Abstract
HIV/AIDS prevalence in South Africa is one of the highest in the world with heterosexual, transmission predominantly promoting the epidemic. The goal of this study is to examine whether, marijuana use and problem drinking mediate the relationship between histories of childhood sexual, abuse (CSA) and HIV risk behaviors among heterosexual men. Participants were 1181 Black men aged, 18–45 from randomly selected neighborhoods in Eastern Cape Province, South Africa. Audio computer assisted, self-interviewing was used to assess self-reported childhood sexual abuse, problem drinking, and marijuana (dagga) use, and HIV sexual transmission behavior with steady and casual partners. Data were analyzed using multiple meditational modeling. There was more support for problem, drinking than marijuana use as a mediator. Findings suggest that problem drinking and marijuana use, mediate HIV sexual risk behaviors in men with histories of CSA. Focusing on men with histories of CSA, and their use of marijuana and alcohol may be particularly useful for designing strategies to reduce, HIV sexual transmission in South Africa.
Keywords: South Africa, Heterosexual, Men, Mediation, Childhood sexual abuse, Problem drinking, Marijuana use, Eastern Cape
HIV/AIDS prevalence in South Africa is one of the highest in the world with heterosexual transmission predominantly promoting the epidemic. Men play a particularly critical role in containing the heterosexual transmission of HIV. Studies show that childhood sexual abuse (CSA) is related to HIV sexual risk behaviors among men and women (Benotsch et al., 2001; O'Leary, Purcell, Remien, & Gomez, 2003; Sweet & Welles, 2012). However, no studies to date have sought to examine the relationship between CSA and sexual transmission risk behavior among a sample comprised exclusively of South African heterosexual men. The present study addresses this gap in the literature.
A meta-analysis of 169 international studies found that lifetime prevalence rates of CSA for females is 25% and for males is 8% (World Health Organization, 2001). A cross-sectional survey of in-school youth in southern African counties in 2003 and 2007 revealed that 19.6% of the female students and 21.1% of the male students aged 11–16 years reported that they had experienced forced or coerced sex (Andersson et al., 2012). Research with rural South African male and female youth in the Eastern Cape found 23.9% of the females and 12.8% of the males reported that they had experienced childhood sexual abuse (Jewkes, Dunkle, Nduna, Jama, & Puren, 2010). The exact prevalence of CSA in the general population is not known as definitions and measures of child sexual abuse differ across studies. Some studies define CSA as the occurrence of some form of direct or indirect physical genital contact experienced by a minor (Andersson et al., 2012; Arreola, Neilands, & Diaz, 2009; Dilorio, Hartwell, Hansen, & Prevention, 2002). Other studies define CSA more broadly to include the sending of electronic sexual images to a minor (Sweet & Welles, 2012). Studies also differ in defining the cut-off age for measuring CSA (Stoltenborgh, van Ijzendoorn, Euser, & Bakermans-Kranenburg, 2011). Measures range from age 13 (Dilorio et al., 2002; Jones et al., 2010; McCarthy, 2010; Wilson, 2010), to more circumscribed criteria, i.e., a sexual experience with a person at least 5 years older than the child if the child was 12 or younger or sexual experience with a person 10 years older if the child was ages 13–16 (Finkelhor, 1979, 2009).
Studies of adults’ reports of CSA have primarily focused on women (Dickson, Herbison, & Paul, 2009; Spiegel, 2003). The limited studies of CSA among men have tended to focus on gay and bisexual men (Jewkes et al., 2010; Purcell, Malow, Dolezal, & Carballo-Dieguez, 2004; Spiegel, 2003). The sparse research on CSA among heterosexual men is based largely on convenience samples (Lloyd & Operario, 2012; Markowitz et al., 2011). Among the few studies utilizing randomly selected samples, Jewkes et al. (2011) found that childhood trauma measured by emotional abuse and neglect, physical abuse and neglect, and sexual abuse, was associated with rape perpetration in South African men. In a large multisite randomized trial of high-risk U.S. men and women, Dilorio et al. (2002) found men with a history of CSA were 1.23 times as likely to report problems with alcohol use. A qualitative study on a small sample investigating CSA in male victims perpetrated by females found substance abuse, suicide, and self-injury among the reported long term effects (Denov, 2004). Other studies report that alcohol and substance abuse, as well as less sexual satisfaction are common among adult men who are victims of CSA (Finkelhor, 1990; Leary & Gould, 2010; Wilsnack, Wilsnack, Kristjanson, Holm-Vogeltanz, & Harris, 2004a).
Recent efforts have been made to identify mediators of the effects of CSA on HIV sexual risk behaviors. Two behaviors in particular, alcohol and marijuana use, have been found to be associated with a history of CSA among adult men and women (Duncan et al., 2008; Howard & Wang, 2005; Wilsnack, Wilsnack, Kristijanson, Holm-Vogeltanz, & Harris, 2004b). Several authors have presented conceptual models theorizing paths through which CSA influences cognitions and attitudes resulting in problem behaviors, including alcohol and drug-related behaviors causing HIV risk behaviors (Miller, 1999; Quina, Morokoff, Harlow, & Zurbriggen, 2004). Benotsch et al. (2001) tested, in a sample of self-identified gay and bisexual men, several possible mediators, including substance use and trauma-related anxiety. They reported that men who had been sexually abused in childhood or adulthood exhibited more symptoms of substance use than did other men. A study by O'Leary and colleagues (2003) found a history of CSA to be significantly associated with unprotected anal sex in a sample of HIV-positive men who have sex with men (MSM) in the US, and found this relationship to be mediated by suicidality (receptive anal intercourse), and hostility (insertive anal intercourse).
Numerous researchers have investigated the relationship between HIV sexual risk behaviors and the use of drugs or alcohol among CSA adult victims. Zierler et al. (1991), investigating the causes of transmission of HIV in a sample of women and men who volunteered for a testing and counseling program, found that survivors of CSA used alcohol or tranquilizers 70–80% more than participants not reporting CSA. Studies also show heterosexual men who reported CSA are more likely to use alcohol before sex and to have more sexual partners (Schraufnagel, Davis, George, & Norris, 2010).
