Abstract
Objective:
There remains concern regarding the use of fiducial-based image-guided radiotherapy (IGRT) in patients with high-risk prostate cancer also undergoing intensity-modulated radiotherapy (IMRT) to pelvic nodes. By a retrospective study, we aim to ascertain the impact of the use of fiducial-based IGRT on lymph node planned target volume (PTV) coverage.
Methods:
30 consecutive IMRT prostate and pelvic node plans were reviewed, and dose was recalculated with 1-mm increment movements in anterior, posterior, superior, inferior, right and left directions up to 10 mm. All patients were treated with a full bladder after drinking 450–750 ml of water and empty rectum with the use of sodium citrate enemas daily. Dose–volume histogram parameters were recorded at each position, specifically nodal PTV V95%, V99% and V100%. A local IGRT database was used to identify the likelihood of a particular bony to fiducial offset in all directions. The combined data were used to calculate the percentage risk of underdosing the lymph node PTV on any given fraction.
Results:
The likelihood of an offset in the left, right and anterior directions occurring and resulting in a failure to cover the PTV was <0.25%. The likelihood of a posterior offset occurring and resulting in inadequate coverage was slightly higher but remained <1%.
Conclusion:
This study confirms the safety of fiducial-based image-guided IMRT (IG-IMRT) with a strict bowel and bladder protocol, allowing a reduction of the clinical target volume to PTV margin of the prostate volume and consequent reduction in rectal toxicity.
Advances in knowledge:
This study strengthens the evidence supporting the safe implementation of fiducial-based IG-IMRT treating the prostate and pelvic nodes in high-risk prostate cancer.
Intensity-modulated radiotherapy (IMRT) is the standard of care in radical radiotherapy for prostate cancer.1 In IMRT delivery, the accuracy of the planned target volume (PTV) definition is critically important as steep dose gradients may increase the risk of geographical miss.2 One of the significant potential errors in prostate radiotherapy arises from prostate motion, the mean and maximum of which are reportedly 4–6 and 8–18 mm, respectively.3–8 The margin from clinical target volume (CTV) to PTV is intended to minimize errors associated with prostate movement during radiation delivery, planning system and delivery uncertainties, as well as daily set-up error.9
Online fiducial-based image-guided radiotherapy (IGRT) uses a minimum of three fiducial markers inserted into the prostate gland for verification and patient realignment. Paired planar tube potential images are taken prior to the treatment and the fiducial position is matched to the planning CT scan. This corresponding shift is performed prior to the treatment, minimizing any systematic error from patient set-up and the random interfraction prostate motion.10 Some reports state that online IGRT allows CTV to PTV margins to be reduced to as little as 2 mm,11 although with the residual intrafraction error perhaps a more realistic margin is 4 mm, as suggested by McNair et al.12 Owing to the reduced margin and resultant decrease in rectal dose and toxicity, IGRT is the standard of care for patients receiving radical radiotherapy for localized prostate cancer, with many centres opting for fiducial-based IGRT.
In addition to improved radiotherapy delivery techniques, the landmark Radiation Therapy Oncology Group (RTOG) 9413 study demonstrated a statistically significant 7-year progression-free survival (PFS) benefit, in the subset of patients who received neoadjuvant and concurrent hormonal therapy, of 40% vs 27% using the whole pelvis compared with prostate-only radiotherapy.13 This is a controversial area as prospective randomized trials attempted before the RTOG 9413 failed to demonstrate any statistically significant advantage with whole pelvis radiotherapy vs prostate-only radiotherapy.14,15 In addition, these studies were not powered to identify an overall survival benefit; therefore, there is no evidence that it affects overall survival. Owing to significantly increased toxicity with this technique, some clinicians believe that the risks outweigh the potential benefits. To minimize toxicity and improve lymph node coverage, IMRT has been used in this setting.16,17
A review article by Kaidar-Person et al18 highlights the issues of using fiducial-based prostate IGRT for patients requiring simultaneous nodal irradiation. The lymph node target coverage may be compromised because lymph nodes and the prostate are moving independently.19 As a result, matching to fiducials may result in underdosing of the nodes. To prevent this, when delivering IMRT to pelvic nodes, many radiotherapy centres perform IGRT based on a bony match to the planning CT, rather than fiducials. However, when using a bony match, the prostate CTV to PTV margin is necessarily larger, resulting in larger rectal doses and consequently more toxicity.
