Abstract
Background: Latinas have high breastfeeding initiation rates that decrease significantly in the first postpartum months. Little is known about the effects of self-efficacy and sociocultural factors on early breastfeeding among low-income Latinas. This study quantifies early breastfeeding rates and identifies factors associated with breastfeeding at 4–6 weeks postpartum in our community.
Subjects and Methods: Mothers were recruited from a newborn clinic (NBC) in the first postpartum week. Questionnaires in the NBC and 4–6 weeks later assessed feeding practices, breastfeeding self-efficacy, and sociocultural factors. Feeding practices in the well baby nursery (WBN) were obtained by chart review. A scale from “1” (exclusive formula feeding) to “5” (exclusive breastfeeding) characterized feeding practices. Paired-sample t tests assessed change in feeding practices, and regression analysis assessed the impact of factors on breastfeeding at 4–6 weeks.
Results: We interviewed 209 women: 86.1% Latina, 47.3% foreign-born, and 94.2% Medicaid-recipients. Breastfeeding increased from WBN to NBC (2.6±1.2 to 2.9±1.4; p<0.05) and then decreased by 4–6 weeks (2.9±1.4 to 2.5±1.44; p<0.05), without significant change between WBN and 4–6 weeks. Higher levels of education [β=0.21 (0.08, 0.56)], breastfeeding a previous child for ≥6 months [β=0.35 (0.57, 1.8)], foreign birth [β=0.2 (0.06, 1.07)], and higher breastfeeding self-efficacy scores [β=0.38 (0.02, 0.05)] were associated with more breastfeeding. Higher breastfeeding self-efficacy scores were associated with exclusive breastfeeding [adjusted odds ratio=1.18 (1.05, 1.32)].
Conclusions: Breastfeeding self-efficacy was the sole, modifiable factor associated with exclusive breastfeeding. Efforts to improve breastfeeding self-efficacy may serve to support breastfeeding in this population.
Introduction
Breastfeeding is the optimal first food for newborns in terms of health outcomes for both mother and child.1,2 However, breastfeeding rates continue to fall short of recommended targets in the United States. Healthy People 2020 goals include increasing the proportion of babies exclusively breastfed through 3 months of age to 46.2%, exclusively breastfed through 6 months of age to 25.5%, and any breastfeeding at 6 months to 60.6%.3 Data from the Centers for Disease Control and Prevention's Breastfeeding Report Card 2013 reveal that rates are below goals, with 3 months exclusive breastfeeding at 37.7%, 6 months exclusive breastfeeding at 16.4%, and 6 months of any breastfeeding at 49%.4 Low-income, minority mothers have the lowest breastfeeding rates in the United States. It is interesting that Latinas have among the highest levels of initiation of breastfeeding; however, rates decrease significantly in the first postpartum months.5,6 Because Latinos constitute the fastest growing and most populous minority group in the United States,7 the public health implications of suboptimal breastfeeding are significant.
Factors unique to Latinas, such as the los dos phenomenon, influence newborn feeding choices and ultimately may result in low long-term breastfeeding rates.8,9 Los dos refers to the routinized practice among Latinas of mixed feeding of both formula and breastmilk concurrently. Reasons for this practice include the belief that formula is part of a healthy newborn's diet, provides necessary vitamins lacking in breastmilk, and is a necessary supplement.8,10 Los dos, which often begins early in the postpartum period, may have a negative impact on milk supply and ultimately on long-term breastfeeding success.10 Although los dos is practiced by mothers of different Latino subgroups, there may be variations in the effects of other sociocultural factors on breastfeeding depending on the particular Latino subgroup.11,12 In light of this, more research is needed to understand the sociocultural factors associated with successful breastfeeding among Latinas in general and also among different subgroups in the early postpartum period.13
An association exists between high breastfeeding self-efficacy and longer durations of breastfeeding and higher levels of breastfeeding exclusivity,9,14 although little is known about the effect among low-income, inner-city Latinas in particular. Self-efficacy, based on Bandura's social cognitive theory, is an individual's perceived ability to perform a specific task or behavior.15 It is important that breastfeeding self-efficacy is a modifiable factor, and several studies have shown that interventions that increase breastfeeding self-efficacy have had positive results on breastfeeding.15,16 Because of this association, it is important to understand how breastfeeding self-efficacy impacts breastfeeding success among Latinas in order to create a culturally competent, successful intervention based on this concept.
