Abstract
Cytotoxic treatments for cancer remain highly toxic, expensive, and variably efficacious. Many chemotherapy regimens are never directly compared in randomized clinical trials (RCTs); as a result, the vast majority of guideline recommendations are ultimately derived from human expert opinion. We introduce an automated network meta-analytic approach to this clinical problem, with nodes representing regimens and edges direct comparison via RCT(s). A chemotherapy regimen network is visualized for the primary treatment of chronic myelogenous leukemia (CML). Node and edge color, size, and opacity are all utilized to provide additional information about the quality and strength of the depicted evidence. Historical versions of the network are also created. With this approach, we were able to compactly compare the results of 17 CML regimens involving RCTs of 9700 patients, representing the accumulation of 45 years of evidence. Our results closely parallel the recommendations issued by a professional guidelines organization, the National Comprehensive Cancer Network (NCCN). This approach offers a novel method for interpreting complex clinical data, with potential implications for future objective guideline development.
Keywords: Computing methodologies, Numerical Analysis, Computer-Assisted, Data Interpretation, Statistical, Medical Informatics Applications
Introduction
Conventional systematic review and meta-analysis are aggregating approaches with a goal of making unifying conclusions based upon multiple independent studies [1]. The traditional meta-analytic approach is generally limited by the requirement that the comparator arms and outcome measures are the same, e.g. progression free survival (PFS) on drug A to PFS on drug B [2]. The traditional meta-analytic approach is challenged by complex scenarios, such as the treatment of cancer, where multiple treatment options with disparate measures of outcome have been tested over the years. In parallel with this increase in complexity, the issuance of clinical management guidelines has increased dramatically over the past years and decades. Most guidelines are derived from collaborations of clinical experts and are therefore subject to subjective interpretation of data. Furthermore, guidelines must be constantly updated due to introductions of new evidence; one published estimate of guideline “half-life” is only 5.5 years [3].
Several approaches have been suggested to meet the need of rigorous objective comparison of multiple treatments used in a common context. These approaches are generally referred to as “network meta-analyses”. Network meta-analysis evaluates multiple treatments and determines the relationships among them, offering a powerful objective solution to this complicated medical need, despite considerable methodological challenges [4, 5]. In this paper, we propose a simplified approach to the construction and display of a meta-analytic network for chemotherapy regimens, with a goal of conveying maximum information about the quality of outcome comparisons, the comparative value of particular regimens, and the relevance of older published regimens to contemporary practice.
Materials and Methods
Pilot Use Case
To demonstrate our proposed approach, we selected a condition with a relatively limited number of commonly used treatments, chronic myelogenous leukemia (CML). We limited our evaluation to published randomized clinical trials (RCTs) investigating primary (first-line) treatments of newly-diagnosed chronic-phase CML. These were first identified through a curated database of chemotherapy regimens at HemOnc.org (http://hemonc.org), a hematology/oncology wiki actively maintained by physicians. The publications identified were manually searched to identify further regimens; a PubMed query for the Medical Subject Headings (MeSH) “Leukemia, Myelogenous, Chronic, BCR-ABL Positive” and “Randomized Controlled Trial [Publication Type]” was also conducted. The results of this analysis were compared to the recommendations provided by the NCCN Guidelines® [6].
Graph Attributes
A network graph was subsequently created, with v vertices corresponding to substantively identical chemotherapy regimens and l edges connecting regimens which were directly compared in the published RCTs. When more than one RCT compared the same regimens, edges were duplicated. Vertices were depicted as circular nodes, and edges as solid lines. The network layout was first automatically determined using the Kamada-Kawai force-based algorithm, with subsequent manual modification to maximize readability [7]. In order to enhance the information value of the graph, the appearance of the nodes and edges was enhanced in a systematic way, as follows:
Node Size and Coloration
Nodes were automatically sized proportionally to the total number of patients who received the specified regimen. Nodes were colored using a gradated three-color system, with red connoting an inferior treatment regimen, green a superior treatment regimen, and yellow a treatment regimen of equivocal value. This value, was calculated by holding a series of m “contests” with the immediately adjacent vertices, based on the published outcome findings. The three possible outcomes E of each contest are:
Win (E = 1): superiority, as defined by an improved outcome with p-value ≤0.05.
