Abstract
Background:
Physiotherapy in the plastic surgery post-operative (PO) is essential to provide means for an adequate and fast recovery as it restores function through the use of physiotherapeutic procedures.
Aim:
The aim of the following study is to verify the effects of the association between the manual lymphatic drainage and the therapeutic ultrasound on pain, oedema and the tissue fibrosis in liposuction and lipoabdominoplasty PO.
Design:
This is a clinical trial prospective.
Materials and Methods:
Eighteen women aged between 18 and 60 years participated in this study, in the late PO period following lipoabdominoplasty or liposuction in the abdomen, flanks and lower trunk, which showed tissue fibrosis of the flanks and abdomen regions. They were divided into two groups: Liposuction group and lipoabdominoplasty group. A total of twelve sessions of therapeutic ultrasound followed by the manual lymphatic drainage were performed. The patients were assessed with regard to pain, oedema and tissue fibrosis in different moments: Initial assessment, during assessment and final assessment through the application of the protocol of evaluation of cysts fibrosis levels.
Statistical Analysis:
The test of equality for two proportions and the confidence interval test for mean to evaluate the distribution of variables. The significance level adopted for statistical tests was 5% (P < 0.05).
Results:
There was a statistically significant reduction of pain, swelling and tissue fibrosis in both groups.
Conclusion:
the association between manual lymphatic drainage and the therapeutic ultrasound reduced the swelling and the tissue fibrosis and made pain disappear in liposuction and lipoabdominoplasty PO period.
KEY WORDS: Oedema, lipectomy, lymphatic system, plastic, surgery, ultrasound therapy
INTRODUCTION
In recent decades, the demand for plastic surgery has gradually increased as well as the concern for the pre-operative and post-operative (PO) periods. Thus, there is an emergence of a concept able to establish a more satisfactory final outcome in plastic surgery not depending only on surgical planning, but also on preoperative and postoperative (PO) care.[1,2,3]
In this context, the Physical Therapy, through improved of its resources and techniques, has been recommended as a form of early and late pre, intermediate and PO treatment, in cosmetic and aesthetic plastic surgeries,[1,3,4] in order to prepare the tissues that will be submitted to surgery, optimize the physical and functional recovery of the function, improve local circulation, prevent, control or minimize the possible PO complications[1,2,3,4] and finally, promote well-being and quality of life.
Physiotherapy in the plastic surgery PO is essential to provide means for an adequate and fast recovery as it restores function through the use of physiotherapeutic procedures, demonstrating the need for physiotherapy in different stages.[1] In addition, the physiotherapist's role is to prevent and/or treat the early and/or late complications, such as: Inflammation with swelling, seroma, hematoma, bruises, pain, wound dehiscence, fibrosis formation, tissue and scarring adhesions and anaesthetic and/or pathological scarring, change in surface sensitivity, body asymmetries, contracture in free grafts, necrosis and infection.[1,5,6]
Swelling and bruises should be reduced as early as possible and it may start even in the early PO period to prevent fibrosis.[4] Fibrosis is the formation of hardened plates in the subcutaneous tissues denoting temporary or definitive irregularities on their surface and affecting affect the body contour.[4,6] From the aesthetic point of view, fibrosis is considered one of the most frequent complications that may interfere negatively and significantly the patient's satisfaction after the surgery.[6]
Therefore, the aim of this study was to investigate the effects of the association between the manual lymphatic drainage and the therapeutic ultrasound on oedema, pain and tissue fibrosis in the liposuction and lipoabdominoplasy PO period.
MATERIALS AND METHODS
This study is a prospective longitudinal clinical trial approved by the Research Ethics Committee of the Universidade Paulista. All the participants agreed to participate in the study and signed the informed consent form.
Eighteen female patients, aged between 18 and 60 years were selected for the study, in the PO period (less T to 1 year — mean: 70,05 days) of liposuction surgery in the abdomen, flanks and lower trunk or lipoabdominoplasty with tissue fibrosis in the flank and abdomen regions. All patients wore the elastic compression garment for 3 months continuously in the PO period.
