Abstract
Context:
Facial fillers have revolutionized the field of cosmetic facial rejuvenation as it has become the prime sought – after rejuvenation procedure offering youthful, 3-dimensional look with minimal invasiveness. Fillers are expensive and need to be redone periodically hence a sound understanding of structural basis on which they are laid is important in reducing the quantity of filler required in each sitting as well as increasing the longevity of results.
Aim:
The aim of the following study is to analyse a novel method of facial filling “The pillars pyramids and tie beams (PPT)” technique and its advantages over the conventional methods.
Subjects and Methods:
A novel technique of injecting the facial fillers was employed on 67 patients visiting our clinic. These patients were followed-up for a period of 3 years.
Results:
We observed that the amount of filler material required in initial sitting remains the same, however the frequency of touch up visits is decreased and so is the amount of filler material required for follow-up injections.
Conclusion:
Facial contour remodelling is being revolutionised by the new filler materials for volume augmentation and no uniform consensus has been reached on the techniques currently used in clinical practice. We advocate this novel PPT technique of facial filling in facial rejuvenation to restore a youthful look as a primary goal.
KEY WORDS: Aging face, facial fillers, facial rejuvenation, hyaluronic acid
INTRODUCTION
The field of cosmetic facial rejuvenation has been revolutionised by the availability of facial fillers in differing densities. Fillers are now a prime sought after rejuvenation procedure as they offer a youthful 3 dimensional look with minimal invasiveness.[1] Aging of human face is a complex dynamic interplay of various factors involving 3 dimensional changes in the skeletal as well as soft tissue structure along with superficial textural changes of skin wrinkling.
Aging individually affects all the components of skin and subcutaneous soft-tissues which comprise of fat, muscle, fascia along with structural support provided by bones and dentition. This is compounded by effects of gravity, sun insult, smoking and hormonal imbalances.[2,3] The net effect has been found to be loss of facial volume and skin texture.[4]
Classically the aging face is assessed by dividing it into three anatomic zones. The midface naturally commands more respect as it is central and comes to the notice first because it is the most dynamic region of the face while one interacts with others. The midfacial attractiveness is a function of synergy among the eyes, nose, lips and malar prominences what is commonly referred to as the central facial triangle.[2] Facial aging involves loss of volume in certain areas of face (periorbital, forehead, malar, temporal, mandibular, mental, glabellar and perioral sites) and persistence or hypertrophy of fat in others (submental, lateral nasolabial fold and labiomental crease, jowls, infraorbital fat pouches and malar fat pad).
A selective hypertrophy of the of the cheek pad fat also complements the ptosis leading to midface aging changes. The ptotic hypertrophied cheek fat needs to be contoured as the facial muscles hardly show changes over age.[5] Apart from the conventional facelift techniques, structural fat grafting has been attributed as an ideal facial filler.[6] The adipose tissue having the maximum percentage of stem cells of any tissues in the body can fill large and small soft-tissue defects of the face thus acting as a permanent facial filler.[6]
A recent trend towards non-surgical techniques of facial rejuvenations has led to increase in demand for the facial fillers for enhancing facial features and symmetry with immediate results and minimal recovery time.
SUBJECTS AND METHODS
A retrospective case series analysis study was carried out at our institute about a novel method of facial filling, the ‘hammock method” which includes building up the pillars and pyramids using a more viscous filler and connecting them using a less viscous filler. The study period spanned from 1st July 2011 to 30th June 2013 over a period of 24 months. 67 patients were included in the study which included 48 females and 19 males.
