Abstract
Objective:
Epipericardial fat necrosis (EFN) is an uncommon benign and self-limited condition that leads patients to the emergency department (ED) owing to the onset of acute pleuritic chest pain. The aim of this study was to describe the cases of this disease in our institution and to illustrate the associated clinical and radiological findings.
Methods:
We reviewed 3604 chest scans referred by the ED from November 2011 to July 2013. Patients diagnosed with epipericardial necrosis had their medical records and original tomography reports analysed.
Results:
Chest pain was the primary complaint in 426 patients; 11 of them had definitive EFN findings characterized by a round soft-tissue attenuation lesion with a varying degree of strands. All patients presented with pleuritic chest pain on the same side as the lesion. Pericardial thickening, pleural effusion and mild atelectasis were the associated tomography findings. Cardiac enzyme and D-dimer tests performed during the episode were normal in all cases. 27% of the cases only were correctly diagnosed with EFN at the time of presentation.
Conclusion:
EFN is a benign inflammatory condition frequently overlooked in the ED by physicians and radiologists but is an important factor in the differential diagnosis of patients with acute chest pain.
Advances in knowledge:
The article adds clinically and radiologically useful information about the condition and displays the importance of making the correct diagnosis to avoid unnecessary examinations.
Epipericardial fat necrosis (EFN) is an uncommon benign condition1 first described in 1957 by Jackson et al.2 The disease usually presents as an acute pleuritic chest pain in previously healthy patients and can mimic acute myocardial infarction, pulmonary embolism or acute pericarditis.3–5
EFN is characterized as a self-limited inflammatory process occurring inside the epipericardial fat, which is the tissue that connects the pericardial layer to the anterior thoracic wall. The aetiology of EFN is still unknown, and the anatomopathological analysis reveals encapsulated fat necrosis, similar to other analogous conditions such as epiploic appendagitis and fat necrosis in the omentum or breast.6,7
Patients usually present to the emergency department (ED) with an acute chest pain, lasting from a few hours to a couple of days.8–10 The physical examination is often unremarkable, but an increased heart rate and diaphoresis may be found. Previously published case reports and reviews also demonstrate normal electrocardiograms and blood tests, as well as normal cardiac enzyme levels and negative Coxsackie viral panels.11–13
The chest radiograph is non-specific and might reveal an ill-defined opacity near the cardiophrenic angle on the side that pain is presenting, with or without concomitant pleural effusion.2,13
CT is the modality of choice for diagnosing EFN because this imaging technique reveals the precise location and the respective fat content. EFN usually presents in CT as a round, encapsulated, fatty lesion with inflammatory changes such as dense strands, thickening of the adjacent pericardium or both (Figure 1a,b). Pleural effusion can also be present at the time of diagnosis.1,11,14,15
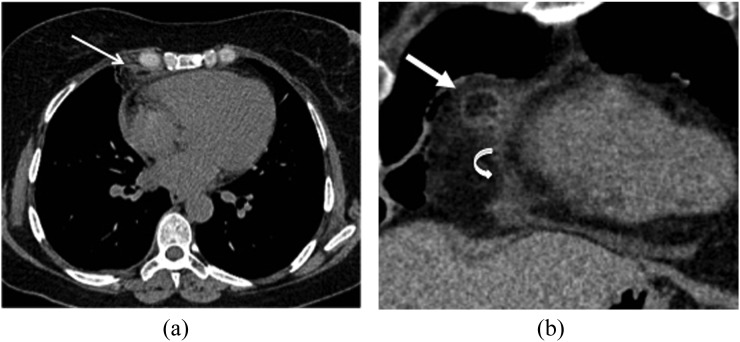
Figure 1.
A 47-year-old female with 5-day right pleuritic chest pain. (a) The axial chest CT scan displays a round soft-tissue attenuation lesion with fatty centre and peripheral strands inside the right epipericardial fat (arrow), which is strongly suggestive of epipericardial fat necrosis (EFN). (b) Coronal reformation of the round soft-tissue attenuation lesion suggestive of EFN (straight arrow). There is notable pericardial thickening (curved arrow).
