Abstract
Background:
Autogenous costal cartilage is a good option for large volume requirements in rhinoplasty, when septal or conchal cartilages do not suffice. Reluctance to use costal cartilage is due to apprehension of warping. However, warping can be avoided if we follow the principle of balanced section as advocated by Gibson and Davis. “Warping” can also be utilized to change the curvature of the graft.
Materials and Methods:
We have used 69 costal cartilage grafts as a solid piece for contour fill in rhinoplasty in 31 patients over the last 10 years. Principle of balanced section as advocated by Gibson and Davis was adhered to while carving the grafts, however some grafts were allowed to warp to get different sizes and shapes.
Results:
All the procedures were uneventful. Aesthetic appearance of all patients was satisfactory and acceptable to all the patients. In two cases, the dorsal graft minimally shifted to one side, but remained straight. In one patient, there was late appearance of distortion.
Conclusion:
The mode of cartilage warping is predictable and it can be used to advantage. Apprehension to use costal cartilage graft is unjustified, as with precision carving a desired shape can be obtained.
KEY WORDS: Autogenous cartilage, balanced section, costal cartilage graft, rhinoplasty, warping
INTRODUCTION
Rhinoplasty is one of the most commonly performed aesthetic operations in India today. A typical Indian nose is broader and lacks projection. Often, there is a need for augmentation and that too by a large volume.[1,2,3] A severe saddle nose or a cleft lip nose deformity may require a large volume of graft for contour fill or augmentation. A variety of alloplastic materials is available for this purpose. However, use of autogenous cartilage is safer and preferable.[4,5] Small to moderate augmentation can be managed with septal or conchal cartilage used alone or in combination.[4,5,6,7] However, if the projection needs to be increased substantially or when the grafts need to be placed in multiple locations, the two above mentioned donor sites may not provide enough volume, necessitating the use of costal cartilage.[8,9]
Modern day plastic surgeon is reluctant to use costal cartilage as it is not considered as a meaningful and practical source because of the apprehension of warping. One may think, “warping” makes the graft impossible to carve in the desired shape. The prejudice is understandable but not justified. If the surgeon has operative patience, understands the mechanism of warping, and follows the principle of balanced section as advocated by Gibson and Davis,[10] warping can not only be avoided but can also be used to our advantage.
The phenomenon of warping
Warping is the inherent tendency of the cartilage to deform when subjected to trauma or surgeon's knife. Costal cartilage is hyaline in nature. The chondrocytes secrete ground substance under varied pressure and this produces compression and tension stresses within the cartilage.[11] The cells at the center of cartilage mass are loose packed, have minimum compression force, and hence are round or oval in shape. The compression force gradually increases from the center to the periphery. Cells near the surface, underneath the perichondrium, are subjected to maximum force and are flat in shape [Figure 1]. The outer layer of compressed cartilage has a natural tendency to expand, but this is prevented by the taut perichondrium. When the perichondrium or the related outer subperichondrial layer is removed or breached by surface incisions, the compression force on the cartilage mass is released and it expands. If the incision is only on one side, that surface will expand causing the cartilage to bend [Figure 2]. The combined effect of all such bends is warping. Gibson and Davis established that to prevent warping, the cartilage should either be harvested with intact perichondrium or sectioned in a balanced manner.[10] The option of intact perichondrium all round is not practical because the cartilage simply cannot be carved. Hence, the carved cartilage piece must fit in the precinct of a balanced section. While carving a piece of cartilage, if the surface incisions (hereafter referred to as “cuts”) are of equal depth, and are equally spread on the opposing surfaces (balanced), both the surfaces will equally expand and the piece will not warp. Conversely, when the concave side of a curved piece is scored, that side will expand, neutralizing the curvature [Figure 3]. If the extent of neutralization is controlled by carefully distributed cuts of varying but precise depths, the surface can be made absolutely straight.
Figure 1.
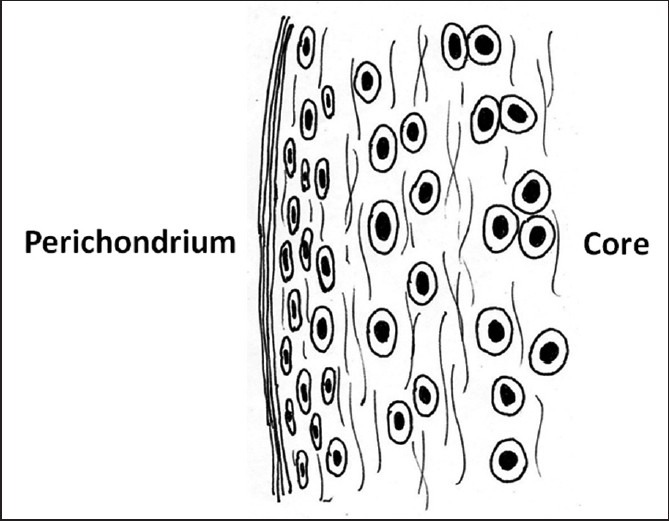
Longitudinal section of the costal cartilage (diagrammatic). The core cells are round while the peripheral (surface) cells are flatter because of compression forces. When relieved of the forces, these cells have a tendency to expand
Figure 2.

Straight piece of cartilage (a). Incision on one side (b). The incision site expands causing the piece to bend (c)
Figure 3.
