Abstract
Objective:
Osteoid osteoma (OO) accounts for approximately 10–12% of all benign bone tumours and 3% of all bone tumours. Spinal involvement appears in 10–25% of all cases. The purpose of this study was to evaluate the safety and efficacy of CT-guided radiofrequency (RF) ablation in the treatment of spinal OOs and report our experience.
Methods:
13 patients suffering from spinal OO and treated at the authors' institution using CT-guided RF ablation were retrospectively evaluated. The RF probe was introduced through a 11-G Jamshidi® needle, and the lesion was heated at 90 °C for 6 min.
Results:
All procedures were considered technically successful as the correct positioning of the probe was proven by CT. 11 of the 13 patients reported pain relief after RF ablation. In two cases, RF ablation was repeated 1 month after the first procedure. Pain relief was achieved in both cases after the second procedure. No recurrence was reported throughout the follow-up. No complications like skin burn, soft-tissue haematoma, infection, vessel damage or neurological deficit were reported.
Conclusion:
This study demonstrates that CT-guided percutaneous RF ablation is a safe and effective method for the treatment of spinal OOs.
Advances in knowledge:
The data of this study support the efficacy and safety of the recently applied CT-guided percutaneous RF ablation technique for the treatment of spinal OOs.
Osteoid osteoma (OO) represents a benign bone tumour first described by Jaffe1 in 1935. The lesion accounts for approximately 10–12% of all benign bone tumours and 3% of all bone tumours. It is characterized by a nidus, consisting of osteoid, osteoblasts and fibrovascular stroma, surrounded by sclerotic bone usually measuring <1.5 cm in diameter. OOs are characteristically seen in children and young adults with a predilection for long bones, particularly in lower extremities.2 Spinal involvement usually affecting the posterior elements appears in 10–25% of all cases.3,4 The typical symptom is localized pain typically worsening at night, ameliorated by the administration of salicylates (acetylsalicylic acid) or non-steroidal anti-inflammatory drugs (NSAIDs). In spinal cases of OO, radiation of pain distally to the lesion site might simulate radiculopathy similar to disc herniation especially if the lesion is located close to a nerve root. Painful antalgic scoliosis is frequent in thoracolumbar lesions in children and adolescents.5,6 Spinal lesions are usually difficult to diagnose, and the reported delay from presentation to final diagnosis and treatment can be as long as 24 months in some cases.7–9 Neurologic deficit does not generally appear.
In the past, conventional surgical excision and more recently minimally invasive surgery techniques were the treatment of choice in cases of spinal OOs when conservative treatment with anti-inflammatory and salicylates fails or is contraindicated.10–15
Rosenthal et al16 first introduced percutaneous radiofrequency (RF) ablation for the treatment of OOs. The effectiveness of RF ablation of OOs localized in the extremities and pelvis has been proven by many studies.16–19
Percutaneous RF ablation for the treatment of spinal OOs is not widely used, probably owing to the potential danger to the adjacent neural and vascular elements. In recent years, however, some clinical studies reported good results in the management of spinal OOs using CT-guided RF ablation.8,20–23
The purpose of this study was to evaluate the safety and efficacy of CT-guided RF ablation in the treatment of spinal OOs and report our experience.
METHODS AND MATERIALS
Between November 2009 and February 2013, after receiving approval from our Institutional Review Board, 13 patients diagnosed with spinal OO were treated at the authors' institution (KAT Hospital, Athens, Greece) using CT-guided RF ablation. Patients' records were retrospectively evaluated. Seven males and six females with a mean age of 19.3 years (range, 12–26 years) underwent RF ablation for OO. The distribution of OOs in the study group was the following: cervical (n = 2), thoracic (n = 4), lumbar (n = 5) and sacral spine (n = 2) (Table 1). The duration of symptoms prior to RF ablation ranged from 5 to 16 months (mean time, 13.1 months). Plain radiography, CT and MRI were performed on all patients. In some cases, bone scintigraphy was additionally performed. All patients underwent needle biopsy that confirmed the diagnosis of OO. None of the patients had undergone any invasive therapeutical procedure prior to ablation treatment.
Table 1.