The treatment is conservative, and non-steroidal anti-inflammatory drugs are usually sufficient to relieve the symptoms. A follow-up CT scan 4–8 weeks after the episode is recommended to confirm the expected healing.1,6
Since the first description by Jackson et al,2 only 35 cases have been published in the English literature, and EFN is currently described as an extremely rare disease.11 However, after a few EFN cases were diagnosed in our institution,10 we hypothesized that this condition could be overlooked, or even misdiagnosed, by emergency physicians and radiologists.
The aim of this study was to report the cases of EFN in our institution and to describe the associated clinical and radiological findings.
METHODS AND MATERIALS
Patients
The present investigation was conducted in a private quaternary hospital (Hospital Sirio-Libanes, São Paulo, Brazil) and was approved by the institutional ethics committee. This study retrospectively analysed all 3604 consecutive chest CT scans referred by the ED from November 2011 to July 2013. The hospital information system and picture archiving and communication system software (Agfa IMPAX v. 6.3.1 Solution; Agfa HealthCare, Mortsel, Belgium, 2009) stores all digital imaging data and associates each study with a brief patient clinical history and the diagnostic hypothesis for requesting CT.
All images were reviewed by two chest radiologists (2 and 8 years' experience) who were blinded to the clinical features and sought for typical EFN findings.3 In brief, these findings were defined as “a round soft-tissue attenuation lesion with a varying degree of peripheral strands with or without fatty centre located in the epipericardial fat” (Figures 2 and 3). Decisions concerning the presence of these findings were reached by consensus. EFN lesions were also evaluated for the presence or absence of fatty centre inside the soft-tissue attenuation lesion and stranding to adjacent fat. Clinical and demographic data of patients with EFN findings regarding the symptoms and laboratory findings at the time of the CT scan, as well as each additional CT finding, were then recorded.
Figure 2.

A 24-year-old male with 3-day left pleuritic chest pain and epipericardial fat necrosis findings. The axial view of an enhanced chest CT scan displays a small round soft-tissue attenuation lesion with mild stranding (arrow) close to the diaphragmatic pleural surface in the epipericardial fat.
Figure 3.

A 40-year-old male with 2-day history of right pleuritic chest pain. An axial chest CT scan displays a small, round lesion with a fatty centre surrounded by dense stranding (arrow), which is another finding strongly suggestive of epipericardial fat necrosis.
CT technique
CT scans were obtained using a second-generation dual-source CT system (SOMATOM® Definition Flash; Siemens Healthcare, Erlangen, Germany). The acquisition parameters were as follows: 170–220 mAs; 120 kVp; tube rotation time, 0.5 s; detector configuration, 128 × 0.6 mm; pitch, 0.12; and field of view, 400–500 mm. When contrast was required, the timing was determined with a test bolus consisting of 10–15 ml of iohexol solution (Omnipaque™ 300; GE Healthcare, Milwaukee, WI) with an iodine concentration of 300 mg ml−1 injected at a flow rate of 4.0–5.5 ml s−1. Contrast imaging was performed with 80–110 ml injected at the same flow rate. Images were reconstructed in axial view using a slice thickness of 1 mm and an increment of 0.7 mm.
Statistical analysis
Parametric variables are expressed as mean and standard deviation. Associated EFN findings were also described according to clinical and demographic features using measures of central tendency and dispersion. The statistical analysis was performed with GraphPad Prism® v. 5.0 for Windows (GraphPad Software, Inc., San Diego, CA—www.graphpad.com).