Previous reports on the use of fiducial-based IGRT with IMRT in prostate and nodal irradiation used very small sample sizes.11,20,21 Hsu et al20 studied five cases, applying each daily fiducial-based IGRT shift to the IMRT treatment course and concluded negligible differences in pelvic lymph node or normal tissue dose, with <1.5% difference in dose delivered. Chung et al11 compared 10 bony IGRT cases with 15 fiducial-based IGRT cases. They reported reduced lymph node coverage with fiducial-based image-guided IMRT (IG-IMRT), which in their opinion was unlikely to lead to clinical detriment. Rossi et al21 reviewed daily treatments for 10 patients treated with fiducial-based IG-IMRT by monitoring the nodal PTV coverage in comparison with the planned coverage. They confirmed, providing no systematic shift occurred, a 2.2% degradation to the planned nodal dose.21 In an ideal setting, the population-based data would be used to calculate an accurate CTV to PTV margin for the lymph nodes using IG-IMRT, in the manner of van Herk et al;22 however, in reality to maintain an acceptable toxicity in view of the questionable benefit, the dose coverage is often limited to achieve small bowel constraints. With an increasing number of centres moving to fiducial-based prostate IGRT, there is a requirement for more robust evidence of safe lymph node coverage using this technique before a change in practice.
We aim to perform a retrospective study to assess the prophylactic dose coverage of lymph nodes when treated with fiducial-based IG-IMRT.
METHODS AND MATERIALS
Patient selection
A retrospective study was performed using the planning CT scans of 30 patients who had completed IMRT to the prostate and pelvic lymph nodes between January 2008 and June 2011. In our centre, all patients with a lymph node risk >20%, using Roach23 formulae, receive whole pelvis IMRT. Patients must have a life expectancy of 10 years and be able to maintain a bladder volume of at least 250 ml for at least 1 h.
Delineation and planning
Patients are immobilized in a supine position using Kneefix™ and Feetfix™, which are indexed on the Combifix™ system (Civco Medical Solutions, Kalona, IA). Our local bladder and rectal preparation protocol requires all patients initially to evacuate their rectum following a sodium citrate enema and to empty their bladder. Thereafter, they drink 450–750 ml of water 30–60 min before the treatment, to achieve a bladder volume of >250 ml and a rectal diameter of <4 cm, for CT scanning. An initial planning CT scan is performed on a LightSpeed® RT 16 multi-slice CT scanner (GE Healthcare, Chalfont St Giles, UK) with scanning parameters set at 120 kV, auto mA with a slice thickness of 2.5 mm. All plans had been delineated by clinical oncologists at St Bartholomew's Hospital, London, UK. Radiotherapy planning was undertaken using the Eclipse™ treatment planning system software v. 10 (Varian Medical Systems, Palo Alto, CA) using the anisotropic analytic algorithm as per our current clinical protocol. Prostate CTV includes the whole prostate and seminal vesicles. To create the prostate PTV, a margin of 10 mm is added in all directions other than in the posterior direction, where 6–10 mm is used. Prophylactic nodes were outlined in accordance with the RTOG guidelines.24 A further margin of 6–10 mm was added to the nodal CTV to create the nodal PTV. This margin is varied to achieve small bowel constraints, and bowel toxicity is prioritized to limit toxicity owing to the questionable benefit of pelvic lymph node irradiation. A single-phase IMRT plan was created with mean prescription doses of 72 or 74 Gy to prostate PTV and 55 Gy to nodal PTV using a simultaneous integrated boost technique in 36–37 fractions using 6-MV photons. All patients were inversely planned to achieve the constraints as noted in Table 1.
Table 1.