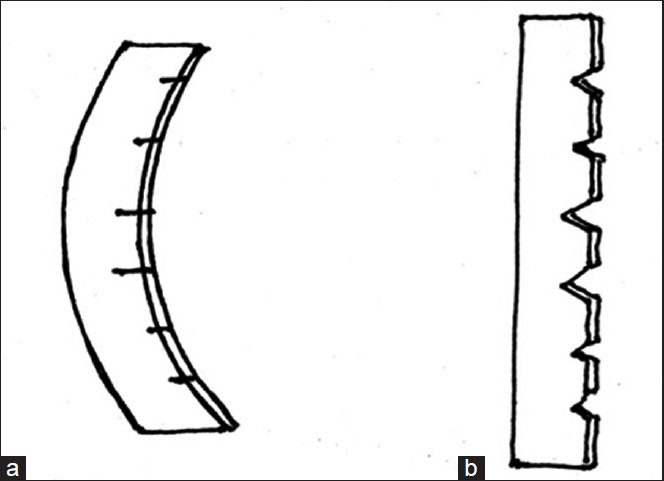
A curved piece of cartilage with incisions on the concave surface (a). The cut surface expands straightening the piece (b)
MATERIAL AND METHODS
We have used 69 costal cartilage grafts in 31 Indian patients (24 males, 7 females) between 18 to 34 years of age over a period of 10 years [Table 1]. Grafts were used for dorsal augmentation, volume fill in lateral wall, as structural graft to ala and columella (columellar strut), and as spreader graft. It has not been used as tip graft in any of our patients [Table 2]. Many patients, particularly reconstructive and cleft patients, required multiple grafts for different locations; the maximum number being 6 (in case 1 described in results). Two-layered construct is considered as one graft.
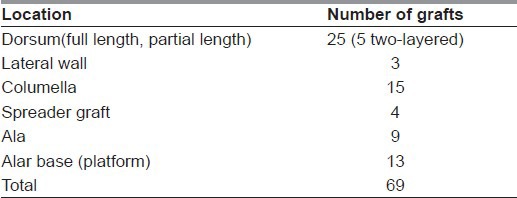
Table 1.
Indications
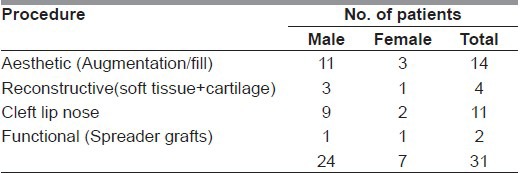
Table 2.
Locations
Procedure
-
Volume Estimation:
The dimensions and volume of the graft were estimated by filling the defect with modeling clay and preparing a template [Figure 4]. The template can be put on a side-trolley for reference during the operation.
-
Method of harvest:
To allow sufficient time for warping, the cartilage harvest and carving is done first, followed by the nasal dissection. If there are two operating teams, graft harvest and nasal steps can be done simultaneously. In any case, sufficient time must elapse before insertion of the carved graft so as to gauge the amount of warping. Any of the 6th, 7th, or 8th costal cartilage may be chosen for harvest. The 8th cartilage has large volume and a straight segment. However, in case of women, 7th or 6th cartilage may be chosen, as these may be harvested through an infra-mammary incision. The 9th cartilage is good for columellar strut.
Cartilage is usually harvested from left side so as not to interfere with the nasal team usually operating from the right side. The harvest is subperichondrial and the perichondrial sleeve is closed.
-
Method of carving:
- Selection of the graft: A relatively straight portion of the harvested cartilage is chosen for carving. The cartilage blocks may be cut from the center (core) or periphery (surface) of the rib cartilage[10,12] [Figure 5]. For large dorsal grafts, the whole width or thickness of the piece is utilized so that the graft is essentially a central piece. The objective is to use the “warping phenomenon” to surgeon's advantage so as to allow a naturally curved piece to warp and straighten. The curvature is neutralized by making the concave surface expand and straighten it by “precision carving.” This can be further shaped as a boat or any other desired shape if required. Two pieces can be stacked one above the other to increase the thickness.
- Analysis of the curvature: The degree of curvature (steep/shallow) and the extent is determined. Occasionally, the curvature may be in two directions, in which case the major curvature is dealt with first.
- An imaginary axis line is drawn along the length of the graft [Figure 6a].
- Incisions of various depths are taken along the concave surface. These decompressing cuts (incisions) can either be superficial, deep, or of intermediate depth [Figure 6a, b]. The superficial cuts (x) reach roughly one fourth the distance between the surface and the axis (one-eighth the distance of the total width of the rib cartilage). The deep cuts (y) reach a bit more than half the distance from surface to the axis, and should never cross the axis. All the cuts begin as superficial cuts and may be deepened subsequently as required.
- Density/spacing of cuts: Two or three cuts, 2-3 mm apart, are first taken at the site of maximum acuity of the curvature. Within seconds, the cut surface expands and curvature is reduced [Figure 7]. As we go away from the region of maximum bend, additional cuts can be superficial and further apart. The initial cuts can be deepened if curvature still persists. The carving has to be conservative as further expansion will take place over a period. One must stop after about 90 to 95% of straightening has taken place. It is a matter of judgment and practice to take precise cuts of adequate depth and spacing to achieve uniform neutralization of the curvature.
-
Obtaining the desired shape.
- Straight or boat: If the piece is to be converted into a boat, the basal surface is conservatively sectioned in an oblique direction [Figure 8a–c]. The expansion may cause curling of the end toward the upper surface. To remove this unwanted projection, the superior surface is also sectioned. When sliced straight [Figure 8d–g], it will expand and will curve downward. Hence, it is cut conservatively, in an oblique plane so as to have a straight surface after expansion [Figure 8h–k].
