Abstract
Purpose
In clinical practice, some patients with asthma show incompletely reversible airflow obstruction, resembling chronic obstructive pulmonary disease (COPD). The aim of this study was to analyze this overlap phenotype of asthma with COPD feature.
Materials and Methods
A total of 256 patients, over the age of 40 years or more with a diagnosis of asthma, based on either 1) positive response to bronchodilator: >200 mL forced expiratory volume in 1 s (FEV1) and >12% baseline or 2) positive methacholine or mannitol provocation test, were enrolled. Among the asthma patients, we defined the overlap group with incompletely reversible airflow obstruction [postbronchodilator FEV1/forced vital capacity (FVC) <70] at the initial time of admission and continuing airflow obstruction after at least 3 months follow up. We evaluated clinical features, serum eosinophil counts, serum total immunoglobulin (Ig) E with allergy skin prick test, spirometry, methacholine or mannitol provocation challenges and bronchodilator responses, based on their retrospective medical record data. All of the tests mentioned above were performed within one week.
Results
The study population was divided into two groups: asthma only (62%, n=159, postbronchodilator FEV1/FVC ≥70) and overlap group (38%, n=97, postbronchodilator FEV1/FVC <70). The overlap group was older, and contained more males and a higher percentage of current or ex-smokers than the asthma only group. Significantly lower FEV1 and higher total lung capacity, functional residual capacity, and residual volume were observed in the overlap group. Finally, significantly lower serum eosinophil count and higher IgE were seen in the overlap group.
Conclusion
Our results showed that the overlap phenotype was older, male asthmatic patients who have a higher lifetime smoking intensity, more atopy and generally worse lung function.
Keywords: Asthma, chronic obstructive pulmonary disease, overlap, airway hyperresponsiveness
INTRODUCTION
Many older asthma patients have pathobiological and symptomatic features of the overlap phenotype of asthma and chronic obstructive pulmonary disease (COPD), necessitating a re-evaluation of the concept of both diseases as separate conditions. From a clinical point of view, the overlap phenotype is composed of COPD patients with increased reversibility and/or of asthmatics with fixed or incompletely reversible airflow obstruction. Its prevalence reports recently estimated that about 13-20% of subjects with COPD have the overlap phenotype, with an increasing trend in the elderly population.1,2,3,4 Physiological ageing of the lung is associated with a decrease in the static elastic recoil, a decrease in compliance of the chest wall, and a decrease in the strength of respiratory muscles. This can lead to decrease of lung function. Also senile emphysema can occur, contributing to the decrement in expiratory flow with ageing.5
Elderly asthmatics are known to have higher rates of airway hyperresponsiveness, more severe asthma, and more difficult to control with corticosteroids.6,7 The Dutch Hypothesis quotes that asthma itself and airway hyperresponsiveness (AHR) predispose patients to develop COPD later in life.8
Patients with the overlap phenotype are known to have worse lung function, more respiratory symptoms, and a lower health-related quality of life than either disease alone.9,10 Recently, the diagnostic criteria for the overlap phenotype has been established by the consensus of a group of experts.11 However, this is limited to COPD patients, but not for the asthma with fixed airflow obstruction.
The aim of this study was to analyze clinical characteristics and lung function of the overlap phenotype of asthma with COPD feature, in the perspective of asthma patients. Most of the previous studies were investigated from COPD perspective. The benefit of our study is that we tried to approach overlap in the perspective of asthma as they may have different clinical and functional characteristics to COPD patients with increased reversibility.
MATERIALS AND METHODS
The medical records of all consecutive patients who were diagnosed with asthma at Seoul St. Mary's Hospital, The Catholic University of Korea, South Korea, between September 2007 and March 2012 were retrospectively reviewed. The study was approved by the Institutional Review Board of the Seoul St. Mary's Hospital, to evaluate and publish information from the patients' records. The requirement for informed consent was waived because of the retrospective nature of the study.