Organ at risk constraints used in the planning process
| Target structures | Volume constraint (%) | Dose required [% (Gy)] | |
|---|---|---|---|
| Prostate PTV | 99 | 90 (66.6) | |
| 95 | 95 (70.3) | ||
| 50 | 100 (74) | ||
| 5 | 105 (77.7) | ||
| Nodal PTV | 99 | 90 (49.5) | |
| 95 | 95 (52.3) | ||
| 50 | 100 (55) | ||
| PTV, planned target volume. | |||
| Risk structures | Dose constraint (Gy) | Volume required | |
| Rectum | 50 | 60% | |
| 60 | 50% | ||
| 65 | 30% | ||
| 70 | 15% | ||
| 75 | 0% | ||
| Bladder | 50 | 50% | |
| 60 | 25% | ||
| 70 | 5% | ||
| Bowel | 45 | 158 cm3 | |
| 50 | 110 cm3 | ||
| 55 | 28 cm3 | ||
| 60 | 6 cm3 | ||
| 65 | 0 cm3 | ||
| Femoral heads | 50 | 50% | |
Dosimetric analysis
In order to calculate the risk of reduced lymph node PTV coverage with different shifts, we used the clinically delivered plan as a reference. We applied incremental 1-mm isocentre shifts in the treatment planning system in each direction in turn, up to 10 mm. All shifts were unidirectional. Each plan was recalculated and the following noted:
• the mean dose to PTV nodes (Gy)
• the volume of PTV nodes receiving at least 52.25 Gy (95% of dose)
• the volume of PTV nodes receiving at least 49.5 Gy (90% of dose)
• whether 50% volume was receiving >55 Gy (100% of dose).
Image-guided radiotherapy database analysis
The local IGRT database includes daily positional data for 36 patients treated over 1278 fractions. This was used to calculate the relative offset between a bony match and the fiducial match. For the purposes of this study, an online bony match representing the lymph node position is considered the standard of care. The relative offset between the bony match and the fiducial match simulates the fiducial-directed treatment position from the previous current gold standard.
The daily offset between fiducial match and bony match was quantified using on-treatment tube potential and MV image data from prostate patients treated with online fiducial-based IGRT in our centre.
Combined dosimetric and image-guided radiotherapy database analysis
We aim to calculate the overall risk of failing to maintain the lymph node PTV parameters in a particular fraction. The relative offset seen in the images from the population database provides the percentage risk of a relative movement being applied in the IGRT population. The dosimetric analysis provides the percentage risk of failing the PTV constraints with each relative movement. The combination of these results will quantify how often a failure to achieve PTV constraints will have occurred during a single fraction of the treatment course in our 30 patients. The PTV failure risk (α, %) was calculated using the equation:
where F is the percentage of patients failing at X mm and A is the percentage risk of X mm offset being applied.
As the prostate position may migrate in one direction over a course of treatment, the individual mean offset over a course of treatment in any one direction may not be zero. We calculated the risk of failure to cover the PTV, with the likelihood of a particular mean offset seen in the IGRT database. For each of the six directions, the percentage of patients having a mean offset in 1-mm increments was calculated. The equation to estimate risk of failure to achieve PTV constraints (β) had the appropriate percentage of patients been treated consistently with the mean offset is:
where M is the percentage risk of X mm mean offset.
RESULTS
Patient demographics
30 consecutive cases were retrospectively planned. 96.6% of cases (n = 29) had completed an IMRT course to include pelvic lymph nodes with 55 Gy prescribed in 1.49 Gy per fraction over 37 fractions. One patient received 55 Gy in 1.53 Gy per fraction over 36 fractions.
Dosimetric analysis
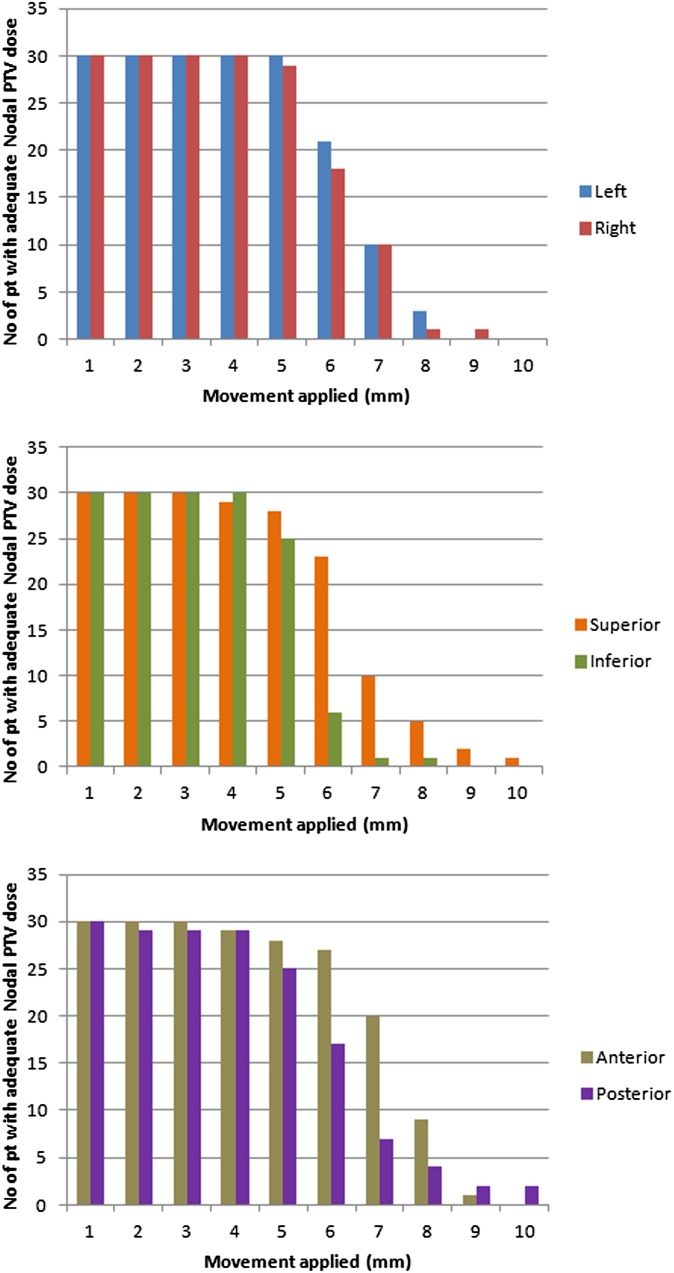
• 95% dose is maintained to at least 95% of the nodal PTV with shifts from the isocentre of ≤5 mm in the right, left, superior and inferior directions, 3 mm anteriorly and 4 mm posteriorly in all cases.
• 99% dose is maintained to at least 90% of the nodal PTV with shifts from the isocentre of ≤4 mm in the right, inferior, anterior and posterior directions, 5 mm left and 3 mm superiorly.
• 100% dose is maintained to at least 50% of the nodal PTV volume with shifts from the isocentre of ≤6 mm in the left and superior directions, 5 mm right, 7 mm inferiorly, 4 mm anteriorly and 2 mm posteriorly.
In 97% (n = 29) of patients, all PTV constraints were maintained when movement was ≤5 mm laterally and 4 mm longitudinally and vertically.
Figure 1 illustrates the number of patients who meet all PTV constraints when incremental displacements up to 10 mm are applied in the lateral, longitudinal and vertical planes.
Figure 1.
The number of patients meeting all planned target volume (PTV) constraints with 1-mm incremental movements applied in each direction. No, number; pt, patients.
Image-guided radiotherapy database analysis
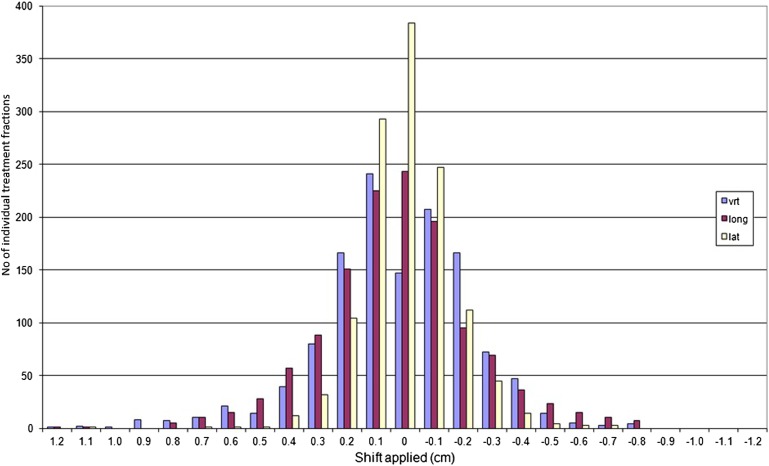
36 patients with 1278 MV portal images are included in the IGRT database, confirming a normally distributed pattern of position discrepancy between pelvic bones and fiducial markers.
Figure 2 illustrates the distribution of fiducial marker to bony match offsets. The mean difference between bony match and fiducial match results is 0 mm in each direction as expected, and the standard deviations are 0.2, 0.3 and 0.3 in the lateral, anteroposterior and superio-inferior directions, respectively.
Figure 2.