The community in which this study was performed consists primarily of low-income, inner-city Latinas, the majority of whom are of Dominican descent, with high rates of mixed feeding. The purpose of this study was to quantify early changes in amounts of breastfeeding in this community and to explore the role of breastfeeding self-efficacy and sociocultural factors associated with any and exclusive breastfeeding in the first 4–6 weeks postpartum. The rationale for focusing on this early postpartum period is that this is a critical time for the establishment of successful breastfeeding, when a strong mother–baby dyad and a breastmilk supply based on baby demand are developed.17
Subjects and Methods
Population and study design
Our study took place at a newborn clinic (NBC) located at an academic medical center in Northern Manhattan, one of the most economically disadvantaged communities in New York City. The ethnic breakdown of this community of approximately 200,000 persons is more than 70% Latino (the majority from the Dominican Republic), 18% white, and 7% African American.18–20 One-third of the community meets federal poverty guidelines standards.18 The hospital is the primary birth center for the community, with approximately 3,500 annual births to women with Medicaid insurance.
Following discharge from the medical center's well baby nurseries (WBNs), approximately 30% of newborns with Medicaid go directly to a community provider for their first visit, whereas 70% of newborns are brought to the NBC within the first week of life. The patient population served by this clinic mirrors the ethnic breakdown of the community; the vast majority of patients are Latino, low income, and Medicaid recipients.
A convenience sample of mothers was recruited from the NBC waiting room. Mothers of full-term (>37 weeks of gestation) singletons were eligible for this study. After informed consent was obtained, the research assistant verbally administered a questionnaire in either English or Spanish, depending on the language preference of the participant. The questionnaire was translated into Spanish by a professional translator and then reviewed for accuracy and cultural-appropriateness by an independent, bilingual, nutritionist/lactation consultant who has worked with breastfeeding mothers in the local community for more than 20 years. The 30-minute-long questionnaire included both open and closed-ended/multiple choice questions about the pregnancy, delivery, and postpartum experiences, current infant feeding practices and beliefs, breastfeeding self-efficacy, and demographics. One month later, the research assistant contacted the mothers via phone to ask follow-up questions about their current feeding practices and rationale. A newborn medical chart review of the nursing flowsheets was completed in order to assess the total number of documented breast and/or formula feeds during the WBN stay.
In order to assess feeding choice rationale, participants were asked via open-ended questions why they chose the particular feeding type they were providing for their baby (exclusive breastfeeding, exclusive formula feeding, or mixed/breastfeeding and formula). Women who indicated they were exclusively formula feeding were asked, “What are some of the reasons you are not currently breastfeeding at this time?” Women who were mixed feeding were asked, “What made you decide to use both formula and breastmilk?” Women who were providing any amount of breastmilk (mixed feeding or exclusively breastfeeding) were asked, “Why do you breastfeed?” Women could provide more than one answer to each question.
Upon completion of the questionnaire in the NBC, participants were given a $2.50 subway voucher as a thank-you gift. This study was approved by the Institutional Review Board of Columbia University Medical Center.
Measures
Our primary outcome variable, feeding practice, was characterized using a 5-point scale from “1” (exclusive formula feeding) to “5” (exclusive breastfeeding) and as a dichotomous outcome (exclusive breastfeeding versus all other feeding types). We quantified feeding practices at three time points: WBN, NBC, and at phone follow-up.
Breastfeeding self-efficacy was measured using the validated Breastfeeding Self-Efficacy Scale-Short Form (BSES-SF), which has been shown to be reliable and valid in both the English and Spanish versions.15,21–23 This form consists of 14 statements related to breastfeeding, each phrased in a positive manner and beginning with “I can always…”: for example, “I can always determine that my baby is getting enough milk.” Mothers rate their level of agreement with each statement using a 5-point Likert scale, from 1 (not at all confident) to 5 (always confident).15 The possible scores of the BSES-SF range from 14 to 70, with higher values indicating higher breastfeeding self-efficacy.