The present study
Research indicates that CSA predicts adult involvement in HIV sexual risk behaviors, including unprotected sexual intercourse and sex with multiple partners (Brennan, Hellerstedt, Ross, & Welles, 2007; Koenig, Doll, O'Leary, & Pequegnat, 2004; Lloyd & Operario, 2012). Studies also reveal relationships between CSA and alcohol and substance use. Although the literature suggests that problem drinking and marijuana use are associated with CSA, an understanding of the causal pathways through which these problem behaviors operate to influence HIV sexual risk behaviors is incomplete. Understanding the mechanisms influencing HIV sexual risk behaviors among adult victims of CSA are best explored via mediation analysis (Baron & Kenny, 1986; Hayes and Preacher, 2008). We empirically tested whether associations between CSA and HIV sexual risk behaviors are mediated through problem drinking and marijuana use among Black South African men who have sex with women.
Method
Participants
Institutional review board (IRB) #8 at the University of Pennsylvania, which was the designated IRB under the federal wide assurance of the University of Pennsylvania and the University of Fort Hare, reviewed and approved this study. The participants were residents of townships near East London in Eastern Cape Province, South Africa, including Mdantsane, Scenery Park, Duncan Village, and Gompo Town, and the semi-rural area of Berlin who completed a baseline questionnaire as part of a neighborhood-based health promotion intervention trial.
As reported elsewhere (Jemmott et al., 2013), participants enrolled in the trial during a 25-month period beginning in November 2007. Before recruiting from a neighborhood, research team members met with community leaders to enlist their support. We then held a meeting to inform men about the study and advertised it using posters and other materials. Using geographical clusters tied to census data in the catchment area matched-pairs of neighborhoods were randomly selected. We recruited men at different hours of the day and days of the week at a variety of venues (e.g., taxi ranks, shebeens [people's homes that are dedicated to alcohol sale and drinking], marketplaces) to reach a diversity of men. Men aged 18–45 years who lived in a selected neighborhood, reported vaginal intercourse in the previous 3 months, did not report plans to relocate beyond a reasonable distance from the study site within the next 15 months, and had a photo ID were eligible. We employed audio computer-assisted self-interviewing (ACASI), which provided both audio and video presentation of the questions and response options on a laptop computer to collect data.
Measures
The measures, which had been pilot tested with over 250 men, were available in isiXhosa (following translation and back translation from English), English, and a combination of isiXhosa (audio) and English (visual). We assessed condom use outcomes separately for steady partners (a woman with whom they had a romantic relationship for at least 6 months) and casual partners. Condom use was assessed as the proportion of condom-protected acts of vaginal intercourse within the last three months, condom use at last vaginal intercourse, and the frequency of condom use during vaginal and anal intercourse, rated on a 5-point scale from 1 never to 5 always. The condom use measures were selected because they are widely used in HIV/STD risk-reduction intervention trials (Crosby et al., 2009; El-Bassel et al., 2010; Jemmott, 3rd, Jemmott, Fong, & Morales, 2010; Kalichman et al., 2007). We used the 4-item CAGE (Cutting down, Annoyance by criticism, Guilty feeling, and Eye-openers) questionnaire (Ewing, 1984), as a continuous variable to assess problem alcohol consumption (alpha = 0.73). We measured marijuana use with the question, how many days in the past month the man had smoked dagga (marijuana). Childhood sexual abuse was measured as the mean response to five binary items used in HIV/STD risk-reduction intervention trials (El-Bassel et al., 2010): Before you were 16 years of age, did anyone have intercourse with you against your will; did anyone force you to lick or suck her vagina or his penis; did anyone put his or her mouth on your penis against your will; did anyone force you to put your finger or an object in her vagina; did anyone put his penis or an object in your bottom or behind or rectum? Participants also completed measures of sociodemographic variables, theoretical mediator variables, health promotion behaviors, and mediators that will be examined in future articles.
We took several steps to increase the validity of self-report measures that have been used in previous HIV/STD risk-reduction intervention studies (Jemmott, 3rd, Jemmott, Braverman, & Fong, 2005; Jemmott et al., 2005; Jemmott, 3rd, Jemmott, & Fong, 1992, 1998; Jemmott, 3rd, et al., 2010; Jemmott, Jemmott, & O'Leary, 2007). To reduce problems in memory, we asked respondents to recall sexual behaviors over a relatively brief period (i.e., 90 days), wrote the dates comprising that period on a whiteboard, and gave them calendars clearly highlighting the dates. We emphasized the importance of responding honestly, informing them that their responses would be used to create programs for South African men like themselves. We assured participants we would keep their responses confidential. The use of ACASI may also serve to increase participants’ motivation to respond accurately (Hewett, Mensch, & Erulkar, 2004; Johnson, Fendrich, & Mackesy-Amiti, 2010; Metzger et al., 2000).
Data analysis
Correlations were performed to establish the relationship between CSA and sexual behavior. Chi-square and t-tests were used to determine if there was a statistically significant difference between men who experienced CSA and men who did not experience CSA for each of the HIV sexual risk behaviors of interest.