The spread of daily bony to fiducial offsets recorded in the image-guided radiotherapy database. lat, lateral; long, longitudinal; no, number; vrt, vertical.
The mean offsets for each patient with all directions combined were 0 mm in 30%, 1 mm in 45%, 2 mm in 15%, 3 mm in 7% and 4 mm in 2%.
Combined dosimetric and image-guided radiotherapy database analysis
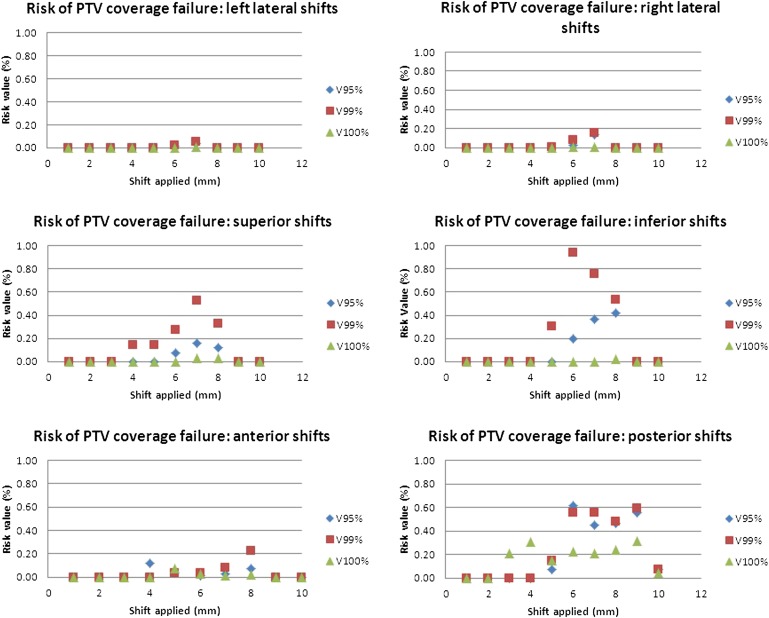
Figure 3 shows the combined analysis used to calculate the subsequent overall risk of failure of maintaining the set constraint parameters in each fraction of treatment.
Figure 3.
The risk of lymph node planned target volume (PTV) being reduced on any given fraction of radiation. V95%, 95% dose (52.25 Gy) maintained to at least 95% of the nodal PTV; V99%, 99% dose (55.45 Gy) maintained to at least 90% of the nodal PTV; V100%, 100% dose maintained to at least 50% of the nodal PTV.
The likelihood of offsets in the left, right and anterior directions occurring and resulting in a failure to cover the PTV was <0.25%. The likelihood of superior, inferior and posterior offsets occurring and resulting in inadequate coverage was slightly higher but remained <1%.
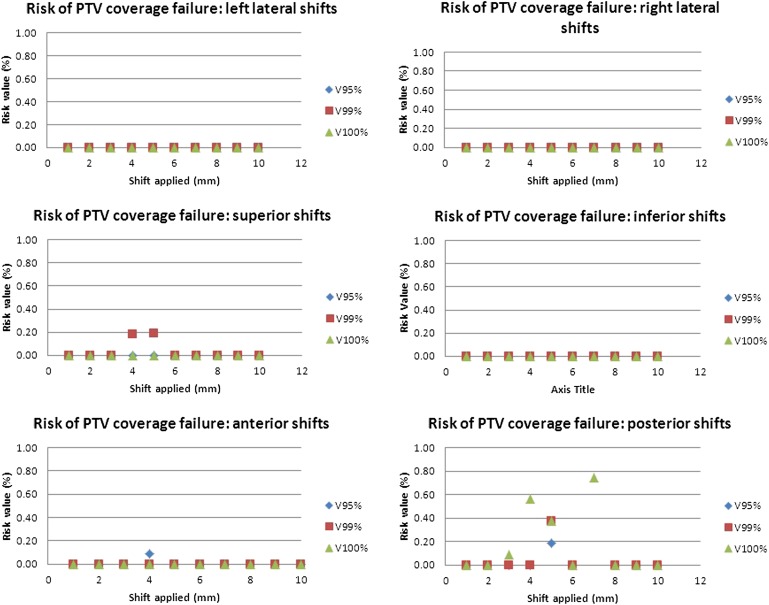
The risk of reduced dose to lymph node PTV had those with a mean offset been treated consistently in that position throughout treatment was <0.2% in all directions other than in the posterior direction, where it reaches 0.8%. Figure 4 demonstrates the risk of underdosing of lymph node PTV using the mean offsets in each direction present in our IGRT database.
