Abstract
Second and third degree burns on breasts at preadolescent period may cause severe breast deformations. This deformation can be variable depending on severity and location of the burns, personal adolescent patterns, and treatment modality in acute burn period. A 21 year old female patient admitted to our department for her breast deformation due to burn contracture at the inferior pole of the right breast. On physical examination we defined that development of the volume of the right breast was equal to the left, and inferior pole of the right breast was flattened due to contracture, and nipple was projected to inferior. We found that inframammary crease of the right breast was 2 cm lower than that of left; andthe distance of nipple-inframamary crease was 4.7 cm while areola-inframmary crease was 2 cm. New nipple-areola complex level was identified according to left breast's level. Medial and lateral lines were planned to merge inferiorly at 2 cm above inframmary crease in a plan similar to vertical mammaplasty. Superior pedicle carrying nipple areola was desepitelised. Lower parenchymal V flap was transposed superiorly and attached to the pectoral muscle. Inferior parts of the lateral and medial glandular flaps were excised to form new inframammary crease. The desired laxity of skin at the lower pole was obtained by performing a new Z- plasty between lateral and medial skin flaps. Breast symmetry was confirmed by postoperative objective measurements between left and right breasts. Patient's satisfaction and aesthetic appearance levels were high. Breasts deformation patterns caused by burns, trauma and mass exsicion due to cancer could not be addressed with traditional defined techniques. Special deformations can be corrected by custom made plannings as we presented here.
KEY WORDS: Burn, burn contracture, post-burn breast deformity
INTRODUCTION
Second- and third-degree burns of the anterior chest wall in preadolescent females can result in scar contracture and subsequently cause severe breast deformations.[1] This deformation can be variable depending on the severity and location of the burns, personal adolescents’ patterns and treatment modality in the acute burn period. Despite these possible effects of the burn on breast shape and location, the breast bud is very rarely damaged by the skin burn. In other words, distortion of the breast and areola and nipple complex does not indicate the underlying gland maldevelopment and future possible lactation problem.[2] However, subtotal damage of the breast bud can result in hypoplasia or distortion of the breast and total damage to the breast bud can result in a complete lack of the breast development. If the breast bud is spared, but the surrounding skin is burned and contracted, breast development can be extrinsically inhibited.[3]
Several procedures have been described in the literature to treat a burn-deformed breast and sub-sequent aesthetic and emotional problems. These techniques are scar excision, contracture release and skin graft, skin flaps, latissimus dorsi mycocutaneous flap with or without an implant and tissue expanders.[2,4,5,6 To avoid further destruction, it is suggested that the repair procedure should be delayed until the reasonable breast development is achieved.[1,2] Otherwise, a deformed breast with a smoothed-out mound and splayed, hypoplastic and flattened breast parenchyma can develop.[1] However, MacLennan et al. stated that “no set age for breast release can be recommended” and the authors performed breast release on “as young as 10 years old.” Hence, they suggested that “surgery is indicated when there is bulging of breast tissue in unburned areas or when the scarred skin is obviously restricting breast growth”.[3] As Grishkevich stated: “The most adequate and effective method for severe breast contractures should be able to restore all three components of the deformity: shape, location of the breast and nipple-areolar complex and breast skin damage”.[1] Thus, according to the well-known principle that “there is no disease but patients”, some solutions may be unique to a specific case. In addition, post-burn breast deformity often has a deleterious effect on the psychological and functional well-being of the patient. These burn-deformities become a source of lifelong shame, guilt, and regret for the patients. They experience serious image problems that disrupt their social lives, even if they have stabilised emotionally.5,6,7 We report our experience in such a specific case in which custom-made planning is required to correct her post-burn breast deformity.
CASE REPORT
The present case report is about a 21-year-old female patient who had a scald burn injury at 1.5 years old was admitted to our department for her breast deformation due to burn contracture at the inferior pole of the right breast [Figure 1a and b]. According to the patient's history, burn wounds were treated with conventional burn dressing. On physical examination, we defined that development of the volume of the right breast was equal to the left, the inferior pole of the right breast was flattened due to contracture, and the nipple was projected to the inferior pole. We found that the inframammary sulcus of the right breast was 2 cm lower than that of the left; the distance of the nipple to inframammary sulcus was 4.7 cm, whereas the areola to inframammary sulcus was 2 cm [Figure 2a and b]. In addition, there was minimal wideness at the base of the right breast due to contracture. The size of the left breast was nearly ideal: The sternal notch-nipple distance was measured at 18 cm and the nipple-inframammary sulcus distance was 7 cm. In addition, the base of the right breast was minimally expanded due to contractures of the lower pole of the breast. In the measurement of the left breast, the sternal notch-nipple distance was 18 cm and the nipple-inframammary sulcus distance was 7 cm — the accepted ideal breast size measurements.