Mediation analysis
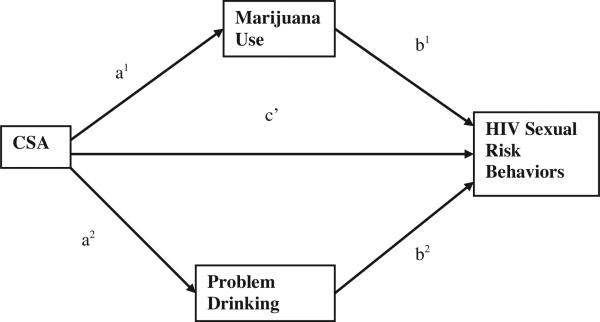
To address the question of what influence childhood sexual abuse has on HIV sexual risk behaviors through problem drinking and marijuana use, mediation analyses were conducted controlling for age using a single multiple mediation method (Hayes and Preacher, 2008). Fig. 1 depicts the mediation model and shows our hypothesis of how CSA (independent variable) was distributed into its indirect effect on specific HIV sexual risk behaviors (dependent variables) through the two mediators, problem drinking and marijuana use, and its direct effect on specific HIV sexual risk behaviors (path c′). The relationships between CSA and the two mediators, marijuana use and problem drinking are represented through paths a1 and a2. The effects of the two mediators on the specific HIV sexual risk behaviors are represented in paths b1 and b2. The total indirect effect of CSA on each HIV sexual risk behavior is the sum of the indirect effects of the two mediators Σ(a1 b1 + a2 b2). Testing a single multiple mediation model rather than separate simple mediation models offers several advantages. Adding up the indirect effects in several simple mediation analyses to obtain the total indirect effect could result in bias, as multiple mediators are typically intercorrelated (Preacher and Hayes, 2008b). Additionally, a single multiple mediation model allows us to determine to what extent a specific variable mediates an effect between an independent and dependent variable, conditional on the presence of other mediators. It also reduces the likelihood of parameter bias resulting from omitting mediators. Furthermore, it allows us to determine the relative magnitude of the specific effects associated with all mediators (Hayes and Preacher, 2008; Preacher and Hayes, 2008a).
Fig. 1.
Illustration of mediation model.
Controlling for age, we analyzed CSA as an independent variable to estimate its direct association with each HIV sexual transmission behavior, path c′. We estimated the associations between CSA and problem drinking and marijuana use (path a) and the associations between problem drinking and marijuana use and each HIV sexual risk behavior (path b). All outcomes were binary variables; therefore associations were tested with logistic regression models. The indirect or meditational effects were calculated using the product of the unstandardized paths (a × b). Pairwise contrasts were conducted to test whether indirect effects of the two mediators were equal in size. Bias-corrected accelerated (BCa) bootstrapping with 5000 replications was used to obtain asymptotic 95% confidence intervals (CIs) around the indirect effects (Table 2). Analyses were conducted using SPSS 20 and an SPSS macro developed by Hayes (2008).
Table 2.
Unstandardized coefficients (standard error), p values, and Bias Corrected and Accelerated (Bca) Confidence Intervals (CI) for analyses of mediators of the relations of childhood sexual abuse to HIV sexual risk behaviors.
| Dependent variable/mediators | Effect ofchild abuse on mediator (a) | Effect of mediator on HIV sexual risk variables (b) | Direct effect of child abuse on HIV sexual risk variables (c') | Indirect effect of child abuse on HIV sexual risk variables through mediators Σ(a1b1 + a2b2) | BCa 95% CI of mediated effects |
|
|---|---|---|---|---|---|---|
| Lower | Upper | |||||
| Unprotected vaginal sex with steady partner | ||||||
| Marijuana use | 3.29 (1.69) | .011 (.007) | .040 (.034) | –.004 | .147 | |
| 0.052 | 0.096 | |||||
| Problem drinking | .221 (.070) | .419 (.161) | .095 (.048) | .018 | .215 | |
| <0.001 | 0.009 | |||||
| Both mediators | .007 (.386) | .135 (.057) | .036 | .260 | ||
| 0.984 | ||||||
| Unprotected vaginal sex with casual partners | ||||||
| Marijuana use | 3.29 (1.69) | .019 (.008) | .065 (.044) | .001 | .200 | |
| 0.052 | 0.010 | |||||
| Problem drinking | .222 (.070) | .674 (.210) | .150 (.065) | .029 | .269 | |
| 0.001 | 0.001 | |||||
| Both mediators | 1.51 (.425) | .215 (.079) | .040 | .320 | ||
| <0.001 | ||||||
| Multiple steady partner vaginal sex | ||||||
| Marijuana use | 3.30 (1.69) | .014 (.007) | .049 (.042) | –.001 | .173 | |
| 0.050 | 0.053 | |||||
| Problem drinking | .221 (.070) | .547 (.194) | .124 (.060) | .031 | .280 | |
| 0.002 | 0.005 | |||||
| Both mediators | 1.52 (.408) | .173 (.070) | .060 | .335 | ||
| 0.002 | ||||||
| Multiple casual partners vaginal sexual | ||||||
| Marijuana use | 3.27 (1.69) | .007 (.008) | .020 (.033) | –.020 | .123 | |
| 0.050 | 0.402 | |||||
| Problem drinking | .221 (.070) | .547 (.202) | .121 (.060) | .035 | .272 | |
| 0.002 | <0.001 | |||||
| Both mediators | 1.21 (423) | .143 (.067) | .044 | .307 | ||
| 0.004 | ||||||
| Unprotected anal sex with steady partner | ||||||
| Marijuana use | 3.54 (1.79) | .017 (.012) | .065 (.068) | –.014 | .347 | |
| 0.049 | 0.142 | |||||
| Problem drinking | .250 (.076) | .497 (.331) | .124 (.090) | –.014 | .337 | |
| 0.001 | 0.133 | |||||
| Both mediators | 2.37 (.578) | .188 (.103) | .014 | .436 | ||
| <0.001 | ||||||
| Unprotected anal sex with a causal partner | ||||||
| Marijuana use | 2.580 (1.80) | .032 (.015) | .0845 (.080) | –.008 | .340 | |