Acculturation was measured using a six-statement Short Acculturation Scale (SAS), which was based on both a 12-statement Acculturation Scale for Hispanics24 and a four-question SAS.25 Scores on this six-statement scale range from 6 to 30. We dichotomized acculturation by defining a “high” level as a score of >15 and “low” as <15.
Statistical analysis
All data analysis was performed using the Statistical Package for Social Sciences software (SPSS version 20 for Windows; SPSS, Inc., Chicago, IL).
Changes in feeding practices
Using the 5-point feeding practices scale, descriptive statistics were used to calculate frequency of feeding practices at each time point. A paired t test was then used to evaluate for change in feeding practices from one time point to another: from WBN to NBC, from NBC to phone follow-up, and from WBN to phone follow-up.
Association of self-efficacy and sociocultural factors with breastfeeding
Bivariate analyses of various sociocultural factors, including receipt of hands-on help with breastfeeding, receipt of free formula, most influential people on feeding type choice, feeding preferences of family members/friends, and having previously seen family members/friends breastfeeding, were then performed. Of all the factors analyzed, seven factors with a significant relationship to higher levels of breastfeeding on binary analysis (p<0.05) were identified and were included in the multivariable model along with six sociodemographic variables (maternal age, educational level, intent to return to work/school within 6 months, ethnicity, insurance type, and Special Supplemental Nutrition Program for Women, Infants, and Children participation). Multivariable linear regression was used to assess the impact of breastfeeding self-efficacy scores and sociocultural factors with feeding practices at phone follow-up. Logistic regression was used to evaluate the association of these factors with exclusive breastfeeding.
Feeding choice rationale
Feeding rationale responses of each participant were reviewed, and descriptive statistics were performed. Responses that were mentioned by 10% or more participants were considered significant by the researchers and reported in this article.
Results
In total, 209 women participated in the study between March and September 2011. The mean age of respondents was 25.6±5.8 years, and the majority were Latina, foreign-born, and Medicaid recipients (Table 1). Of the 209 women initially interviewed in the NBC, 156 had a phone interview (75% retention) 4–6 weeks later. The mean age of was 2.4±0.6 days infants upon discharge from the WBN, 5±1.6 days at the NBC, and 40±10 days at phone follow-up. Two-thirds of participants were either born in the Dominican Republic (32%) or had one or both parents from the Dominican Republic (30%). The mean breastfeeding self-efficacy scale score for the study population as a whole was 50.3 (range, 14–70).
Table 1.
Study Population Characteristics (n=209)
| Demographic | Value |
|---|---|
| Mean (±SD) age of mother (years) | 25.6 (±5.8) |
| Ethnicity [% (n)] | |
| Latino | 86.1 (180) |
| African American | 8.6 (18) |
| White | 2.9 (6) |
| Other | 2.4 (5) |
| Education level [% (n)] | |
| Less than HS degree | 24.1 (51) |
| HS degree/GED | 47.7 (100) |
| 2-year college | 12.6 (26) |
| 4-year college | 13.6 (28) |
| Graduate school | 2 (4) |
| Mean (±SD) total number of children | 1.8 (±1.1) |
| Foreign-born [% (n)] | 47.3 (97) |
| Medicaid recipient/eligible [% (n)] | 94.2 (194) |
| Enrolling in WIC [% (n)] | 96.6 (200) |
| Vaginal delivery [% (n)] | 77.0 (161) |
HS, high school; SD, standard deviation; WIC; Special Supplemental Nutrition Program for Women, Infants, and Children.