Figure 1.
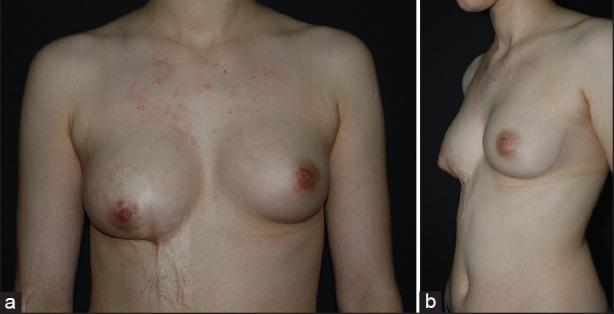
The pre-operative appearance of the patient. (a) Frontal view, (b) lateral view
Figure 2.
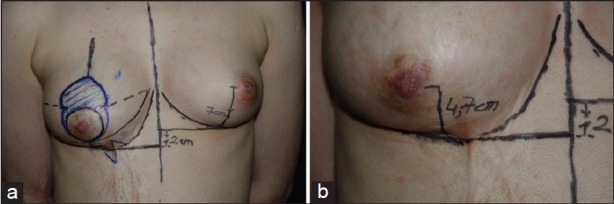
Pre-operative planning. (a) The new position of the nipple-areolar complex is marked, (b) close-up view of the distance between the nipple-areolar complex and inframammarian fold
Pre-operative planning
We had three aims when we were planning the surgery:
Moving the nipple-areola complex to the same level as the other breast,
Moving the inframammary sulcus to 2 cm above, and
Releasing the lower pole contracture of the breast.
We could achieve the first two of these aims with a superior pedicle technique of reduction mammoplasty with minimal tissue excision. In addition, Z-plasty was planned to release the contracture. A new nipple-areola complex level was identified according to the left breast's level. Medial and lateral lines were planned to merge inferiorly at 2 cm above the inframammary sulcus [Figure 2a and b]. According to this technique, the diameter of the medial and lateral vertical will determine the length of the nipple to inframammary sulcus [Figure 3].
Figure 3.
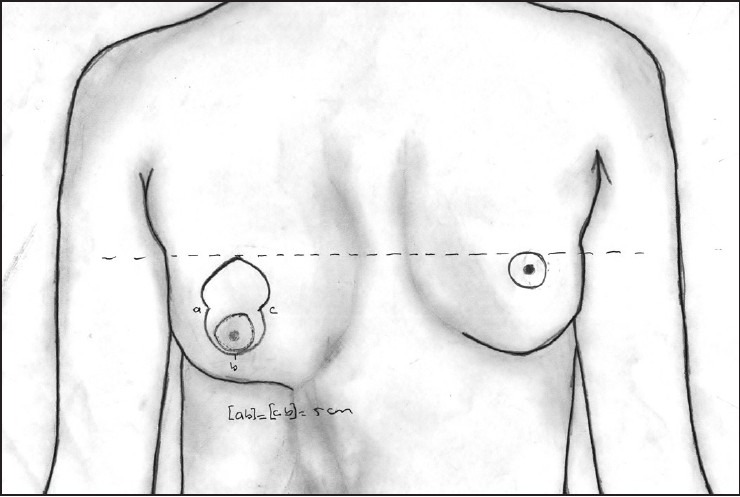
The schematic drawing of pre-operative planning
This technique is also a bit narrow in the breast base. Z-plasty was planned to relieve the contracture of the lower pole as the third objective.
Operation technique
A superior pedicle carrying the nipple-areola was de-epithelialised. A lower parenchymal V flap was transposed superiorly and attached to the pectoral muscle. Inferior parts of the lateral and medial glandular flaps were minimally excised to form a new inframammary sulcus. The desired laxity of skin at the lower pole was obtained by performing a new Z-plasty between the lateral and medial flaps.
RESULT
Breast symmetry was confirmed by post-operative objective measurements between the left and right breasts. The patient's satisfaction and aesthetic appearance levels were high [Figure 4a and b].
Figure 4.