| 0.153 | 0.029 | |||||
| Problem drinking | .235 (.075) | .821 (.464) | .199 (.125) | .002 | .488 | |
| 0.002 | 0.076 | |||||
| Both mediators | 2.52 (.682) | .284 (.150) | .0387 | .626 | ||
| 0.002 | ||||||
| Multiple steady partner anal sex | ||||||
| Marijuana use | 3.54 (1.79) | .042 (.014) | .155 (.108) | .007 | .466 | |
| 0.049 | 0.002 | |||||
| Problem drinking | .250 (.076) | 1.44 (.478) | .373 (.164) | .108 | .753 | |
| 0.001 | 0.002 | |||||
| Both mediators | 2.66 (.681) | .532 (.182) | .193 | .909 | ||
| 0.001 | ||||||
| Multiple casual partner anal sex | ||||||
| Marijuana use | 2.58 (1.80) | .018 (.015) | .046 (.064) | –.027 | .276 | |
| 0.153 | 0.228 | |||||
| Problem drinking | .235 (.076) | .579 (.450) | .146 (.126) | –.061 | .435 | |
| 0.002 | 0.198 | |||||
| Both mediators | 1.92 (.736) | .192 (.131) | ||||
| <.001 | ||||||
Results
Table 1 gives basic demographic information and information on the variables of interest for all participants and participants with and without a history of CSA. Of the 1181 participants, 247 (20.9%) reported histories of CSA. The men ranged in age from 18 to 45 years (M = 26.7, SD = 6.61). Only 5.8% were married, but 80% had a steady partner. Table 1 shows that men with a history of CSA were slightly younger (M = 25.6, SD = 6.05) than the men who did not report a history of childhood sexual abuse (M = 26.9, SD = 6.77) (p = 0.007). About half (48.2%) of the men who had not experienced CSA reported having a casual sex partner in 90 days, as compared with more than half (61.5%) of the men with histories of CSA (p < 0.001). Men who reported CSA history reported on average a larger number of days in using marijuana (M = 5.43, SD = 9.42) compared with men who did not report a history of CSA (M = 4.19, SD = 8.74) (p = 0.026). Men with a history of CSA were significantly more likely to report vaginal sex with multiple steady partners (33.2% vs. 21.5%, p < 0.001), more likely to report having unprotected anal sex with a steady partner (13.1% vs. 5.4%, p < 0.001), and more likely to report having anal sex with multiple steady partners (9.1% vs. 2.8%, p < 0.001) compared with men who did not reported CSA. Men who reported a history of CSA were significantly more likely to report having unprotected vaginal sex with a casual partner (27.1% vs. 16.8%, p < 0.001), vaginal sex with multiple casual partners (27.1% vs. 19%, p < 0.005), unprotected anal sex with a casual partner (7.1% vs. 3.1%, p < 0.001), and anal sex with multiple casual partners (8.1% vs. 2.8%, p < 0.001) than men with no reported CSA histories.
Table 1.
Sociodemographic characteristics of men reporting Childhood Sexual Abuse (CSA) or No CSA, Eastern Cape Providence, South Africa 2007-2009.
| Variable | Total | CSA history | No CSA | p value |
|---|---|---|---|---|
| Agea | 26.7 ± 6.61 | 25.6 ± 6.05 | 26.9 ± 6.77 | 0.007 |
| Completed High School | 518/1181 (43.9%) | 91/247 (36.8%) | 427/934 (45.7%) | 0.014 |
| Unemployed | 793/1181 (67.1%) | 225/247(91.1%) | 855/934 (92.0%) | 0.798 |
| Marriedb | 67/1114 (5.7%) | 14/247(5.7%) | 54/934 (5.9%) | 0.946 |
| Steady Partner last 90 daysb | 945/1181 (80.2%) | 189/247(76.5%) | 758/934 (81.2%) | 0.104 |
| Casual Partner last 90 daysb | 602/1181 (51.0%) | 152/247 (61.5%) | 450/934 (48.2%) | <0.001 |
| Problem Drinkingb | 902/1181 (76.4%) | 208/247 (84.2%) | 694/934 (74.3%) | 0.001 |
| Marijuana (dagga) use in last 30 daysa | 4.46 ± 8.9 | 5.43 ± 9.42 | 4.19 ± 8.74 | 0.026 |
| Unprotected Vaginal Sex Steady Partner | 558/1181 (47.3%) | 119/247 (48.1%) | 439/934 (47.0%) | 0.742 |
| Unprotected Vaginal Sex Casual Partnerb | 226/1180 (19.2%) | 66/247 (27.1%) | 160/933 (16.8%) | <0.001 |
| Vaginal Sex Multiple Steady Partnerb | 282/1177 (24.0%) | 82/247 (33.2%) | 200/930 (21.5%) | <0.001 |
| Vaginal Sex Multiple Casual Partnerb | 245/1178 (19.2%) | 68/247 (27.1%) | 177/931 (19.0%) | 0.005 |
| Unprotected Anal Sex with a Steady Partnerb | 78/1124 (6.9%) | 29/222 (13.1%) | 49/903(5.4%) | <0.001 |
| Unprotected Anal Sex with a Causal Partnerb | 41/1059 (3.9%) | 15/212 (7.1%) | 26/848(3.1%) | 0.006 |
| Anal Sex Multiple Steady Partnerb | 45/1124 (4.0%) | 20/221 (9.1%) | 25/903 (2.8%) | <0.001 |
| Anal Sex Multiple Casual Partnerb | 41/1059 (3.9%) | 17/212 (8.1%) | 24/848 (2.8%) | <0.001 |
| Ever had insertive anal sex with a male | 26/1181 (2.2%) | 16/247 (6.5%) | 10/934 (1.1%) | <0.001 |
| Ever had receptive anal sex with a male | 10/934 (1.1%) | 10/247 (4%) | 6/934 (.6%) | <0.001 |
Values summarized are means ± SD with corresponding p-values from t-tests.
Values summarized are n(%) with corresponding p-values from Chi-Square tests.
As shown in Table 2, behaviors that were significantly predicted by both mediators included unprotected vaginal sex with casual partners, having vaginal sex with multiple steady and casual partners, unprotected anal sex with steady and casual partners, and having anal sex with multiple steady and casual partners. None of the pairwise contrasts was statistically significant, which indicates that the magnitudes of the indirect effects of marijuana and problem drinking did not differ significantly.