Lose (E = −1): inferiority, as defined by an inferior outcome with p-value ≤0.05.
Tie (E = 0): either an outcome with a non-significant p-value or an equivalent outcome as defined by formal non-inferiority, with p-value ≤0.05.
E was further multiplied by a “relative value measure” RV, representing the quality of the measured outcome: 1.0 for a weak surrogate measure (e.g. response rate); 1.25 for a strong surrogate measure (e.g. PFS); 1.5 for overall survival. Finally, the average of the sum of the products of these values was multiplied by the logarithm of the total patients in all contests involving the vertex, as shown in Equation (1):
| (1) |
Nodes with negative were automatically colored in the red range, gradating towards yellow for about zero, and towards the green range for positive .
Edge Width and Coloration
Edge width was automatically sized proportionate to the number of patients being compared across the two treatment regimen vertices for the uniquely referent RCT. If more than one RCT compared the same regimens, the width of each duplicate edge was determined independently. Edges were also colored on a three-color scale, without gradation, to reflect the quality of the measured outcome, which was determined manually: red for weak surrogates (e.g. response rate); yellow for strong surrogates (e.g. PFS); green for overall survival.
Node and Edge Aging Effects
In order to convey information about how recently a regimen was formally evaluated, transparency was automatically assigned to older nodes and edges, using the alpha opacity channel. Edges were assigned initial alpha of 1.0 and decayed by 0.1/year to a minimum of 0.2, based upon the “survival analysis” by Shojania et al [3]. Nodes were also assigned initial alpha of 1.0 and decayed in a similar fashion; however, nodes were refreshed to an alpha of 1.0 whenever a new RCT was published which involved the node.
Node alpha was also varied with significant perturbations of the network. Specifically, when new evidence caused one or more extant nodes to change value (from green/superior to red/inferior, or vice versa), the alpha of all nodes immediately adjacent to the changed node was automatically refreshed to 1.0. This effect was carried over to the legend, so that nodes determined to be aged (those with low alpha) were faintly displayed, and thus considered to be “outdated” regimens.
Historical Representation of Meta-Analytic Network
In order to create the enhancements described above, it was necessary to temporally develop the network, beginning with the first year of publication and proceeding to the most recent year. As a result, visualization of changes in evidence over time was possible.
General Considerations
The analysis was undertaken using the R statistical programming language (http://www.r-project.org/). iGraph, a freely available package for R and other applications, was used for graph visualization (http://igraph.sourceforge.net/).
Results
We identified 24 RCTs comparing at least two treatments for newly-diagnosed CML, with n=17 substantively identical regimens [8-31]. These are shown chronologically in Table 1. A total of 9700 patients were enrolled across all trials.
Table 1. Summary of RCTs.
| Author (year) | Regimen 1 | Regimen 2 | |
|---|---|---|---|
| Witts et al. (1968) | Busulfan | Radiation | |
| Canellos et al. (1975) | Busulfan | DBM | |
| Silver et al. (1987) | Busulfan | DBM | |
| Hehlmann et al. (1993) | Busulfan | Hydrea | |
| Tura et al. (1994) | Busulfan | Hydrea | IFNA |
| Hehlmann et al. (1994) | Busulfan | Hydrea | IFNA |
| Allan et al. (1995) | Busulfan | Hydrea | |
| Busulfan/IFNA | Hydrea/IFNA | ||
| Ohnishi et al. (1995) | Busulfan | IFNA | |
| Guilhot et al. (1997) | IFNA | IFNA/LoDAC | |
| Baccarani et al. (2002) | IFNA | IFNA/LoDAC | |
| Kuhr et al. (2003) | Hydrea/IFNA | IFNA/LoDAC | |
| O’Brien et al. (2003) | IFNA/LoDAC | Imatinib | |
| Ohnishi et al. (2004) | IFNA | MRD allo-SCT | |
| Olsson et al. (2004) | Busulfan | Hydrea | |
| Deenik et al. (2007) | IFNA/HiDAC | IFNA/LoDAC | |
| Baccarani et al. (2009) | Imatinib | Imatinib-HD | |
| Cortes et al. (2010) | Imatinib | Imatinib-HD | |
| Kantarjian et al. (2010) | Dasatinib | Imatinib | |
| Preudhomme et al. (2010) | Imatinib | Imatinib-HD | |
| Imatinib/IFNA | Imatinib/LoDAC | ||
| Saglio et al. (2010) | Imatinib | Nilotinib | |
| Hehlmann et al. (2011) | Imatinib | Imatinib- HD |
Imatinib/ IFNA |
| Simonsson et al. (2011) | IFNA/Imatinib | Imatinib | |
| Cortes et al. (2012) | Bosutinib | Imatinib | |
| Radich et al. (2012) | Dasatinib | Imatinib | |
DBM: dibromomannitol; Hydrea: hydroxyurea; IFNA: interferon-α; Lo/HiDAC: low-/high-dose cytarabine; MRD allo-SCT: matched related donor allogeneic stem cell transplant; HD: high dose
Imatinib and busulfan were the most highly connected treatment regimens, with degree of 13 in both cases. Five treatments (29%) were singly connected to the network. Additional graph measures are shown in Figure 1.