RESULTS
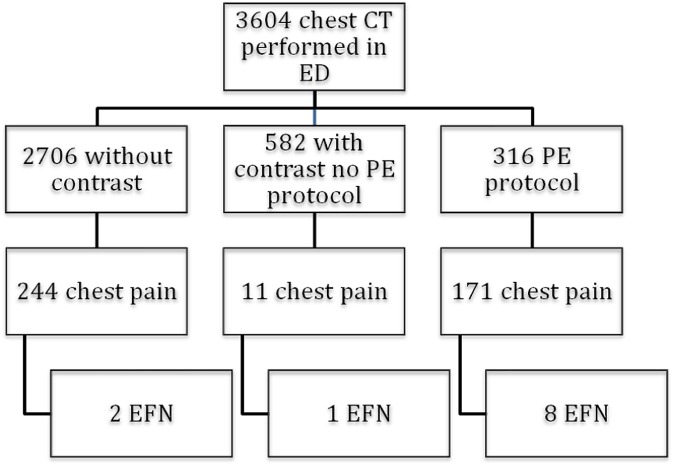
Of the 3604 chest CT scans evaluated, 426 (11.8%) were requested owing to chest pain, and 188 (44.1%) of these cases were described as pleuritic pain (data regarding the protocols/pain characteristic are displayed in Figure 4).
Figure 4.
Diagram of the protocols and the patients diagnosed with epipericardial fat necrosis (EFN) in each protocol group. ED, emergency department; PE, pulmonary embolism.
There were 264 (61.9%) males and 162 (38.1%) females, ranging in age from 16 to 92 years (mean, 49.3 ± 11.3 years). Defined imaging criteria for EFN were found in 11 chest CT scans, and all these patients had pleuritic chest pain recorded in their medical data from the day of the examination. There were no cases of EFN in patients without chest pain.
Features of each EFN lesion were evaluated, and a focal soft-tissue lesion with a fatty centre inside was observed in five patients and an entire soft-tissue attenuation was observed in another six patients. We also observed stranding to the adjacent fat in six patients.
The CT findings associated with EFN were focal pericardial thickening (4 of 11 patients), small pleural effusion (9 of 11 patients) and mild atelectasis of the lung bases (7 of 11 patients). Among all patients with EFN, there were three females (27%) and eight males (73%), with a mean age of 45.7 ± 14.9 years. Table 1 summarizes the clinical and demographic data of the EFN patients. Interestingly, in all cases, the chest pain was ipsilateral to the EFN lesion side found on the chest CT.
Table 1.
Clinical and demographic features of the epipericardial fat necrosis (EFN) patients
| Patient | Age (years) | Gender | Pain | Side | Irradiation | Other symptoms | Physical examination | Symptom duration | EFN side in the chest CT |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 23 | Female | Pleuritic | Right | No | No | Tachycardia | 1 day | Right |
| 2 | 40 | Male | Pleuritic | Right | Back | No | No | 2 days | Right |
| 3 | 80 | Male | Pleuritic | Left | Shoulder | No | No | 9 h | Left |
| 4 | 59 | Female | Pleuritic | Left | No | No | No | 1 day | Left |
| 5 | 44 | Male | Pleuritic | Left | No | No | No | 3 days | Left |
| 6 | 46 | Male | Pleuritic | Left | No | Dyspnoea | No | 2 days | Left |
| 7 | 52 | Female | Pleuritic | Pre-cordial/right | No | No | No | 5 days | Right |
| 8 | 41 | Male | Pleuritic | Left | No | No | No | 6 days | Left |
| 9 | 49 | Male | Pleuritic | Left | No | No | No | 2 days | Left |
| 10 | 24 | Male | Pleuritic | Left | No | No | Local pain | 3 days | Left |
| 11 | 45 | Male | Pleuritic | Right | No | No | No | 2 days | Right |
9 out of 11 patients with EFN had troponin, creatine kinase (CK), creatine kinase, muscle and brain (CK-MB) and D-dimer tests performed. All results were below the cut-off value: troponin <0.16 ng ml−1; mean CK, 108 ± 31 U l−1 (normal range, 18–174 U l−1); mean CK-MB, 1.9 ± 0.3 U l−1 (normal range, <5 U l−1); and mean D-dimer, 348 ± 76 μg l−1 (normal range, <540 μg l−1). Two patients had only cardiac enzyme tests, two other patients had only D-dimer tests and the seven remaining patients had both tests.