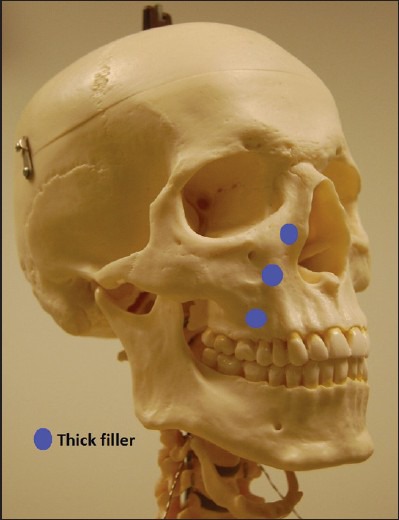
A detailed history about the past medical events, medications being used, history of drug allergies, with stress on diabetic and anticoagulant medication were recorded. Patients with the above medical conditions were excluded from the study. A detailed clinical examination and the patient's expectations on the outcome were discussed and explained in detail. Pre-operative photographs were taken [Figure 1]. A written informed consent was taken after having a detailed discussion on the pros and cons of the procedure including the full details about the filler to be used, expected longevity of results, its approval status, possible side effects and the cost. Furthermore, the newer methods of facial filling and its advantages were explained to the patients.
Figure 1.

Deep nasolabial folds
Procedure included cleaning the area with povidine-iodine solution and wiping the area with wet normal saline wipes. Later EMLA cream (eutectic mixture of lidocaine 2.5% and prilocaine 2.5%) is applied onto the area to be injected and covered with occlusal dressing and left in place for 15-20 min. No local infiltration anaesthesia was given in routine cases but, in apprehensive and sensitive patient's infraorbital blocks were given in addition.
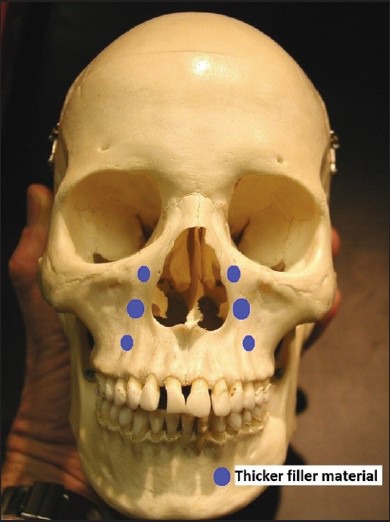
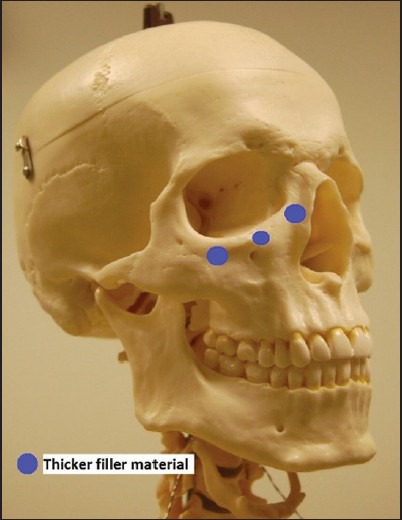
In the nasolabial folds and the infraorbital area our technique involved a novel method of laying the fillers, called the pillars pyramids and tie beams (PPT) technique by constructing pillars, pyramids and tie beams in the form of a hammock. Here the filler was used in 3 layers the supra periosteal, the subdermal and the dermal layer [Figures 2 and 3]. 0.5 ml of the more viscous filler was used in erecting the pyramids 3-4 pyramids in each area with their base down supraperiosteally and 0.5 ml lesser viscous fillers was used in each area by connecting the pillars and pyramids dermally and subdermally by the threading method [Figures 4–9]. The technique included creating a hammock tied to the tips of the pillars and pyramids [Figure 10]. By this method the standard volume of filling was adhered and rejuvenation was done to patient's satisfaction. The patient was asked for a follow-up at the end of a week. The patient was advised to avoid exposure to extreme cold or heat, avoid massaging treated areas for 6 h, avoid strenuous physical activity for 6 h, sleep with the head elevated for one night, analgesics if needed and allowed to continue the skin care products the next day. Furthermore, the patient was explained that a bruise may be seen the next day with pain which will usually subside in a weeks’ time which can be camouflaged with skin cosmetics. Since the needle manipulation was minimal the swelling of the area along with pain was limited.
Figure 2.