Figure 1. Graph summary statistics, over time. Vertical axes are logarithmic for both panels. In the right panel, total number of patients is normalized to 100 (year 2012).
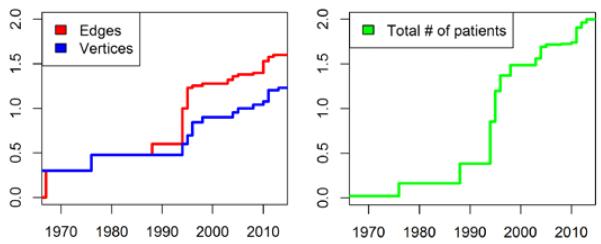
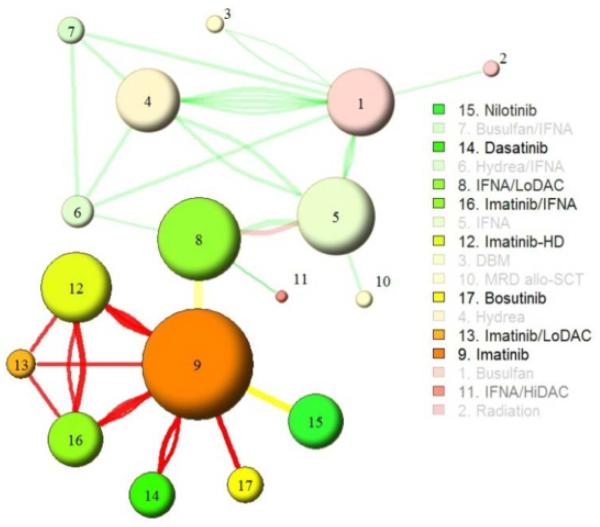
Figure 2 shows the enhanced graph for the year 2012.
Figure 2. CML primary treatment network analysis, 2012.
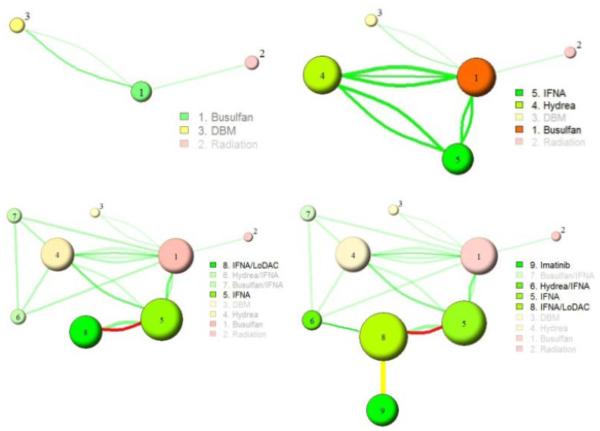
Figure 3 shows four historical representations of the graph. Between 1992 and 1994 (top panels), two new treatments were introduced, and the older “superior” treatment (busulfan) transitioned to an “inferior” status. Between 2002 and 2003 (bottom panels) evidence for imatinib was introduced, and it rose to the top of the “superior” treatment options.
Figure 3. Historic CML primary treatment network analyses for the years 1992, 1994, 2002, 2003.
An animated movie of the graph evolution from 1968 to 2012 is freely available at http://hemonc.org/docs/CMLhistory.avi. The R code is freely available upon request.