Study subjects and baseline data
We identified all out- and inpatients at Seoul St. Mary's Hospital, aged 41-79 years with a diagnosis of asthma in the set period. The identified cases were checked to ascertain whether they met the following criteria of asthma: Physician's diagnosis of asthma by specialists in pulmonary and allergy departments with either 1) positive response to bronchodilator: >200 mL forced expiratory volume in 1 s (FEV1) and >12% baseline and/or 2) positive methacholine or mannitol provocation test. All enrolled patients had at least one chronic persistent respiratory symptom consisting of cough, wheezing, dyspnea and chest tightness worsening at night or in the early morning for more than 3 months. Subjects who did not meet these criteria were excluded. Patients with the following diagnosis, based on history or tests, were excluded: COPD patients (defined by a post-bronchodilator FEV1/forced vital capacity (FVC) ratio of <0.70 due to GOLD criteria12) and with negative bronchodilator and/or bronchoprovocation response, bronchiectasis, tuberculosis destroyed lung, allergic bronchopulmonary aspergillosis, anthracofibrosis, interstitial lung disease, malignancy, and heart failure.
The enrolled study population was divided into two groups according to the presence of airflow obstruction. We defined overlap patients who had incompletely reversible airflow obstruction (postbronchodilator FEV1/FVC <70) at the time of initial admission and continuing airflow obstruction after at least 3 months follow-up regardless of treatment. Asthma only patients were defined as having postbronchodilator FEV1/FVC ≥70. Initial asthma patients with airflow obstruction who recovered from obstruction (FEV1/FVC ≥70) in their follow-up pulmonary function tests (PFTs) were allocated in the asthma only group. Subjects who did not have follow up lung function results were excluded as they did not meet our definition. The baseline clinical data included demographic data, smoking history, body mass index, height, spirometry, lung volumes, diffusing capacity, methacholine and mannitol provocation challenges, bronchodilator responses (BDRs), serum eosinophil percentage, serum eosinophil count, total serum immunoglobulin (Ig) E count and skin test results. All of the tests mentioned above were performed within one week.
Pulmonary function tests
PFTs were performed in all patients by three technicians experienced in lung function testing following American Thoracic Society (ATS)/European Respiratory Society (ERS)guidelines in a licensed laboratory.13,14 Spirometry and body plethysmography were performed according to current recommendations.13,14 The residual volume (RV), functional residual capacity (FRC) and total lung capacity (TLC) were determined by body plethysmograph. Diffusing capacity of the lung for carbon monoxide (DLCO) was measured in duplicate by the single-breath method according to ATS/ERS guidelines.15 Post-bronchodilator (BD) FEV1 (ΔFEV1) was measured 15 min after the administration of 400 mcg salbutamol using a metered dose inhaler and a large volume spacer.
According to ATS guidelines, medications that can decrease airway responsiveness were withheld before the test.16
Bronchoprovocation tests
Non-specific bronchial responsiveness was assessed by bronchial challenge with methacholine chloride and mannitol. Bronchoprovocation tests using methacholine were performed in accordance with ATS guidelines.16 The methacholine challenge schedule started with an inhalation of saline, followed by increasing concentrations of methacholine up to a cumulative dose of 25 mg/mL. The test was stopped when either the maximum cumulative dose had been reached or FEV1 had fallen by 20% or more. Positive methacholine results were defined as provocative concentration of methacholine required to decrease FEV1 (PC20) by 20% less than or equal to 16 mg/mL.16
Dry powder mannitol (Aridol; Pharmaxis, Sydney, Australia) was administered according to the recommendations of the manufacturer, and FEV1 was recorded in line with current guidelines.17 The mannitol challenge schedule started with an inhalation of 0 mg placebo, followed by increasing concentrations of mannitol up to a cumulative dose of 635 mg. The challenge was stopped when FEV1 decreased of 15% or more from baseline values or when the maximum cumulative dose of 635 mg had been administered. Positive mannitol results were defined as PD15 less than or equal to 635 mg.17,18 Patients with severe airflow limitation (FEV1 <50% predicted or <1.0 L) were contraindicated for bronchoprovocation tests. Medications that can decrease airway responsiveness were withheld before the test, according to ATS guidelines.16
Evaluation of allergy and atopy
Atopy was defined as either at least one positive specific IgE or one positive skin prick test to aeroallergens (cat, dog, house dust mite, grasses, and fungi). Skin prick test was considered positive when there was a 3 mm or larger wheal and/or erythema of 10 mm or more, greater than the negative control. All patients were asked to discontinue using antihistamine for 3 days prior to testing.19 Furthermore, the increase of eosinophils, eosinophil count, and total IgE were analyzed between groups.
Data analysis
Continuous variables are presented as mean±standard error of mean and analyzed using two independent sample t-test. Categorical variables are presented as frequency and percentage and analyzed using Pearson's chi-square tests or Fisher's exact tests. All tests were two-sided, and p-value <0.05 was considered statistically significant. All analyses were performed with the SPSS computer package, version 18.0 (SPSS Inc., Chicago, IL, USA).