Summary of patient information and treatment follow-up
| Case number | Sex | Age (years) | Spinal location | Symptom | VAS score BP | VAS score AP | Time required for pain relief after RF ablation | Repeated RF ablation | Follow-up time (months) | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 19 | Laminae | L3 | Local pain | 8 | 0 | Day 1 | No | 38 |
| 2 | M | 26 | Pedicle | Th9 | Local pain | 10 | 0 | Day 3 | No | 36 |
| 3 | M | 21 | Lateral mass | C5 | Local pain/torticollis | 9 | 0 | Day 1 | No | 30 |
| 4 | F | 26 | Pedicle | L4 | Local/radicular pain | 8 | 0 | Day 5 | No | 25 |
| 5 | F | 22 | Body | C2 | Local pain | 9 | 0 | Day 1 | No | 24 |
| 6 | F | 14 | Laminae | Th7 | Local pain/scoliosis | 9 | 0 | Day 1 | No | 25 |
| 7 | M | 18 | Pedicle | L2 | Local pain | 10 | 6 | Yes | 25 | |
| 8 | M | 13 | Laminae | S3 | Local pain | 7 | 0 | Day 1 | No | 24 |
| 9 | F | 12 | Laminae | Th8 | Local pain/scoliosis | 8 | 0 | Day 3 | No | 20 |
| 10 | F | 25 | Pedicle | L4 | Local pain | 10 | 7 | Yes | 18 | |
| 11 | F | 21 | Laminae | L5 | Local/radicular pain | 9 | 0 | Day 1 | No | 18 |
| 12 | M | 14 | Laminae | Th1 | Local pain | 8 | 0 | Day 1 | No | 12 |
| 13 | M | 20 | Laminae | S1 | Local pain | 7 | 0 | Day 1 | No | 6 |
| 7M/6F: mean age, 19.3 years | Mean BP VAS score, 8.6 | |||||||||
AP, after procedure; BP, before procedure; C, cervical; F, female; L, lumbar; M, male; RF, radiofrequency; Th, thoracic; VAS, visual analogue scale.
Presenting symptoms other than localized pain were painful torticollis in one patient, antalgic scoliosis in two patients and radicular pain in two patients.
Neurological examination and pain evaluation using the visual analogue scale (VAS) were performed for each patient prior to the procedure, before discharge, at 1 week, and 1, 3 and 6 months after the procedure and at 6-month interval thereafter. CT was applied to identify the location, evaluate the dimensions of the nidus, further assess the proximity of the spinal cord and vessel elements to the tumour and plan the trajectory of the needle for the RF ablation. Follow-up CT evaluation was performed at 1 and 2 years after the procedure (Figures 1–3). Patients were evaluated for a minimum of 6–39 months after ablation, with a mean follow-up time of 23.1 months. No patient was lost to follow-up.
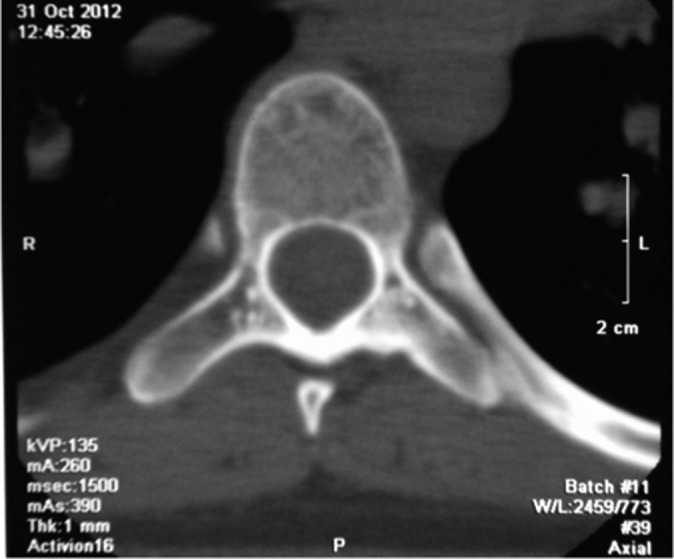
Figure 1.

A 26-year-old male patient with osteoid osteoma localized on the pedicle of the ninth thoracic vertebra (arrow).
Figure 3.
The same male patient as in Figure 1 30 months after the ablation remains free of symptoms.
Figure 2.
