MBBS examination undergo medical apprenticeship under the supervision of a consultant. He is expected to learn clinical skills, perform routine clinical procedures and exhibit a good clinical judgment to arrive at patient management decision. Rational prescription writing is a skill which should be mastered at the earliest. Most of the budding doctors are unaware of the fact that prescribing errors contribute significantly in escalating occurrence of adverse events. Internship is the period where undergraduate medical education can be consolidated through continued learning and acquisition of knowledge and skills under the direct supervision of teachers. Their attitude toward good prescribing, rational drug use is of utmost importance as they constitute the future generation of doctors. They should know how to prescribe safely and correctly and for this the knowledge and understanding, skill and attitude is required by medical graduates.
A literature search was conducted, which consisted of a Medical Literature Analysis and Retrieval System Online database search (accessed on 16.4.2010) and a World Wide Web search (search engine: Google, accessed on 16.4.2010) using the following keywords: Prescribing pattern and intern and study. The search revealed that very few studies have been conducted to assess the prescribing pattern of interns.[2,3]
Our study was conducted against this backdrop with the objective of exploring the prescribing pattern of interns in a medical college.
Materials and Methods
Study design
A cross-sectional study was conducted in the primary health center attached to the institute for a period of 2 months (June 1 2010-July 30 2010).
Ethical issues
Prior permission was obtained from institutional ethics committee for conducting the study.
Sample size calculation
In this study, the primary health center which has been visited by the interns of the institute was considered to be the primary sampling unit. As per WHO recommendations,[4] a study of a single health facility should measure facility specific prescribing indicators with a 95% confidence limit ± 10%. Accordingly, it has been recommended that at least 600 encounters should be included in a cross-sectional survey with a greater number if possible. In the present study, a total of 760 prescriptions have been analyzed.
Study procedure
Batches of 25 internees’ of the institute visited the center twice a week accompanied by a faculty member from the Department of Community Medicine and provided medical service to the villagers. A resident from Department of Pharmacology used to visit the health center during the study period for the purpose of data collection. Data collection was done by attaching a plain white paper along with a carbon paper with the original prescription form at ticket registration counter. The carbon copy of that prescription form was taken from the patient before he/she leaves the health center. Details of the prescription were entered into a previously prepared proforma. In the current piece of work, WHO suggested criteria[5] were used to assess the rationality of the prescriptions, which are enumerated below:
Therapeutic indication of the prescribed drug
Dose strength and dosage schedule
Duration of therapy
Fixed-dose combinations (FDCs) prescribed: Rational or not.
Any prescription which fails to comply with any of the above mentioned criteria were considered irrational. The rationality of first three criteria were judged as per Standard Treatment Guidelines, issued by Government of West Benga[6] and National Formulary of India.[7] For the fourth criteria, only those FDCs mentioned in the current version of WHO formulary (17th list, 2011)[8] and national essential drug list (EDL) of India (2011)[9] were considered rational. Analysis of prescriptions was done in Department of Pharmacology of the institute.
Statistical analysis
Data obtained were analyzed in computer by using Statistical Package for Social Sciences program version 10 (Chicago, IL, USA). Data analysis was done by using descriptive and inferential statistical methods: Frequencies, percentage, and mean standard deviation.
Results
During the study period, a total of 760 prescriptions were analyzed and the total number of drugs prescribed amounted to 1968. Average number of drugs per prescription was 2.58, while the number of drugs per prescription varied from 1 to 7 [detailed in Table 1]. The frequency of drug administration was mentioned in 726 (95.52%) of the prescriptions, while the duration of therapy was recorded in 586 (77.1%) of them. Analgesic was the most commonly prescribed drug (25.78%) followed by antibiotics, drugs used for gastrointestinal symptom (diarrhea/vomiting etc.) multivitamins, anti-malarial, antihistaminic, hematinics, etc., [Table 2]. Regarding prescribing indicators, in 435 prescriptions (22.4%), antibiotics were advised. A total of 688 (34.97%) drugs were prescribed by generic name while the percentage of drugs prescribed from EDL of India was 58.47%. Injectables were prescribed in 89 prescriptions (4.49%).
Table 1.
Number of drugs per prescription
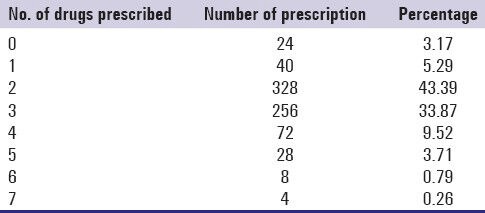
Table 2.
Commonly prescribed drugs in the health center
Discussion
The present study provides an insight to the performance of interns in several key dimensions related to rational use of drugs. In our study, the average number of drugs prescribed per patient varied from 0 to 7 with the average of 2.58. This parameter is used to measure the degree of polypharmacy. In this regard, the result obtained in the present study is similar to studies conducted in Manipal (2.76),[2] Delhi (2.47),[3] Madhya Pradesh (2.8)[10] and Pune (2.8).[11] The most common drugs prescribed in the current study was analgesics followed by antibiotics, drugs for the gastrointestinal tract, multivitamins while it was hematinics followed by analgesics in Manipal;[2] analgesics, antibiotics in Delhi,[3] Madhya Pradesh.[10] The variation in drugs most commonly used can be attributable to differential prevalence of diseases in varied geographical locations.