Figure 4.
The risk of lymph node planned target volume (PTV) being reduced had the patients with a mean offset been treated with that offset consistently throughout the treatment course.
DISCUSSION
Our study uses a large patient cohort, with a strong IGRT database of 1278 offsets recorded to assess the impact of fiducial-based IG-IMRT on lymph node dose. This therefore strengthens the evidence that IG-IMRT does not impact clinically on the nodal dose. Specifically, our results correlate very closely with the <1.5% decrease in lymph node dose published by Hsu et al20 and the 2% decrease in coverage of D95% reported by Chung et al11 with D95% dropping to 47.8 Gy for a prescribed dose of 48.6 Gy. Our results suggest less impact on lymph node dose than that published by Rossi et al,21 which may reflect one of the key limitations of our study, which is not taking into account the multidirectional nature of movements which are applied throughout a course of IGRT. Despite different analysis techniques, our study further confirms that the use of IG-IMRT is safe within the documented population, as there is a <1% risk of underdosing lymph node PTV on any given fraction.
The interpretation and clinical application of our data is dependent on a number of factors.
• The CTV to PTV margin encompasses a large number of errors, including lymph node motion independent to the bones, interclinician variation, planning system and delivery uncertainties. Many of these are centre dependent, or clinician or case dependent, as in our study population group. In our centre, the CTV–PTV margin around lymph nodes is reduced until small bowel constraints can be achieved to minimize toxicity owing to the questionable benefit of pelvic nodal irradiation. In keeping with this strategy, within our case cohort, there was a significant variation in the margins applied to the lymph node CTV. By calculating PTV coverage, we could be sure that, irrelevant of margins used, our lymph nodes received a full dose. We also felt that, by analysing PTV, the results would be applicable to other centres, which may use different margins.
• It is a limitation of our study that only unidirectional movements were assessed; therefore, we cannot extrapolate accurately the impact of multidirectional movements that are often applied when using IGRT or rotational movement that although not applied can be present. The mean offsets for each patient with all directions combined in the IGRT database (0 mm in 30%, 1 mm in 45%, 2 mm in 15%, 3 mm in 7% and 4 mm in 2%) serve to highlight that multidirectional movements that occurred were generally much smaller than the distances we covered in the unidirectional analysis.
• It is not confidently known what dose must be delivered to lymph nodes in prostate cancer to treat microscopic disease. The PFS benefit with lymph node irradiation in prostate cancer, from the RTOG 9413,20 was from 50.4 Gy delivered in 1.8 Gy per fraction over 28 fractions (38.8 Gy, 2-Gy equivalent using α/β = 1.5), whereas a more commonly reported dose is 45 Gy in 25 fractions (34.7 Gy, 2-Gy equivalent).17,25 The findings of this study can be related to any of these doses as the PTV constraints are presented as percentage doses. In our population with a prescribed dose to lymph nodes of 55 Gy in 37 fractions (46 Gy, 2-Gy equivalent), even if the dose is reduced by 1%, it will remain higher than doses used in other studies. Therefore, with our prescribed dose, it is extremely unlikely that lymph nodes would receive an equivalent dose of <45 Gy in 1.8 fractions, which is an accepted lymph node dose.
• Finally, the IGRT database used is our local database where all patients underwent a strict bowel and bladder protocol, minimizing fiducial-based shifts. Any variation in this protocol may incur different bony to fiducial offsets and as such different results. The use of more invasive techniques, e.g. insertion of a balloon system for prostate–rectum separation, which has been shown to decrease rectal radiation dose delivered,25 would possibly yield different results too. Should a strategy of IG-IMRT be implemented based on these results, a local bony to fiducial offset analysis should be performed prior to implementation to ensure comparable results.
Following these results, the authors plan to implement fiducial-based IG-IMRT. This will enable a reduction in the CTV to PTV margin around the prostate with the associated reduction in rectal toxicity. The results also raise the possibility of reducing CTV to PTV margins around the lymph nodes. We plan to prospectively assess CTV lymph node coverage in this group with a consistent smaller margin with the aim of further reducing associated pelvic toxicity.