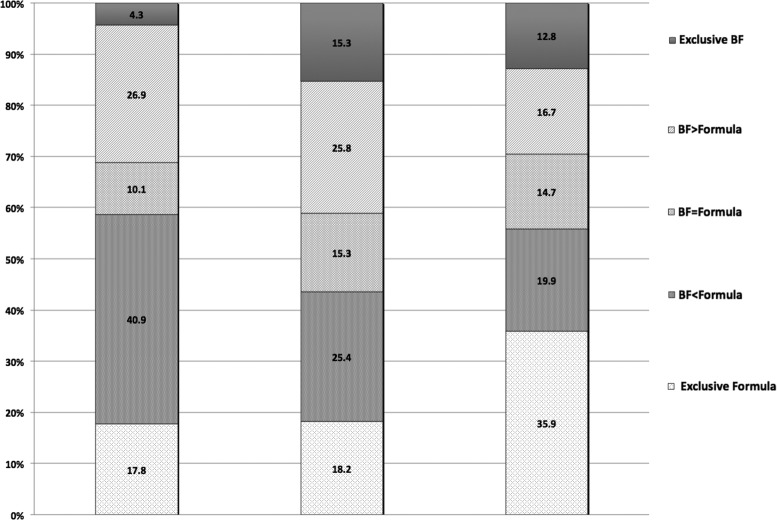
Amounts of breastfeeding and formula feeding varied at the three time points (Fig. 1). High rates of mixed feeding were identified at all three time points, including very early in the postpartum period: the majority of mothers were both breastfeeding and providing formula (77.9%, n=162) in the WBN. There was a significant increase in the mean score on the feeding practices scale from WBN to NBC (from 2.6±1.2 to 2.9±1.4; p<0.05) and a subsequent decrease in mean score from NBC to phone follow-up (from 2.9±1.4 to 2.5±1.44; p<0.05). Overall, there was no significant change in mean feeding practices score between the WBN and phone follow-up.
FIG. 1.
Feeding practices (%) in the first 4–6 weeks of life: (first column) well baby nursery (mean age, 2.4±0.6 days); (second column) newborn clinic (mean age, 5±1.6 days); and (third column) phone follow-up (mean age, 40±10 days). BF, breastfeeding.
Using linear regression, we found that women who were foreign-born, had higher levels of formal education, had breastfed a previous child for at least 6 months, and had higher breastfeeding self-efficacy scores had higher scores on the feeding practices scale, indicating higher amounts of breastfeeding at phone follow-up (Table 2). The only factor associated with exclusive breastfeeding was a higher breastfeeding self-efficacy score (Table 3).
Table 2.
Linear Regression Analysis of Feeding Practice (Feeding Practices Scale)
| Covariate | β | CI |
|---|---|---|
| Mother's age | 0.16 | −0.38, 0.46 |
| Ethnicity | −0.25 | −1.08, 0.82 |
| Education | 0.21 | 0.08, 0.56 |
| Mean total number of children | −0.16 | −0.44, 0.05 |
| Breastfeeding for ≥6 months with previous child | 0.35 | 0.57, 1.80 |
| Foreign-born | 0.20 | 0.06, 1.07 |
| Level of acculturation | −0.08 | −0.70, 0.27 |
| Self-efficacy | 0.38 | 0.02, 0.05 |
| Received free formula | −0.04 | −1.06, 0.64 |
| FOB prefers breastfeeding | 0.06 | −0.27, 0.67 |
| MGM prefers breastfeeding | 0.00 | −0.60, 0.58 |
| Medicaid recipient/eligible | 0.01 | −1.14, 1.24 |
| WIC recipient/eligible | 0.02 | −1.94, 2.54 |
Values for statistically significant covariates are given in bold type.
CI, confidence interval; FOB, father of baby; MGM, maternal grandmother; WIC; Special Supplemental Nutrition Program for Women, Infants, and Children.
Table 3.
Logistic Regression Analysis of Feeding Practice (Exclusive Breastfeeding Versus All Other Feeding Types)
| Covariate | AOR | CI |
|---|---|---|
| Mother's age | 0.76 | 0.16, 3.52 |
| Ethnicity | 0.40 | 0.36, 4.23 |
| Education | 2.50 | 0.59, 10.43 |
| Mean total number of children | 1.18 | 0.48, 2.86 |
| Breastfeeding for ≥6 months with previous child | 3.06 | 0.55, 17.22 |
| Foreign-born | 0.51 | 0.11, 2.39 |
| Level of acculturation | 0.47 | 0.10, 2.24 |
| Self-efficacy | 1.18 | 1.05, 1.32 |
Values for statistically significant covariates are given in bold type.
AOR, adjusted odds ratio; CI, confidence interval.