Pyramids and pillars placed with high molecular weight fillers
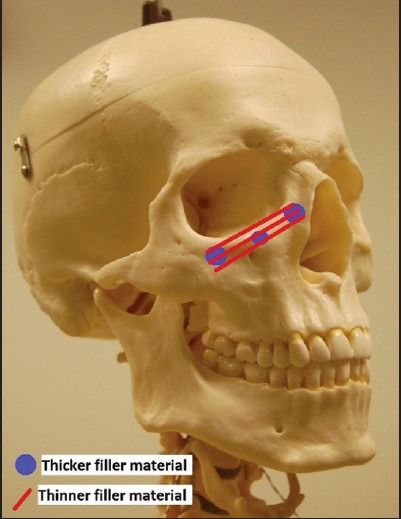
Figure 3.

Pillars being connected with low molecular weight filler tie beams
Figure 4.
Pyramids placed using high molecular weight filler material, more on the periosteum and minimal subdermally
Figure 9.
Schematic diagram of the low molecular weight filler material used as tie beams over pyramids
Figure 10.
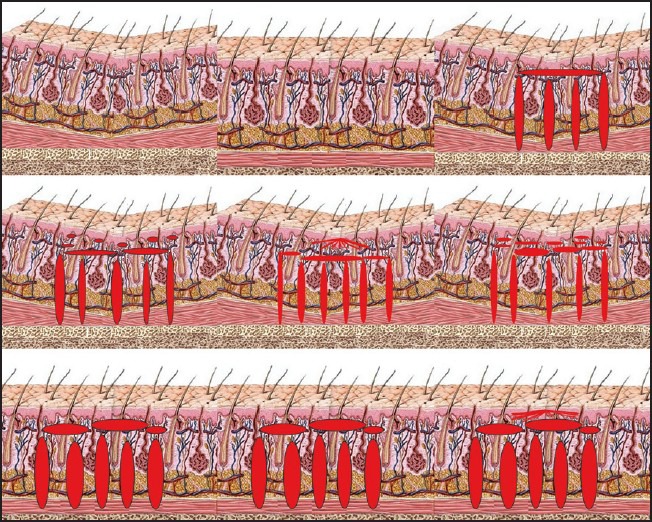
Schematic representation of the “pillars pyramids and tie beams technique” of facial filling. Note that the filler gets hydrated over initial week to restore the lost volume
Figure 5.
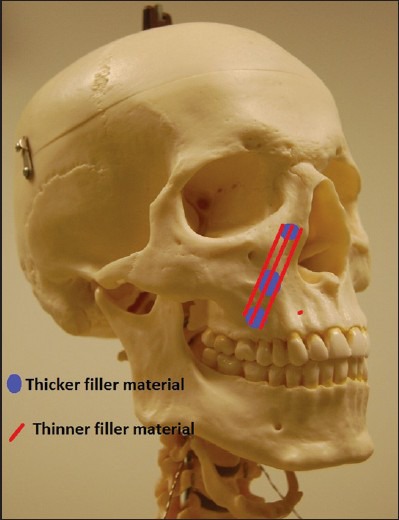
Low molecular weight filler materials placed as tiebeams across the pyramids
Figure 6.
Schematic diagram of the high molecular weight filler material used as pillars
Figure 7.
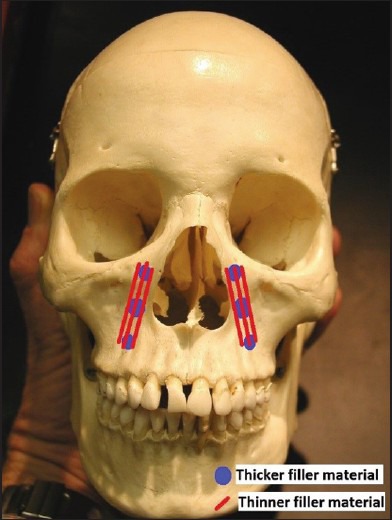
Schematic diagram of the low molecular weight filler material used as tie beams over pyramids
Figure 8.
Schematic diagram of the high molecular weight filler material used as pillars
All the patients were followed-up regularly at 1 week, 6 weeks and 6 months post injection. After that the patients were asked to follow-up whenever they felt that they needed a touch up to add to the area.
RESULTS
This novel method of dermal filling has given considerably better results particularly in the midface volume restoration. As minimal amount of filler with strict adherence of the standard guidelines was done, the complication rate was negligible. Immediate concerns like pain and bruising were seen in some patients but no incidence of erythema, asymmetry, bumpiness, lumpiness, anaphylaxis, oedema, acneiform eruptions was seen. No incidences of late complications like an inflammatory nodule, Tyndall effect, allergic reactions, vascular occlusion and granulomas were seen.