Discussion and Conclusion
Several notable conclusions can be made by examining the modern and historical meta-analytic network graphs. First, there is a clear inflection point in the mid-1990’s, after which the number of regimens, clinical trials, and clinical trial participants increased rapidly (Figure 1). Second, overall survival was substituted by surrogate outcomes from 2003 onwards, reflecting the radical improvement in prognosis of CML. While this is welcome news, the general decrease in the quality of the outcome evidence makes interpretation of the modern RCTs more difficult [32]. Third, several distinct “paradigm shifts” can be discerned, based upon the phenomenon of over-turning of previously superior treatment regimens: busulfan in 1994, hydroxyurea in 1995, and imatinib in 2010.
In terms of concordance with the most recent NCCN Guidelines®, our two most superior (and current) regimens, nilotinib and dasatinib, are recommended; the guidelines also suggest consideration of interferon-α for patients intolerant of tyrosine kinase inhibitors (TKI’s) [6]. Imatinib, which is ranked as an inferior regimen in Figure 2, continues to be recommended by the NCCN. Notably, this recommendation hinges primarily on the assertion that imatinib has shown a definitive long-term survival advantage, which is based on historical comparisons, not RCTs (the seminal IRIS trial of imatinib vs. interferon-α/low-dose cytarabine experienced a crossover rate of 90%, making long-term comparisons unreliable) [33, 34]. Because our analysis only includes RCTs, this information is not present in the visualization. This decision to include only high levels of evidence was intentional, although future work will focus on methods of inclusion of historical and contemporaneous comparative effectiveness data.
The treatment for chronic-phase CML has evolved through several eras, which are captured effectively by the modern and historical graphs. In the first era, conventional chemotherapy was the only option; several trials in the early 1990’s established the superiority of hydroxyurea to the standard treatment since the 1940’s, busulfan. From the mid-1990’s, improved mortality was observed with the introduction of interferon-α, ushering in the so-called “interferon era.” The IRIS trial in 2003 led to the “imatinib era,” as shown in Figure 3, lower right panel [19]. Most recently, a series of 2nd and 3rd generation TKI’s, as well as combinations of imatinib with other drugs, have begun to usher in the “post-imatinib era” [35]. Of note, a curative treatment has been available through most of these eras: allogeneic stem cell transplant [36]. As Figure 2 demonstrates, this treatment has rarely been compared against others in a randomized fashion.
There are several important limitations to the current approach. As with any meta-analysis, the results should be interpreted cautiously, since the study populations may differ significantly and publication bias may be present. Additionally, we simplified the valuing of vertices considerably by introducing a win/lose/tie schema, which does not measure the magnitude of outcomes. Future work will explore direct incorporation of outcome magnitudes into the model. We also did not adjust vertex value by indirect comparisons but rather elected to let aged nodes “outdate” through a fading process, with the implications that regimens that have not been studied for some time are unlikely to be a part of current practice. There are clearly exceptions to this rule, such as a regimen whose utility was proven beyond a doubt many years ago. Future work will investigate ways of resolution of these exceptions, as well as application of inheritance rules to the graph. Multiple regimens can contain the same drug(s) and conveyance of this information will require further refinement. Finally, this visualization includes neither comparative effectiveness data nor the other two components of quality measurement: toxicity and cost. In order to make fully informed decisions about optimal treatment strategy, this information is usually taken under consideration; its inclusion in the automated network analysis will also be the focus of future work.
In conclusion, we have demonstrated a new approach to the analysis and visualization of complex clinical data, which does not rely on subjective human interpretation. In the example of primary treatment of CML, the constructed hierarchy closely parallels that developed by human expert consensus. Our method is generalizable and should therefore work with more complicated disease phenotypes and contexts, such as the adjuvant treatment of breast cancer. Once more broadly validated, this automated method has the potential to augment or replace the current approach to guideline development.
Acknowledgments
Funding: NIH grants 5R21DA025168-02 (GA), 1R01HG004836-01 (GA), and 4R00LM009826-03 (GA).