At the time of the NBC visit, mothers' feeding choice rationales differed among the various feeding types. The most common reasons cited by women providing only formula (n=38) included a perception of insufficient breastmilk supply (37%), and that their baby rejected the breast and preferred being bottle-fed (39%). Most common reasons cited by women who were mixed feeding by both breastfeeding and providing formula (n=139) included a perception of insufficient milk supply (55%), there were health benefits to using formula (13%), their baby had rejected the breast and preferred the bottle (12%), they had to return to work/school (11%), and they were embarrassed about breastfeeding (10%). The most common reasons cited by women who were breastfeeding about why they decided to breastfeed (either exclusively or mixed) (n=171) included health benefits for the child (100%), health benefits for the mother (22%), and because breastmilk is better than formula (21%).
At phone follow-up 4–6 weeks later, feeding rationale responses were similar to those provided at the time of the NBC visit, with some variation noted in the overall frequency of the responses. At phone follow-up among women giving only formula (n=56), again the most common reasons why mothers decided on this feeding type included a perception of insufficient milk supply (30%) and that their baby had rejected the breast (30%). The most common reasons cited by women who were mixed feeding at that time (n=80) again included a perception of insufficient milk supply (29%), that they were returning to work/school (16%), and that there were health benefits to using formula (10%). Other reasons cited at the time of the NBC visit (their baby had rejected the breast and preferred the bottle, or they were embarrassed about breastfeeding) were not commonly cited at the time of phone follow-up.
Similarly, the most common reasons cited by women who were breastfeeding about why they decided to breastfeed (either exclusively or mixed) (n=85) included health benefits for the child (87%) and because breastmilk is better than formula (21%). The other reason cited initially at the time of the NBC visit (health benefits for the mother) was not commonly mentioned at phone follow-up.
Discussion
Although mixed feeding was practiced by the majority of mothers, several factors were associated with increasing amounts of breastfeeding among the low-income, predominantly Latina mothers in this study. Mothers with higher levels of education, who had breastfed a previous child for at least 6 months, who were foreign-born, and who had higher breastfeeding self-efficacy scores were breastfeeding more at 4–6 weeks postpartum. It is notable that a higher level of breastfeeding self-efficacy was the only factor associated with exclusive breastfeeding. We found that breastfeeding amounts increased in the first week after hospital discharge and that the perception of insufficient milk supply was the top reason for giving formula in our study population.
Our findings from the multivariate analysis mirror other studies that have shown a positive association between the above-mentioned factors and increased amounts of breastfeeding.5,11,26,27 Other sociocultural factors noted in the literature to be associated with positive breastfeeding beliefs and improved breastfeeding rates (such as breastfeeding support by the mother's partner, older maternal age, lower levels of acculturation)9,28,29 and those negatively associated with breastfeeding (such as higher number of children and receipt of free formula from the hospital)12,30 were not significant on multivariable analysis in this present study. Our findings suggest that extra effort and breastfeeding support should focus on primaparous mothers, mothers who breastfed a previous child less than 6 months, and mothers who are not foreign-born.
Breastfeeding self-efficacy was the only modifiable factor associated with increased amounts of breastfeeding and with exclusive breastfeeding in particular at 4–6 weeks postpartum in our study population. This positive association has been previously described in the literature, albeit not necessarily among low-income, inner-city Latinas in particular. There are important implications to our finding in this study population. First, using the BSES-SF as a way to screen mothers in the first few days postpartum may identify women at greater need of support and targeted intervention.22 Second, interventions and programs that focus on increasing breastfeeding self-efficacy may support long-term breastfeeding success.16,31 For example, in a study by Kingston et al.,15 researchers investigated the influence of prenatal and postpartum experiences on self-efficacy on white, educated, married mothers and found that vicarious experience (seeing other mothers breastfeed) was most influential at 48 hours postpartum. Specifically, mothers who had observed breastfeeding audiovisual tapes during the prenatal or immediate postpartum period had significantly higher BSES-SF scores, along with higher rates of breastfeeding at 4 weeks postpartum, than those who had not seen the tapes. Lastly, targeted research is needed in order to elucidate which experiences most positively impact breastfeeding self-efficacy among Latinas in order to create culturally competent programs that promote breastfeeding self-efficacy.