Regarding individuals with EFN findings, electrocardiography was performed in six patients, and the only abnormal finding was left ventricular overload in one previously hypertensive patient. Echocardiography was performed in four patients and was unremarkable in all. Two patients also had venous Doppler ultrasounds requested, which were all negative for deep vein thrombosis. One patient underwent myocardial perfusion scintigraphy and coronary angiography, which revealed mild obstructive atherosclerosis.
When the CT report of each EFN patient was reviewed, we observed that in three cases only (27%) was the diagnosis correctly suggested. In another five cases (45%), findings were described as “unspecific mediastinal stranding” or “strandings in the cardiophrenic region”. The remaining four cases had no mention of the EFN lesion in the original CT report. Conversely, all associated findings of pleural effusion and atelectasis were correctly described.
Four patients were submitted to a CT follow-up scan after the diagnosis, and all of them revealed healing of the inflammatory changes, as presented in Figures 5 and 6.
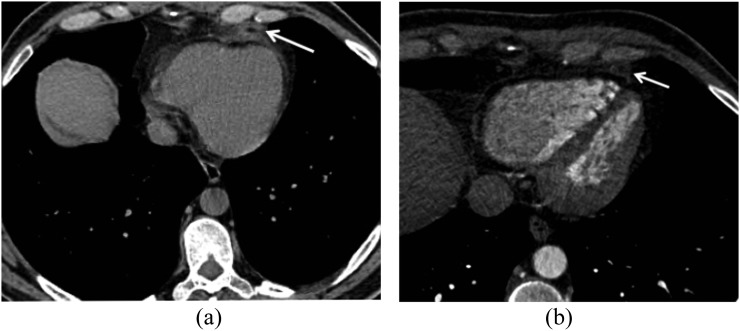
Figure 5.
A 44-year-old male with 3-day left pleuritic chest pain. (a) The axial view of an unenhanced chest CT scan displays a round soft-tissue attenuation lesion with strands (arrow) in the epipericardial fat and focal pericardial thickening. (b) Axial view of the chest CT control performed 4 weeks later. The lesion has almost completely resolved, with mild residual focal stranding in the epipericardial fat (arrow).
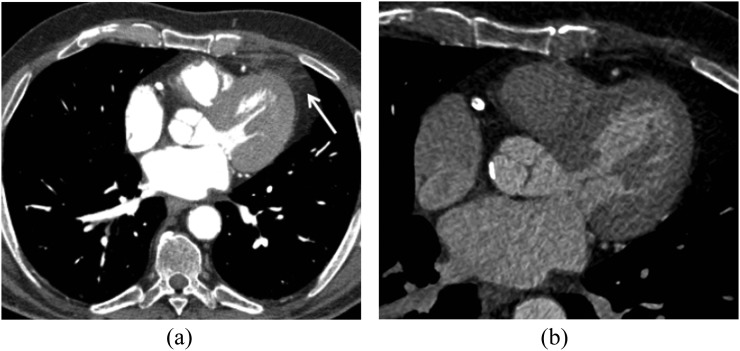
Figure 6.
An 80-year-old male with 9-h left pleuritic chest pain. (a) An enhanced chest CT scan displays a soft-tissue attenuation lesion and stranding in the left epipericardial fat (arrow). (b) The axial chest CT follow-up scan performed 7 weeks later demonstrates complete resolution of the findings.