- Two-layered construct: Two appropriately shaped pieces can be stacked one above the other [Figure 9]. More than a centimeter of projection can be achieved in this manner.
- Curved piece (eg. for ala): A piece from the surface (peripheral) with no violation of outer side will automatically bend toward the outer side [Figure 5b]. A thinner piece will bend more. If required, it can be scored to increase/decrease the curvature.
- For spreader graft, preferably a core piece is chosen [Figure 5a].
- Columellar strut is fashioned from the tip of ninth cartilage or from a central piece of any other cartilage [Figure 10].
Sufficient time (about 45 minutes) is allowed for warping to take place. If the desired shape of the graft is obtained, it may be inserted in the pocket. If there is over-correction causing a reverse bend, which is usually not the case, a few balancing cuts can be made on the opposite surface.
Fixation: The grafts are preferably fixed to maintain the position. Pull-out sutures of 6-0 nylon are used to maintain the position in closed approach while they are sutured to the bed in open approach.
Splintage: Plaster of Paris splint is applied for two weeks. The splint is changed at 48 hours and the position of the graft is inspected. Any minor deviation/shift of the graft can be corrected at this time.
Figure 4.

(a,b) Clay template used to estimate volume and shape of grafts
Figure 5.
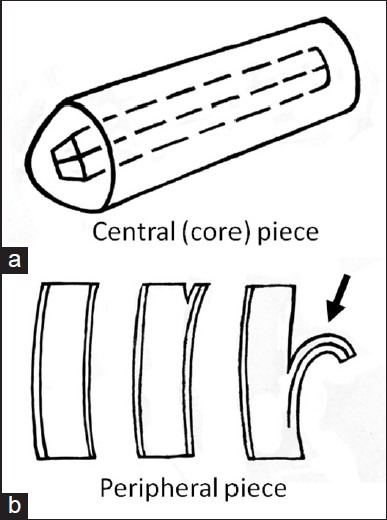
A central piece (a) and peripheral piece (b) harvested from cartilage
Figure 6.
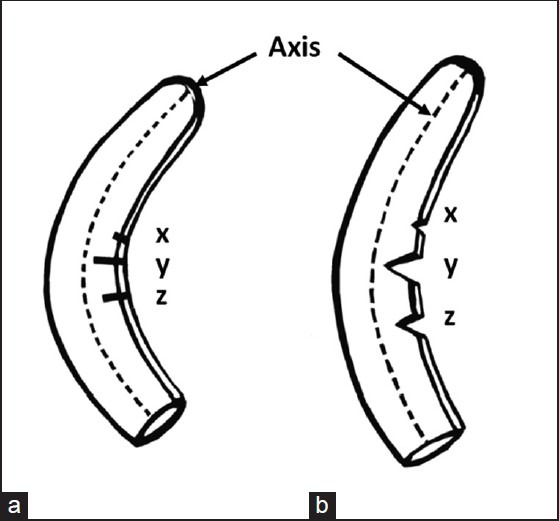
(a,b) Imaginary line drawn along the longitudinal axis of graft. Incisions of superficial (x), deep (y), and intermediate (z) depths
Figure 7.
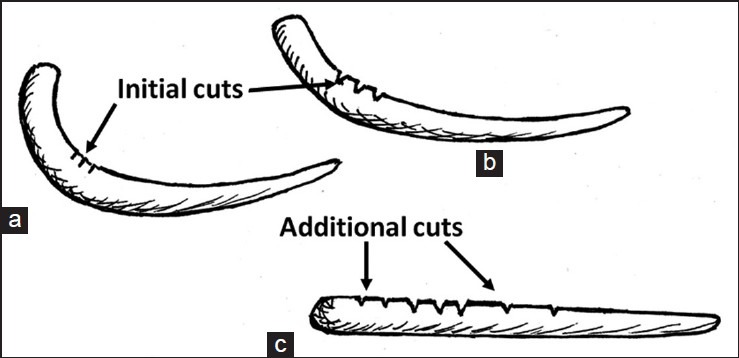
Gradual straightening of the cartilage piece with incisions of varying depths placed at proper distance (a,b,c)
Figure 8.
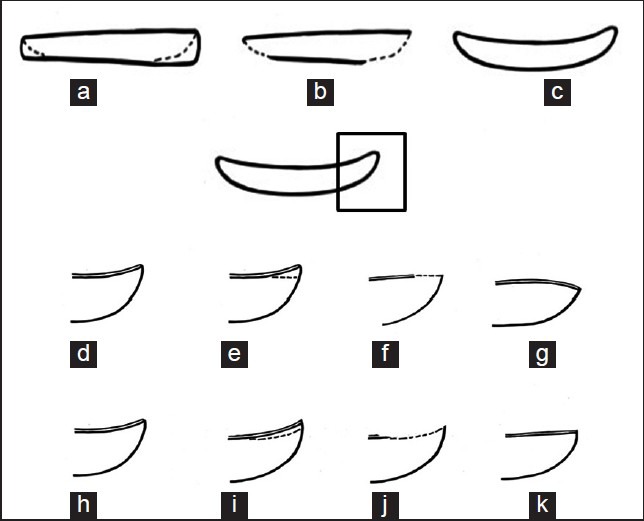
Making a “boat”. A straight piece is beveled at either ends cutting the bottom surface. The cut surface expands and the piece bends at the ends (a,b,c). If the top surface is cut flat, the expansion woul d make that surface slightly convex (d,e,f,g). The correct way is to cut the top surface conservatively (slightly concave), so that expansion makes that surface flat (i,j,k,l)
Figure 9.

