Abstract
Objective. To investigate whether interventions that have positive effects on psychological symptoms and quality of life compared with usual care would also reduce days on sick leave. Design. A randomized controlled trial. Setting. A large primary health care centre in Stockholm, Sweden. Intervention. Patients with common mental disorders were recruited by their GPs and randomized into one of two group interventions that took place in addition to usual care. These group interventions were: (a) group cognitive behavioural therapy (CBT), and (b) group multimodal intervention (MMI). Both types of intervention had previously shown significant effects on quality of life, and MMI had also shown significant effects on psychological symptoms. Patients. Of the 245 randomized patients, 164 were employed and had taken sick leave periods of at least two weeks in length during the study period of two years. They comprised the study group. Main outcome measures. The odds, compared with usual care, for being sick-listed at different times relative to the date of randomization. Results. The mean number of days on sick leave increased steadily in the two years before randomization and decreased in the two years afterwards, showing the same pattern for all three groups .The CBT and MMI interventions did not show the expected lower odds for sick-listing compared with usual care during the two-year follow-up. Conclusion. Reduction in psychological symptoms and increased well-being did not seem to be enough to reduce sickness absence for patients with common mental problems in primary care. The possibility of adding workplace-oriented interventions is discussed.
Key Words: General practice, group psychotherapy, primary health care, psychological symptoms, psychosocial interventions, randomized controlled trial, sick leave, Sweden
Psychological symptoms may be reduced by psychosocial interventions but the effects on sick leave are still unclear.
In this randomized controlled trial, was no reduction found in sick leave with group therapy compared with usual care.
A topic for further studies is whether psychosocial interventions in combination with workplace-oriented interventions have better effects on work ability and sick leave than either intervention alone.
Introduction
Patients with common mental problems such as depression, anxiety, and stress are common in primary care and, together with those with musculo-skeletal problems, they represent the largest groups in terms of sickness absence in Sweden [1]. There are several studies of cognitive behavioural therapy (CBT) in primary care which show that good results can be achieved in the treatment of anxiety disorders and depression, as are reviewed in a number of meta-analyses [2–4]. Almost all of these studies investigated treatments designed for specific disorders. Attempts have also been made to develop transdiagnostic CBT (i.e. the same treatment protocol is used regardless of the diagnosis) [5]. In a separate report from the present trial [6] we showed that it is possible to design group therapy for common mental disorders in primary care, and that this therapy is promising as a basic treatment for mild to moderate symptoms. Two transdiagnostic group treatments, CBT and a multimodal intervention (MMI), were compared with usual care for patients with anxiety, depressive, and stress-related disorders in a randomized controlled trial. The primary outcome measure was the mental component summary score (MCS) of the Short Form 36 health survey questionnaire (SF-36) [7]. Both treatments were significantly better than usual care, and MMI was more effective than CBT. On the secondary outcome measures (symptoms of anxiety, depression, and stress), only MMI showed significantly larger improvements than usual care. The effects persisted during a one-year follow-up.
With regard to sick leave, previous research on the effects of psychosocial interventions gives a mixed impression. Whereas a small number of studies have demonstrated positive effects on reducing sick leave [8–10], several studies have reported no or small effects [11,12], or even a negative effect [13]. Because of the effects we have found on symptoms and quality of life by group therapy with a transdiagnostic approach, we expected to find a decrease in sick leave by these interventions. The purpose of the present study was thus to investigate whether CBT or MMI, compared with usual care, can reduce sick-leave days for patients with common mental problems in primary care. Since there is conflicting evidence as to whether psychosocial interventions focusing on symptoms also have an effect on work ability, this study should add valuable knowledge to this issue.
Material and methods
Design and main outcome
The study was a randomized controlled trial with three conditions including usual care and two different group treatments, CBT and MMI. The main outcome in the present study was the odds of being sick-listed, compared with usual care, at different times relative to randomization.