Exclusion criteria were as follows: The presence of infections and/or acute inflammation, phlebitis, thrombosis or thrombophlebitis, use of pacemaker, hyperthyroidism, cardiopathies, chronic kidney diseases, metaplasias, immune disorders, carotid sinus hypersensitivity; had undergone previous treatments for tissue fibrosis, a history of PO complications such as hematoma, seroma and infection; pregnancy and/or lactation, women in pharmacological and/or clinical for weight loss and aesthetic treatments, aesthetic treatments, and taking a diuretic, steroid and anti-inflammatory drugs.
The patients were divided into 2 groups according to the type of surgery they were submitted to; the liposuction group (LG) (n = 10) and the lipoabdominoplasty group (LAG) (n = 8). Both groups underwent 12 sessions of physiotherapy, 3 times a week, duration of approximately 40 min each, with the application of therapeutic ultrasound technique followed by the manual lymphatic drainage. They were evaluated in three different moments: In pre-intervention, called initial assessment (IA), which was held prior to the beginning of the sessions; after the 6th session of physiotherapy, called during assessment (DA); and in post-intervention, after the twelfth session, the final assessment (FA). All the therapeutic procedure was applied by a single, qualified physical therapist. The patient was placed in a supine position on a stretcher; the therapeutic ultrasound, Sonopulse model III Saphire Line (Ibramed®) was applied. The following parameters were used: Frequency of 3 MHz, continuous mode, intensity of 0.8 W/cm2, power of 2.8 W, direct contact application technique with carbopol gel. The time for the application was calculated specifically for each patient, with the ratio of the treatment area and the effective radiation area being equal to 1.
Subsequently, the technique of manual lymphatic drainage was applied using the Leduc method[7] in the upper and lower abdomen, lower trunk and flanks. The technique initiated with fifteen drainage manoeuvres in the supra-clavicle lymph nodes followed by a sequence of 3 repetitions of diaphragmatic breathing exercises in order to stimulate the activity of ducts and deep lymph trunks. Then, fifteen drainage manoeuvres were applied in the axillary and inguinal lymph nodes. The region to be drained was divided into quadrants, using the reabsorption manoeuvre of the proximal quadrant lymph node chain passing to the next and draining again toward all the adjacent areas and then making the same movement in the corresponding lymph nodes. In liposuction, the umbilical line was used as a parameter in the physiological lymphatic drainage to determine the direction of the inguinal or axillary lymph nodes; for patients submitted to lipoabdominoplasty, the surgical scar was used: Above it for the axillary lymph nodes and below it for the inguinal lymph nodes. In both surgeries, the manual lymph drainage of the upper and lower abdomen was performed with the patient supine; for the lower trunk regions and flanks, the patient sat on the floor.
The AI, AD and AF evaluations were performed by the same qualified evaluator, who was not involved in the research, using the protocol of evaluation of cysts fibrosis levels.[8] This is a validated data collection instrument, which precisely assesses the levels of fibrosis in liposuction or lipoabdominoplasty PO period. It consists of a visual and palpable assessment of pain, oedema and fibrosis.
Pain, swelling and tissue fibrosis were evaluated by their presence or absence: “Yes” (present) and “No” (absent). The fibrosis was specifically quantified in four different levels: Level zero when fibrosis was not identified during the visual and palpable evaluation, in orthostatic, ventral and dorsal decubitus positions; level one (L1), fibrosis is detected only during palpation in ventral and dorsal decubitus; level 2 (L2), fibrosis is observed after visual assessment in orthostatic position, but in the dorsal and ventral decubitus, only after palpation; and level 3 (L3), fibrosis is visually detected in each of the mentioned positions.[6]
The statistical analysis was described in percentage, mean and standard deviation. The test of equality for two proportions and the confidence interval test for mean to evaluate the distribution of variables. The significance level adopted for statistical tests was 5% (P < 0.05).
RESULTS
Initially, the sample comprised 23 patients; however, during the procedures, there was a sample loss of 5 patients because the treatment was interrupted because these patients did not follow the periodicity agreed. Therefore, the study consisted of 18 patients who complained of tissue fibrosis in the abdomen and flanks in the LG or LAG.