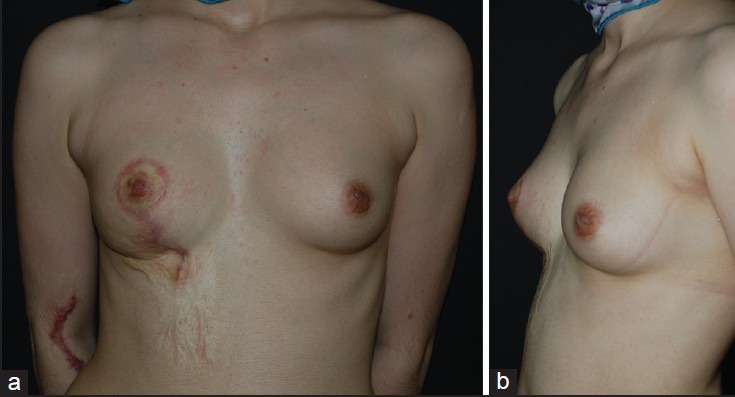
Post-operative appearance of the patient 12 months after surgery. (a) Frontal view, (b) lateral view
DISCUSSION
A study by Ozgur et al. classified the post-burn breast deformities as either mild or severe. According to this classification, if the breast development was normal but the position of the areola was affected by the traction of the contracted scar, post-burn breast deformity is classified as mild deformity. In this group of patients in their series, their treatment choice was reconstruction with skin grafts or contracted scar release with Z-plasty or local skin flaps.[8] Deformity of our presented case can be considered a mild deformity. However, we did not choose the skin grafting technique as the reconstruction method of this case, and the desired laxity of skin at the lower pole was obtained by performing a new Z-plasty between the lateral and medial flaps.
Although breast development is normal, the areola may replace secondary due to burn contractures. There are two main points for reconstruction of these secondary deformities:
Moving the nipple-areola complex to the natural level, and
releasing the burn contracture of the breast.
A superior, inferior, medial or lateral pedicle technique of reduction mammoplasty has to be performed according to changes in the direction of the areola. The second issue is the release of the contracture, which can be done using conventional methods such as skin grafts and local flaps. However, if there is an inhibition for the growth of breast parenchymal tissue, the tissue expanders, prostheses, and local or free flaps can be used for reconstruction.
Although general rules of scar revision can be applied in common cases of breast deformities, some breast deformation patterns caused by burns, trauma and mass excision could not be addressed with traditionally defined techniques. Special deformations of the breast, especially those having occurred in the post-burn period, require various surgical techniques in relation to these deformations.
El-Otiefy and Darwish reported their experience in 74 post-burn breast deformities.[2] 32 out of the 74 patients present downward contracture and 16 out of the 74 patients present loss or distortion of the nipple and areola. Patients presented with downward contracture that was reconstructed with transposition flaps from the abdomen to elevate the pulled-down breast. They reported that “a sliding skin flap from the abdomen (superiorly, laterally or medially based) to the inframammary sulcus allows the tissue to be brought upward onto the chest wall according to patients’ need”.[2] In addition, contracture release and skin grafts were used for this purpose. However, they also stated that a “skin graft in the upper half of the breast offers a better prognosis than a graft in the lower half and the inframammary groove, which nearly always develops re-contraction”.[2]
Grishkevich reported his experience with 13 post-burn breasts with an author-suggested, improved free-skin grafting technique.[1] In their author-suggested technique, “all scars were excised about the entire parenchymal surface and an incision was made down to the chest wall fascia. The symmetrical form and positioning were achieved by circularly led sutures, using mattress sutures, which are passed through the fat layer of different levels of the breast. The suture ends are passed through the skin out and beyond the wound area and affixed in a place opposite to the breast displacement”.[1] In addition, the nipple-areolar complex positioning is also normalised with the above-mentioned technique of the author. He used a split-thickness skin graft for wound coverage.[1]
In the presented case, new inframammarian sulci were formed by excision of the inferior parts of the lateral and medial glandular flaps. Inframammary fold re-creation can also be achieved by a U-shaped incision with skin grafting, pedicled flap or transposition flap.[1,9,10,11,12] However, as Grishkevich stated: “the inframammary fold re-creation only partially corrects the shape and positioning of the breast”.[1]
Scar excision with a thick split-thickness skin graft is considered to be the most effective reconstruction method for severe cases of post-burn breast deformity.[1,13,14] However, according to some authors, the breast is flattened in severe contractures and scar excision and skin grafting will not significantly improve the shape and location of the breast. Thus, the breast remains flat and some post-operative measures are to be needed, such as post-operative splint and compression garments.[1,15] However, in the presented case, and in Grishkevich's series, there was no need for these kinds of measures. To solve this problem, Grishkevich proposed the above-mentioned technique, which is “scar excision, parenchyma mobilization, restoration of shape and positioning using the circular-forming sutures and skin grafting”.[1] Grishkevich proposed that the nipple-areolar transposition reconstruction could be made in the second stage if needed. In addition, MacLennan et al. also suggested that “reconstruction of the nipple-areola is delayed until reconstruction of the breast mound is complete and scars are settled and supple. This is generally 9-12 months after breast mound re-construction”.[3] However, in the presented case we transposed the nipple-areola complex in the same stage.