Patients
Patients aged 18–-65 years with symptoms of depression, anxiety, somatoform disorders, or stress, attending a large primary health care centre in Stockholm, Sweden, with approximately 30 000 enlisted individuals were recruited by the GPs. Patients fulfilling diagnostic criteria for bipolar or psychotic disorders, severe personality disorders, or at high risk of suicidal behaviours were excluded.
The working situation and sick-listing status of patients were not criteria in the recruitment process of participants to this study.
Data collection
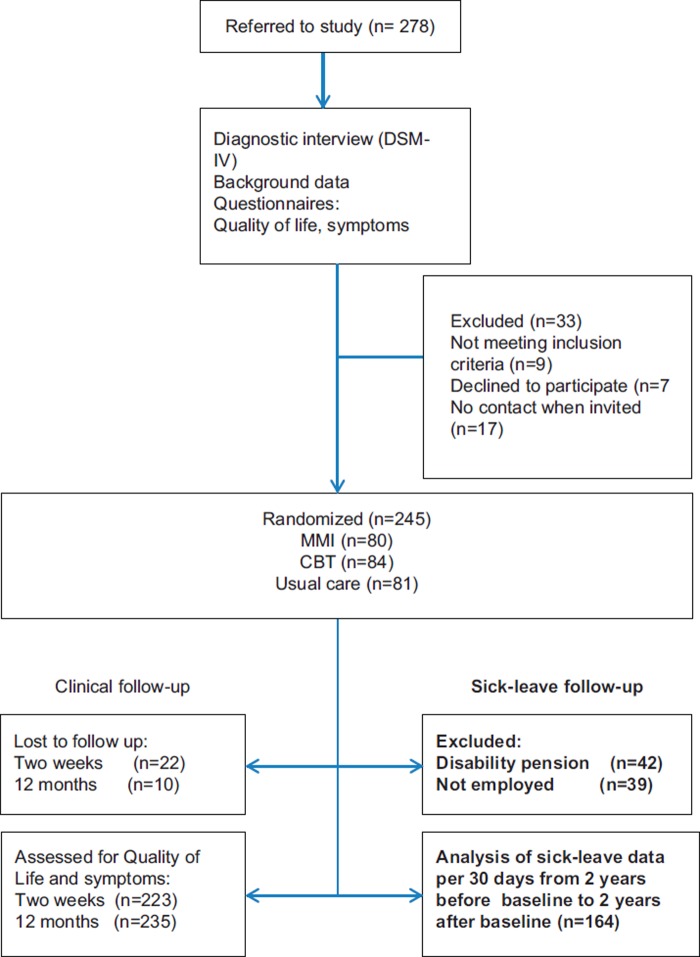
The 278 patients who were referred to the study underwent a structured clinical interview in order to obtain DSM-IV diagnoses; background data and measures on quality of life and psychological symptoms were collected. Sick-listing data were obtained from the Social Insurance Agency (SIA). If the length of the sick leave was shorter than two weeks no information was available from the SIA, and these sick leave periods are thus not included. Sick leave was measured as the number of whole days (part-time sick leave was transformed to whole days by multiplying number of days by degree of sick leave) during a period of 30 days. For each month, from 24 months before randomization to 24 months after, the number of sick-leave days was calculated as the sum during the preceding 30 days, disregarding the type of benefit. The benefits included, besides sickness benefit, qualifying days of sickness/waiting period, sick pay from employer, rehabilitation allowance, preventive sickness benefit, and occupational injury benefit. Individuals who received permanent or temporary disability pension at any time during the study period, before or after the randomization, were excluded as it was unlikely that this situation would be influenced by the interventions. Figure 1 shows the selection of patients for the present study. Of the 278 referred patients, 33 were excluded or declined to participate. Of the remaining 245 patients, 42 received disability pension and were excluded. Another 39 were excluded from the analyses since their SIA sick days did not include sick pay from the employer (they were unemployed and/or running their own business). The remaining 164 patients comprised the study group, with sick leave periods of at least two weeks in length. Forty-six patients had no sick days registered at the SIA during the four-year period.