The average age was 33.6 years (±6.4); 50% of the women (n = 9) were married, 33.3% (n = 6) were single, 11.1% (n = 2) divorced and 5.6% (n = 1) widows; education level, 44.4% (n = 8) with complete higher education, 44.4% (n = 8) high school and 11.1% (n = 2) elementary school. The results were described according to the groups as previously determined: 44.4% (n = 8) represented the LG and 55.6% (n = 10), the LAG; no statistically significant difference was found between the groups (P = 0.505).
For patients with pain complaints in the LG, there was a statistically significant decrease from IA to FA (P = 0.002) and a trend towards the significance from DA to FA (P = 0.055). In the LAG, a statistically significant decrease was observed only from IA to FA (P = 0.003); however in FA, there was the absence of pain sensation [Figure 1].
Figure 1.
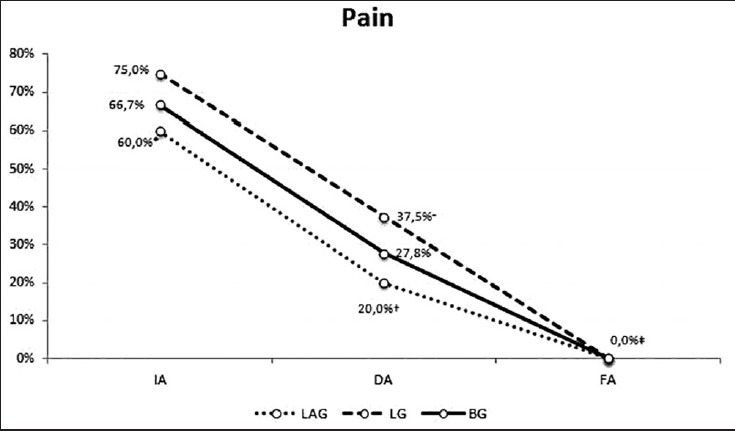
IA, DA and FA values of the LG and LAG groups and BG for the variable pain, IA: Initial assessment; DA: During assessment; FA: Final assessment; LG: Liposuction group; LAG: Lipoabdominoplasty group; BG: Both groups; *= P < 0.05 from IA to DA; †= P < 0.05 from DA to FA; ‡= P < 0.05 from IA to FA
As regards to the presence of oedema in the LG, there was a statistically significant decrease from IA to FA (P = 0.046) and from DA to FA (P = 0.046); in the LAG, there was a statistically significant decrease from IA to DA (P = 0.019) and to FA (P = 0.002). It should be emphasised that in FA, there was oedema in both groups; the LG still had 25% (n = 2) and the LAG 20% (n = 2) of diagnosed oedema [Figure 2].
Figure 2.
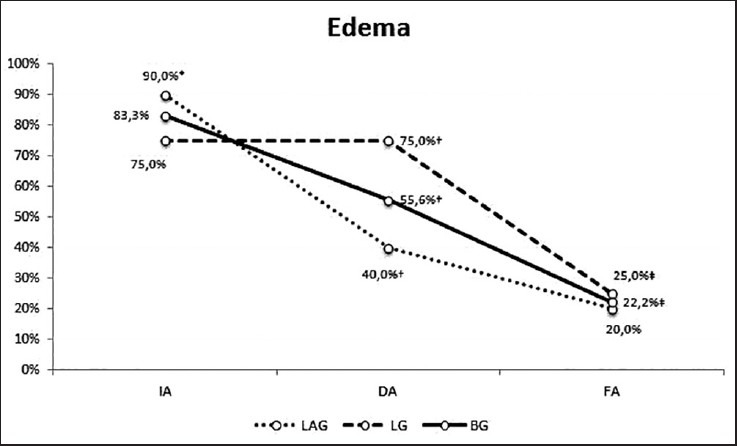
IA, DA and FA values of the LG and LAG groups and the BG for the variable oedema, IA: Initial assessment; DA: During assessment; FA: Final assessment; LG: Liposuction group; LAG: Lipoabdominoplasty group; BG: Both groups; *= P < 0.05 from IA to DA; †= P < 0.05 from DA to FA; ‡= P < 0.05 from IA to FA
And finally, as for the presence of tissue fibrosis, in IA, 100% (n = 18) exhibited tissue fibrosis clinically diagnosed using the protocol of evaluation of cysts fibrosis levels. In the LG, there was a statistically significant decrease from IA to FA (P = 0.007) and from DA to FA (P = 0.007); in the LAG, a statistically significant decrease was observed only from IA to FA (P = 0.010). In FA, the tissue fibrosis was not totally absent in both groups; 37.5% (n = 3) and 50% (n = 5) in the LG and LAG still had tissue fibrosis, respectively; however, evidence showed a lower degree, when compared with that in IA as follows [Figure 3].