Discussion
Findings suggest that problem drinking and marijuana use mediate HIV sexual risk behaviors in men who reported experiencing CSA. A significant indirect relationship was observed between experiencing CSA, problem drinking and marijuana use, and unprotected vaginal sex with a casual partner, vaginal sex with multiple steady and casual partners, unprotected anal sex with steady and causal partners, and anal sex with multiple steady or casual partners. Marijuana use and problem drinking did not have a significant indirect effect on the relationship between experiences of childhood sexual abuse and unprotected vaginal sex with a steady partner. The higher rates of CSA reported by men in this study compared to CSA rates for males globally (World Health Organization, 2001) may result from our use of ACASI which has been found to increase participants’ motivation to respond accurately (Metzger et al., 2000).
From the sociodemographic data several implications appear. We found that younger men were more likely to report CSA than were older men, which may result from the difficulties older men experience in acknowledging that they had experienced CSA. Men with a history of CSA were also found to be less likely to have completed high school. This finding is consistent with the literature that shows poor educational achievement to be a negative consequence of CSA (Boden, Horwood, & Fergusson, 2007; Buckle, Lancaster, Powell, & Higgins, 2005). The findings that a significantly higher percentage of men who had experienced CSA reported having a casual partner in the last 90 days is also consistent with the literature (Duncan et al., 2008; Hayatbakhsh et al., 2007). Consistent with our findings, other studies have shown higher rates of multiple partners among men with CSA histories compared with men without CSA histories (Dilorio et al., 2002; Holmes, Foa, & Sammel, 2005). It should also be noted that, consistent with the literature, men who reported CSA were significantly more likely to engage in all of the HIV sexual risk behaviors (Dilorio et al., 2002; O'Cleirigh, Safren, & Mayer, 2012; Markowitz et al., 2011; Pence et al., 2012; Wilson, 2010; Zierler et al., 1991).
Studies of heterosexual men in the Unites States show men are more likely to use condoms with their casual partners (Catania et al., 1992; Hunt, Myers, & Dyche, 1999). We found however problem drinking and marijuana use to significantly affect HIV sexual risk behaviors for both casual and steady partners of men with histories of CSA. Notwithstanding this finding, we also observed marijuana and problem drinking to have a greater effect on HIV sexual risk behaviors of CSA men and their causal partners than steady partners. The findings between men's risk behaviors with causal and steady partners provide some insights into the complexities of the relationships between marijuana use, problem drinking, and HIV sexual risk behaviors among men who have experienced CSA and the need for further research.
This is perhaps the first study to examine the effects of problem drinking and marijuana use on the HIV sexual risk behaviors in a large randomly selected sample of men in South Africa who have sex with women. Studies of CSA reported by adult males have primarily been conducted in Europe and North America among bisexual and gay men or both heterosexual men and women (Finkelhor, 1994; Markowitz et al., 2011; Pereda, Guilera, Forns, & Gómez-Benito, 2009).
Strengths of this study include the large sample comprised exclusively of men who have sex with women recruited from randomly selected neighborhoods in a high-level heterosexual epidemic and the use of ACASI with questions heard in isiXhosa and displayed in English. The reliance on self-reports of behavior is a limitation. Additionally, while the nature of the sample afforded a unique opportunity to learn about the effects of problem drinking and marijuana use among South African men with histories of CSA in the Eastern Cape, the findings may not generalize to all South African men.
In conclusion, this study examined whether problem drinking and marijuana use mediate the relation between CSA and HIV sexual risk behavior in heterosexual men. Problem drinking and marijuana use mediated the relations of history of childhood sexual abuse to unprotected vaginal sex with casual sexual partners, having multiple sexual partners, and having unprotected anal sex with a steady or casual sexual partner. The findings have implications for HIV prevention practitioners and researchers. Studies suggest difference in men's risk behaviors for casual and steady partners. However, the findings suggest that interventions are needed to dissuade HIV transmission behaviors among men with histories of CSA irrespective of their sexual partner. Intervention targeting men with histories of CSA could reduce heterosexual transmission in South Africa.
Acknowledgments
The authors appreciate the contributions of Craig Carty, MS, Janet Hsu, BA, Loretta S. Jemmott, PhD, Shasta Jones, PhD, Monde Makiwane, PhD, Xoliswa Mtose, PhD, Pretty Ndyebi, BA, Zolani Ngwane, PhD, Lulama Sidloyi, BA, and Thomas Ten Have, PhD. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. The results and discussion in this paper reflect the views of the authors and not necessarily official views of the Centers for Disease Control and Prevention. The corresponding author, Professor Larry D. Icard had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention. This study was funded by research grant 1 R01 HD053270 from the National Institutes of Health.