Figure 1.
Flow-chart of how patients were recruited. MMI refers to multimodal intervention, CBT to cognitive behavioural therapy. Entries with bold text indicate data for the present study.
Interventions
The participants were randomized between January 2006 and July 2007 into one of three groups: (i) CBT (ii) MMI, and (iii) usual care. The randomization was computer-generated. For the allocation to one of the three groups an e-mail with a code number was sent to a statistician not involved in conducting the study.
Group CBT was based on generally accepted cognitive and behavioural treatment principles from the domain of anxiety and mood disorders with a transdiagnostic approach, i.e. using the same treatment protocol regardless of the diagnosis [5]. There was one 120-minute group session per week for 12 weeks, led by one of two psychologists. The sessions included conceptualizations of the problems and the role of thoughts and behaviours; rationales for exposure interventions and behavioural activation; exposure to feared stimuli and emotional awareness training; and finally acquiring new skills in order to prevent relapse.
MMI was a group intervention following a protocol created by one of the authors (RS) consisting of a mix of existing group interventions and exercises utilized in a variety of therapeutic schools. The group intervention comprised 150-minute group sessions twice a week for six weeks, led by one of three assistant nurses. The main components of the first week's sessions were a unified goal-setting among the group members, and psycho-education about thoughts, emotions, and behaviours that are common in persons with depressive and anxiety symptoms. During the second week the participants were introduced to an exercise in which one participant shared a personal problem with the group and obtained feedback. The focus was also on the importance of physical training, and participants were taught to do a few yoga exercises. The focus of the third and fourth weeks was on understanding the difference between emotions and thoughts, and strategies on how to deal with conflicts. During the fifth week the participants were asked to invite important people in their lives to attend two sessions to work on team building. During the sixth week, strategies for handling difficult thoughts and emotions in highly stressful situations were presented. Following group therapy, each participant also had two additional individual sessions with the assistant nurse to discuss individual goals that would be set prior to group therapy. The assistant nurses had no formal psychotherapeutic education and their training prior to this study was to take part in an MMI group treatment as a member and subsequently as an observer. All three received weekly supervision from the originator of MMI or a group therapist.
Participants in the usual care group were not offered group therapy. Their GPs prescribed medication and sick-listing when necessary and could refer to psychosocial counselling in primary health care and more rarely to a psychiatric clinic.
None of the interventions had a specific focus on work ability.
Statistical methods
A mixed model to analyse the effect of treatment and time was not considered useful as the residuals were not normally distributed, the number of days of sick leave per month usually being 0 or 30 days. Our primary outcome measure was therefore defined as odds (odds ratios, OR) for being sick-listed or not in a comparison between groups at different points in time, adjusted for whether one was sick-listed before the start of the trial. In this analysis, an individual was considered as being sick-listed during a certain time period if he or she had at least one day of payment administered by the SIA. For the purpose of visualizing the time trends in sick days we showed graphically the mean number of total days registered as sick leave by SIA for the three study groups.
An independent statistical company (Statisticon AB) performed the analyses on behalf of the authors.
Results
Most participants were women of average to high educational level (Table I). Mood disorders were most prevalent among DSM-IV diagnoses for all three groups. For all three groups the majority of patients had 0 sick leave days the month before randomization, whereas > 20 days was the second most common sick leave pattern.
Table I.