Figure 3.
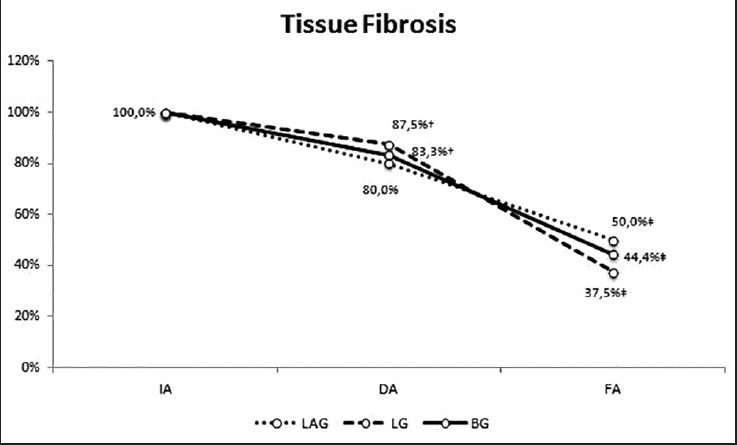
IA, DA and FA values of the LG and LAG groups and the BG for the variable tissue fibrosis, IA: Initial assessment; DA: During assessment; FA: Final assessment; LG: Liposuction group; LAG: Lipoabdominoplasty group; BG: Both groups; †= P < 0.05 from DA to FA; ‡= P < 0.05 from IA to FA
After the detection of tissue fibrosis measured by the protocol of evaluation of cysts fibrosis levels, the values are shown in Table 1. In the LG, the IA showed that 50% (n = 4) were in L3 and the other 50% (n = 4) in L2; the DA showed a decrease of the L3-12.5% (n = 1), 37.5% (n = 3) were in L2 and the other 37.5% (n = 3) in L1; finally, the FA revealed that 37.5% (n = 3) that still had fibrosis were classified into L1, therefore 62.5% (n = 5) did not present any sign of tissue fibrosis.
Table 1.
IA, DA and FA of LG, LAG and BG according to the protocol of evaluation of cysts fibrosis levels
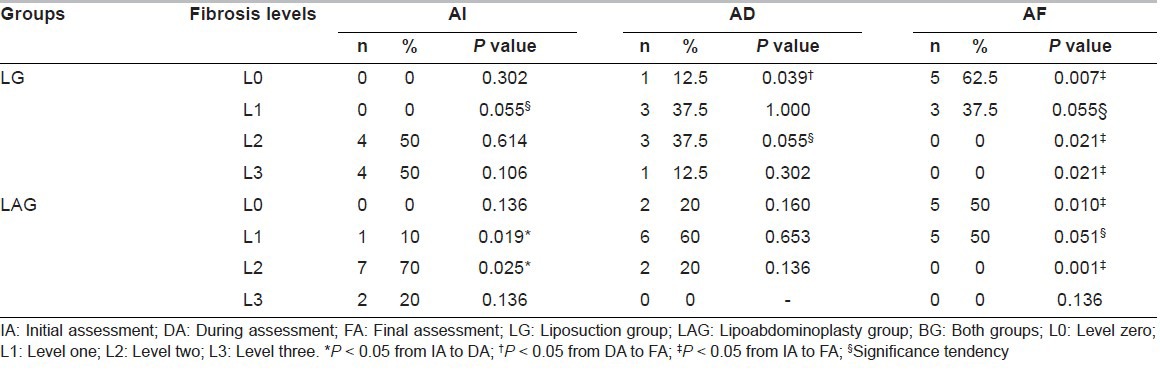
In relation to LAG, the IA showed 20% (n = 2) in L3, 70% (n = 7) in L2 and 10% (n = 1) in L1; in DA, L3 was absent, L2 was reduced to 20% (n = 2) and L1 increased to 60% (n = 6); the FA showed absence of L3 and of L2; thus, 50% (n = 5) were in L1 and the other 50% (n = 5) did not present any sign of tissue fibrosis. In short, the patients who remained with tissue fibrosis, after the proposed procedure, were classified with the lowest degree of tissue fibrosis according to the protocol of evaluation of cysts fibrosis levels; L1, 37.5% (n = 3) in the LG and 50% (n = 5) in the LAG.