RESULTS
During the study period, 1898 patients with a suspected diagnosis of asthma were enrolled. After evaluation, a total of 566 (30%) eligible patients who had asthma according to the definition criteria were included: all relevant clinical data and initial spirometry results were available for these patients. Of these patients, we excluded 310 patients who did not follow up PFTs. Thus, a total of 256 asthma patients (13.4%) were enrolled in the study.
We divided the 256 asthma patients into two groups according to the presence of airflow obstruction. Finally, 159 (62%) patients were enrolled in the asthma only group and 97 (38%) patients in the overlap group.
Clinical characteristics of enrolled patients
The clinical characteristics of 256 asthma patients are shown in Table 1. The overlap group was older (63.0±0.9 vs. 57.6±0.7, p<0.01) and had more males (37.1% vs. 18.2%, p<0.01) than the asthma only group. There was higher percentage of current or ex-smokers (46.2% vs. 14.9%, p<0.01) in the overlap group.
Table 1.
Comparison between Overlap and Asthma Only Group
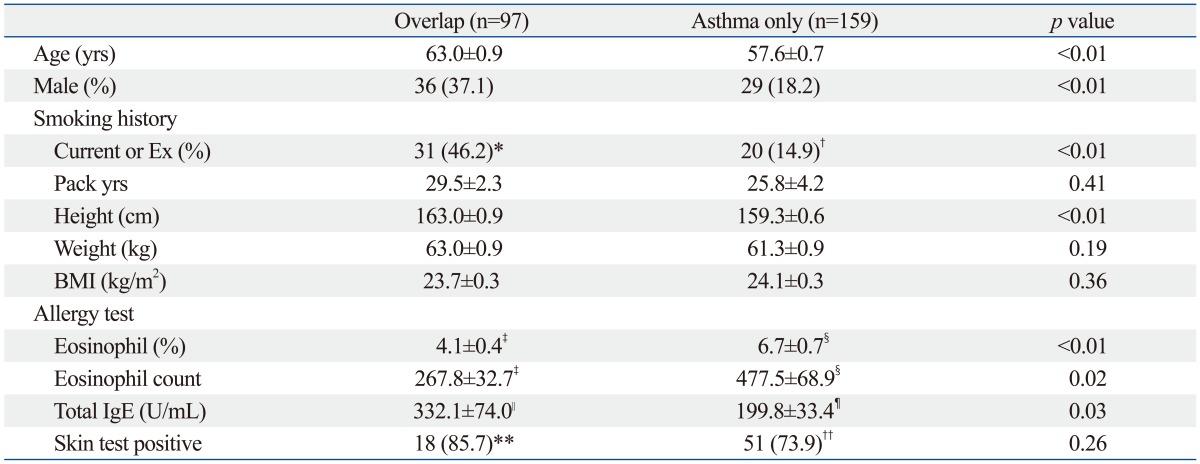
BMI, body mass index; SEM, standard error of mean.
Values are mean±SEM or number of patients (%).
*n=67.
†n=134.
‡n=42.
§n=98.
∥n=22.
¶n=55.
**n=21.
††n=69.
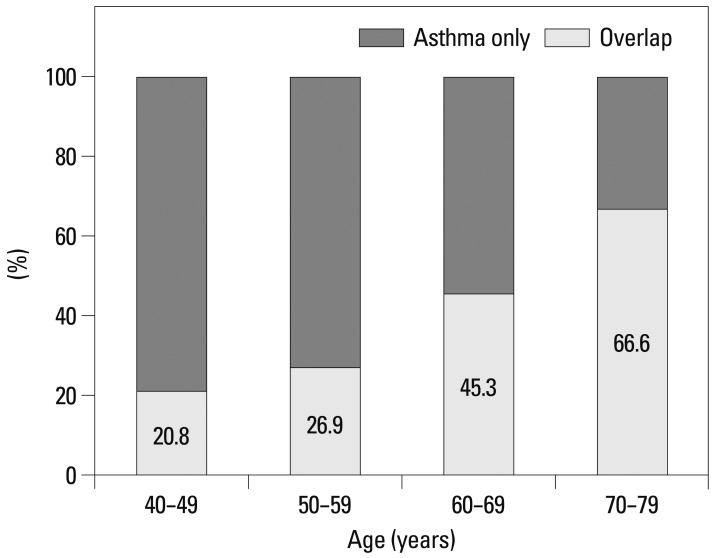
Percentage of patients with the overlap phenotype in different age groups are shown in Fig. 1. Among subjects with asthma, the percentage of overlap was 20.8%, 26.9%, 45.3%, and 66.6% in the 40-49, 50-59, 60-69, and 70-79 years age groups, respectively (Fig. 1). The highest percentage was shown in the 70 s.