CONCLUSIONS
This study confirms the safety of changing practice from a bony match to fiducial-based IG-IMRT. This will allow a reduction of the CTV to PTV margin of the prostate volume and consequent reduction in rectal toxicity.
REFERENCES
- 1.Sheets NC, Goldin GH, Meyer AM, Wu Y, Chang Y, Stürmer T, et al. Intensity-modulated radiation therapy, proton therapy, or conformal radiation therapy and morbidity and disease control in localized prostate cancer. JAMA 2012; 307: 1611–20. doi: 10.1001/jama.2012.460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kupelian PA, Langen KM, Zeidan OA, Meeks SL, Willoughby TR, Wagner TH, et al. Daily variations in delivered doses in patients treated with radiotherapy for localized prostate cancer. Int J Radiat Oncol Biol Phys 2006; 66: 876–82. doi: 10.1016/j.ijrobp.2006.06.011 [DOI] [PubMed] [Google Scholar]
- 3.Polat B, Guenther I, Wilbert J, Goebel J, Sweeney RA, Flentje M, et al. Intra-fractional uncertainties in image-guided intensity-modulated radiotherapy (IMRT) of prostate cancer. Strahlenther Onkol 2008; 184: 668–73. doi: 10.1007/s00066-008-1875-6 [DOI] [PubMed] [Google Scholar]
- 4.Crook JM, Raymond Y, Salhani D, Yang H, Esche B. Prostate motion during standard radiotherapy as assessed by fiducial markers. Radiother Oncol 1995; 37: 35–42. [DOI] [PubMed] [Google Scholar]
- 5.Padhani AR, Khoo VS, Suckling J, Husband JE, Leach MO, Dearnaley DP. Evaluating the effect of rectal distension and rectal movement on prostate gland position using cine MRI. Int J Radiat Oncol Biol Phys 1999; 44: 525–33. [DOI] [PubMed] [Google Scholar]
- 6.Zellars RC, Roberson PL, Strawderman M, Zhang D, Sandler HM, Ten Haken RK, et al. Prostate position late in the course of external beam therapy: patterns and predictors. Int J Radiat Oncol Biol Phys 2000; 47: 655–60. [DOI] [PubMed] [Google Scholar]
- 7.Ten Haken RK, Forman JD, Heimburger DK, Gerhardsson A, McShan DL, Perez-Tamayo C, et al. Treatment planning issues related to prostate movement in response to differential filling of the rectum and bladder. Int J Radiat Oncol Biol Phys 1991; 20: 1317–24. [DOI] [PubMed] [Google Scholar]
- 8.Chung PW, Haycocks T, Brown T, Cambridge Z, Kelly V, Alasti H, et al. On-line aSi portal imaging of implanted fiducial markers for the reduction of interfraction error during conformal radiotherapy of prostate carcinoma. Int J Radiat Oncol Biol Phys 2004; 60: 329–34. [DOI] [PubMed] [Google Scholar]
- 9.International Commission on Radiation Units and Measurements. Prescribing, recording, and reporting photon beam therapy. ICRU Report 62 (supplement to ICRU Report 50). Bethesda, MD: ICRU; 1999.