Rates of exclusive breastfeeding, mixed feeding, and formula feeding measured at the three distinct time periods varied in the first 4–6 weeks. Our finding that breastfeeding increased in the first week may be related to study participants running out of the formula given to them at WBN discharge. Almost all mothers reported leaving the hospital with some free formula. It is possible that the NBC visit represented an early window in time after the hospital formula samples ran out and before the mothers purchased or received formula from elsewhere. Capitalizing on this window to promote breastfeeding self-efficacy would likely help improve breastfeeding outcomes. The initial, early outpatient visit in the first week of life is an optimal time to evaluate and troubleshoot for feeding problems, to support breastfeeding, and encourage mothers to continue to increase the frequency of breastfeeding while weaning from formula.28,32–34
Based on our descriptive analysis looking at mothers' reasons for feeding choice rationale, we found that a perception of milk insufficiency was the most commonly cited reason to provide formula in the first week of life. This may be another target of intervention in our study group. This perception is reported as the most common problem that women experience with breastfeeding, often resulting in early cessation of breastfeeding.10,35–37 Thus, education and reassurance, particularly in the first week of life as mothers' milk comes in, may dispel the perception of insufficient supply and be crucial for supporting breastfeeding. Practices such as weighing babies before and after breastfeeding in order to document a rise in weight may prove very helpful as tangible evidence of milk production and sufficiency.12
Although it is encouraging that many mothers in this study recognized the important health benefits associated with breastfeeding, a troubling dichotomy was found to exist: indeed, 100% of mothers who were giving breastmilk to their babies cited its health benefits as a reason for doing so, yet 13% of these women believed that formula offered health benefits as well. This dichotomy has been noted previously among Latina women in other studies.35,38 Healthcare providers need to inform mothers that formula is not a substitute for breastmilk but rather a substandard alternative. Physicians have an influential role in breastfeeding initiation and continuation39 and should promote breastfeeding as an optimal feeding source, starting prenatally and extending throughout the nursery stay and beyond.40
Our study fills a gap in the literature, particularly when looking at the association between breastfeeding self-efficacy and exclusive breastfeeding among Latinas, but it is important to note that our sample might not be representative of other populations or of other Latina subgroups. Another possible limitation to our study relates to how we collected data on feeding type. WBN feeding type was obtained from a medical chart review, where the total number and type of feeds were documented. Feeding type at the NBC and the 4–6-week phone follow-up were obtained by the mother's self-report. It is possible that mothers inflated their reported breastfeeding frequency when asked face-to-face at the time of the NBC questionnaire. Thus, the increase noted in breastfeeding amounts between WBN and NBC may not have represented an increase in breastfeeding as large and significant as we calculated.
Conclusions
This study builds on previous research showing a positive association between various sociocultural factors and breastfeeding, specifically higher levels of education, previously having breastfed another child for more than 6 months, maternal foreign birth, and higher levels of breastfeeding self-efficacy. The results of this study highlight the importance and impact of these factors on early breastfeeding in this community and provide information critical to the design of breastfeeding promotion programs among inner-city, low-income Latinas. The finding that higher levels of breastfeeding self-efficacy were associated with increasing amounts of breastfeeding and with breastfeeding exclusivity in our population is notable. As the only modifiable factor identified in this study, it supports the use of interventions to improve breastfeeding self-efficacy as a means to increase breastfeeding duration and exclusivity in this population. More targeted research will help inform what experiences and sociocultural factors are most closely linked with high levels of self-efficacy in order to create maximally effective, culturally competent interventions and breastfeeding support programs that target inner-city, low-income Latina mothers.
Acknowledgments
We would like to thank the research assistants who worked with us on this project: Adriene Giese, Jane Lim, Jacqueline Rodriguez, Emily Vroegindewey, and Regina Yang. We also thank New York Presbyterian Hospital and its Ambulatory Care Network. This study was supported by Primary Care Faculty Development grant D55HP05154 from the Health Resources and Services Administration.
Disclosure Statement
No competing financial interests exist.