Fig. 1.
The percentage of patients diagnosed with overlap in different age groups. The values above each bar represent the percentage of patients diagnosed with overlap in each age groups.
Allergic test findings
Allergic test results are shown in Table 1. Significantly lower serum eosinophil count (267.8±32.7 vs. 477.5±68.9, p=0.02) and higher IgE (332.1±74.0 vs. 199.8±33.4, p=0.03) were seen in the overlap group. However, there was no significant difference in positive allergic skin test results in either group.
Pulmonary function test findings
Pulmonary function test findings at the time of presentation are shown in Table 2. The overlap group had lower FEV1 (58.0±1.2% vs. 69.4±1.2%, p<0.01), and higher TLC (111.1±2.2% vs. 101.6±1.6%, p<0.01), FRC (125.2±4.0% vs. 101.9±2.3%, p<0.01), and RV (125.6±6.0% vs. 99.0± 3.9%, p<0.01). There was no significant difference in DLCO values in both groups.
Table 2.
Comparison between Overlap and Asthma Only Group
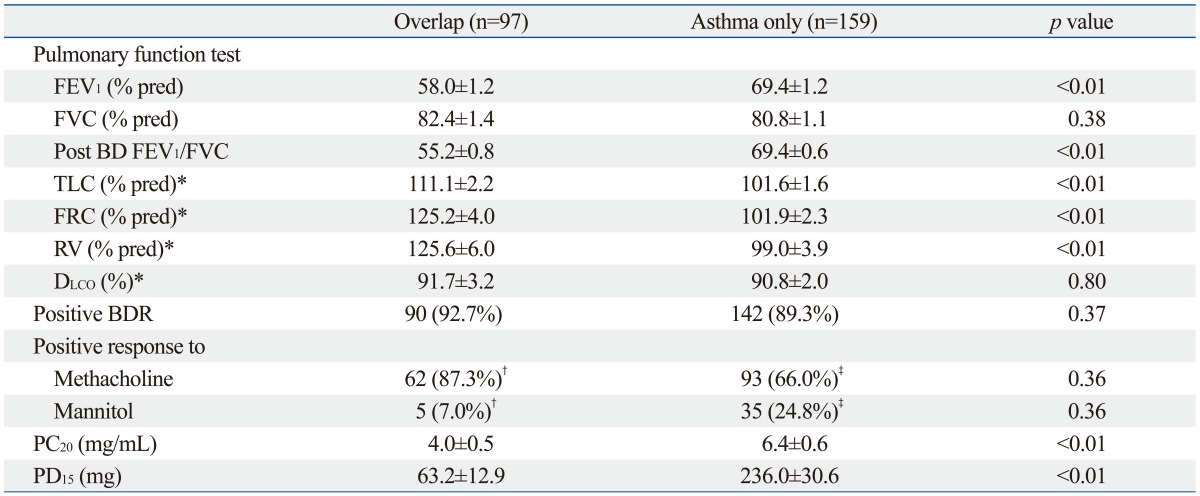
BDR, bronchodilator response; TLC, total lung capacity; FRC, functional residual capacity; RV, residual volume; BD, bronchodilator; SEM, standard error of mean; DLCO, difffusing capacity of the lung for carbon monoxide; FEV1, forced expiratory volume in 1 s; FVC, forced vital capacity.
Values are mean±SEM or number of patients (%).
Positive BDR: positive response to bronchodilator: >200 mL FEV1 and >12% baseline.
*Overlap (n=39), asthma only (n=66).
†n=71.
‡n=141.
There was no significant difference in AHR with either methacholine or mannitol and BDR in the two groups. However, the mean PC20 (3.9 vs. 6.4, p<0.01), and PD15 (63.2 vs. 236.0, p<0.01) values were significantly lower in the overlap group, as shown in Table 2.