References
- [1].Jones DR. Meta-analysis: weighing the evidence. Statistics in Medicine. 1995;14(2):137–49. doi: 10.1002/sim.4780140206. [DOI] [PubMed] [Google Scholar]
- [2].Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151(4):W65–94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]
- [3].Shojania KG, Sampson M, Ansari MT, Ji J, Doucette S, Moher D. How quickly do systematic reviews go out of date? A survival analysis. Ann Intern Med. 2007;147(4):224–33. doi: 10.7326/0003-4819-147-4-200708210-00179. [DOI] [PubMed] [Google Scholar]
- [4].Li T, Puhan MA, Vedula SS, Singh S, Dickersin K. Network meta-analysis-highly attractive but more methodological research is needed. BMC Med. 2011;9:79. doi: 10.1186/1741-7015-9-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Mills EJ, Ioannidis JP, Thorlund K, Schunemann HJ, Puhan MA, Guyatt GH. How to use an article reporting a multiple treatment comparison meta-analysis. JAMA. 2012;308(12):1246–53. doi: 10.1001/2012.jama.11228. [DOI] [PubMed] [Google Scholar]
- [6].The National Comprehensive Cancer Network [accessed 2012 December 3rd];NCCN Clinical Practice Guidelines in Oncology: Chronic Myelogenous Leukemia Version 3.2013. Available from: www.nccn.org.
- [7].Kamada T, Kawai S. An algorithm for drawing general undirected graphs. Information Processing Letters. 1989:7–15. [Google Scholar]
- [8].Canellos GP, Young RC, Neiman PE, DeVita VT., Jr Dibromomannitol in the treatment of chronic granulocytic leukemia: a prospective randomized comparison with busulfan. Blood. 1975;45(2):197–203. [PubMed] [Google Scholar]
- [9].Silver RT, Mick R, Cooper R, Ellison RR, Levy R, Brunner K, Schwartz JM, Holland JF. A comparative study of dibromomannitol and busulfan in the treatment of chronic myeloid leukemia. A study of cancer and leukemia group B. Cancer. 1987;60(7):1442–8. doi: 10.1002/1097-0142(19871001)60:7<1442::aid-cncr2820600706>3.0.co;2-w. [DOI] [PubMed] [Google Scholar]
- [10].Witts LJ, Blackburn EK, Callender ST, Dacie JV, Davidson WM, Doll R, Easson EC, Fountain JR, Hardisty RM, Hayhoe GJ, Holman CA, Jacobs A, Pike MC, Sacker LS, Scott RB, Thompson RB, Wetherly-Mein G, Galton DAG. Chronic granulocytic leukaemia: comparison of radiotherapy and busulphan therapy. Report of the Medical Research Council’s working party for therapeutic trials in leukaemia. BMJ. 1968;1(5586):201–8. doi: 10.1136/bmj.1.5586.201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Ohnishi K, Ohno R, Tomonaga M, Kamada N, Onozawa K, Kuramoto A, Dohy H, Mizoguchi H, Miyawaki S, Tsubaki K, Miura Y, Omine M, Kobayashi T, Naoe T, Ohshima T, Hirashima K, Ohtake S, Takahashi I, Morishima Y, Naito K, Asou N, Tanimoto M, Sakuma A, Yamada K. A randomized trial comparing interferon-alpha with busulfan for newly diagnosed chronic myelogenous leukemia in chronic phase. Blood. 1995;86(3):906–16. [PubMed] [Google Scholar]
- [12].Allan NC, Richards SM, Shepherd PC. UK Medical Research Council randomised, multicentre trial of interferon-alpha n1 for chronic myeloid leukaemia: improved survival irrespective of cytogenetic response. The UK Medical Research Council’s Working Parties for Therapeutic Trials in Adult Leukaemia. Lancet. 1995;345(8962):1392–7. doi: 10.1016/s0140-6736(95)92596-1. [DOI] [PubMed] [Google Scholar]