Two properly shaped pieces of cartilage can be stacked one above the other and sutured together to achieve greater projection
Figure 10.

A core piece of 9th costal cartilage may be fashioned as columellar strut
RESULTS
The patients were assessed at 4-6 weeks and at 6 months. Subsequent follow-up varied from one to 10 years. All the patients had an uneventful recovery and were satisfied with the outcome.
The results were evaluated taking into consideration the patient satisfaction, graft displacement, warping/distortion of the graft, preservation of shape and volume of the graft. The aesthetic appearance was assessed according to patient's own perception, comparison of photographs, and evaluation by colleagues from allied specialities. Aesthetic results were good to excellent in most of our patients.
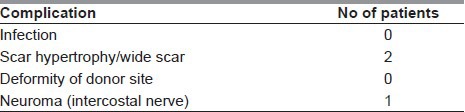
We could get abundant volume of the cartilage so as to meet the requirement. Warping/distortion was seen in only one dorsal graft. In two other cases, the dorsal graft slightly shifted to one side, but remained essentially straight. There was no occurrence of infection or resorption of graft [Table 3]. Donor site complications were minimum [Table 4].
Table 3.
Recipient site complications
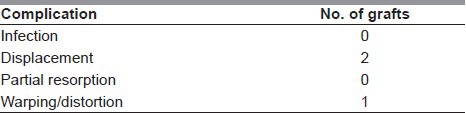
Table 4.
Donor site complications
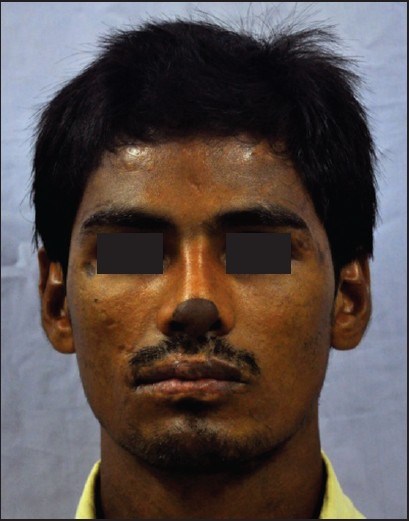
Case 1
A 20-year-old boy had soft tissue reconstruction of lobule and columella done earlier using medial arm flap for a defect following thermal injury. The skin and soft tissues were adequate but cartilaginous framework of the alae and columella was missing. The nasal dorsum lacked definition and the projection was inadequate [Figure 11a, b]. The dorsum required significant volume to get adequate projection as suggested by the template [Figure 11c, d]. Cartilaginous framework was reconstructed using 8th and part of 7th costal cartilage [Figure 12]. Seventh was used for the columellar strut, while 8th was cut into multiple pieces. Two large pieces sutured together as two-layered graft were used for dorsal augmentation. The smaller pieces were carved into suitable grafts for alae and alar base. Postoperative photographs show adequate projection and definition of the dorsum and good structural reconstruction of the tip [Figure 13]. Late postoperative frontal view shows two straight light-reflection lines indicating good definition. There is no evidence of warping [Figure 14].
Figure 11.
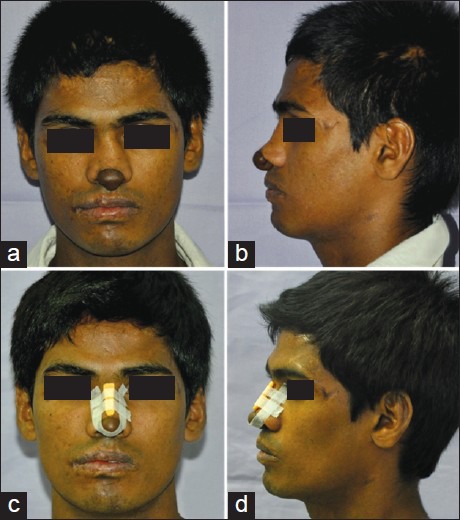
Loss of lobule in this 20-year-old boy was treated earlier with medial arm flap. There is lack of definition of tip and nasal dorsum and inadequate projection (a,b). The volume and shape of the only graft was estimated by using a template (c,d)
Figure 12.

The grafts were fashioned from the 8th costal cartilage and a part of 7th costal cartilage. The piece from 7th cartilage (piece 3) was sliced on the opposite side to fashion the columellar strut. 8th cartilage was cut into multiple pieces piece 1 and 2 were stacked to form a two-layered graft for dorsal augmentation. Piece 4 and 5 were split and used for the ala and alar base, respectively
Figure 13.
Pre-operative (a,b) and 6-month postoperative (c,d) pictures showing good definition and adequate projection of the dorsum and good configuration of the tip
Figure 14.
Twenty-month postoperative picture shows two dorsum defining lines reflecting light. There is no evidence of warping
Case 2
A 22-year-old man had post-traumatic deformity of the nose. There was severe depression of the dorsum and collapse of the right lateral wall. The overlying scarred and unstable skin was replaced earlier with a forehead flap [Figure 15a]. Reconstruction of framework was done later using 8th and 9th costal cartilages. Two large pieces from 8th cartilage were used for the dorsum and the lateral wall, while the 9th was used for columellar strut [Figure 15b–d]. Postoperative photographs show good aesthetic reconstruction of the dorsum and side wall [Figure 16a–h].
Figure 15.

A 22-year-old man with post-traumatic severe depression of dorsum and collapse of right lateral wall of nose. Unstable scar over the dorsum was replaced earlier with forehead flap (a). Eighth costal cartilage was cut into two pieces (b,d) one for the dorsum and the other for the lateral wall. Ninth costal cartilage was used for the columellar strut (c,d)
Figure 16.