DISCUSSION
The growing number of plastic surgeries performed has raised considerable concern about the PO care. Consequently, new fields of expertise are being created to develop some specific techniques to ensure a satisfactory aesthetic outcome.
In the year 2005, a survey was conducted on the knowledge of the physiotherapeutic practice in liposuction surgery by plastic surgeons. This study revealed that doctors recommend the PO care and encourage the use of the manual lymphatic drainage and therapeutic ultrasound during this period as they have subjectively observed that when the manual lymphatic drainage is used, the recovery is faster.[4] Such findings demonstrate the lack of scientific information, denoting the need for reliable and trusted publications based on randomised controlled clinical trials to allow the use of the evidence-based practice[9] not only to help the physiotherapists to make decisions about their daily practices but also to give support so that the physician can evaluate the real needs to refer their patients to the PO care process.
The main focus of this study was to propose a treatment protocol for tissue fibrosis complaints as it is considered the main aesthetic PO complication due to the presence of contour irregularities post liposuction, which may affect significantly the end result and the patient's satisfaction.[4] In addition, there was also a concern about the presence of oedema and pain complaints even in the late PO period of LG and LAG.
Swelling and bruises are expected to reduce as early as possible and may even start in the early PO period to help control the formation of fibrosis.[1,4]
Still, as there remains no consensus on how to best treat tissue fibrosis,[4] the use of manual lymphatic drainage associated with the therapeutic ultrasound was adopted due to the plastic surgeons’ knowledge in the field and because both therapeutic methods can influence the reduction of oedema,[1,10,11,12,13,14,15] promote analgesia and have antifibrotic and fibrinolytic effects.[16,17]
Manual lymphatic drainage is a special type of massage therapy recommended for oedema from different sources, such as: Orthopaedic,[10] abdominoplasty PO,[11] fleboedema,[12] premenstrual oedema,[13] reflex sympathetic dystrophy[14] and fibromyalgia;[15] it is also part of the lymphedema treatment that uses the complex physical therapy proposed by the International Society of Lynphology.[18]
The association between the manual lymphatic drainage and the therapeutic ultrasound provided a statistically significant decrease in oedema and fibrosis and was also able to eliminate pain in both groups.
In the LG and LAG, a gradual decrease of classification levels was observed, specifically in relation to tissue fibrosis. Initially, the LG patients were divided into the highest levels (L2 and L3); and 70% of the LAG patients were classified as L2. After the application of this protocol, 62.5% and 50% of patients from both groups had the fibrosis reduced completely; the remaining ones showed the lowest degree of fibrosis, classified as L1.
All patients exhibited fibrosis in the upper or lower abdomen while 72.2% of them, in the flanks. Subjectively, it can be said that the fibrosis in flanks was eliminated easier.
Satisfactory results were also observed for the swelling and pain variables. Although the swelling still remained, a significant reduction in the LG (IA = 75%, FA = 25%) and in the LAG (IA = 90%, AF = 20%). According to IA, pain was present in 75% of LG patients and 60% in the LAG; it vanished completely in FA, therefore, after the use of this protocol, none of the patients had pain complaints.
All patients were wearing an elastic compression strap. During the study, 66.7% were wearing those, which may have influenced the process of resolution of the fibrosis as they limit the expansion of oedema.