- [13].Hehlmann R, Heimpel H, Hasford J, Kolb HJ, Pralle H, Hossfeld DK, Queisser W, Loffler H, Hochhaus A, Heinze B. Randomized comparison of interferon-alpha with busulfan and hydroxyurea in chronic myelogenous leukemia. The German CML Study Group. Blood. 1994;84(12):4064–77. [PubMed] [Google Scholar]
- [14].Tura S, Baccarani M, Zuffa E, Russo D, Fanin R, Zaccaria A, Fiacchini M. Interferon alfa-2a as compared with conventional chemotherapy for the treatment of chronic myeloid leukemia. The Italian Cooperative Study Group on Chronic Myeloid Leukemia. N Engl J Med. 1994;330(12):820–5. doi: 10.1056/NEJM199403243301204. [DOI] [PubMed] [Google Scholar]
- [15].Hehlmann R, Heimpel H, Hasford J, Kolb HJ, Pralle H, Hossfeld DK, Queisser W, Loffler H, Heinze B, Georgii A, Wussow PV, Bartram C, Griesshammer L, Bergmann L, Essers U, Falge C, Hochhaus A, Queisser W, Sick C, Meyer P, Schmitz N, Verpoort K, Eimermacher H, Walther F, Westerhausen M, Kleeberg UR, Heilein A, Kabisch A, Barz C, Zimmerman R, Meuret G, Tichelli A, Berdel WE, Kanz L, Anger B, Tigges FJ, Schmid L, Brockhaus W, Zankovich R, Schlafer U, Weissenfels I, Mainzer K, Tobler A, Perker M, Hohnloser J, Messener D, Thiele J, Buhr T, Ansari H. Randomized comparison of busulfan and hydroxyurea in chronic myelogenous leukemia: prolongation of survival by hydroxyurea. The German CML Study Group. Blood. 1993;82(2):398–407. [PubMed] [Google Scholar]
- [16].Guilhot F, Chastang C, Michallet M, Guerci A, Harousseau JL, Maloisel F, Bouabdallah R, Guyotat D, Cheron N, Nicolini F, Abgrall JF, Tanzer J. Interferon alfa-2b combined with cytarabine versus interferon alone in chronic myelogenous leukemia. French Chronic Myeloid Leukemia Study Group. N Engl J Med. 1997;337(4):223–9. doi: 10.1056/NEJM199707243370402. [DOI] [PubMed] [Google Scholar]
- [17].Baccarani M, Rosti G, de Vivo A, Bonifazi F, Russo D, Martinelli G, Testoni N, Amabile M, Fiacchini M, Montefusco E, Saglio G, Tura S. A randomized study of interferon-alpha versus interferon-alpha and low-dose arabinosyl cytosine in chronic myeloid leukemia. Blood. 2002;99(5):1527–35. doi: 10.1182/blood.v99.5.1527. [DOI] [PubMed] [Google Scholar]
- [18].Kuhr T, Burgstaller S, Apfelbeck U, Linkesch W, Seewann H, Fridrik M, Michlmayr G, Krieger O, Lutz D, Lin W, Pont J, Kock L, Abbrederis K, Baldinger C, Buder R, Geissler D, Hausmaninger H, Lang A, Zabernigg A, Duba C, Hilbe W, Eisterer W, Fiegl M, Greil R, Gastl G, Thaler J. A randomized study comparing interferon (IFN alpha) plus low-dose cytarabine and interferon plus hydroxyurea (HU) in early chronic-phase chronic myeloid leukemia (CML) Leuk Res. 2003;27(5):405–11. doi: 10.1016/s0145-2126(02)00223-0. [DOI] [PubMed] [Google Scholar]
- [19].O’Brien SG, Guilhot F, Larson RA, Gathmann I, Baccarani M, Cervantes F, Cornelissen JJ, Fischer T, Hochhaus A, Hughes T, Lechner K, Nielsen JL, Rousselot P, Reiffers J, Saglio G, Shepherd J, Simonsson B, Gratwohl A, Goldman JM, Kantarjian H, Taylor K, Verhoef G, Bolton AE, Capdeville R, Druker BJ. Imatinib compared with interferon and low-dose cytarabine for newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2003;348(11):994–1004. doi: 10.1056/NEJMoa022457. [DOI] [PubMed] [Google Scholar]
- [20].Ohnishi K, Ino A, Kishimoto Y, Usui N, Shimazaki C, Ohtake S, Taguchi H, Yagasaki F, Tomonaga M, Hotta T, Ohno R. Multicenter prospective study of interferon alpha versus allogeneic stem cell transplantation for patients with new diagnoses of chronic myelogenous leukemia. Int J Hematol. 2004;79(4):345–53. doi: 10.1532/ijh97.03160. [DOI] [PubMed] [Google Scholar]