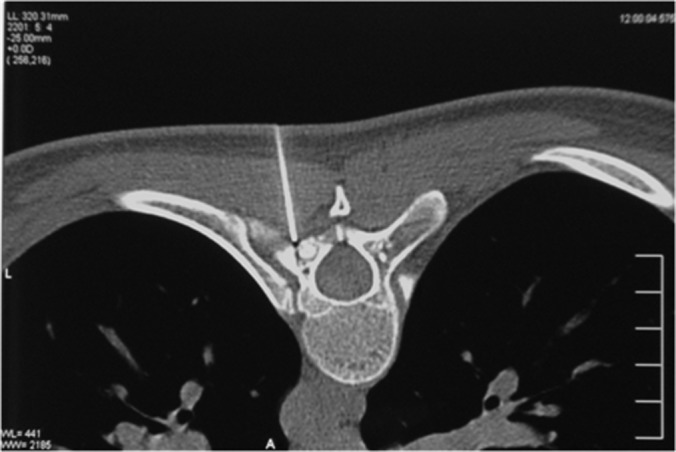
The same male patient as in Figure 1 during the procedure of radiofrequency ablation. The correct positioning of the guiding needle was confirmed by CT scan.
Technique
All procedures were performed under general anaesthesia in the radiology department by the same radiologist. A single dose of intravenous antibiotics was administrated 2 h prior to the procedure to all patients according to our study protocol. The procedure was performed taking into account the technical considerations described by Pinto et al.24 The lesion was localized on fine-section CT (slice thickness of 1.2 mm). Before entering the guide needle, vessel enhancement was achieved by intravenously injecting 60 ml of contrast medium (Ultravist®; Bayer Schering Pharma AG, Berlin, Germany) through an 18-G catheter. This step of the procedure is important in order to identify any vessel anatomical variants and avoid damage to vessels close to the nidus. The skin was disinfected using 10% povidone iodine solution, sterile drapes were applied and a 21-G spinal needle was used as a guide needle in order to precisely localize the nidus and find the correct trajectory so that the neurovascular elements were avoided. A quick CT check confirmed that the needle was appropriately positioned in the nidus. A bolus of 8–10 ml of sterile water was injected over a period of 1 min in the area near the nidus in order to reduce the possible thermal injury to the adjacent neurovascular structures. Additionally, 2 ml of 7.5% ropivacaine was infiltrated prior to ablation at the lesion site. A small skin incision was made, and a Cook trephine 11-G needle 15 cm in length (Osteo-Site Bone Access Needle Set Murphy M2; Cook, Bjaeverskov, Denmark) was inserted in the nidus. Afterwards, the RF probe was introduced through the needle at the site of the lesion. A non-cooled monopolar tip Rita StarBurst® XL electrosurgical device (Rita Medical Systems, Mountain View, CA) with nine deployable electrodes was introduced into the nidus through the Cook needle. The RF probe was connected to the Rita 1500X (Rita Medical Systems), and the lesion was heated at 90 °C for 6 min. The generator was set to 150 W. The probe was set to ablate at a ray of 5 mm from the tip. Caution was taken to ensure that the tip of the probe was 1 cm away from the tip of the penetrating needle and that the exposed probe tip did not come in contact with the penetration needle. When the procedure was completed, the electrode array and the Cook needle were removed, and a sterile drape of the skin was performed. The average time of the intervention including anaesthesia and the ablation was approximately 60 min. After the procedure, NSAIDs were avoided, and the only analgesic drug administered within the first 24 h was paracetamol in an effort to evaluate the effect of the procedure on pain management.
RESULTS
For all patients, histopathological confirmation of the diagnosis was obtained prior to ablation. All procedures were considered technically successful as proof of the correct positioning of the probe at the lesion site was obtained by CT, and a temperature of 90 °C was reached and maintained for 6 min.