Baseline data for the three study groups.1
| MMI (n = 45) | CBT (n = 58) | Usual care (n = 61) | |
| Mean age (SD), years | 43.1 (8.4) | 42.4 (9.9) | 44.5 (9.2) |
| Women, n (%) | 38 (84) | 43 (74) | 51 (84) |
| Education, highest (%): | |||
| Elementary school | 9 (20) | 10 (17) | 14 (23) |
| Secondary school | 17 (38) | 25 (43) | 25 (41) |
| Higher | 19 (42) | 23 (40) | 22 (36) |
| Baseline sick leave days (%) (transformed to whole days, during 30 days before the study): | |||
| 0 | 21 (47) | 35 (60) | 37 (61) |
| 1–4 | 0 (0) | 0 (0) | 1 (2) |
| 5–20 | 9 (20) | 9 (16) | 9 (15) |
| > 20 | 15 (33) | 14 (24) | 14 (23) |
| DSM-IV diagnoses (%): | |||
| Mood disorders | 24 (53.3) | 35 (60.3) | 29 (48.3) |
| Anxiety disorders | 16 (35.6) | 22 (37.9) | 20 (33.3) |
| Somatoform disorders | 5 (11.1) | 2 (3.4) | 3 (5) |
| None of the above (not fulfilling criteria for any DSM-IV diagnosis) | 10 (22.2) | 11 (19) | 20 (33.3) |
Note: 1Disorders add up to more than 100% as more than one diagnosis could be present for a single patient.
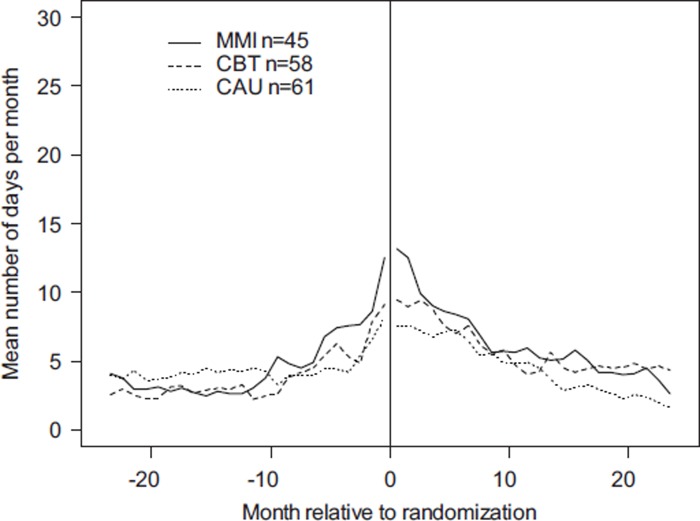
For all three groups, sick-leave days increased up to the date of randomization, and decreased, in a uniform way, up to two years after the beginning of the trial. There was no clear pattern as to the relationship between groups at different points in time (Figure 2).
Figure 2.
Mean number of sick-leave days at different points in time, relative to randomization for the three groups. CAU refers to “care as usual”.
We did not find lower odds for sick-listing with active treatment compared with usual care (Table II) and CBT compared with usual care had a significantly elevated OR for sick listing at 24 months.
Table II.
Odds ratios (95% CI) for being sick-listed as comparisons between groups at different times, relative to randomization.1
| Comparison | 6 months | p-value | 12 months | p-value | 24 months | p-value |
| MMI vs. usual care | 1.17 (0.41:3.33) | 0.77 | 1.04 (0.38:2.76) | 0.94 | 1.71 (0.49:6.39) | 0.40 |
| CBT vs. usual care | 1.91 (0.70:5.44) | 0.22 | 0.84 (0.32:2.22) | 0.73 | 3.59 (1.19:12.43) | 0.03 |
Note: 1Adjustments were made for the number of days on sick leave in the month before randomization.
Discussion
The hypothesis that symptom reduction following psychosocial interventions would be accompanied by a decrease in sickness absence, compared with care as usual, was not confirmed. We found a uniform pattern with an increase in the number of sick days before the date of randomization, followed by a decrease during the follow-up period for all groups. The odds for being sick-listed at different times after randomization showed no group effect with the exception of higher odds for CBT compared with usual care at 24 months. This latter finding should be interpreted with caution as it was restricted to one of three measurement points with a low significance level in a context of multiple comparisons.