References
- Andersson N, Paredes-Solis S, Milne D, Omer K, Marokoane N, Laetsang D, Cockcroft A. Prevalence and risk factors for forced or coerced sex among school-going youth: National cross-sectional studies in 10 southern African countries in 2003 and 2007. BMJ Open. 2012;2:e000754. doi: 10.1136/bmjopen-2011-000754. http://dx.doi.org/10.1136/bmjopen-2011-000754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arreola SG, Neilands TB, Diaz R. Childhood sexual abuse and the sociocultural context of sexual risk among adult Latino gay and bisexual men. American Journal of Public Health. 2009;99:S432–S438. doi: 10.2105/AJPH.2008.138925. http://dx.doi.org/10.2105/Ajph.2008.138925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baron R, Kenny D. The moderator-mediator variables distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Benotsch E, Rompa D, Gore-Felton C, Austin J, Luke W, DiFonzo K, Simpson DS. Unwanted sexual experiences and sexual risks in gay and bisexual men: Associations among revictimization, substance use, and psychiatric symptoms. Journal of Sex Research. 2001;38:9. [Google Scholar]
- Boden JM, Horwood LJ, Fergusson DM. Exposure to childhood sexual and physical abuse and subsequent educational achievement outcomes. Child Abuse & Neglect. 2007;31:1101–1114. doi: 10.1016/j.chiabu.2007.03.022. http://dx.doi.org/10.1016/j.chiabu.2007.03.022. [DOI] [PubMed] [Google Scholar]
- Brennan DJ, Hellerstedt WL, Ross MW, Welles SL. History of childhood sexual abuse and HIV risk behaviors in homosexual and bisexual men. American Journal of Public Health. 2007;97:1107–1112. doi: 10.2105/AJPH.2005.071423. http://dx.doi.org/10.2105/Ajph.2005.071423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buckle SK, Lancaster S, Powell MB, Higgins DJ. The relationship between child sexual abuse and academic achievement in a sample of adolescent psychiatric inpatients. Child Abuse & Neglect. 2005;29:1031–1047. doi: 10.1016/j.chiabu.2004.12.013. http://dx.doi.org/10.1016/j.chiabu.2004.12.013. [DOI] [PubMed] [Google Scholar]
- Catania JA, Coates TJ, Stall R, Turner H, Peterson J, Hearst N, Dolcini MM, Hudes E, Gagnon J, Wiley J, Groves R. Prevalence of AIDS-related risk factors and condom use in the United States [Research Support, U.S. Gov't, P. H. S.]. Science. 1992;258(5085):1101–1106. doi: 10.1126/science.1439818. [DOI] [PubMed] [Google Scholar]
- Crosby R, DiClemente RJ, Charnigo R, Snow G, Troutman A. A brief, clinic-based, safer-sex intervention for heterosexual African American men newly diagnosed with an STD: A randomized controlled trial. American Journal of Public Health. 2009;99:S96–S103. doi: 10.2105/AJPH.2007.123893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Denov MS. The long-term effects of child sexual abuse by female perpetrators: A qualitative study of male and female victims [Reports – Evaluative]. Journal of Interpersonal Violence. 2004;19:1137–1156. doi: 10.1177/0886260504269093. [DOI] [PubMed] [Google Scholar]
- Dickson N, Herbison P, Paul C. Child sexual abuse and persistence of risky sexual behaviors and negative sexual outcomes over adulthood: Findings from a birth cohort. Child Abuse & Neglect. 2009;33:12. doi: 10.1016/j.chiabu.2008.09.006. http://dx.doi.org/10.1016/j.chiabu.2008.09.006. [DOI] [PubMed] [Google Scholar]
- Dilorio C, Hartwell T, Hansen N, Prevention NMH. Childhood sexual abuse and risk behaviors among men at high risk for HIV infection. American Journal of Public Health. 2002;92:214–219. doi: 10.2105/ajph.92.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan AE, Sartor CE, Scherrer JF, Grant JD, Heath AC, Nelson EC, Bucholz KK. The association between cannabis abuse and dependence and childhood physical and sexual abuse: Evidence from an offspring of twins design. Addiction. 2008;103:990–997. doi: 10.1111/j.1360-0443.2008.02210.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Bassel N, Jemmott JB, Landis JR, Pequegnat W, Wingood GM, Wyatt GE, Bellamy SL. National Institute of Mental Health Multisite Eban HIV/STD prevention intervention for African American HIV serodiscordant couples: A cluster randomized trial. Archives of Internal Medicine. 2010;170:1594–1601. doi: 10.1001/archinternmed.2010.261. http://dx.doi.org/10.1001/archinternmed.2010.261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ewing J. Detecting alcoholism: The CAGE questionnaire. Journal of the American Medical Association. 1984;252:1905–1907. doi: 10.1001/jama.252.14.1905. [DOI] [PubMed] [Google Scholar]
- Finkelhor D. What's wrong with sex between adults and children? Ethics and the problem of sexual abuse. American Journal of Orthopsychiatry. 1979;49:692–697. doi: 10.1111/j.1939-0025.1979.tb02654.x. [DOI] [PubMed] [Google Scholar]
- Finkelhor D. Early and long-term effects of child sexual abuse: An update. Professional Psychology: Research and Practice. 1990;21:325–330. http://dx.doi.org/10.1037/0735-7028.21.5.325. [Google Scholar]
- Finkelhor D. Current information on the scope and nature of child sexual abuse [Information Analyses]. Future of Children. 1994;4:31–53. [PubMed] [Google Scholar]
- Finkelhor D. The prevention of childhood sexual abuse. Future of Children. 2009;19:169–194. doi: 10.1353/foc.0.0035. [DOI] [PubMed] [Google Scholar]
- Hayatbakhsh MR, Najman JM, Jamrozik K, Mamun AA, Alati R, Bor W. Cannabis and anxiety and depression in young adults: A large prospective study [Reports – Research]. Journal of the American Academy of Child & Adolescent Psychiatry. 2007;46:408. doi: 10.1097/chi.0b013e31802dc54d. [DOI] [PubMed] [Google Scholar]
- Hayes AF. [August 6, 2011];Indirect. 2008 From http://www.afhayes.com/spss-sas-and-mplus-macros-and-code.html.