References
- 1.American Academy of Pediatrics, Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics 2012;129:e827–e841 [DOI] [PubMed] [Google Scholar]
- 2.Scariati PD, Grummer-Strawn LM, Fein SB. A longitudinal analysis of infant morbidity and the extent of breastfeeding in the United States. Pediatrics 1997;99:E5. [DOI] [PubMed] [Google Scholar]
- 3.U.S. Department of Health and Human Services. Healthy People 2020, Maternal, Infant, and Child Health (MICH) Objective 21. www.healthypeople.gov/2020/topicsobjectives2020/objectiveslist.aspx?topicId=26 (accessed January17, 2014)
- 4.Centers for Disease Control and Prevention's (CDC) Division of Nutrition, Physical Activity, and Obesity, National Center for Chronic Disease Prevention and Health Promotion. Breastfeeding Report Card. United States/2013. July2013. www.cdc.gov/breastfeeding/pdf/2013BreastfeedingReportCard.pdf (accessed January17, 2014)
- 5.Jones JR, Kogan MD, Singh GK, et al. Factors associated with exclusive breastfeeding in the United States. Pediatrics 2011;128:1117–1125 [DOI] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Progress in increasing breastfeeding and reducing racial/ethnic differences—United States, 2000–2008 births. MMWR Morb Mortal Wkly Rep 2013;62(5):77–80 [PMC free article] [PubMed] [Google Scholar]
- 7.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. May2011. www.census.gov/prod/cen2010/briefs/c2010br-04.pdf (accessed January17, 2014)
- 8.Bunik M, Clark L, Zimmer LM, et al. Early infant feeding decisions in low-income Latinas. Breastfeed Med 2006;1:225–235 [DOI] [PubMed] [Google Scholar]
- 9.Schlickau JM, Wilson ME. Breastfeeding as health-promoting behaviour for Hispanic women: Literature review. J Adv Nurs 2005;52:200–210 [DOI] [PubMed] [Google Scholar]
- 10.Bartick M, Reyes C. Las dos cosas: An analysis of attitudes of Latina women on non-exclusive breastfeeding. Breastfeed Med 2012;7:19–24 [DOI] [PubMed] [Google Scholar]
- 11.Chapman DJ, Perez-Escamilla R. US national breastfeeding monitoring and surveillance: Current status and recommendations. J Hum Lact 2009;25:139–150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gill SL. Breastfeeding by Hispanic women. J Obstet Gynecol Neonatal Nurs 2009;38:244–252 [DOI] [PubMed] [Google Scholar]
- 13.Bartick M, Reinhold A. The burden of suboptimal breastfeeding in the United States: A pediatric cost analysis. Pediatrics 2010;125:e1048–e1056 [DOI] [PubMed] [Google Scholar]
- 14.Semenic S, Loiselle C, Gottlieb L. Predictors of the duration of exclusive breastfeeding among first-time mothers. Res Nurs Health 2008;31:428–441 [DOI] [PubMed] [Google Scholar]
- 15.Kingston D, Dennis CL, Sword W. Exploring breast-feeding self-efficacy. J Perinat Neonatal Nurs 2007;21:207–215 [DOI] [PubMed] [Google Scholar]
- 16.Noel-Weiss J, Rupp A, Cragg B, et al. Randomized controlled trial to determine effects of prenatal breastfeeding workshop on maternal breastfeeding self-efficacy and breastfeeding duration. J Obstet Gynecol Neonatal Nurs 2006;35:616–624 [DOI] [PubMed] [Google Scholar]
- 17.American Academy of Pediatrics, Section on Breastfeeding. Sample Hospital Breastfeeding Policy for Newborns. http://www2.aap.org/breastfeeding/curriculum/documents/pdf/Hospital%20Breastfeeding%20Policy_FINAL.pdf (accessed January17, 2014)
- 18.Olson E, Van Wye G, Kerker B, Thorpe L, et al.. Take Care Inwood and Washington Heights. NYC Community Health Profiles, 2nd ed. New York: New York City Department of Health and Mental Hygiene, 2006;(19):1–16 [Google Scholar]
- 19.The City of New York. Manhattan Community District 12 Profile. www.nyc.gov/html/dcp/pdf/lucds/mn12profile.pdf#profile (accessed January17, 2014)
- 20.Bergad LW. Washington Heights/Inwood Demographic, Economic, and Social Transformations 1990–2005 with a Special Focus on the Dominican Population. December2008. http://clacls.gc.cuny.edu/files/2013/10/Washington-Heights-Inwood-Demographic-Economic-and-Social-Transformations-1990_2005-with-a-Special-Focus-on-the-Dominican-Population.pdf (accessed January17, 2014)