No complications, such as skin burn, soft-tissue haematoma, infection, vessel damage or neurological deficit, were reported. Prior to the procedure, the mean VAS score was 8.6 (ranging from 7 to 10). 11 of the 13 patients reported no pain 1 week after the RF ablation (VAS score 0). In eight patients, pain ceased within 24 h after the intervention, whereas in three patients pain disappeared completely 3–5 days after ablation, although symptom improvement was noted within the first 24 h. In two patients, pain improved only slightly at the 1-month follow-up (VAS score >6) (Table 1). For these patients, RF ablation was repeated 1 month after the first procedure. In both patients, the diameter of the nidus was >1 cm and in the second procedure two RF probes were used simultaneously (the probe used in our study ablated at a ray of 5 mm). In both cases, the intervention achieved complete remission of pain 24 h after the second procedure. In total, 15 RF ablations were performed in 13 patients. Complete remission of pain (VAS score 0) was achieved in all patients, and no recurrence was reported throughout the follow-up, including the two cases for which the ablation was repeated.
In one case where painful torticollis was the presenting symptom, it disappeared after the ablation. Also in one of the two cases in which the nidus caused painful scoliosis, the deformity subsided almost completely after the intervention. In the second case of painful scoliosis, the deformity improved only slightly and bracing was required.
DISCUSSION
Spinally located OOs might occur in up to 25% of all cases, predominantly in the lumbar spine and the posterior elements.3,25
Scoliosis is a commonly associated deformity of OOs and appears in up to 70% of the thoracolumbar spinal lesions. Painful scoliosis is caused by muscle spasm owing to local irritation. When scoliosis is present, the nidus is located in the concavity of the apex of the curve. This deformity might become permanent in some cases.5,6,11,26,27 In our study, two female patients with the nidus located in the pedicle of the seventh and eighth thoracic vertebrae, respectively, presented painful scoliosis. In both patients, the RF ablation was successful in managing pain but in only one case the deformity decreased. In the other patient, scoliosis remained almost unchanged.
In one male patient where the nidus was located on the lateral mass of the fifth cervical vertebra, torticollis improved after successful RF ablation. To our knowledge, there has been no documented report of torticollis caused by OO.
Treatment of OOs may be conservative owing to characteristic pain relief after administration of salicylates or NSAIDs. Spontaneous healing or healing after long-term administration of medication has been reported.28–30 However, some patients cannot tolerate long-term medication regimens owing to the side effects of salicylates and NSAIDs. In the past, complete surgical excision of the nidus had been the treatment of choice. Surgical treatment varies from local resection with a burr and curettage to wide en bloc resection. In cases of spinally located OOs, there is an increased risk of spinal cord, nerve root or vertebral artery damage, especially in cases of cervical location of the nidus. Additionally, intra-operative identification of the lesion may be difficult, resulting in incomplete resection. Navigation systems have been developed to facilitate intra-operative localization of the nidus; however, secondary instability following wide resection might necessitate spinal fusion.2,3,11,31–33
Recently, new minimally invasive techniques have been developed for the treatment of OOs. Percutaneous treatment options include RF ablation, percutaneous CT-guided excision using trephines and needles,34 drilling of the nidus 35 and laser photocoagulation.36–40 Percutaneous RF ablation of OOs was first described in 1992 by Rosental et al.41 The first report of an OO located in the lumbar spine treated by RF ablation was made in 1998 by Osti and Sebben.42 Since then, several studies have reported excellent results with the use of RF for the treatment of OOs that are comparable with those of surgical resection.7,8,16,20–23,43,44
Many physicians avoided using RF ablation for the treatment of spinal OOs owing to the risk of neural injury. In 2000, Dupuy et al22 published their experimental findings of RF ablation in the vertebral bodies of five porcine models. Their study concluded that in cases where cortical bone is present between the lesion and the neural elements, it has an insulating effect. In addition, this study demonstrated that the heat provoked by the RF is decreased locally by the presence of a rich epidural venous plexus and the cerebrospinal fluid circulation. This protective effect on neural elements of the spine against excessive heating during RF ablation of spinal OOs has also been proven by other studies in animal and human models.43,45 In order to reduce even more the likelihood of the thermal damage to neural elements adjacent to the nidus before the ablation, a bolus of 8–10 ml of sterile water was infused in the area near the nidus as also described by other authors.21,23,36 We do not consider a cool tip system necessary because it might increase the risk of neural injury as it enlarges the size of the treatment zone and makes the size of ablation unpredictable. Additionally, it prevents temperature measurements during ablation, a fact that makes monitoring of the procedure difficult.7,46,47
No neural damage was observed. Similar to Liu et al,48 the results of this study demonstrate that RF ablation of spinal OOs represents a safe procedure for the neural elements as long as all the necessary precautions are taken.