- Hayes AF, Preacher KJ. Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior Research Methods. 2008;40:13. doi: 10.3758/brm.40.3.879. http://dx.doi.org/10.3758/brm.40.3.879. [DOI] [PubMed] [Google Scholar]
- Hewett PC, Mensch BS, Erulkar AS. Sexually Transmitted Infections. Suppl. 2. Vol. 80. U.S. Gov't; 2004. Consistency in the reporting of sexual behaviour by adolescent girls in Kenya: A comparison of interviewing methods. pp. i43–i48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holmes WC, Foa EB, Sammel MD. Men's pathways to risky sexual behavior: Role of co-occurring childhood sexual abuse, posttraumatic stress disorder, and depression histories. Journal of Urban Health. 2005;82(1 (Suppl. 1)):i89–i99. doi: 10.1093/jurban/jti028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Howard DE, Wang MQ. Psychosocial correlates of U.S. adolescents who report a history of forced sexual intercourse. Journal of Adolescent Health. 2005;36:372–379. doi: 10.1016/j.jadohealth.2004.07.007. http://dx.doi.org/10.1016/j.jadohealth.2004.07.007. [DOI] [PubMed] [Google Scholar]
- Hunt W, Myers H, Dyche M. Living with risk: Male partners of HIV-positive women. Cultural Diversity Ethnic Minorith Psychology. 1999;5:10. [Google Scholar]
- Jemmott JB, 3rd, Jemmott LS, Braverman PK, Fong GT. HIV/STD risk reduction interventions for African American and Latino adolescent girls at an adolescent medicine clinic: A randomized controlled trial. [Clinical Trial Randomized Controlled Trial Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. Archives of Pediatrics & Adolescent Medicine. 2005;159:440–449. doi: 10.1001/archpedi.159.5.440. http://dx.doi.org/10.1001/archpedi.159.5.440. [DOI] [PubMed] [Google Scholar]
- Jemmott JB, 3rd, Jemmott LS, Fong GT. Reductions in HIV risk-associated sexual behaviors among black male adolescents: Effects of an AIDS prevention intervention. [Clinical Trial Randomized Controlled TrialResearch Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. American Journal of Public Health. 1992;82:372–377. doi: 10.2105/ajph.82.3.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott JB, 3rd, Jemmott LS, Fong GT. Abstinence and safer sex HIV risk-reduction interventions for African American adolescents: A randomized controlled trial. Journal of the American Medical Association. 1998;279:1529–1536. doi: 10.1001/jama.279.19.1529. [DOI] [PubMed] [Google Scholar]
- Jemmott JB, 3rd, Jemmott LS, Fong GT, Morales KH. Effectiveness of an HIV/STD risk-reduction intervention for adolescents when implemented by community-based organizations: A cluster-randomized controlled trial. American Journal of Public Health. 2010;100:720–726. doi: 10.2105/AJPH.2008.140657. http://dx.doi.org/10.2105/AJPH.2008.140657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemmott JB, 3rd., Jemmot LS, O'leary A, Ngwane Z, Icard LD, Heeren GA, Carty C. Neighborhood-based randomized controlled trial of an HIV/ST risk-reduction intervention for South African Men. American Journal of Public Health. 2013 [in press] [Google Scholar]
- Jemmott LS, Jemmott JB, 3rd, O'Leary A. Effects on sexual risk behavior and STD rate of brief HIV/STD prevention interventions for African American women in primary care settings. [Randomized Controlled Trial Research Support, N.I.H., Extramural]. American Journal of Public Health. 2007;97:1034–1040. doi: 10.2105/AJPH.2003.020271. http://dx.doi.org/10.2105/AJPH.2003.020271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Dunkle K, Nduna M, Jama PN, Puren A. Associations between childhood adversity and depression, substance abuse and HIV and HSV2 incident infections in rural South African youth. Child Abuse & Neglect. 2010;34:833–841. doi: 10.1016/j.chiabu.2010.05.002. http://dx.doi.org/10.1016/j.chiabu.2010.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jewkes R, Sikweyiya Y, Morrell R, Dunkle K. PLOS ONE. Vol. 6. ARTN; 2011. Gender inequitable masculinity and sexual entitlement in rape perpetration South Africa: Findings of a cross-sectional study. p. e29590. http://dx.doi.org/10.1371/journal.pone.0029590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson TP, Fendrich M, Mackesy-Amiti ME. Computer literacy and the accuracy of substance use reporting in an ACASI survey. Social Science Computer Review. 2010;28:515–523. [Google Scholar]
- Jones DJ, Runyan DK, Lewis T, Litrownik AJ, Black MM, Wiley T, Nagins DS. Trajectories of childhood sexual abuse and early adolescent HIV/AIDS risk behaviors: The role of other maltreatment, witnessed violence, and child gender. Journal of Clinical Child & Adolescent Psychology. 2010;39:667–680. doi: 10.1080/15374416.2010.501286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Simbayi LC, Vermaak R, Cain D, Jooste S, Peltzer K. HIV/AIDS risk reduction counseling for alcohol using sexually transmitted infections clinic patients in Cape Town, South Africa. Journal of Acquired Immune Deficiency Syndromes. 2007;44(5):594–600. doi: 10.1097/QAI.0b013e3180415e07. http://dx.doi.org/10.1097/QAI.0b013e3180415e07. [DOI] [PubMed] [Google Scholar]
- Koenig LJ, Doll L, O'Leary SA, Pequegnat W. From child sexual abuse to adult sexual risk: Trauma, revictimization, and intervention. 1st ed. American Psychological Association; Washington, DC: 2004. [Google Scholar]
- Lloyd S, Operario D. HIV risk among men who have sex with men who have experienced childhood sexual abuse: Systematic review and meta-analysis. AIDS Education and Prevention. 2012;24:228–241. doi: 10.1521/aeap.2012.24.3.228. [DOI] [PubMed] [Google Scholar]
- Markowitz SM, O'Cleirigh C, Hendriksen ES, Bullis JR, Stein M, Safren SA. Childhood sexual abuse and health risk behaviors in patients with HIV and a history of injection drug use. AIDS and Behavior. 2011;15:1554–1560. doi: 10.1007/s10461-010-9857-y. http://dx.doi.org/10.1007/S10461-010-9857-Y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy JA. Internet sexual activity: A comparison between contact and non-contact child pornography offenders. Journal of Sexual Aggression. 2010;16:14. [Google Scholar]