There was no study with direct focus on the effects of the association between the therapeutic ultrasound and the manual lymphatic drainage as a type of treatment for oedema, pain and tissue fibrosis in liposuction and lipoabdominoplasty PO period. Therefore, this is considered the first clinical trial that describes the daily clinical practice of the physiotherapist in the area of plastic surgery.
However, some studies[6,11] that have used the ultrasound therapeutic or the manual lymph drainage in an isolated manner were found. With regard to the therapeutic ultrasound, the tissue fibrosis rates decreased after the use of external therapeutic ultrasound applied on the surface of the area aspirated.[5] It is suggested that the energy emitted by the therapeutic ultrasound favours the dissolution of tissue fibrosis and provides a safe uniformity.[19,20]
In relation to the manual lymphatic drainage, it proved to be more effective than the lymphatic mechanical drainage in the abdominoplasty PO period.[11]
A resource used in plastic surgery post-operatively that has been recently included in the literature is the Endermologie®. It is a mechanical, non-invasive type of massage that is applied using a device that delivers intermittent suction and rolling to the skin and subcutaneous tissue and is also considered an efficient and safe method.[21,22] The use of Endermologie in the liposuction PO period improves the body contouring, reduces body circumference, the tissue irregularities, tissue necrosis, oedema, pain and bruising, due to the increase of local blood and lymphatic flows, promoting the healing of tissues and consequently, providing a better aesthetic result, for the patient's great satisfaction.[6,21,22]
Despite its positive effects on the liposuction PO, there are no studies addressing its use in lipoabdominoplasty and/or abdominoplasty. Therefore, studies should be carried out to prove the effects provided post-operatively by the Endermologie, the physiotherapeutic techniques and other resources. After reviewing the literature, a lack of standardisation was found in respect to the application of therapeutic ultrasound and manual lymphatic drainage, restrict the number of cases, subjective evaluation methods, studies with insufficient scientific evidence published in non-indexed magazines, which makes the knowledge in the area more difficult.
In pre-operative, it is important doing the chest physiotherapy in tummy tuck position helped prevent chest complications.[2]
It is necessary to highlight the difficulty found in the assessment of tissue fibrosis since its result depends on a physical examination (palpation) performed by a qualified professional. In this study, we used the protocol of evaluation of cysts fibrosis levels, a validated instrument, which carefully evaluates the levels of fibrosis and was especially developed to be applied in liposuction or lipoabdominoplasty PO. To obtain reliable results, all assessments were performed by an experienced and independent ratter.
However, further scientific studies in this area are necessary as the existing ones do not allow the comparison of results obtained in the liposuction and lipoabdominoplasty pre- and PO period.
The association between the manual lymphatic drainage and the therapeutic ultrasound reduced swelling and tissue fibrosis and pain-free PO of liposuction and lipoabdominoplasty.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Reidy JP. The relation of physiotherapy to plastic surgery. Phys Med. 1944;37:705–8. doi: 10.1177/003591574403701210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kanjoor JR, Singh AK. Lipoabdominoplasty: An exponential advantage for a consistently safe and aesthetic outcome. Indian J Plast Surg. 2012;45:77–88. doi: 10.4103/0970-0358.96592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Silva DB. A fisioterapia dermato-funcional como potencializadora no pré e pós-operatório de cirurgia plástica. Fisio Terapia. 2001;28:13–5. [Google Scholar]