DISCUSSION
It is often difficult to clinically distinguish overlapping COPD and asthma, and there have been many studies to investigate the characteristics of such phenotype.1,2,3,4,6,20 Diagnostic criteria for this overlap phenotype in COPD have been proposed, including positive BDR, eosinophilia in sputum, personal history of asthma before age 40 years, high total IgE level, and a personal history of atopy.11 However, this was investigated from COPD perspective. From the perspective of asthma, overlap phenotype can be defined as asthmatics with fixed airflow obstruction.2 To investigate the overlap phenotype from the perspective of asthma, we excluded COPD patients without asthmatic components.
Previous studies showed that asthma is a risk factor for the development of fixed airflow obstruction,8,21 while cigarette smoking is the main risk factor for the development of persistent airflow obstruction in asthmatics.22 Asthmatics with a history of smoking, exhibit higher numbers of neutrophils in bronchoalveolar lavage fluid and biopsies.23,24 In our present study, we defined the overlap group within our enrolled asthma patients, which is different from other studies. In the diagnosis of asthma, we excluded physician's diagnosis of asthma without either positive BD or provocation results because of the potential inaccuracy. To try and differentiate overlap, which shows persistent irreversible obstruction, from severe asthma with reversible airflow obstruction, patients who recovered airflow obstruction at follow up PFTs (at least 3 months interval) were designated in the asthma group. Patients who did not have follow-up PFTs were excluded. Of the initial 566 asthma patients, we only enrolled 256 patients with follow up PFTs.
In our asthma clinic cohort, the prevalence of overlap was approximately half of that of asthma only (37.9% vs. 62.1%). This finding is consistent with a previous study that the prevalence of overlap is nearly half of that of asthma (24.3% vs. 52.9%), representing a significant proportion of patients with both phenotypes.6 In our cohort, the highest percentage was observed in patients in their 70 s, and large population studies found that the prevalence of this overlap phenotype increases with age.4,6 In our study, the age distribution also followed this trend. Age is a very important variable when assessing obstructive lung diseases, due to the known changes in lung function that occur with increased age.5 A combination of exercise intolerance, static or dynamic hyperinflation and senile emphysema in the elderly patient can lead to a decrease in lung function.5 The annual decrease in FEV1 is approximately 20 mL/year in subjects up to age 40 years and is approximately double that number when an individual's age is greater than 65 years. The decrease in FEV1 is slightly greater than that in FVC, particularly from 50 to 60 years of age, resulting in a decrease in the FEV1/FVC ratio in older individuals.5,25
Furthermore, there was significant increase of ex-smokers in the overlap group. It is known that asthmatics who smoke have more neutrophils in their airways, leading to steroid resistance.19,20 This in turn can lead to more severe symptoms and an accelerated decline in lung function.21,22
Total IgE was significantly increased in the overlap group compared to the asthma only group. Atopic persons often have increased plasma total IgE concentrations, and quantitative IgE antibodies may serve as a marker of asthma severity.26,27 It has been reported that AHR to methacholine is correlated with the level of total IgE in the serum, which has been observed not only in subjects with asthma and rhinitis, but also in asymptomatic subjects.28 Based on these findings, we conclude that more severe degree of atopy in asthma patients may lead to the development of mixed phenotype.
In the present study, we compared pulmonary function between the two groups, and observed a lower FEV1 in the overlap group. This could be explained by the fact that the overlap group had more smokers than the asthma only group. Moreover, asthma itself is significantly associated with an increased risk for chronic bronchitis, emphysema and COPD compared to nonasthmatic subjects, and smoking significantly accelerates the decline in lung function in subjects with or without asthma.21,29 It is well known that cigarette smoking accelerates the loss of lung function by up to 50 mL per year.30 Its effect may be greater in asthmatic smokers, since they have more severe asthma symptoms, accelerated decline in FEV1, reduced response to corticosteroids and increased neutrophilic airway inflammation.31,32,33,34
Previous studies have suggested that factors associated with accelerated lung function decline in asthma also include more severe AHR, adult-onset asthma, frequent severe exacerbations, persistent symptoms, baseline airflow obstruction and persistent elevation of exhaled nitric oxide (NO).35,36,37 In the present study, we found more severe AHR in the overlap group which could be an another contributing factor of lower pulmonary function and irreversible airway obstruction.