The longevity of results was found to be consistently better than the conventional filler laying methods [Figures 11a–d and 12a and b] The conventional method required later refilling sessions at 8-10 months whereas in the PPT technique this is at 12-14 months. Also the amount of filler material required in subsequent sessions was found to be lesser in our technique.
Figure 11a.

Pre procedure front view of a 42 year lady with deep nasojugal and nasolabial folds
Figure 11d.

Post procedure half lateral view of a 42 year lady with deep nasojugal and nasolabial folds
Figure 12a.
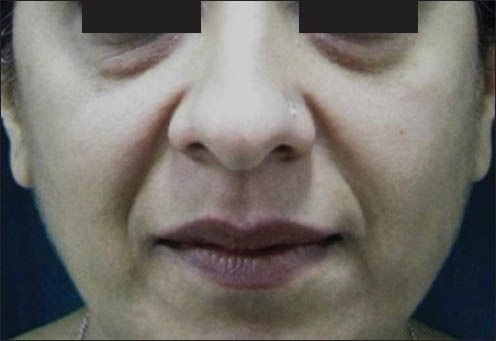
Pre procedure picture of a 47 year lady with deep nasolabial and nasojugal folds
Figure 12b.

Post procedure picture of a 47 year lady with deep nasolabial and nasojugal folds
Figure 11b.

Post procedure front view of a 42 year lady with deep nasojugal and nasolabial folds
Figure 11c.

Pre procedure half lateral view of a 42 year lady with deep nasojugal and nasolabial folds
DISCUSSION
A balanced distribution of superficial and deep fat conferring a 3 dimensional anatomy well-delineated by a series of arcs and convexities is a feature of a normal youthful face.[7,8] The aging process is not uniform all along the face and leaves a contour abnormality resulting from volume deficiency below the dermal plane.[2] As the subcutaneous fat of the face is not uniform and is compartmentalised and each compartment ages at a different pace in the same individual, so each compartment should be addressed individually.[8,9]
Hyaluronic acid (HA) dermal fillers are the most sought after, non-permanent injectable materials available today for the correction of aging changes of the face.[10] HA has excellent water binding capacity and also is fluid enough which offers an ease of injection.[10,11] Facial fat gets redistributed and appear as pockets due to the disappearing of surrounding fullness which is seen particularly in submaxillary areas and bony protuberances.[9,12] Furthermore the malar fat pad gradually slides forward and down bulging against the nasolabial crease, giving rise to prominence of the nasal fold.[9,12] This redistribution and demarcation of fat gives the senile face an unbalanced appearance.[9,12]
The unbalanced facial appearance with fat redistribution and loss of fullness is to be restored as a primary goal of facial rejuvenation. It involves smoothening the facial pockets and recreating the primary arcs and convexities of the youth. Surgical face lift procedures includes lifting and tightening the facial skin which has sagged as a result of atrophy and loss of elasticity.[12,13] Recent trends in facial rejuvenation involve a paradigm shift from conventional excision and suspension procedures to conservative skin excision, deep fascial–superficial musculoaponeurotic system manipulation, volume restoration and modification of facial animation.[13] Facial fillers have emerged as logical and effective modality for lifting, filling and resurfacing the facial soft tissues and can also be used along with other surgical facial rejuvenation techniques.[12,13]
Midfacial volume restoration is not basically correcting the deficiency in tissue levels of HA but a true augmentation of the HA.[14] The HA ratios in the foetal as well as the aged skin is nearly unaltered, so HA as the filler will only act as a mere augmentation.[14,15] It has the intricate physical properties of increased longevity, filling capacity and the ease of injection making it accurate for facial rejuvenation. The longevity of the filler depends on the degree of crosslinking in HA which increases the viscosity and reduces free radical and enzymatic degradation. The more the crosslinks, more is the viscosity and cohesivity giving a sustained dermal lift but more difficult to inject through a thin needle.[16,17] The lower molecular weight, higher viscous HA is slowly biodegraded as it is in excess to the naturally existing HA in the dermis. It retains water and volume, until it reaches a critical level where it rapidly disappears.[18]