- [21].Olsson-Stromberg U, Simonsson B, Ahlgren T, Bjorkholm M, Carlsson K, Gahrton G, Hast R, Lofvenberg E, Linder O, Ljungman P, Malm C, Paul C, Rodjer S, Turesson I, Uden AM, Wahlin A, Killander A, Wadman B, Westin J, Vikrot O, Zettervall O, Oberg G. Comparison of busulphan, hydroxyurea and allogeneic bone marrow transplantation (BMT) in chronic myeloid leukaemia: BMT prolongs survival. Hematol J. 2004;5(6):462–6. doi: 10.1038/sj.thj.6200552. [DOI] [PubMed] [Google Scholar]
- [22].Deenik W, van der Holt B, Verhoef GE, Schattenberg AV, Verdonck LF, Daenen SM, Zachee P, Westveer PH, Smit WM, Wittebol S, Schouten HC, Lowenberg B, Ossenkoppele GJ, Cornelissen JJ. High-vs low-dose cytarabine combined with interferon alfa in patients with first chronic phase chronic myeloid leukemia. A prospective randomized phase III study. Ann Hematol. 2007;86(2):117–25. doi: 10.1007/s00277-006-0186-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Baccarani M, Rosti G, Castagnetti F, Haznedaroglu I, Porkka K, Abruzzese E, Alimena G, Ehrencrona H, Hjorth-Hansen H, Kairisto V, Levato L, Martinelli G, Nagler A, Lanng Nielsen J, Ozbek U, Palandri F, Palmieri F, Pane F, Rege-Cambrin G, Russo D, Specchia G, Testoni N, Weiss-Bjerrum O, Saglio G, Simonsson B. Comparison of imatinib 400 mg and 800 mg daily in the front-line treatment of high-risk, Philadelphia-positive chronic myeloid leukemia: a European LeukemiaNet Study. Blood. 2009;113(19):4497–504. doi: 10.1182/blood-2008-12-191254. [DOI] [PubMed] [Google Scholar]
- [24].Cortes JE, Baccarani M, Guilhot F, Druker BJ, Branford S, Kim DW, Pane F, Pasquini R, Goldberg SL, Kalaycio M, Moiraghi B, Rowe JM, Tothova E, De Souza C, Rudoltz M, Yu R, Krahnke T, Kantarjian HM, Radich JP, Hughes TP. Phase III, randomized, open-label study of daily imatinib mesylate 400 mg versus 800 mg in patients with newly diagnosed, previously untreated chronic myeloid leukemia in chronic phase using molecular end points: tyrosine kinase inhibitor optimization and selectivity study. J Clin Oncol. 2010;28(3):424–30. doi: 10.1200/JCO.2009.25.3724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25.Saglio G, Kim DW, Issaragrisil S, le Coutre P, Etienne G, Lobo C, Pasquini R, Clark RE, Hochhaus A, Hughes TP, Gallagher N, Hoenekopp A, Dong M, Haque A, Larson RA, Kantarjian HM. Nilotinib versus imatinib for newly diagnosed chronic myeloid leukemia. N Engl J Med. 2010;362(24):2251–9. doi: 10.1056/NEJMoa0912614. [DOI] [PubMed] [Google Scholar]
- [26].Kantarjian H, Shah NP, Hochhaus A, Cortes J, Shah S, Ayala M, Moiraghi B, Shen Z, Mayer J, Pasquini R, Nakamae H, Huguet F, Boque C, Chuah C, Bleickardt E, Bradley-Garelik MB, Zhu C, Szatrowski T, Shapiro D, Baccarani M. Dasatinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia. N Engl J Med. 2010;362(24):2260–70. doi: 10.1056/NEJMoa1002315. [DOI] [PubMed] [Google Scholar]
- [27].Preudhomme C, Guilhot J, Nicolini FE, Guerci-Bresler A, Rigal-Huguet F, Maloisel F, Coiteux V, Gardembas M, Berthou C, Vekhoff A, Rea D, Jourdan E, Allard C, Delmer A, Rousselot P, Legros L, Berger M, Corm S, Etienne G, Roche-Lestienne C, Eclache V, Mahon FX, Guilhot F. Imatinib plus peginterferon alfa-2a in chronic myeloid leukemia. N Engl J Med. 2010;363(26):2511–21. doi: 10.1056/NEJMoa1004095. [DOI] [PubMed] [Google Scholar]