DISCUSSION
The epipericardial or parietal layer of fat tissue is found outside the visceral pericardium and represents the external surface of the parietal pericardium, connecting the pericardial layer to the anterior thoracic wall. The embryologic origin of the epipericardial layer is from the primitive thoracic mesenchyme, and its blood supply comes from non-coronary sources, such as the pericardiophrenic branches of the internal mammary artery.4
The aetiology of EFN remains unknown, but some theories have been proposed to explain its origin. Acute torsion of a vascular pedicle is described in some cases, although the presence of a vascular pedicle has been described in only two patients who underwent surgery.11 Furthermore, increased intrathoracic pressure due to heavy lifting or Valsalva's manoeuvre might trigger rapid changes in capillary pressure, leading to haemorrhagic necrosis, especially if pre-existing structural abnormalities of the adipose tissue, such as lipoma, hamartoma or lipomatosis, are present.16 In all patients who underwent surgery to exclude malignant processes, the pathological findings demonstrated a varying degree of inflammatory reactions surrounding a central focus of necrotic fat cells.4,5,11,14 Both males and females are affected, and neither age predilections nor pre-disposing factors have been described.11
Pineda et al3 described a triad of acute chest pain, dense stranding of an encapsulated fatty lesion on CT and thickening of the adjacent pericardium as being highly suggestive of EFN.11 Indeed, the typical CT finding is a lesion of soft-tissue attenuation surrounded by increased attenuation of anterior mediastinal paracardiac fat adjacent to the pericardium.1
This study was the first to evaluate chest CT scans referred by the ED and consider EFN findings, and it represents the largest reported series of EFN cases from a single hospital. Although symptoms and CT findings of EFN are well described in the literature, there is no description of its true incidence in the general population. Although we cannot extrapolate our findings to the true incidence in the ED population, we found a proportion of 2.58% EFN in patients with acute chest pain who underwent chest CTs during their ED evaluations.
Moreover, we found a high prevalence of non-specific-associated CT findings (82% had associated pleural effusions, 63% had mild atelectasis and 36% had pericardial thickening). In all cases, the chest pain was pleuritic and ipsilateral to the EFN lesions on the CT scan. An important finding was that EFN is indeed overlooked in the ED. Of the 11 patients with a CT scan compatible with EFN, 27% only were accurately diagnosed at the first CT report. Furthermore, we analysed further diagnostic tests performed on the day of the episode. When present, the troponin, D-dimer, electrocardiogram and echocardiogram results were normal.
The first case of EFN with successful conservative management was published in 2005 by Pineda et al3 and revealed that a CT follow-up scan is useful to prevent unnecessary surgery and to confirm the inflammatory nature of the changes. Subsequent reports also reinforced the same management.5,8,17 Our study also supports this theory, as all four of our patients who underwent a follow-up CT scan after the chest pain episode experienced healing of their inflammatory changes.
Our study has limitations. Because all cases were retrospectively assessed, the clinical and laboratory data were not uniformly available. Furthermore, in most cases, non-contrast scans were requested by the referring physician. Nevertheless, the use of contrast appears not to change the final diagnosis. Additionally, because most cases were originally overlooked, we could only assess a follow-up CT in 4 of the 11 EFN patients.
In summary, because acute chest pain is an extremely common symptom seen in the ED and because the differential diagnosis often includes severe conditions such as pulmonary embolism or acute coronary syndrome, the identification of EFN is crucial. The EFN diagnosis ensures not only that there is no other potentially serious condition generating symptoms but also avoids other unnecessary examinations or invasive diagnostic procedures. We herein demonstrate that EFN is a more prevalent condition in the ED than previously thought, and the characteristic CT findings in a setting of acute pleuritic chest pain associated with normal electrocardiogram, cardiac enzyme and D-dimer tests may be enough to diagnose this condition, thereby avoiding further tests. Therefore, knowledge of this condition should be widespread in medical practice.