All procedures were performed under general anaesthesia because it made the procedure easier for both the physician and the patient, as the patients did not experience any pain during the ablation, and perfect immobilization was ensured, something that is crucial for the correct measurements and placement of the penetrating needle and probe and the maintenance of the correct positioning throughout the ablation. Like other authors,8,21,23 we recommend general anaesthesia for the RF ablation of spinal OOs.
Additionally, before planning the pathway for the penetration needle, an intravenous contrast medium was administered in order to achieve vessel enhancement. We found that this step of the procedure was important especially in RF ablation of cervical located OOs in order to locate any anatomical variants of the vertebral artery and to plan a safe trajectory of the needle.
In both patients of our study, whose pain was slightly ameliorated by the ablation and a second procedure was performed, the diameter of the nidus was >1 cm. We consider that the success of the second procedure is owing to the fact that two RF probes were used simultaneously, the probes used ablated at a ray of 5 mm.
No complications, such as skin burn, soft-tissue haematoma, infection, vessel damage or neurological deficit, were documented in our study.
CT-guided percutaneous RF ablation is a minimally invasive procedure. Compared with open surgical excision of spinal OOs, by performing RF ablation the lesion is precisely located under CT guidance, shorter anaesthesia times are required, blood loss, tissue exposure and damage are minimal and there is no need for fusion after excision. Shorter hospitalization and recovery periods are also required.21,23,47 Initial follow-up should be based on patients' symptoms to detect persistent pain requiring a second thermal ablation. Following the initial period, patients should be evaluated clinically and radiologically at a regular basis to assess infilling of the nidus with sclerotic bone. Surgery-related complications such as infection, vascular damage or spontaneous fusion with deformity are avoided.49 CT-guided percutaneous RF ablation has similar results in terms of efficacy of treatment and recurrence to those of open surgery for spinal located OOs.4,16,21,23,46,50
Despite the efforts to ensure the validity of this study, certain limitations exist. The study is retrospective, and the study group is relatively small to draw safe conclusions. Additionally, although no recurrences were reported, mean follow-up was almost 2 years.
CONCLUSIONS
This study demonstrates that CT-guided percutaneous RF ablation is a safe and an effective method for the treatment of spinally located OOs with excellent mean-time results. Several technical considerations should be taken into account when treating spinal OOs by RF ablation. We believe that CT-guided percutaneous RF ablation is the treatment of choice for the management of spinal OOs. Further studies with larger series of patients and long-term follow-up are needed in order to demonstrate the safety, the efficacy and the recurrence rate of the procedure in the treatment of spinal OOs.
REFERENCES
- 1.Jaffe HL. Osteoid osteoma, a benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg 1935; 31: 709–28. [Google Scholar]
- 2.Cantwell CP, Obyrne J, Eustace S. Current trends in treatment of osteoid osteoma with an emphasis on radiofrequency ablation. Eur Radiol 2004; 14: 607–17. doi: 10.1007/s00330-003-2171-6 [DOI] [PubMed] [Google Scholar]