Preoperative (a,b,c,d) and postoperative (e,f,g,h) pictures showing results at 6 months. Grafts have retained their shapes without any warping
Case 3
A 33-year-old male presented with functional airway obstruction due to internal nasal valve collapse. This was treated with spreader grafts and a columellar strut carved from 7th costal cartilage. Superficial edges of the spreader grafts contribute to the nasal dorsum defining lines and should remain straight. More than two years later, patient is breathing well and nasal dorsum is straight indicating no warping. Tip-plasty has improved tip definition [Figure 17a–g].
Figure 17.
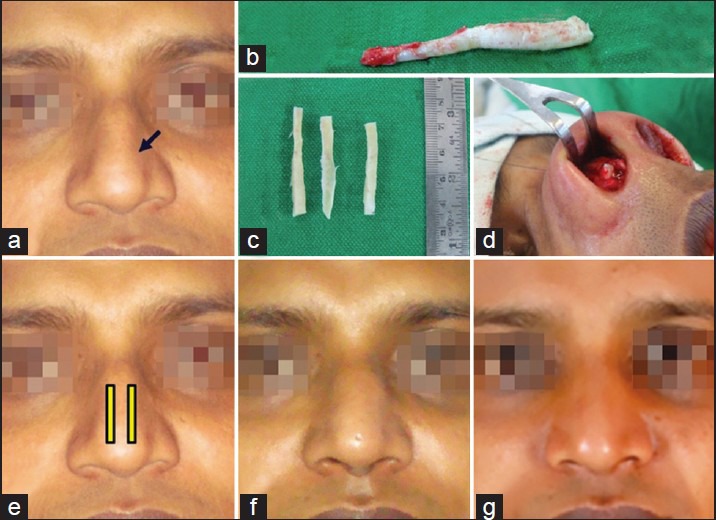
A 33-year-old male with internal nasal valve collapse (arrow) (a). Spreader grafts and a columellar strut were carved from 7th costal cartilage (b,c). Intraoperative placement of spreader grafts and its pictorial representation showing their relationship with nasal dorsum (d,e). The hump was also rasped. Three-month postoperative pictures show no warping (f). At 2 years 5 months (g), the edema has settled, nasal dorsum is straight, not too wide, and there is good definition of the tip
Case 4
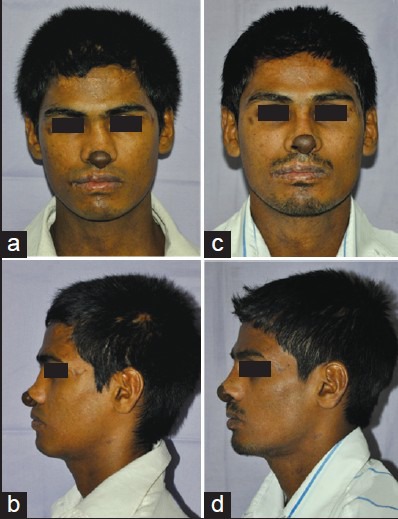
A 35-year-old male had depressed nasal bridge and alar base [Figure 18]. Estimation of the volume and shape of dorsal and alar base grafts was done using templates [Figure 19a, c]. Grafts were carved from the 8th costal cartilage [Figure 19b]. Two triangular pieces were used for the alar base while a two-layered graft was used for the dorsum [Figure 19d, e]. Twelve-month postoperative views show good projection of nasal dorsum [Figure 20].
Figure 18.

A 35-year-old male with depressed nasal bridge and depression along the alar base
Figure 19.
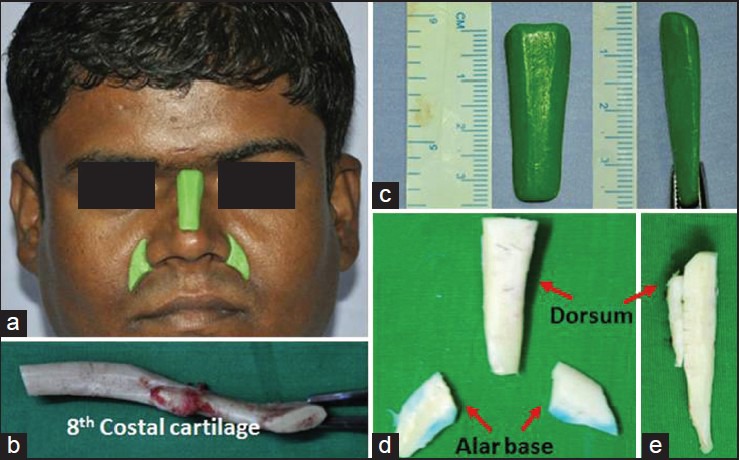
Preoperative estimation of volume and shape of the grafts was done using templates (a). Eighth costal cartilage was harvested (b). The templates (c) were used as a guide to carve the grafts (d). Dorsal graft was made of two layers to achieve required projection (e)
Figure 20.

Preoperative (a,b) and 12 months postoperative (c,d) pictures show good dorsal augmentation without any warping
Case 5
A 20-year-old man had two previous operations for correction of cleft lip nasal deformity [Figure 21a, b]. Correction was done by repositioning of the alar cartilages and augmentation of the dorsum using a graft from 8th costal cartilage. The postoperative views at 12 months [Figure 21c, d] show adequate correction and a well-defined dorsum. There is slight shift of the graft to the right but there is no evidence of warping. Even after 10 years, the graft has remained straight [Figure 21e, f].