- Metzger DS, Koblin B, Turner C, Navaline H, Valenti F, Holte S, Gross M, Sheon A, Miller H, Gooley P, Seage G. Randomized controlled trial of audio computer-assisted self-interviewing: Utility and acceptability in longitudinal studies. HIVNET Vaccine Preparedness Study Protocol Team. American Journal of Epidemiology. 2000;152:99–106. doi: 10.1093/aje/152.2.99. [DOI] [PubMed] [Google Scholar]
- Miller M. A model to explain the relationship between sexual abuse and HIV risk among women. [Research Support, U.S. Gov't, P.H.S.]. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV. 1999;11:3–20. doi: 10.1080/09540129948162. http://dx.doi.org/10.1080/09540129948162. [DOI] [PubMed] [Google Scholar]
- O'Leary A, Purcell D, Remien RH, Gomez C. Childhood sexual abuse and sexual transmission risk behaviour among HIV-positive men who have sex with men. AIDS Care-Psychological and Socio-Medical Aspects of AIDS/HIV. 2003;15:17–26. doi: 10.1080/0954012021000039725. http://dx.doi.org/10.1080/0954012021000039725. [DOI] [PubMed] [Google Scholar]
- O'Leary N, Gould N. Exploring coping factors amongst Men who were sexually abused in childhood. British Journal of Social Work. 2010;40:2669–2686. [Google Scholar]
- O'Cleirigh C, Safren SA, Mayer KH. The pervasive effects of childhood sexual abuse: Challenges for improving HIV prevention and treatment interventions. Journal of Acquired Immune Deficiency Syndromes: JAIDS. 2012;59:331–334. doi: 10.1097/QAI.0b013e31824aed80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pence BW, Mugavero MJ, Carter TJ, Leserman J, Thielman NM, Raper JL, Proeschold-Bell RJ, Reif S, Whetten K. Childhood trauma and health outcomes in HIV-infected patients: An exploration of causal pathways. [Research Support, N.I.H., Extramural]. Journal of Acquired Immune Deficiency Syndromes. 2012;59:409–416. doi: 10.1097/QAI.0b013e31824150bb. http://dx.doi.org/10.1097/QAI.0b013e31824150bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pereda N, Guilera G, Forns M, Gómez-Benito J. The international epidemiology of child sexual abuse: A continuation of Finkelhor (1994). Child Abuse & Neglect. 2009;33(6):331–342. doi: 10.1016/j.chiabu.2008.07.007. http://dx.doi.org/10.1016/j.chiabu.2008.07.007. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Hayes AF. Contemporary approaches to assessing mediation in communication research. In: Hayes AF, Slater MD, Snyder LB, editors. The Sage sourcebook of advanced data analysis methods for communication research. Sage Publications; Los Angeles: 2008a. pp. 13–55. [Google Scholar]
- Preacher KJ, Hayes AF. Contemporary approaches to assessing mediation in communication research. In: Hayes AF, Slater MD, Snyder LB, editors. The Sage sourcebook of advanced data analysis methods for communication research. Sage; Los Angeles: 2008b. [Google Scholar]
- Purcell DW, Malow RM, Dolezal C, Carballo-Dieguez A. Sexual abuse of boys: Short and long term associations and implications for HIV prevention. In: Koenig LJ, Doll L, O'Lary SA, Pequegnat W, editors. From child sexual abuse to adult sexual risk: Trauma, revictimization, and intervention. American Psychological Association; Washington, DC: 2004. p. 21. [Google Scholar]
- Quina K, Morokoff PJ, Harlow LL, Zurbriggen EL. Cognitive and additudinal paths from childhood trauma to adult HIV Risk. In: Koenig LJ, Doll L, O'Lary SA, Pequegnat W, editors. From child sexual abuse to adult sexual risk: Trauma, revictimization, and intervention. American Psychological Association; Washington, DC: 2004. p. 27. [Google Scholar]
- Schraufnagel TJ, Davis KC, George WH, Norris J. Childhood sexual abuse in males and subsequent risky sexual behavior: A potential alcohol-use pathway. Child Abuse & Neglect. 2010;34:369–378. doi: 10.1016/j.chiabu.2009.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spiegel J. Sexual abuse of males: The SAM model of theory and practice. Brunner-Routledge; New York: 2003. [Google Scholar]
- Stoltenborgh M, van Ijzendoorn MH, Euser EM, Bakermans-Kranenburg MJ. A global perspective on child sexual abuse: Meta-analysis of prevalence around the world. [Comparative Study Meta-Analysis Research Support, Non-U. S. Gov't]. Child Maltreatment. 2011;16:79–101. doi: 10.1177/1077559511403920. http://dx.doi.org/10.1177/1077559511403920. [DOI] [PubMed] [Google Scholar]
- Sweet T, Welles SL. Associations of sexual identity or same-sex behaviors with history of childhood sexual abuse and HIV/STI risk in the United States. Journal of Acquired Immune Deficiency Syndromes: JAIDS. 2012;59:400–408. doi: 10.1097/QAI.0b013e3182400e75. [DOI] [PubMed] [Google Scholar]
- Wilsnack SC, Wilsnack RW, Kristijanson AF, Holm-Vogeltanz ND, Harris TR. Child sexual abuse and alcohol use among women: Setting the stage for risky sexual behavior. In: Koenig LJ, Doll L, O'Leary SA, Pequegnat W, editors. From child sexual abuse to adult sexual risk: Trauma, revictimization, and intervention. American Psychological Association; Washington, DC: 2004. p. 20. [Google Scholar]
- Wilsnack SC, Wilsnack RW, Kristjanson AF, Holm-Vogeltanz ND, Harris TR. Child sexual abuse and alcohol use among women: Setting the stage for risky behavior. In: Koenig LJ, Doll L, O'Leary SA, Pequegnat W, editors. From child sexual abuse to adult sexual risk: Trauma, revictimization, and intervention. 1st ed. American Psychological Association; Washington, DC: 2004. pp. 181–200. [Google Scholar]
- Wilson DR. Health consequences of childhood sexual abuse. Perspectives in Psychiatric Care. 2010;46:56–64. doi: 10.1111/j.1744-6163.2009.00238.x. [DOI] [PubMed] [Google Scholar]
- World Health Organization . Comparative risk assessment: Child Sexual Abuse. Sydney, Australia: 2001. [Google Scholar]
- Zierler S, Feingold L, Laufer D, Velentgas P, Kantrowitz-Gordon I, Mayer K. Adult survivors of childhood sexual abuse and subsequent risk of HIV infection. American Journal of Public Health. 1991;81:572–575. doi: 10.2105/ajph.81.5.572. [DOI] [PMC free article] [PubMed] [Google Scholar]