We evaluated lung volume in both groups (asthma only; n=66, overlap; n=39). In the overlap group, TLC, FRC, and RV were significantly increased compared to the asthma only group, indicating that air trapping was more severe in the overlap group, in good agreement with a previous study that the overlap group had more gas trapping on expiratory chest CT scans compared to subjects with COPD alone.3 Unfortunately, we were not able to evaluate CT imaging studies since this was a retrospective study. More imaging studies are needed to differentiate the two groups in the future.
The findings in the present study led us to suggest that the mechanisms behind the differences between the two groups involve the combination of aging, cigarette smoking and airway remodeling. First, aging has an effect on decreased lung function, as seen previously.5,25 Second, cigarette smoking in asthmatic patients can significantly accelerate the decline in lung function and increase the risk of COPD.21,29 Third, asthmatic patients can develop airway remodeling as a consequence of persistent airway inflammation which can lead to fixed airflow obstruction. Therefore, these three factors may contribute to the manifestation of overlap syndrome. To what extent they individually contribute to the disease remains unclear and needs to be studied further.
One limitation of this study is the possibility that selection bias might have influenced the significance of our findings, given its retrospective nature. However, a strict diagnostic criteria for asthma was applied to the patients during the enrolling process. As a result, only 13.4% (256 cases) of patients out of 1898 cases of suspected asthma, were enrolled in the study. Thus, we are quite certain that our diagnosis of asthma was reliable, as patients with only the physician's diagnosis of asthma have potential inaccuracy and they were excluded. In our study, we evaluated the differences in lung functions and airway hyperresponsiveness in both groups, and therefore, initial and follow up PFTs were essential to our study. The patients without follow up PFT results were also excluded. Another limitation is the lack of evaluation in inflammatory markers, such as sputum eosinophil and neutrophil counts or exhaled NO. Comparison of these markers would have assisted in comparing the pathologic differences in these two groups.
In conclusion, the overlap phenotype was found to be older, male asthmatic patients who had a higher lifetime smoking intensity and an increased total serum IgE. Lung functions in this group showed lower FEV1 and higher TLC, FRC and RV which suggests more air trapping. The causes of differences between the two groups may be due to the combination of aging, smoking and airway remodeling. Further studies on this overlap phenotype are needed to establish definite diagnostic criteria in asthmatic patients.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Soriano JB, Davis KJ, Coleman B, Visick G, Mannino D, Pride NB. The proportional Venn diagram of obstructive lung disease: two approximations from the United States and the United Kingdom. Chest. 2003;124:474–481. doi: 10.1378/chest.124.2.474. [DOI] [PubMed] [Google Scholar]
- 2.Gibson PG, Simpson JL. The overlap syndrome of asthma and COPD: what are its features and how important is it? Thorax. 2009;64:728–735. doi: 10.1136/thx.2008.108027. [DOI] [PubMed] [Google Scholar]
- 3.Hardin M, Silverman EK, Barr RG, Hansel NN, Schroeder JD, Make BJ, et al. The clinical features of the overlap between COPD and asthma. Respir Res. 2011;12:127. doi: 10.1186/1465-9921-12-127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.de Marco R, Pesce G, Marcon A, Accordini S, Antonicelli L, Bugiani M, et al. The coexistence of asthma and chronic obstructive pulmonary disease (COPD): prevalence and risk factors in young, middle-aged and elderly people from the general population. PLoS One. 2013;8:e62985. doi: 10.1371/journal.pone.0062985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Janssens JP, Pache JC, Nicod LP. Physiological changes in respiratory function associated with ageing. Eur Respir J. 1999;13:197–205. doi: 10.1034/j.1399-3003.1999.13a36.x. [DOI] [PubMed] [Google Scholar]