Figure 21.
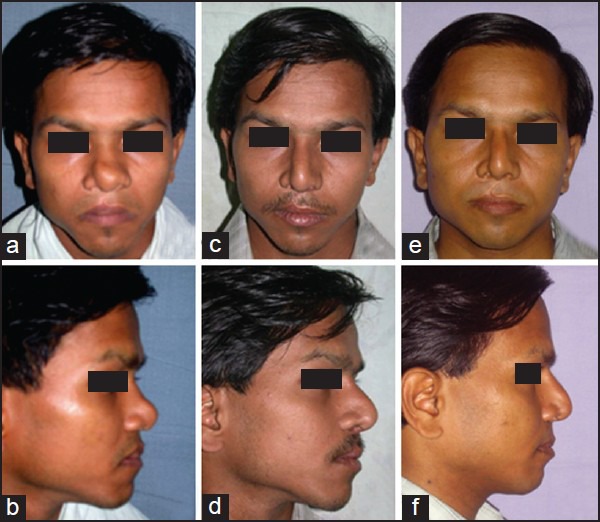
A 20-year-old man operated twice before for correction of cleft lip nasal deformity (a,b). Repositioning of the alar cartilages was done along with a dorsal graft from 8th costal cartilage. Twelve-month postoperative view shows the graft has shifted slightly to the right, but has remained straight (c,d). The result is maintained at 10 years (e,f)
Case 6
An 18-year-old girl had cleft lip nose deformity. Left ala was hypoplastic and displaced. The tip was broad and turned to the left side and columella was short [Figure 22a]. The lip was revised and a flap from the previous scar was used for columellar lengthening [Figure 22b]. The alar cartilage was repositioned and multiple grafts harvested from 7th costal cartilage were used for columellar support and augmentation of the ala, alar base, and nasal dorsum [Figure 22c, d]. Septal correction and lateral and medial osteotomies were also performed. Eight-month postoperative views show a slender nose with a straight dorsum and well-defined tip. There is good dome symmetry and the alar platform is also augmented [Figure 23a–h].
Figure 22.
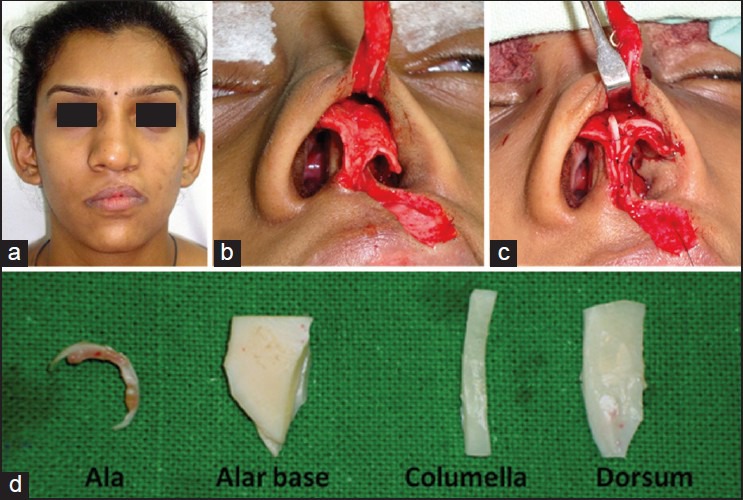
An 18-year-old girl with cleft lip nasal deformity (a). The columella is short and the alar cartilage is malpositioned (b). Intraoperative view of the reconstruction showing the columellar strut, repositioning of the alar cartilage and a graft for the ala (c). The grafts used for reconstruction were cut from 7th costal cartilage(d)
Figure 23.

Preoperative (a,b,c,d) and eight-month postoperative views (e,f,g,h) following nasal osteotomies, septoplasty, columella lengthening, and cartilage reconstruction. The dorsum is straight, alar cartilages are well positioned with good dome configuration. Alar base is also augmented
Case 7
A 22-year-old male had inadequate projection of the nasal dorsum [Figure 24a, b]. A two-layered graft from 7th costal cartilage was used for dorsal augmentation [Figure 24c]. Postoperative views taken at 6 months as well as at 2 years show a pleasing dorsal line of the nose [Figure 25]. The graft has maintained both volume and shape.
Figure 24.
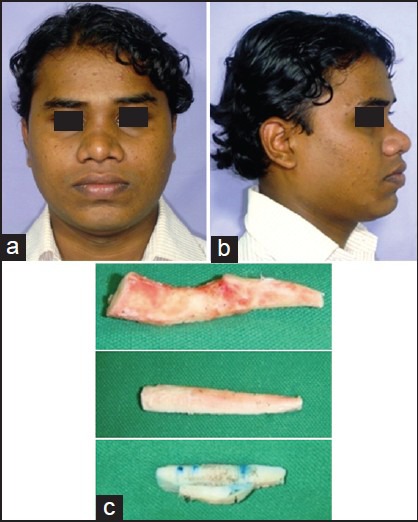
A 22-year-old male with inadequate projection of dorsum (a,b). Seventh costal cartilage was carved into a straight piece, which was cut into two pieces. A two-layered graft was used for dorsal augmentation (c)
Figure 25.