- 4.Tacani RE, Alegrance FC, Assumpção JD, Gimenes RO. Investigação do encaminhamento médico a tratamentos fisioterapêuticos de pacientes submetidos a lipoaspiração. O Mundo da Saúde. 2005;29:192–8. [Google Scholar]
- 5.Illouz YG. Body contouring by lipolysis: A 5-year experience with over 3000 cases. Plast Reconstr Surg. 1983;72:591–7. doi: 10.1097/00006534-198311000-00001. [DOI] [PubMed] [Google Scholar]
- 6.Kim YH, Cha SM, Naidu S, Hwang WJ. Analysis of postoperative complications for superficial liposuction: A review of 2398 cases. Plast Reconstr Surg. 2011;127:863–71. doi: 10.1097/PRS.0b013e318200afbf. [DOI] [PubMed] [Google Scholar]
- 7.Leduc A, Leduc O. Drenagem linfática: Teoria e prática. Editora Manole. 2007 [Google Scholar]
- 8.Lisboa FL, Meyer PF, Alves DK, Wanderley SC. Protocolo para avaliação fisioterapêuticados níveis de fibrose cicatricial em pós-operatório de lipoaspiração associada ou não à abdominoplastia. Reabilitar. 2003;19:11–8. [Google Scholar]
- 9.Adams S, Farrington M, Cullen L. Evidence into practice: Publishing an evidence-based practice project. J Perianesth Nurs. 2012;27:193–202. doi: 10.1016/j.jopan.2012.03.004. [DOI] [PubMed] [Google Scholar]
- 10.Vairo GL, Miller SJ, McBrier NM, Buckley WE. Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: An evidence-based practice approach. J Man Manip Ther. 2009;17:e80–9. doi: 10.1179/jmt.2009.17.3.80E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Soares LM, Soares SM, Soares AK. Estudo comparativo da eficácia da drenagem linfática manual e mecânica no pós-operatório de dermolipectomia. RBPS. 2005;18:199–204. [Google Scholar]
- 12.Molski P, Ossowski R, Hagner W, Molski S. Patients with venous disease benefit from manual lymphatic drainage. Int Angiol. 2009;28:151–5. [PubMed] [Google Scholar]
- 13.Steiner M. Premenstrual syndrome and premenstrual dysphoric disorder: Guidelines for management. J Psychiatry Neurosci. 2000;25(5):459–68. [PMC free article] [PubMed] [Google Scholar]
- 14.Duman I, Ozdemir A, Tan AK, Dincer K. The efficacy of manual lymphatic drainage therapy in the management of limb edema secondary to reflex sympathetic dystrophy. Rheumatol Int. 2009;29:759–63. doi: 10.1007/s00296-008-0767-5. [DOI] [PubMed] [Google Scholar]
- 15.Ekici G, Bakar Y, Akbayrak T, Yuksel I. Comparison of manual lymph drainage therapy and connective tissue massage in women with fibromyalgia: A randomized controlled trial. J Manipulative Physiol Ther. 2009;32:127–33. doi: 10.1016/j.jmpt.2008.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Kasseroller RG. The Vodder School: The Vodder method. Cancer. 1998;83(12 Suppl American):2840–2. doi: 10.1002/(sici)1097-0142(19981215)83:12b+<2840::aid-cncr37>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 17.Planas J. Prophylactic use of external ultrasound for breast implant capsular contracture. Aesthet Surg J. 2002;22:205–7. doi: 10.1067/maj.2002.123123. [DOI] [PubMed] [Google Scholar]
- 18.International Society of Lymphology. The diagnosis and treatment of peripheral lymphedema. 2009 Concensus Document of the International Society of Lymphology. Lymphology. 2009;42:51–60. [PubMed] [Google Scholar]
- 19.Gasperoni C, Salgarello M, Gasperoni P. External ultrasound used in conjunction with superficial subdermal liposuction: A safe and effective technique. Aesthetic Plast Surg. 2000;24:253–8. doi: 10.1007/s002660010042. [DOI] [PubMed] [Google Scholar]
- 20.Gasperoni C, Salgarello M. The use of external ultrasound combined with superficial subdermal liposuction. Ann Plast Surg. 2000;45:369–73. doi: 10.1097/00000637-200045040-00003. [DOI] [PubMed] [Google Scholar]
- 21.Chang P, Wiseman J, Jacoby T, Salisbury AV, Ersek RA. Noninvasive mechanical body contouring: (Endermologie) a one-year clinical outcome study update. Aesthetic Plast Surg. 1998;22:145–53. doi: 10.1007/s002669900182. [DOI] [PubMed] [Google Scholar]
- 22.Ersek RA, Mann GE, 2nd, Salisbury S, Salisbury AV. Noninvasive mechanical body contouring: A preliminary clinical outcome study. Aesthetic Plast Surg. 1997;21:61–7. doi: 10.1007/s002669900084. [DOI] [PubMed] [Google Scholar]