- 6.Zeki AA, Schivo M, Chan A, Albertson TE, Louie S. The Asthma-COPD Overlap Syndrome: A Common Clinical Problem in the Elderly. J Allergy (Cairo) 2011;2011:861926. doi: 10.1155/2011/861926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Enright PL. The diagnosis and management of asthma is much tougher in older patients. Curr Opin Allergy Clin Immunol. 2002;2:175–181. doi: 10.1097/00130832-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Orie NG. The dutch hypothesis. Chest. 2000;117(5 Suppl 1):299S. doi: 10.1016/s0012-3692(15)51044-1. [DOI] [PubMed] [Google Scholar]
- 9.Kauppi P, Kupiainen H, Lindqvist A, Tammilehto L, Kilpeläinen M, Kinnula VL, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011;48:279–285. doi: 10.3109/02770903.2011.555576. [DOI] [PubMed] [Google Scholar]
- 10.Miravitlles M, Soriano JB, Ancochea J, Muñoz L, Duran-Tauleria E, Sánchez G, et al. Characterisation of the overlap COPD-asthma phenotype. Focus on physical activity and health status. Respir Med. 2013;107:1053–1060. doi: 10.1016/j.rmed.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Soler-Cataluña JJ, Cosío B, Izquierdo JL, López-Campos JL, Marín JM, Agüero R, et al. Consensus document on the overlap phenotype COPD-asthma in COPD. Arch Bronconeumol. 2012;48:331–337. doi: 10.1016/j.arbres.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 12.Vestbo J, Hurd SS, Agustí AG, Jones PW, Vogelmeier C, Anzueto A, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187:347–365. doi: 10.1164/rccm.201204-0596PP. [DOI] [PubMed] [Google Scholar]
- 13.Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–338. doi: 10.1183/09031936.05.00034805. [DOI] [PubMed] [Google Scholar]
- 14.Wanger J, Clausen JL, Coates A, Pedersen OF, Brusasco V, Burgos F, et al. Standardisation of the measurement of lung volumes. Eur Respir J. 2005;26:511–522. doi: 10.1183/09031936.05.00035005. [DOI] [PubMed] [Google Scholar]
- 15.Macintyre N, Crapo RO, Viegi G, Johnson DC, van der Grinten CP, Brusasco V, et al. Standardisation of the single-breath determination of carbon monoxide uptake in the lung. Eur Respir J. 2005;26:720–735. doi: 10.1183/09031936.05.00034905. [DOI] [PubMed] [Google Scholar]
- 16.Crapo RO, Casaburi R, Coates AL, Enright PL, Hankinson JL, Irvin CG, et al. Guidelines for methacholine and exercise challenge testing-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med. 2000;161:309–329. doi: 10.1164/ajrccm.161.1.ats11-99. [DOI] [PubMed] [Google Scholar]
- 17.Brannan JD, Anderson SD, Perry CP, Freed-Martens R, Lassig AR, Charlton B, et al. The safety and efficacy of inhaled dry powder mannitol as a bronchial provocation test for airway hyperresponsiveness: a phase 3 comparison study with hypertonic (4.5%) saline. Respir Res. 2005;6:144. doi: 10.1186/1465-9921-6-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson SD, Charlton B, Weiler JM, Nichols S, Spector SL, Pearlman DS, et al. Comparison of mannitol and methacholine to predict exercise-induced bronchoconstriction and a clinical diagnosis of asthma. Respir Res. 2009;10:4. doi: 10.1186/1465-9921-10-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bernstein IL, Li JT, Bernstein DI, Hamilton R, Spector SL, Tan R, et al. Allergy diagnostic testing: an updated practice parameter. Ann Allergy Asthma Immunol. 2008;100(3 Suppl 3):S1–S148. doi: 10.1016/s1081-1206(10)60305-5. [DOI] [PubMed] [Google Scholar]
- 20.Kim TB, Oh YM, Chang YS, Cho YS, Jang AS, Cho SH, et al. The reality of an intermediate type between asthma and COPD in practice. Respir Care. 2012;57:1248–1253. doi: 10.4187/respcare.01232. [DOI] [PubMed] [Google Scholar]
- 21.Silva GE, Sherrill DL, Guerra S, Barbee RA. Asthma as a risk factor for COPD in a longitudinal study. Chest. 2004;126:59–65. doi: 10.1378/chest.126.1.59. [DOI] [PubMed] [Google Scholar]