- 10.Nederveen AJ, Dehnad H, van der Heide UA, van Moorselaar RJ, Hofman P, Lagendijk JJ. Comparison of megavoltage position verification for prostate irradiation based on bony anatomy and implanted fiducials. Radiother Oncol 2003; 68: 81–8. [DOI] [PubMed] [Google Scholar]
- 11.Chung HT, Xia P, Chan LW, Park-Somers E, Roach M 3rd. Does image-guided radiotherapy improve toxicity profile in whole pelvic-treated high-risk prostate cancer? Comparison between IG-IMRT and IMRT. Int J Radiat Oncol Biol Phys 2009; 73: 53–60. doi: 10.1016/j.ijrobp.2008.03.015 [DOI] [PubMed] [Google Scholar]
- 12.McNair HA, Hansen VN, Parker CC, Evans PM, Norman A, Miles E, et al. A comparison of the use of bony anatomy and internal markers for offline verification and an evaluation of the potential benefit of online and offline verification protocols for prostate radiotherapy. Int J Radiat Oncol Biol Phys 2008; 71: 41–50. [DOI] [PubMed] [Google Scholar]
- 13.Roach M 3rd, DeSilvio M, Valicenti R, Grignon D, Asbell SO, Lawton C, et al. Whole-pelvis, “mini-pelvis,” or prostate-only external beam radiotherapy after neoadjuvant and concurrent hormonal therapy in patients treated in the Radiation Therapy Oncology Group 9413 trial. Int J Radiat Oncol Biol Phys 2006; 66: 647–53. [DOI] [PubMed] [Google Scholar]
- 14.Asbell SO, Martz KL, Shin KH, Sause WT, Doggett RL, Perez CA, et al. Impact of surgical staging in evaluating the radiotherapeutic outcome in RTOG #77-06, a phase III study for T1BN0M0 (A2) and T2N0M0 (B) prostate carcinoma. Int J Radiat Oncol Biol Phys 1998; 40: 769–82. [DOI] [PubMed] [Google Scholar]
- 15.Bagshaw MA. Radiotherapeutic treatment of prostatic carcinoma with pelvic node involvement. Urol Clin North Am 1984; 11: 297–304. [PubMed] [Google Scholar]
- 16.Nutting CM, Convery DJ, Cosgrove VP, Rowbottom C, Padhani AR, Webb S, et al. Reduction of small and large bowel irradiation using an optimized intensity-modulated pelvic radiotherapy technique in patients with prostate cancer. Int J Radiat Oncol Biol Phys 2000; 48: 649–56. [DOI] [PubMed] [Google Scholar]
- 17.Wang-chesebro A, Xia P, Coleman J, Akazawa C, Roach M 3rd. Intensity-modulated radiotherapy improves lymph node coverage and dose to critical structures compared with three-dimensional conformal radiation therapy in clinically localized prostate cancer. Int J Radiat Oncol Biol Phys 2006; 66: 654–62. [DOI] [PubMed] [Google Scholar]
- 18.Kaidar-Person O, Roach M 3rd, Créhange G. Whole-pelvic nodal radiation therapy in the context of hypofractionation for high-risk prostate cancer patients: a step forward. Int J Radiat Oncol Biol Phys 2013; 86: 600–5. doi: 10.1016/j.ijrobp.2013.02.006 [DOI] [PubMed] [Google Scholar]
- 19.Landoni V, Saracino B, Marzi S, Gallucci M, Petrongari MG, Chianese E, et al. A study of the effect of setup errors and organ motion on prostate cancer treatment with IMRT. Int J Radiat Oncol Biol Phys 2006; 65: 587–94. doi: 10.1016/j.ijrobp.2006.01.021 [DOI] [PubMed] [Google Scholar]
- 20.Hsu A, Pawlicki T, Luxton G, Hara W, King CR. A study of image-guided intensity-modulated radiotherapy with fiducials for localized prostate cancer including pelvic lymph nodes. Int J Radiat Oncol Biol Phys 2007; 68: 898–902. doi: 10.1016/j.ijrobp.2007.02.030 [DOI] [PubMed] [Google Scholar]
- 21.Rossi PJ, Schreibmann E, Jani AB, Master VA, Johnstone PA. Boost first, eliminate systematic error, and individualize CTV to PTV margin when treating lymph nodes in high-risk prostate cancer. Radiother Oncol 2009; 90: 353–8. doi: 10.1016/j.radonc.2008.09.021 [DOI] [PubMed] [Google Scholar]
- 22.van Herk M, Remeijer P, Rasch C, Lebesque JV. The probability of correct target dosage: dose-population histograms for deriving treatment margins in radiotherapy. Int J Radiat Oncol Biol Phys 2000; 47: 1121–35. [DOI] [PubMed] [Google Scholar]
- 23.Roach M. Equations for predicting the pathologic stage of men with localized prostate cancer using the preoperative prostate specific antigen. J Urol 1993; 50: 1923–24. [DOI] [PubMed] [Google Scholar]
- 24.Taylor A, Rockall AG, Reznek RH, Powell ME. Mapping pelvic lymph nodes: guidelines for delineation in intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 2005; 63: 1604–12. doi: 10.1016/j.ijrobp.2005.05.062 [DOI] [PubMed] [Google Scholar]
- 25.Gez E, Cytron S, Yosef RB, London D, Corn BW, Alani S, et al. Application of an interstitial and biodegradable balloon system for prostate-rectum separation during prostate radiotherapy: a prospective multi-center study. Radiat Oncol 2013; 8: 96–102. [DOI] [PMC free article] [PubMed] [Google Scholar]