- 3.Raskas DS, Graziano GP, Herzenberg JE, Heidelberger KP, Hensinger RN. Osteoid osteoma and osteoblastoma of the spine. J Spinal Disord 1992; 5: 204–11. [DOI] [PubMed] [Google Scholar]
- 4.Hadjipavlou AG, Lander PH, Marchesi D, Katonis PG, Gaitanis IN. Minimally invasive surgery for ablation of osteoid osteoma of the spine. Spine (Phila Pa 1976) 2003; 28: E472–7. doi: 10.1097/01.BRS.0000092386.96824.DB [DOI] [PubMed] [Google Scholar]
- 5.Keim HA, Reina EG. Osteoid-osteoma as a cause of scoliosis. J Bone Joint Surg Am 1975; 57: 159–63. [PubMed] [Google Scholar]
- 6.Saifuddin A, White J, Sherazi Z, Shaikh MI, Natali C, Ransford AO. Osteoid osteoma and osteoblastoma of the spine. Factors associated with the presence of scoliosis. Spine (Phila Pa 1976) 1998; 23: 47–53. [DOI] [PubMed] [Google Scholar]
- 7.Rybak LD, Gangi A, Buy X, La Rocca Vieira R, Wittig J. Thermal ablation of spinal osteoid osteomas close to neural elements: technical considerations. AJR Am J Roentgenol 2010; 195: W293–8. doi: 10.2214/AJR.10.4192 [DOI] [PubMed] [Google Scholar]
- 8.Cové JA, Taminiau AH, Obermann WR, Vanderschueren GM. Osteoid osteoma of the spine treated with percutaneous computed tomography-guided thermocoagulation. Spine (Phila Pa 1976) 2000; 25: 1283–6. [DOI] [PubMed] [Google Scholar]
- 9.Yildiz Y, Bayrakci K, Altay M, Saglik Y. Osteoid osteoma: the results of surgical treatment. Int Orthop 2001; 25: 119–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marcove RC, Heelan RT, Huvos AG, Healey J, Lindeque BG. Osteoid osteoma. Diagnosis, localization, and treatment. Clin Orthop Relat Res 1991; 267: 197–201. [PubMed] [Google Scholar]
- 11.Ozaki T, Liljenqvist U, Hillmann A, Halm H, Lindner N, Gosheger G. Osteoid osteoma and osteoblastoma of the spine: experiences with 22 patients. Clin Orthop Relat Res 2002; 397: 394–402. [DOI] [PubMed] [Google Scholar]
- 12.Fenichel I, Garniack A, Morag B, Palti R, Salai M. Percutaneous CT-guided curettage of osteoid osteoma with histological confirmation: a retrospective study and review of the literature. Int Orthop 2006; 30: 139–42. doi: 10.1007/s00264-005-0051-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Donahue F, Ahmad A, Mnaymneh W, Pevsner NH. Osteoid osteoma. Computed tomography guided percutaneous excision. Clin Orthop Relat Res 1999; 366: 191–6. [PubMed] [Google Scholar]
- 14.Parlier-Cuau C, Champsaur P, Nizard R, Hamze B, Laredo JD. Percutaneous removal of osteoid osteoma. Radiol Clin North Am 1998; 36: 559–66. [DOI] [PubMed] [Google Scholar]
- 15.Sans N, Galy-Fourcade D, Assoun J, Jarlaud T, Chiavassa H, Bonnevialle P, et al. Osteoid osteoma: CT-guided percutaneous resection and follow-up in 38 patients. Radiology 1999; 212: 687–92. doi: 10.1148/radiology.212.3.r99se06687 [DOI] [PubMed] [Google Scholar]
- 16.Rosenthal DI, Hornicek FJ, Wolfe MW, Jennings LC, Gebhardt MC, Mankin HJ. Percutaneous radiofrequency coagulation of osteoid osteoma compared with operative treatment. J Bone Joint Surg Am 1998; 80: 815–21. [DOI] [PubMed] [Google Scholar]
- 17.de Berg JC, Pattynama PM, Obermann WR, Bode PJ, Vielvoye GJ, Taminiau AH. Percutaneous computed-tomography-guided thermocoagulation for osteoid osteomas. Lancet 1995; 346: 350–1. [DOI] [PubMed] [Google Scholar]
- 18.Rimondi E, Mavrogenis AF, Rossi G, Ciminari R, Malaguti C, Tranfaglia C. Radiofrequency ablation for non-spinal osteoid osteomas in 557 patients. Eur Radiol 2012; 22: 181–8. doi: 10.1007/s00330-011-2240-1 [DOI] [PubMed] [Google Scholar]