- [28].Hehlmann R, Lauseker M, Jung-Munkwitz S, Leitner A, Muller MC, Pletsch N, Proetel U, Haferlach C, Schlegelberger B, Balleisen L, Hanel M, Pfirrmann M, Krause SW, Nerl C, Pralle H, Gratwohl A, Hossfeld DK, Hasford J, Hochhaus A, Saussele S. Tolerability-adapted imatinib 800 mg/d versus 400 mg/d versus 400 mg/d plus interferon-alpha in newly diagnosed chronic myeloid leukemia. J Clin Oncol. 2011;29(12):1634–42. doi: 10.1200/JCO.2010.32.0598. [DOI] [PubMed] [Google Scholar]
- [29].Simonsson B, Gedde-Dahl T, Markevarn B, Remes K, Stentoft J, Almqvist A, Bjoreman M, Flogegard M, Koskenvesa P, Lindblom A, Malm C, Mustjoki S, Myhr-Eriksson K, Ohm L, Rasanen A, Sinisalo M, Sjalander A, Stromberg U, Bjerrum OW, Ehrencrona H, Gruber F, Kairisto V, Olsson K, Sandin F, Nagler A, Nielsen JL, Hjorth-Hansen H, Porkka K. Combination of pegylated IFN-alpha2b with imatinib increases molecular response rates in patients with low- or intermediate-risk chronic myeloid leukemia. Blood. 2011;118(12):3228–35. doi: 10.1182/blood-2011-02-336685. [DOI] [PubMed] [Google Scholar]
- [30].Radich JP, Kopecky KJ, Appelbaum FR, Kamel-Reid S, Stock W, Malnassy G, Paietta E, Wadleigh M, Larson RA, Emanuel P, Tallman M, Lipton J, Turner AR, Deininger M, Druker BJ. A randomized trial of dasatinib 100 mg versus imatinib 400 mg in newly diagnosed chronic-phase chronic myeloid leukemia. Blood. 2012;120(19):3898–905. doi: 10.1182/blood-2012-02-410688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Cortes JE, Kim DW, Kantarjian HM, Brummendorf TH, Dyagil I, Griskevicius L, Malhotra H, Powell C, Gogat K, Countouriotis AM, Gambacorti-Passerini C. Bosutinib versus imatinib in newly diagnosed chronic-phase chronic myeloid leukemia: results from the BELA trial. J Clin Oncol. 2012;30(28):3486–92. doi: 10.1200/JCO.2011.38.7522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Korn EL, Freidlin B, Abrams JS. Overall survival as the outcome for randomized clinical trials with effective subsequent therapies. J Clin Oncol. 2011;29(17):2439–42. doi: 10.1200/JCO.2011.34.6056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kantarjian HM, Talpaz M, O’Brien S, Jones D, Giles F, Garcia-Manero G, Faderl S, Ravandi F, Rios MB, Shan J, Cortes J. Survival benefit with imatinib mesylate versus interferon-alpha-based regimens in newly diagnosed chronic-phase chronic myelogenous leukemia. Blood. 2006;108(6):1835–40. doi: 10.1182/blood-2006-02-004325. [DOI] [PubMed] [Google Scholar]
- [34].Roy L, Guilhot J, Krahnke T, Guerci-Bresler A, Druker BJ, Larson RA, O’Brien S, So C, Massimini G, Guilhot F. Survival advantage from imatinib compared with the combination interferon-alpha plus cytarabine in chronic-phase chronic myelogenous leukemia: historical comparison between two phase 3 trials. Blood. 2006;108(5):1478–84. doi: 10.1182/blood-2006-02-001495. [DOI] [PubMed] [Google Scholar]
- [35].Saglio G, Baccarani M. First-line therapy for chronic myeloid leukemia: new horizons and an update. Clin Lymphoma Myeloma Leuk. 2010;10(3):169–76. doi: 10.3816/CLML.2010.n.026. [DOI] [PubMed] [Google Scholar]
- [36].Radich J. Stem cell transplant for chronic myeloid leukemia in the imatinib era. Semin Hematol. 2010;47(4):354–61. doi: 10.1053/j.seminhematol.2010.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]