- 22.Lee JH, Haselkorn T, Borish L, Rasouliyan L, Chipps BE, Wenzel SE. Risk factors associated with persistent airflow limitation in severe or difficult-to-treat asthma: insights from the TENOR study. Chest. 2007;132:1882–1889. doi: 10.1378/chest.07-0713. [DOI] [PubMed] [Google Scholar]
- 23.Wenzel SE, Szefler SJ, Leung DY, Sloan SI, Rex MD, Martin RJ. Bronchoscopic evaluation of severe asthma. Persistent inflammation associated with high dose glucocorticoids. Am J Respir Crit Care Med. 1997;156(3 Pt 1):737–743. doi: 10.1164/ajrccm.156.3.9610046. [DOI] [PubMed] [Google Scholar]
- 24.Louis R, Lau LC, Bron AO, Roldaan AC, Radermecker M, Djukanović R. The relationship between airways inflammation and asthma severity. Am J Respir Crit Care Med. 2000;161:9–16. doi: 10.1164/ajrccm.161.1.9802048. [DOI] [PubMed] [Google Scholar]
- 25.Schmidt CD, Dickman ML, Gardner RM, Brough FK. Spirometric standards for healthy elderly men and women. 532 subjects, ages 55 through 94 years. Am Rev Respir Dis. 1973;108:933–939. doi: 10.1164/arrd.1973.108.4.933. [DOI] [PubMed] [Google Scholar]
- 26.Gould HJ, Sutton BJ, Beavil AJ, Beavil RL, McCloskey N, Coker HA, et al. The biology of IGE and the basis of allergic disease. Annu Rev Immunol. 2003;21:579–628. doi: 10.1146/annurev.immunol.21.120601.141103. [DOI] [PubMed] [Google Scholar]
- 27.Wickman M. Experience with quantitative IgE antibody analysis in relation to allergic disease within the BAMSE birth cohort--towards an improved diagnostic process. Allergy. 2004;59(Suppl 78):30–31. doi: 10.1111/j.1398-9995.2004.00572.x. [DOI] [PubMed] [Google Scholar]
- 28.Sears MR, Burrows B, Flannery EM, Herbison GP, Hewitt CJ, Holdaway MD. Relation between airway responsiveness and serum IgE in children with asthma and in apparently normal children. N Engl J Med. 1991;325:1067–1071. doi: 10.1056/NEJM199110103251504. [DOI] [PubMed] [Google Scholar]
- 29.Lange P, Parner J, Vestbo J, Schnohr P, Jensen G. A 15-year follow-up study of ventilatory function in adults with asthma. N Engl J Med. 1998;339:1194–1200. doi: 10.1056/NEJM199810223391703. [DOI] [PubMed] [Google Scholar]
- 30.Anthonisen NR, Connett JE, Murray RP. Smoking and lung function of Lung Health Study participants after 11 years. Am J Respir Crit Care Med. 2002;166:675–679. doi: 10.1164/rccm.2112096. [DOI] [PubMed] [Google Scholar]
- 31.Chaudhuri R, Livingston E, McMahon AD, Thomson L, Borland W, Thomson NC. Cigarette smoking impairs the therapeutic response to oral corticosteroids in chronic asthma. Am J Respir Crit Care Med. 2003;168:1308–1311. doi: 10.1164/rccm.200304-503OC. [DOI] [PubMed] [Google Scholar]
- 32.Thomson NC, Chaudhuri R, Livingston E. Active cigarette smoking and asthma. Clin Exp Allergy. 2003;33:1471–1475. doi: 10.1046/j.1365-2222.2003.01805.x. [DOI] [PubMed] [Google Scholar]
- 33.Althuis MD, Sexton M, Prybylski D. Cigarette smoking and asthma symptom severity among adult asthmatics. J Asthma. 1999;36:257–264. doi: 10.3109/02770909909075409. [DOI] [PubMed] [Google Scholar]
- 34.Siroux V, Pin I, Oryszczyn MP, Le Moual N, Kauffmann F. Relationships of active smoking to asthma and asthma severity in the EGEA study. Epidemiological study on the Genetics and Environment of Asthma. Eur Respir J. 2000;15:470–477. doi: 10.1034/j.1399-3003.2000.15.08.x. [DOI] [PubMed] [Google Scholar]
- 35.ten Brinke A, Zwinderman AH, Sterk PJ, Rabe KF, Bel EH. Factors associated with persistent airflow limitation in severe asthma. Am J Respir Crit Care Med. 2001;164:744–748. doi: 10.1164/ajrccm.164.5.2011026. [DOI] [PubMed] [Google Scholar]
- 36.Bai TR, Vonk JM, Postma DS, Boezen HM. Severe exacerbations predict excess lung function decline in asthma. Eur Respir J. 2007;30:452–456. doi: 10.1183/09031936.00165106. [DOI] [PubMed] [Google Scholar]
- 37.van Veen IH, Ten Brinke A, Sterk PJ, Sont JK, Gauw SA, Rabe KF, et al. Exhaled nitric oxide predicts lung function decline in difficult-to-treat asthma. Eur Respir J. 2008;32:344–349. doi: 10.1183/09031936.00135907. [DOI] [PubMed] [Google Scholar]