Generic prescribing is a potential measure for reducing the cost of drugs. Recently, regulatory authorities of different countries are emphasizing on generic prescribing to cut total healthcare cost. Similar endeavor has also been taken up by local state government. In this backdrop, the percentage of drugs prescribed by generic name in our study was very low, i.e. 34.97% which is comparable to study reported from Delhi (49.5%),[3] Madhya Pradesh (48.5%).[10] In a study conducted in Jordon, the percentage was also low (5.1%).[12] Inappropriate sensitization of the interns to generic prescribing and the frequent visit of the medical representatives at health facilities may be the probable cause of the under prescribing of the drugs by generic name. The percentage of prescription with antibiotics was 22.4% as compared to 60.9% in Madhya Pradesh[10] and 25% in Bangladesh[13] and Burkina Faso.[14] According to WHO, 15-25% prescription with antibiotics is expectable in most of the countries where infectious disease is more prevalent.[4] In a study conducted in India, Bapna et al. have reported 29.9% prescriptions containing one or more antibiotics.[15] The percentage of prescription with an injection was 4.49%. Studies conducted in other parts of India reported that the injection practices comparatively similar results, i.e. 5.2% by Bapna et al.[15]
The overall percentage of drugs prescribed from an EDL is a measure to examine the degree to which the practices confirm to national drug policy, as indicated by prescribing from national EDL was 58.94%. Ideally, it should be 100%. In Bangladesh[13] and Burkina Faso[14] it was 85% and 88%, respectively. The reasons for such wrong practices in our study were inadequate supply of drugs at health centers and unavailability of copy of EDL.
Internship is the period when the prescribing behavior of a doctor usually develops, which determines his/her approach to rational drug use in subsequent medical life. In this perspective, the prescribing pattern of interns, as observed in our study, calls for an urgent intervention to sensitize these young medical graduates with the principles of rational drug use. A further follow-up study is needed to compare the outcome of such intervention on the prescribing behavior of the interns of the institute. However, adequately powered multicentric studies with a similar objective can provide a more meaningful answer.
Limitations
The present study was conducted among medical interns catering patients of a single rural health center attached to a medical college and thus cannot be generalized.
Conclusion
The present study shows that irrational prescribing practices are common among interns of the institute. The art of rational prescribing should be taught to them by medical teachers who are adequately trained in rational drug use. The manuals of Standard Treatment Guideline and copy of EDL should be made available to every interns.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
References
- 1.WHO. The selection of essential drugs. World Health Organ Tech Rep Ser. 1977;615:36. [PubMed] [Google Scholar]
- 2.Pati RR. Prescribing pattern among medical interns at the rural health centres of a medical college, Manipal Karnataka. Indian J Community Med. 2004;29:128–9. [Google Scholar]
- 3.Rehan HS, Lal P. Drug prescribing pattern of interns at a government healthcare centre in northern India. Trop Doct. 2002;32:4–7. doi: 10.1177/004947550203200105. [DOI] [PubMed] [Google Scholar]
- 4.Vol. 1. Geneva: World Health Organization; 1993. How to Investigate Drug Use in Health Facilities: Selected Drug Use Indicators; pp. 1–87. WHO/DAP. [Google Scholar]
- 5.World Health Organisation; [Last accessed on 2012 Oct 6]. Promoting rational prescribing. Available from: http://www.apps.who.int/medicinedocs/documents/s19606en/s19606en.pdf . [Google Scholar]
- 6.2nd ed. Issued by Ministry of Health and Family Welfare, Government of West Bengal; 2011. Feb, [Last accessed on 2012 Oct 10]. Standard Treatment Guidelines for Primary Healthcare Facilities. Available from: http://www.ihfwkolkata.org/stg/stg-document2.html . [Google Scholar]
- 7.National Formulary of India. 2011. [Last accessed on 2012 Oct 6]. Available from: http://www.cdsco.nic.in/NFI_2011.pdf .
- 8.WHO Model list of Essential Medicines. 17th List. 2011. [Last accessed on 2012 Oct 6]. Available from: http://www.whqlibdoc.who.int/hq/2011/a95053_eng.pdf .
- 9.National list of essential medicines of India. 2011. [Last accessed on 2012 Oct 6]. Available from: http://www.cdsco.nic.in/National%20List%20of%20Essential%20Medicine-%20final%20copy.pdf .
- 10.Bhartiy SS, Shinde M, Nandeshwar S, Tiwari SC. Pattern of prescribing practices in the Madhya Pradesh, India. Kathmandu Univ Med J (KUMJ) 2008;6:55–9. [PubMed] [Google Scholar]
- 11.Kshirsagar MJ, Langade D, Patil S, Patki PS. Prescribing patterns among medical practitioners in Pune, India. Bull World Health Organ. 1998;76:271–5. [PMC free article] [PubMed] [Google Scholar]
- 12.Otoom S, Batieha A, Hadidi H, Hasan M, Al-Saudi K. Evaluation of drug use in Jordan using WHO patient care and health facility indicators. East Mediterr Health J. 2002;8:544–9. [PubMed] [Google Scholar]
- 13.Guyon AB, Barman A, Ahmed JU, Ahmed AU, Alam MS. A baseline survey on use of drugs at the primary health care level in Bangladesh. Bull World Health Organ. 1994;72:265–71. [PMC free article] [PubMed] [Google Scholar]
- 14.Krause G, Borchert M, Benzler J, Heinmüller R, Kaba I, Savadogo M, et al. Rationality of drug prescriptions in rural health centres in Burkina Faso. Health Policy Plan. 1999;14:291–8. doi: 10.1093/heapol/14.3.291. [DOI] [PubMed] [Google Scholar]
- 15.Bapna JS, Tekur U, Gitanjali B, Shashindran CH, Pradhan SC, Thulasimani M, et al. Drug utilization at primary health care level in southern India. Eur J Clin Pharmacol. 1992;43:413–5. doi: 10.1007/BF02220618. [DOI] [PubMed] [Google Scholar]