- 21.Molina Torres M, Davila Torres RR, Parrilla Rodriguez AM, et al. Translation and validation of the breastfeeding self-efficacy scale into Spanish: Data from a Puerto Rican population. J Hum Lact 2003;19:35–42 [DOI] [PubMed] [Google Scholar]
- 22.Dennis CL. The Breastfeeding Self-Efficacy Scale: Psychometric assessment of the short form. J Obstet Gynecol Neonatal Nurs 2003;32:734–744 [DOI] [PubMed] [Google Scholar]
- 23.Oliver-Roig A, d'Anglade-Gonzalez ML, Garcia-Garcia B, et al. The Spanish version of the Breastfeeding Self-Efficacy Scale-Short Form: Reliability and validity assessment. Int J Nurs Stud 2012;49:169–173 [DOI] [PubMed] [Google Scholar]
- 24.Marin G, Sabogal F, VanOss Marin B, et al. Development of a short acculturation scale for Hispanics. Hispanic J Behav Sci 1987;9:183–205 [Google Scholar]
- 25.Gibson MV, Diaz VA, Mainous AG 3rd, et al. Prevalence of breastfeeding and acculturation in Hispanics: Results from NHANES 1999–2000 study. Birth 2005;32:93–98 [DOI] [PubMed] [Google Scholar]
- 26.Grummer-Strawn LM, Shealy KR. Progress in protecting, promoting, and supporting breastfeeding: 1984–2009. Breastfeed Med 2009;4(Suppl 1):S31–S39 [DOI] [PubMed] [Google Scholar]
- 27.Hurley KM, Black MM, Papas MA, et al. Variation in breastfeeding behaviours, perceptions, and experiences by race/ethnicity among a low-income statewide sample of Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) participants in the United States. Matern Child Nutr 2008;4:95–105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Faraz A. Clinical recommendations for promoting breastfeeding among Hispanic women. J Am Acad Nurse Pract 2010;22:292–299 [DOI] [PubMed] [Google Scholar]
- 29.Pachon H, Olson C. Retrospective analysis of exclusive breastfeeding practices among four Hispanic subgroups in New York's EFNEP. J Nutr Educ 1999;31:39–46 [Google Scholar]
- 30.Sutherland T, Pierce CB, Blomquist JL, et al. Breastfeeding practices among first-time mothers and across multiple pregnancies. Matern Child Health J 2012;16:1665–1671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Nichols J, Schutte NS, Brown RF, et al. The impact of a self-efficacy intervention on short-term breast-feeding outcomes. Health Educ Behav 2009;36:250–258 [DOI] [PubMed] [Google Scholar]
- 32.American Academy of Pediatrics, Committee on Fetus and Newborn. Hospital stay for healthy term newborns. Pediatrics 2010;125:405–40920100744 [Google Scholar]
- 33.American Academy of Pediatrics, Committee on Fetus and Newborn. Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics 2004;114:297–316 [DOI] [PubMed] [Google Scholar]
- 34.Brenner MG, Buescher ES. Breastfeeding: A clinical imperative. J Womens Health (Larchmt) 2011;20:1767–1773 [DOI] [PubMed] [Google Scholar]
- 35.Gatti L. Maternal perceptions of insufficient milk supply in breastfeeding. J Nurs Scholarsh 2008;40:355–363 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schwartz K, D'Arcy HJ, Gillespie B, et al. Factors associated with weaning in the first 3 months postpartum. J Fam Pract 2002;51:439–444 [PubMed] [Google Scholar]
- 37.Wagner EA, Chantry CJ, Dewey KG, et al. Breastfeeding concerns at 3 and 7 days postpartum and feeding status at 2 months. Pediatrics 2013;132:e865–e875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Rios E. Promoting breastfeeding in the Hispanic community. Breastfeed Med 2009;4(Suppl 1):S69–S70 [DOI] [PubMed] [Google Scholar]
- 39.Taveras EM, Capra AM, Braveman PA, et al. Clinician support and psychosocial risk factors associated with breastfeeding discontinuation. Pediatrics 2003;112:108–115 [DOI] [PubMed] [Google Scholar]
- 40.Wolynn T. Breastfeeding—So easy even a doctor can support it. Breastfeed Med 2011;6:345–347 [DOI] [PMC free article] [PubMed] [Google Scholar]