- 19.Woertler K, Vestring T, Boettner F, Winkelmann W, Heindel W, Lindner N. Osteoid osteoma: CT-guided percutaneous radiofrequency ablation and follow-up in 47 patients. J Vasc Interv Radiol 2001; 12: 717–22. [DOI] [PubMed] [Google Scholar]
- 20.Laus M, Albisinni U, Alfonso C, Zappoli FA. Osteoid osteoma of the cervical spine: surgical treatment or percutaneous radiofrequency coagulation? Eur Spine J 2007; 16: 2078–82. doi: 10.1007/s00586-007-0478-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Klass D, Marshall T, Toms A. CT-guided radiofrequency ablation of spinal osteoid osteomas with concomitant perineural and epidural irrigation for neuroprotection. Eur Radiol 2009; 19: 2238–43. doi: 10.1007/s00330-009-1404-8 [DOI] [PubMed] [Google Scholar]
- 22.Dupuy DE, Hong R, Oliver B, Goldberg SN. Radiofrequency ablation of spinal tumors: temperature distribution in the spinal canal. AJR Am J Roentgenol 2000; 175: 1263–6. doi: 10.2214/ajr.175.5.1751263 [DOI] [PubMed] [Google Scholar]
- 23.Martel J, Bueno A, Nieto-Morales ML, Ortiz EJ. Osteoid osteoma of the spine: CT-guided monopolar radiofrequency ablation. Eur J Radiol 2009; 71: 564–9. doi: 10.1016/j.ejrad.2008.04.020 [DOI] [PubMed] [Google Scholar]
- 24.Pinto CH, Taminiau AH, Vanderschueren GM, Hogendoorn PC, Bloem JL, Obermann WR. Technical considerations in CT-guided radiofrequency thermal ablation of osteoid osteoma: tricks of the trade. AJR Am J Roentgenol 2002; 179: 1633–42. doi: 10.2214/ajr.179.6.1791633 [DOI] [PubMed] [Google Scholar]
- 25.Sim FH, Dahlin CD, Beabout JW. Osteoid-osteoma: diagnostic problems. J Bone Joint Surg Am 1975; 57: 154–9. [PubMed] [Google Scholar]
- 26.Mehta MH. Pain provoked scoliosis. Observations on the evolution of the deformity. Clin Orthop Relat Res 1978; 135: 58–65. [PubMed] [Google Scholar]
- 27.Hoeffel C, Gaucher H, Hoeffel JC, Galloy MA, Arnould V. Painful scoliosis. Klin Padiatr 1997; 209: 78–83. doi: 10.1055/s-2008-1043932 [DOI] [PubMed] [Google Scholar]
- 28.Kneisl JS, Simon MA. Medical management compared with operative treatment for osteoid-osteoma. J Bone Joint Surg Am 1992; 74: 179–85. [PubMed] [Google Scholar]
- 29.Coulier B, Mailleux P, Munting E. Spontaneous remission of an osteoid osteoma of the axis. JBR-BTR 2005; 88: 43. [PubMed] [Google Scholar]
- 30.Neumann D, Dorn U. Osteoid osteoma of the dens axis. Eur Spine J 2007; 16(Suppl. 3): 271–4. doi: 10.1007/s00586-007-0332-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Azouz EM, Kozlowski K, Marton D, Sprague P, Zerhouni A, Asselah F. Osteoid osteoma and osteoblastoma of the spine in children. Report of 22 cases with brief literature review. Pediatr Radiol 1986; 16: 25–31. [DOI] [PubMed] [Google Scholar]
- 32.Maiuri F, Signorelli C, Lavano A, Gambardella A, Simari R, D'Andrea F. Osteoid osteomas of the spine. Surg Neurol 1986; 25: 375–80. [DOI] [PubMed] [Google Scholar]
- 33.Pettine KA, Klassen RA. Osteoid-osteoma and osteoblastoma of the spine. J Bone Joint Surg Am 1986; 68: 354–61. [PubMed] [Google Scholar]
- 34.Labbé JL, Clement JL, Duparc B, Poey C, Railhac JJ. Percutaneous extraction of vertebral osteoid osteoma under computed tomography guidance. Eur Spine J 1995; 4: 368–71. [DOI] [PubMed] [Google Scholar]
- 35.Van Royen BJ, Baayen JC, Pijpers R, Noske DP, Schakenraad D, Wuisman PI. Osteoid osteoma of the spine: a novel technique using combined computer-assisted and gamma probe-guided high-speed intralesional drill excision. Spine (Phila Pa 1976) 2005; 30: 369–73. [DOI] [PubMed] [Google Scholar]