The results seem to indicate that a reduction in psychological symptoms and an increased quality of life among patients with common psychological problems is not enough to reduce the risk of being sick-listed. An alternative or complementary strategy is the use of interventions targeting the working situation and/or workplace. There is some evidence that a combination of the two approaches may be beneficial [14,15]. However, empirical evidence concerning the effects of workplace interventions on work ability or sickness absence seems to be rather scarce. A meta-analysis from 2009 covering randomized controlled trials on the effects of workplace interventions concluded that, due to a lack of good studies, the issue is unclear regarding mental health problems [16]. A recent literature review [17] focused on mental health problems and included different outcomes related to return to work. There was some evidence that workplace-based interventions had the potential to affect work absence duration and other outcome measures such as work functioning. The included studies used different ways to combine psychotherapeutic treatment with work-related actions and it is unclear how different components should ideally be combined, and which procedures are best suited for different types of mental problems. We are currently testing a combined model in primary care, designed for patients on sick leave for mental problems. One to three workplace visits by a psychologist are combined with CBT treatment in a clinical setting. Also, MMI in combination with work-related intervention has been used with good preliminary results.
The strengths of the study are the randomized design and the availability of registry data on sick leave for all participants. An important limitation is that the study was not designed primarily for addressing the sick-listing issue, and we can therefore not evaluate its statistical power in this respect; being sick-listed was not an inclusion criterion, which probably reduced the study's ability to demonstrate effects of psychosocial interventions on sick leave. It could also have been useful to include measures other than days on sick-leave, e.g. self-reported work ability, as in the Work Ability Index [18]. Other limitations are the small number of therapists (two and three respectively), which restricts the generalizability to other settings, and differences between CBT and MMI in terms of, for example, total therapy time.
To summarize, group psychosocial interventions designed for patients with common mental problems within primary care showed no more reduction in sick-leave days than was achieved with usual care.
Acknowledgments
Ethics
Ethical approval was obtained from the Regional Ethics Committee of Stockholm (Dnr 2005/447-3; 2009/833-32).
Funding
The trial was funded by the Stockholm County Council.
Declaration of interest
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Ruslan Savitskij has, since the trial, started a private company that provides treatment based on the MMI used here, under the name Inner Leadership Development (ILD).
Trial registration number
The RCT was indexed at http://www.clinicaltrials.gov (ID number NCT01565213).
References
- 1.Social Insurance Agency, SSI. figures 2012. Available online at http://www.forsakringskassan.se. (accessed June 2013)
- 2.Cape J, Whittington C, Buszewicz M, Wallace P, Underwood L. Brief psychological therapies for anxiety and depression in primary care: Meta-analysis and meta-regression. BMC Med. 2010;June:8 doi: 10.1186/1741-7015-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bortolotti B, Menchetti M, Bellini F, Montaguti MB, Berardi D. Psychological interventions for major depression in primary care: A meta-analytic review of randomized controlled trials. Gen Hosp Psychiatry. 2008;30:293–302. doi: 10.1016/j.genhosppsych.2008.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Seekles W, Cuijpers P, Kok R, Beekman A, van Marwijk H, van Straten A. Psychological treatment of anxiety in primary care: A meta-analysis. Psychol Med. 2013;43:351–61. doi: 10.1017/S0033291712000670. [DOI] [PubMed] [Google Scholar]