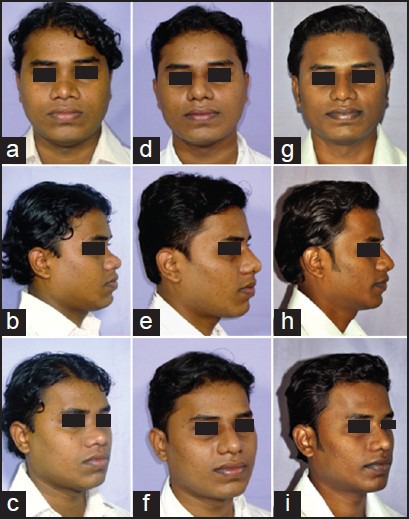
The preoperative views (a,b,c) show inadequate projection of the dorsum. Six-month postoperative views (d,e,f) show vastly improved dorsal line. The result is maintained at 2 years (g,h,i)
Case 8
A 34-year-old man had skin and soft tissue defect of the right lateral wall and ala reconstructed using forehead flap [Figure 26a, e]. The nose had inadequate projection of dorsum and tip and lack of support for the right ala. Eighth and 9th costal cartilages were used for dorsal augmentation and columellar strut grafts [Figure 26d, h]. Two thin slices of warped cartilage were used for right ala. Six-week postoperative photographs [Figure 26b, f] show good augmentation and straight dorsum. Twenty-month postoperative photographs [Figure 26c, g] show distortion of the dorsal graft. The deforming forces caused by scarring around the bed could have contributed to this late distortion either alone or in combination with actual warping. No revision was attempted as the patient has accepted the result well.
Figure 26.

A 34-year-old male had forehead flap reconstruction done earlier for the defect of right ala and lateral wall of nose. Preoperative views (a,e) show inadequate projection of dorsum, collapse of the right ala and improper draping of the skin cover. Eight and 9th costal cartilages were used (d,h) to carve the grafts for the dorsum (1), columella (2), and right ala (3) along with redraping of skin. After 6 weeks, dorsum is straight with good projection and right ala is well supported (b,f). At 20 months (c,g), there is distortion of the dorsum
DISCUSSION
Autogenous cartilage is the most favorable material for nasal augmentation.[4,5] It withstands functional stresses and its demands for blood supply are less. As it can survive by delivery of nutrients by diffusion alone, chances of resorption are less.[7,13] The nasal septum and the ear concha are better source of cartilage, but the volume is limited.[6] These sources may have been exhausted because of previous operations. The costal cartilage provides abundant volume which is required in difficult situations like revision rhinoplasty, severe saddle nose, deformities following previous submucous resection of the septum, and cleft lip nose.[4,9] In saddle nose, the desired augmentation may be a centimeter or more, while in cleft lip nose, cartilage is required at multiple locations, including a large volume at the alar base to correct the retruded maxillary platform. Judicious use of costal cartilage is a logical and realistic solution for these challenging cases.
The majority of the patients in our series are men as most women seem to be reluctant to have the costal cartilage harvested. However, women with cleft lip nose did not mind removal of cartilage and the resultant scar.
The cartilage is removed subperichondrially. Exclusion of perichondrium does not alter the shape of the harvested piece. The intact perichondrial sleeve at the donor site may result in regeneration of cartilage.[14]
Most of the cases in our series had good outcome as the shape and the volume of the graft were estimated preoperatively. As the graft is prepared at the beginning of the operation, enough time elapses before the insertion. Almost 90% of the warping is complete at 15 minutes in case of central grafts and at 30 minutes in case of peripheral grafts.[12] It is a good practice to get only 95% of the straightening on table, as the rest will occur over course of time. It does require judgment to decide how much is 95% and how much more is expected; but the room for error is less in any case. Secondly, the cuts have to be well planned, and precise in depth and spacing. That is why we call this maneuver “precision carving.”
The result at four weeks can be considered as stable in shape, as further warping is unlikely to occur. In our series, one patient developed late deformation of the dorsal graft [Figure 26]. Scot Harris et al.[12] have suggested two explanations for this late deformation of graft after remaining straight for months resolution of local swelling revealing true warpage that occurred much earlier and presence of deforming forces around the graft. In the latter situation, an external force is responsible for the distortion and “warping” phenomenon is unnecessarily blamed. In the above patient, the contractile forces created by the scarred tissues on right side might have caused the late distortion of graft. In two other patients, the grafts shifted slightly to one side, but there was no warping [Figure 21].
Gibson and Davis have described four different shapes for the dorsal grafts.[10] These limited options of shapes are difficult to execute and suitable for moderate volume. For finesse in rhinoplasty, we need to have variety of shapes with natural contours. We recommend simple straightening of the full thickness rib cartilage followed by converting it into the desired shape (eg., a boat). These grafts are unbalanced grafts, as they are not equally carved on opposite surfaces. Warping is not prevented, in fact it is allowed, so that the graft is made to “warp into” the shape. It may be stacked to make a two-layered graft which can achieve a projection of more than a centimeter.
Other methods of prevention of warping are passing an axial K wire,[15] the “Turkish delight” technique described by Erol,[16] and use of “diced cartilage-fascia” described by Daniel et al.[17]
Passing an axial K wire through the graft is cumbersome, particularly in the case of a columellar strut. There is a possibility of extrusion of the K wire, and the patient may not be comfortable with the idea of having a K wire in the nose. The “Turkish delight” and “diced cartilage wrapped in fascia” techniques are effective in preventing warping and have produced excellent results. Both the authors mention that the graft is malleable for some days postoperatively.[16,17] The malleability is definitely an advantage; however, we feel that accidental change of shape is possible with an unintentional pressure, including that from a stiff envelope. If proper care, including not using the glasses temporarily as suggested by Daniel et al.,[17] is not taken, they may distort (No such complication is reported in the above two series.). As stated by these authors[16,17] and also by others,[18] it is difficult to use the diced graft for structural support (ala, spreader graft, or columellar strut).