- 36.Gangi A, Alizadeh H, Wong L, Buy X, Dietemann JL, Roy C. Osteoid osteoma: percutaneous laser ablation and follow-up in 114 patients. Radiology 2007; 242: 293–301. doi: 10.1148/radiol.2421041404 [DOI] [PubMed] [Google Scholar]
- 37.Moser T, Giacomelli MC, Clavert JM, Buy X, Dietemann JL, Gangi A. Image-guided laser ablation of osteoid osteoma in pediatric patients. J Pediatr Orthop 2008; 28: 265–70. doi: 10.1097/BPO.0b013e318164f472 [DOI] [PubMed] [Google Scholar]
- 38.Sequeiros RB, Hyvönen P, Sequeiros AB, Jyrkinen L, Ojala R, Klemola R, et al. MR imaging-guided laser ablation of osteoid osteomas with use of optical instrument guidance at 0.23 T. Eur Radiol 2003; 13: 2309–14. doi: 10.1007/s00330-003-1897-5 [DOI] [PubMed] [Google Scholar]
- 39.Gangi A, Dietemann JL, Gasser B, Mortazavi R, Brunner P, Mourou MY, et al. Interstitial laser photocoagulation of osteoid osteomas with use of CT guidance. Radiology 1997; 203: 843–8. doi: 10.1148/radiology.203.3.9169714 [DOI] [PubMed] [Google Scholar]
- 40.DeFriend DE, Smith SP, Hughes PM. Percutaneous laser photocoagulation of osteoid osteomas under CT guidance. Clin Radiol 2003; 58: 222–6. [DOI] [PubMed] [Google Scholar]
- 41.Rosenthal DI, Alexander A, Rosenberg AE, Springfield D. Ablation of osteoid osteomas with a percutaneously placed electrode: a new procedure. Radiology 1992; 183: 29–33. doi: 10.1148/radiology.183.1.1549690 [DOI] [PubMed] [Google Scholar]
- 42.Osti OL, Sebben R. High-frequency radio-wave ablation of osteoid osteoma in the lumbar spine. Eur Spine J 1998; 7: 422–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Samaha EI, Ghanem IB, Moussa RF, Kharrat KE, Okais NM, Dagher FM. Percutaneous radiofrequency coagulation of osteoid osteoma of the “Neural Spinal Ring”. Eur Spine J 2005; 14: 702–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Miyazaki M, Aoki J, Miyazaki A, Nakajima T, Koyama Y, Shinozaki T, et al. Percutaneous radiofrequency ablation of osteoid osteoma using cool-tip electrodes without the cooling system. Jpn J Radiol 2011; 29: 138–43. doi: 10.1007/s11604-010-0529-7 [DOI] [PubMed] [Google Scholar]
- 45.Bitsch RG, Rupp R, Bernd L, Ludwig K. Osteoid osteoma in an ex vivo animal model: temperature changes in surrounding soft tissue during CT-guided radiofrequency ablation. Radiology 2006; 238: 107–12. doi: 10.1148/radiol.2381041500 [DOI] [PubMed] [Google Scholar]
- 46.Vanderschueren GM, Obermann WR, Dijkstra SP, Taminiau AH, Bloem JL, van Erkel AR. Radiofrequency ablation of spinal osteoid osteoma: clinical outcome. Spine (Phila Pa 1976) 2009; 34: 901–4. doi: 10.1097/BRS.0b013e3181995d39 [DOI] [PubMed] [Google Scholar]
- 47.Cantwell CP, O'Byrne J, Eustace S. Radiofrequency ablation of osteoid osteoma with cooled probes and impedance-control energy delivery. AJR Am J Roentgenol 2006; 186: S244–8. [DOI] [PubMed] [Google Scholar]
- 48.Liu C, Liu XG, Zhu B, Yuan HS, Han SB, Ma YQ. CT-guided percutaneous radiofrequency ablation of spinal osteoid osteoma. Chin Med J (Engl) 2011; 124: 4083–5. [PubMed] [Google Scholar]
- 49.Nagashima H, Nishi T, Yamane K, Tanida A. Case report: osteoid osteoma of the C2 pedicle: surgical technique using a navigation system. Clin Orthop Relat Res 2010; 468: 283–8. doi: 10.1007/s11999-009-0958-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gasbarrini A, Cappuccio M, Bandiera S, Amendola L, van Urk P, Boriani S. Osteoid osteoma of the mobile spine: surgical outcomes in 81 patients. Spine (Phila Pa 1976) 2011; 36: 2089–93. doi: 10.1097/BRS.0b013e3181ffeb5e [DOI] [PubMed] [Google Scholar]