- 5.Barlow DH. Psychological treatments. American Psychologist. 2004;59:869–78. doi: 10.1037/0003-066X.59.9.869. [DOI] [PubMed] [Google Scholar]
- 6.Ejeby K, Savitskij R, Öst L-G, Ekbom A, Brandt L, Ramnerö J, et al. Transdiagnostic group treatments for patients with common mental disorders in primary health care: A randomized controlled trial comparing cognitive behavioural therapy, multimodal intervention, and care as usual. Fam Pract. 2014 doi: 10.1093/fampra/cmu006. 10.1093/fampra/cmu006doi (accepted) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.SF-36 Health Survey. Manual and interpretation guide. Lincoln, RI: QualityMetric; 1993. [Google Scholar]
- 8.Mintz J, Mintz LI, Arruda MJ, Hwang SS. Treatments of depression and the functional capacity to work. Arch Gen Psychiatry. 1992;49:761–8. doi: 10.1001/archpsyc.1992.01820100005001. [DOI] [PubMed] [Google Scholar]
- 9.Linden M, Zubragel D, Bar T. Occupational functioning, sickness absence and medication utilization before and after cognitive-behaviour therapy for generalized anxiety disorders. Clin Psychol Psychother. 2011;18:218–24. doi: 10.1002/cpp.712. [DOI] [PubMed] [Google Scholar]
- 10.Lexis MAS, Jansen NWH, Huibers MJH, van Amelsvoort L, Berkouwer A, Ton GTA, et al. Prevention of long-term sickness absence and major depression in high-risk employees: A randomised controlled trial. Occup Environ Med. 2011;68:400–7. doi: 10.1136/oem.2010.057877. [DOI] [PubMed] [Google Scholar]
- 11.Knekt P, Lindfors O, Laaksonen MA, Raitasalo R, Haaramo P, Jarikoski A, et al. Effectiveness of short-term and long-term psychotherapy on work ability and functional capacity: A randomized clinical trial on depressive and anxiety disorders. J Affect Disord. 2008;107:95–106. doi: 10.1016/j.jad.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 12.De Vente W, Kamphuis JH, Emmelkamp PM, Blonk RW. Individual and group cognitive-behavioral treatment for work-related stress complaints and sickness absence: A randomized controlled trial. J Occup Health Psychol. 2008;13:214–31. doi: 10.1037/1076-8998.13.3.214. [DOI] [PubMed] [Google Scholar]
- 13.Carlsson L, Englund L, Hallqvist J, Wallman T. Early multidisciplinary assessment was associated with longer periods of sick leave: A randomized controlled trial in a primary health care centre. Scand J Prim Health Care. 2013;31:141–6. doi: 10.3109/02813432.2013.811943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Blonk RWB, Brenninkmeijer V, Lagerveld SE, Houtman ILD. Return to work: A comparison of two cognitive behavioural interventions in cases of work-related psychological complaints among the self-employed. Work and Stress. 2006;20:129–44. [Google Scholar]
- 15.Lagerveld SE, Blonk RW, Brenninkmeijer V, Wijngaards-de Meij L, Schaufeli WB. Work-focused treatment of common mental disorders and return to work: A comparative outcome study. J Occup Health Psychol. 2012;17:220–34. doi: 10.1037/a0027049. [DOI] [PubMed] [Google Scholar]
- 16.Van Oostrom SH, Driessen MT, de Vet HCW, Franche R-L, Schonstein E, Losiel P, et al. Workplace interventions for preventing work disability. Cochrane Database of Systematic Reviews. 2009 doi: 10.1002/14651858.CD006955.pub2. (2) [DOI] [PubMed] [Google Scholar]
- 17.Pomaki G, Frache RL, Murray E, Khushrushahi N, Lampinen TM. Workplace-based work disability prevention interventions for workers with common mental health conditions: A review of the literature. J Occup Rehabil. 2012;22:182–95. doi: 10.1007/s10926-011-9338-9. [DOI] [PubMed] [Google Scholar]
- 18.Aamland A, Malterud K, Werner EL. Phenomena associated with sick leave among primary care patients with medically unexplained physical symptoms: S systematic review. Scand J Prim Health Care. 2012;30:147–55. doi: 10.3109/02813432.2012.704812. [DOI] [PMC free article] [PubMed] [Google Scholar]