In general the narrowest calibre needle that can deliver the filler subdermally with the least amount of pain sensation is used. The amount of the filler, the type and the depth is determined by the defect. The less deep defects can be filled with less volume of fillers used superficially while the deep defects need more volume at deeper levels and lesser volume superficially.[19]
As far as the techniques for filler injection are concerned no consensus has been reached. Commonly used techniques are the serial puncture, threading, fanning, crosshatching and the sandwich methods.[19] Techniques are tailored to surgeon's expertise, defect volume and anatomy and the viscosity of the filler being used. Lip augmentation and superficial defects filling are done by the serial puncture technique where small boluses are delivered along a line to be augmented with serial punctures.[19] The threading technique, where the needle is inserted and tunnelled and the filler is deposited at a slow continuous line when the needle is withdrawn making it a better technique for nasolabial fold and lip defects. Threading done in a radial fashion without withdrawing the needle is also called as a fanning technique, while series of threads injected in a perpendicular fashion is the cross-hatching technique. These are used to fill larger defects; mixture of superficial and deep threading and serial punctures is what is described as the sandwich technique.[19]
Desired results are not attained if an under correction or overcorrection of the defect is done. Under correction is seen when a lesser amount of filler is placed in the subcutaneous plane. Furthermore it occurs when lesser amount of fillers are used in a larger defect due to financial constraints. Lesser viscous fillers if used at a deeper plane without superficial augmentation also leads to under correction.[20] Overcorrection is seen where excess fillers are used in comparison to the volume deficiency and appear as palpable nodules. This gives an unnatural look which is less satisfactory as compared to under correction. The only treatment for overcorrection is to use hyalase to breakdown the filler.[21] In an effort to standardise the technique of dermal filling we introduced the PPT method (PPT technique) which uses a minimum amount of filler in a systematic method to optimise results.
The logic behind the PPT technique is that laying the higher density filler material in a structurally sound manner creates a firm background over which fine tuning can effectively be done with a lighter density filler material. The use of lighter density filler material on this solid base in miniscule quantities virtually eliminates the risk of overcorrection. Also we encountered that the average time interval between subsequent sittings is increased to 12-14 months as compared to 8-10 months for conventional techniques. Also the volume of filler material required in subsequent sittings is reduced as the pillars and pyramids constructed with higher density material continue to provide residual support for longer periods.
CONCLUSION
Facial fillers being a safe, simple and effective modality of facial rejuvenation can be made to work well with this PPT technique. Secret of facial rejuvenation lies in an accurate knowledge of the topography of facial aging, areas of injection, proper patient selection and a suitable technique giving optimal results with minimal complications.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Klein AW, Elson ML. The history of substances for soft tissue augmentation. Dermatol Surg. 2000;26:1096–105. [PubMed] [Google Scholar]
- 2.Coleman SR, Grover R. The anatomy of the aging face: Volume loss and changes in 3-dimensional topography. Aesthet Surg J. 2006;26:S4–9. doi: 10.1016/j.asj.2005.09.012. [DOI] [PubMed] [Google Scholar]