Our method is time-consuming and does have a learning curve. Once one is familiar with the technique, the total time to shape the graft is about 45 to 60 minutes depending on the number of grafts to be used. The graft can be given the exact desired shape by using a template and carrying out precision carving. The graft is rigid and holds shape well. We do not claim that rigid grafts are superior to the diced ones; but the advantage is they can be used for structural support. The appearance is natural and long lasting and the complications are few. The “visibility” of the graft edges is not a problem in Indian patients. Above all, there is a tremendous benefit of having the autogenous material in abundance. We believe the benefits simply outweigh the disadvantages.
CONCLUSION
Warping phenomenon is not yet fully understood. However, rather than its prevention, it may be allowed to happen, in a controlled, programmed manner so that it can be used to straighten a curved piece of cartilage (or vice versa), the manner in which cartilage warps is not capricious, but very much predictable. With precision carving, even unbalanced costal cartilage graft can be used safely for providing required shape and volume. It can also be used as a two-layered graft if more augmentation is required.
Neither the apprehension nor the criticism is justified; as with precision carving, a desired shape of the graft can be obtained.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bhat U, Patel B. Primary rhinoplasty: An Indian Perspective. Indian J Plast Surg. 2008;41:9–19. [PMC free article] [PubMed] [Google Scholar]
- 2.Ortiz Monasterio F, Michelena J. The use of Augmentation rhinoplasty techniques for the correction of the Non-Caucasian nose. Clin Plast Surg. 1988;15:57–72. [PubMed] [Google Scholar]
- 3.Matory WE, Falces E. Non- Caucasian rhinoplasty: A 16- year experience. Plast Reconstr Surg. 1986;77:239–52. doi: 10.1097/00006534-198602000-00011. [DOI] [PubMed] [Google Scholar]
- 4.Lovice DB, Mingrone MD, Toriumi DM. Grafts and implants in rhinoplasty and nasal reconstruction. Otolaryngol Clin North Am. 1999;32:113–41. doi: 10.1016/s0030-6665(05)70118-3. [DOI] [PubMed] [Google Scholar]
- 5.Staffel G, Shockley W. Nasal Implants. Otolaryngol Clin North Am. 1995;28:295–308. [PubMed] [Google Scholar]
- 6.Gunter JP, Rohrich RJ. Augmentation Rhinoplasty: Dorsal onlay grafting using shaped autogenous septal cartilage. Plast Reconstr Surg. 1990;86:39–45. [PubMed] [Google Scholar]
- 7.Rodney JR, Arshad RM. Primary rhinoplasty. In: Mathes SJ, Hentz VR, editors. Plastic Surgery. 2nd Ed. Vol. 2. Philadelphia, PA: Elsevier Saunders; 2006. pp. 427–72. [Google Scholar]
- 8.Hartley JH., Jr . Secondary rhinoplasty. In: Mathes SJ, Hentz VR, editors. Plastic Surgery. 2nd Ed. Vol. 2. Philadelphia, PA: Elsevier Saunders; 2006. pp. 765–99. [Google Scholar]
- 9.Sherris DA, Kern EB. The versatile autogenous rib graft in septorhinoplasty. Am J Rhinol. 1998;12:221–7. doi: 10.2500/105065898781390136. [DOI] [PubMed] [Google Scholar]
- 10.Gibson T, Davis WB. The distortion of autogenous cartilage grafts: Its cause and prevention. Br J Plast Surg. 1958;10:257. [Google Scholar]
- 11.Fry H. Cartilage and cartilage grafts: The basic properties of the tissues and the components responsible for them. Plast Reconstr Surg. 1967;40:426. [PubMed] [Google Scholar]
- 12.Harris S, Pan Y, Peterson R, Stall S, Spira M. Cartilage warping: An experimental model. Plast Reconstr Surg. 1993;92:912–5. [PubMed] [Google Scholar]
- 13.Randolph MA, Yaremchuk MJ. Repair, Grafting, and Engineering of Cartilage. In: Mathes SJ, Hentz VR, editors. Plastic Surgery. 2nd Ed. Vol. 1. Philadelphia, PA: Elsevier Saunders; 2006. pp. 621–38. [Google Scholar]
- 14.Lester CW. Tissue replacement after subperichondrial resection of costal cartilage: Two case reports. Plast Reconstr Surg Transplant Bull. 1959;23:49–54. [PubMed] [Google Scholar]
- 15.Gunter JP, Clark CP, Friedman RM. Internal stabilization of autogenous rib cartilage grafts in rhinoplasty: A barrier to cartilage warping. Plast Reconstr Surg. 1997;100:161–9. doi: 10.1097/00006534-199707000-00026. [DOI] [PubMed] [Google Scholar]
- 16.Erol OO. The Turkish delight: A pliable graft for rhinoplasty. Plast Reconstr Surg. 2000;105:2229–41. doi: 10.1097/00006534-200005000-00051. [DOI] [PubMed] [Google Scholar]
- 17.Daniel RK, Calvert JW. Diced cartilage grafts in rhinoplasty surgery. Plast Reconstr Surg. 2004;113:2156–71. doi: 10.1097/01.prs.0000122544.87086.b9. [DOI] [PubMed] [Google Scholar]
- 18.Kelly MH, Bulstrod NW, Waterhouse N. Versatility of diced cartilage-fascia grafts in dorsal nasal augmentation. Plast Reconstr Surg. 2007;120:1654–58. doi: 10.1097/01.prs.0000285185.77491.ab. [DOI] [PubMed] [Google Scholar]