MacLennan et al. reported that after reconstruction with a skin graft, a “burned breast does not stretch with age like an unburned breast and is less likely to become ptotic.” However, in their six patients, burned breasts went on to develop macromastia.[3] In the presented case with our custom-made technique, it is difficult to estimate whether the reconstructed breast will develop macromastia, ptosis or other acquired breast deformities. A large clinical series with long-term follow-up is needed in order to recommend our proposed technique for similar cases.
CONCLUSION
There is not a standard solution for reconstruction of the breast burn-deformity. For this reason, the most important point of reconstruction is the creativity and ability to produce a solution according to the patient's deformity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Grishkevich VM. Restoration of the shape, location and skin of the severe burn-damaged breast. Burns. 2009;35:1026–35. doi: 10.1016/j.burns.2008.12.008. [DOI] [PubMed] [Google Scholar]
- 2.El-Otiefy MA, Darwish AM. Post-burn breast deformity: Various corrective techniques. Ann Burns Fire Disasters. 2011;24:42–5. [PMC free article] [PubMed] [Google Scholar]
- 3.MacLennan SE, Wells MD, Neale HW. Reconstruction of the burned breast. Clin Plast Surg. 2000;27:113–9. [PubMed] [Google Scholar]
- 4.Wainwright DJ. Burn reconstruction: The problems, the techniques, and the applications. Clin Plast Surg. 2009;36:687–700. doi: 10.1016/j.cps.2009.05.009. [DOI] [PubMed] [Google Scholar]
- 5.Durmus M. How to approach a patient who refuses the recommended mammoplasty technique. Arch Clin Exp Surg. 2013;2:69–70. [Google Scholar]
- 6.Sever C, Uygur F, Kulahci Y, Oksuz S, Sahin C, Yuksel F. Treatment of facial burn scars with CO2 laser resurfacing and thin skin grafting. J Craniofac Surg. 2010;21:1024–8. doi: 10.1097/SCS.0b013e3181e47d70. [DOI] [PubMed] [Google Scholar]
- 7.Kulahci Y, Sever C, Noyan N, Uygur F, Ates A, Evinc R, et al. Burn assault with paint thinner ignition: An unexpected burn injury caused by street children addicted to paint thinner. J Burn Care Res. 2011;32:399–404. doi: 10.1097/BCR.0b013e318217f87a. [DOI] [PubMed] [Google Scholar]
- 8.Ozgur F, Gokalan I, Mavili E, Erk Y, Kecik A. Reconstruction of postburn breast deformities. Burns. 1992;18:504–9. doi: 10.1016/0305-4179(92)90186-x. [DOI] [PubMed] [Google Scholar]
- 9.McCauley RL. Reconstruction of the trunk and genitalia. In: Herndon D, editor. Total Burn Care. Philadelphia: W.B. Saunders; 2002. pp. 707–10. [Google Scholar]
- 10.McCauley RL, Killion GW, Boven K. Reconstruction of the burned breast and nipple — areolar complex. In: McCauley RL, editor. Functional and Aesthetic Reconstruction of Burned Patients. Boca Raton: Taylor and Francis; 2005. pp. 379–91. [Google Scholar]
- 11.Haik J, Grabov-Nardini G, Goldan O, Tessone A, Regev E, Mendes D, et al. Expanded reverse abdominoplasty for reconstruction of burns in the epigastric region and the inframammary fold in female patients. J Burn Care Res. 2007;28:849–53. doi: 10.1097/BCR.0b013e3181599b69. [DOI] [PubMed] [Google Scholar]
- 12.Neale HW, Smith GL, Gregory RO, MacMillan BG. Breast reconstruction in the burned adolescent female (an 11-year, 157 patient experience) Plast Reconstr Surg. 1982;70:718–24. doi: 10.1097/00006534-198212000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Kunert P, Schneider W, Flory J. Principles and procedures in female breast reconstruction in the young child's burn injury. Aesthetic Plast Surg. 1988;12:101–6. doi: 10.1007/BF01576922. [DOI] [PubMed] [Google Scholar]
- 14.Palao R, Gómez P, Huguet P. Burned breast reconstructive surgery with Integra dermal regeneration template. Br J Plast Surg. 2003;56:252–9. doi: 10.1016/s0007-1226(03)00101-2. [DOI] [PubMed] [Google Scholar]
- 15.Slator RC, Wilson GR, Sharpe DT. Postburn breast reconstruction: Tissue expansion prior to contracture release. Plast Reconstr Surg. 1992;90:668–71. [PubMed] [Google Scholar]