- 3.Bartlett SP, Grossman R, Whitaker LA. Age-related changes of the craniofacial skeleton: An anthropometric and histologic analysis. Plast Reconstr Surg. 1992;90:592–600. doi: 10.1097/00006534-199210000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Pessa JE, Zadoo VP, Yuan C, Ayedelotte JD, Cuellar FJ, Cochran CS, et al. Concertina effect and facial aging: Nonlinear aspects of youthfulness and skeletal remodeling, and why, perhaps, infants have jowls. Plast Reconstr Surg. 1999;103:635–44. doi: 10.1097/00006534-199902000-00042. [DOI] [PubMed] [Google Scholar]
- 5.Gosain AK, Klein MH, Sudhakar PV, Prost RW. A volumetric analysis of soft-tissue changes in the aging midface using high-resolution MRI: Implications for facial rejuvenation. Plast Reconstr Surg. 2005;115:1143–52. doi: 10.1097/01.prs.0000156333.57852.2f. [DOI] [PubMed] [Google Scholar]
- 6.Coleman SR. St. Louis, MO: Quality Medical Publishing; 2004. Structural Fat Grafting. [Google Scholar]
- 7.Zimbler MS, Kokoska MS, Thomas JR. Anatomy and pathophysiology of facial aging. Facial Plast Surg Clin North Am. 2001;9:179–87. vii. [PubMed] [Google Scholar]
- 8.Hamra ST. The role of orbital fat preservation in facial aesthetic surgery. A new concept. Clin Plast Surg. 1996;23:17–28. [PubMed] [Google Scholar]
- 9.Donofrio LM. Fat distribution: A morphologic study of the aging face. Dermatol Surg. 2000;26:1107–12. [PubMed] [Google Scholar]
- 10.Brandt FS, Cazzaniga A. Hyaluronic acid gel fillers in the management of facial aging. Clin Interv Aging. 2008;3:153–9. doi: 10.2147/cia.s2135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Duranti F, Salti G, Bovani B, Calandra M, Rosati ML. Injectable hyaluronic acid gel for soft tissue augmentation. A clinical and histological study. Dermatol Surg. 1998;24:1317–25. doi: 10.1111/j.1524-4725.1998.tb00007.x. [DOI] [PubMed] [Google Scholar]
- 12.Coleman SR. Facial recontouring with lipostructure. Clin Plast Surg. 1997;24:347–67. [PubMed] [Google Scholar]
- 13.Rohrich RJ, Rios JL, Fagien S. Role of new fillers in facial rejuvenation: A cautious outlook. Plast Reconstr Surg. 2003;112:1899–902. doi: 10.1097/01.PRS.0000097307.62862.27. [DOI] [PubMed] [Google Scholar]
- 14.Carruthers J, Carruthers A. A prospective, randomized, parallel group study analyzing the effect of BTX-A (Botox) and nonanimal sourced hyaluronic acid (NASHA, Restylane) in combination compared with NASHA (Restylane) alone in severe glabellar rhytides in adult female subjects: Treatment of severe glabellar rhytides with a hyaluronic acid derivative compared with the derivative and BTX-A. Dermatol Surg. 2003;29:802–9. doi: 10.1046/j.1524-4725.2003.29212.x. [DOI] [PubMed] [Google Scholar]
- 15.Price RD, Berry MG, Navsaria HA. Hyaluronic acid: The scientific and clinical evidence. J Plast Reconstr Aesthet Surg. 2007;60:1110–9. doi: 10.1016/j.bjps.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 16.Tezel A, Fredrickson GH. The science of hyaluronic acid dermal fillers. J Cosmet Laser Ther. 2008;10:35–42. doi: 10.1080/14764170701774901. [DOI] [PubMed] [Google Scholar]
- 17.Solish N, Beer K. Hyaluronic acids: basic science. In: Jones D, editor. Injectable Fillers: Principles and Practice. Oxford: Wiley-Blackwell; 2010. [Google Scholar]
- 18.Muhn C, Rosen N, Solish N, Bertucci V, Lupin M, Dansereau A, et al. The evolving role of hyaluronic acid fillers for facial volume restoration and contouring: A Canadian overview. Clin Cosmet Investig Dermatol. 2012;5:147–58. doi: 10.2147/CCID.S30794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Murray CA, Zloty D, Warshawski L. The evolution of soft tissue fillers in clinical practice. Dermatol Clin. 2005;23:343–63. doi: 10.1016/j.det.2004.09.009. [DOI] [PubMed] [Google Scholar]
- 20.Duffy DM. Complications of fillers: Overview. Dermatol Surg. 2005;31:1626–33. doi: 10.2310/6350.2005.31251. [DOI] [PubMed] [Google Scholar]
- 21.Menon H, Thomas M, D’silva J. Low dose of hyaluronidase to treat over correction by HA filler – A case report. J Plast Reconstr Aesthet Surg. 2010;63:e416–7. doi: 10.1016/j.bjps.2010.01.005. [DOI] [PubMed] [Google Scholar]