REFERENCES
- 1.Hernandez D, Galimany J, Pernas JC, Llauger J. Case 170: pericardial fat necrosis. Radiology 2011; 259: 919–22. doi: 10.1148/radiol.10090786 [DOI] [PubMed] [Google Scholar]
- 2.Jackson RC, Clagett OT, McDonald JR. Pericardial fat necrosis: report of three cases. J Thorac Surg 1957; 33: 723–9. [PubMed] [Google Scholar]
- 3.Pineda V, Caceres J, Andreu J, Vilar J, Domingo ML. Epipericardial fat necrosis: radiologic diagnosis and follow-up. AJR Am J Roentgenol 2005; 185: 1234–6. doi: 10.2214/AJR.04.1310 [DOI] [PubMed] [Google Scholar]
- 4.Baig A, Campbell B, Russell M, Singh J, Borra S. Epicardial fat necrosis: an uncommon etiology of chest pain. Cardiol J 2011; 19: 424–8. [DOI] [PubMed] [Google Scholar]
- 5.Lee HH, Ryu DS, Jung SS, Jung SM, Choi SJ, Shin DH. MRI findings of pericardial fat necrosis: case report. Korean J Radiol 2011; 12: 390–4. doi: 10.3348/kjr.2011.12.3.390 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.van den Heuvel DA, van Es HW, Cirkel GA, Bos WJ. Acute chest pain caused by pericardial fat necrosis. Thorax 2010; 65: 188. doi: 10.1136/thx.2009.114637 [DOI] [PubMed] [Google Scholar]
- 7.Ghahremani GG, White EM, Hoff FL, Gore RM, Miller JW, Christ ML. Appendices epiploicae of the colon: radiologic and pathologic features. Radiographics 1992; 12: 59–77. doi: 10.1148/radiographics.12.1.1734482 [DOI] [PubMed] [Google Scholar]
- 8.Lacasse MC, Prenovault J, Lavoie A, Chartrand-Lefebvre C. Pericardial fat necrosis presenting as acute pleuritic chest pain. J Emerg Med 2012; 44: e269–71. doi: 10.1016/j.jemermed.2012.05.032 [DOI] [PubMed] [Google Scholar]
- 9.Peres Claro I, Magalhaes V, Correia I, Campos P, Sotto-Mayor R, Bugalho de Almeida A. Epipericardial fat necrosis—case report. [In Portuguese.] Rev Port Pneumol 2010; 16: 507–12. [PubMed] [Google Scholar]
- 10.Giassi KS, Costa AN, Apanavicius A, Bachion GH, Musolino RS, Kairalla RA. Epipericardial fat necrosis: an unusual cause of chest pain. J Bras Pneumol 2013; 39: 627–9. doi: 10.1590/S1806-37132013000500014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ataya D, Chowdhry AA, Mohammed TL. Epipericardial fat pad necrosis: computed tomography findings and literature review. J Thorac Imaging 2011; 26: W140–2. doi: 10.1097/RTI.0b013e3181fa6d7c [DOI] [PubMed] [Google Scholar]
- 12.Estebanez-Seco S, Julian-Jimenez A, Puche-Paniagua JJ, Yague MC, Perez CC, Tenorio FC. Acute chest pain caused by pericardial fat necrosis: a diagnosis to consider in some patients. Rev Clin Esp 2010; 210: e47–9. [DOI] [PubMed] [Google Scholar]
- 13.Bensard DD, St Cyr JA, Johnston MR. Acute pleuritic chest pain and lung mass in an elderly woman. Chest 1990; 97: 1473–4. [DOI] [PubMed] [Google Scholar]
- 14.Runge T, Greganti MA. Epipericardial fat necrosis - a rare cause of pleuritic chest pain: case report and review of the literature. Arch Med Sci 2011; 7: 337–41. doi: 10.5114/aoms.2011.22088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Fred HL. Pericardial fat necrosis: a review and update. Tex Heart Inst J 2010; 37: 82–4. [PMC free article] [PubMed] [Google Scholar]
- 16.Lee BY, Song KS. Calcified chronic pericardial fat necrosis in localized lipomatosis of pericardium. AJR Am J Roentgenol 2007; 188: 21–4. doi: 10.2214/AJR.04.1989 [DOI] [PubMed] [Google Scholar]
- 17.Mazzamuto G, Ghaye B. Epipericardial fat necrosis. JBR-BTR 2012; 95: 154–5. [DOI] [PubMed] [Google Scholar]