Abstract
Background
Organised follow-up is a common feature of several strategies at the primary health care level to promote health behaviour change, e.g. to increase physical activity. In Norway, municipal ‘healthy living’ centres run by health care personnel are established to offer counselling and organised follow-up of health behaviour change during a 12-week programme. We report the results of a systematic review commissioned by the Norwegian Directorate of Health concerning organised follow-up to improve physical activity.
Methods
We searched ten electronic databases up to June 2012, reference lists of included publications, and relevant journals. Study selection and quality risk of bias assessment were carried out independently. Data were synthesised narratively due to heterogeneity of measurements of physical activity. The GRADE approach was used to assess our confidence in the effect estimate for each outcome in each comparison.
Results
Fourteen randomised controlled trials from seven countries and with a total of 5,002 participants were included in the systematic review. All studies were carried out in primary care or community settings. The interventions comprised referral to supervised group physical activity (2 studies), referral to local resources with follow-up (6 studies), and self-organised physical activity with follow-up (6 studies). The narrative synthesis, comprising a total of 39 comparisons, indicated effects of self-organised physical activity with follow-up (compared to both advice and no treatment) and referral to local resources with follow-up (compared to advice) in some of the comparisons where we rated our confidence in the effect estimates as moderate. However, the results indicated no difference between intervention and control groups for the majority of comparisons. Follow-up in the studies was mainly short-term with the longest follow-up 9 months post-treatment. We rated our confidence in the effect estimates as low or very low in most comparisons, both for positive and neutral results.
Conclusions
The results of this systematic review indicate considerable uncertainty concerning effects of organised follow-up during 10–14 weeks on physical activity. Major methodological problems concerning the measurement of physical activity are discussed.
Trial registration
Systematic review registration: PROSPERO CRD42011001598.
Keywords: Health behavior, Primary health care, Review
Background
Physical inactivity has been identified as the fourth leading risk factor for global mortality (6% of deaths globally), and it is estimated that approximately 21–25% of breast and colon cancer, 27% of diabetes, and approximately 30% of ischemic heart disease can be attributed to physical inactivity [1]. Participation in regular physical activity (PA) is known to reduce the risk of several non-communicable diseases [2].
Current guidelines on PA for adults aged 18–64 years state that each week, 150 minutes of moderate-intensity aerobic PA should be done or at least 75 minutes of vigorous-intensity aerobic PA or an equivalent combination of moderate- and vigorous-intensity activity [3]. The primary health care level is well suited to identify persons with unhealthy behaviours such as physical inactivity as 70-80% of adults in developed countries may visit a general practitioner at least once a year [4]. Several strategies to improve the ability to promote healthy behaviours of primary care patients have been reported in recent years. These include establishing ‘bridges’ between primary care practices and communities [5], ‘community health education liaisons’ [6] and ‘medical assistant referral programmes’ [7]. Strategies more specifically directed at PA include PA promotion [8], exercise referral schemes [9], and systematically integrating PA promotion into the primary care setting by means of ‘physical activity pathways’ [10]. Recent systematic reviews of PA promotion based in primary care [11] and exercise referral schemes [12] indicate small to moderate improvement of self-reported PA at 12 months’ follow-up, while only process evaluation data are available for the physical activity pathways so far [10].
In Norway, the Directorate of Health has supported the development of municipal ‘healthy lifestyle’ centres (in Norwegian, frisklivssentraler) since 2004. Briefly, healthy lifestyle centres are organisations at the primary health care level run by health care personnel who offer a structured, yet flexible programme for counselling and organised follow-up of behaviours that may increase risk of disease in adults [13]. One important feature of the centres is the co-ordinating function between primary health care and community resources. Presently, targeted behaviours are PA, diet, smoking, and alcohol use. Persons can be referred to a healthy lifestyle centre by health care professionals or they make contact without a referral. A programme period lasts 12 weeks, starting with a motivational health conversation which includes formulation of goals and an individual plan for the period. Several options then exist for each of the targeted behaviours. A person with a goal to increase PA may choose among individual counselling, supervised group exercise at the centre, or referral to local resources such as leisure centres or sports organisations. Follow-up during the programme period can be by individual meetings, phone, e-mail or text messages. The programme concludes with a second motivational health conversation in which goal attainment and need for another programme period is assessed. Although the focus of the programme is to prepare participants for self-organised activities, several periods with follow-up from the healthy lifestyle centre may be needed to accomplish behavioural change.
The Norwegian Directorate of Health commissioned a systematic review of the effects of organised follow-up at the primary health care/community level on behaviour that may increase risk of disease in adults (physical activity, diet, smoking, and alcohol use). The review [14] was used to inform a national guideline for municipal healthy lifestyle centres.
In the present paper we focus on the review of effects of organised follow-up on PA. Because persons can make contact with healthy lifestyle centres without a referral, the recent systematic reviews on effects of exercise referral schemes [12], and effectiveness of PA promotion based in primary care [11] would only partially answer our question, since these included studies in which participants were referred from or recruited via primary care. During the course of the review, issues related to the measurement of the primary outcome, PA, and potential consequences for data synthesis and interpretation of the results became evident. Implications of these issues will be discussed.
Thus, in this paper we aim to 1) systematically review and report the results of relevant studies concerning effects of organised follow-up on PA, and 2) discuss issues in data synthesis and interpretation of results from non-standardised reporting of PA outcomes and measurement in the included studies.
Methods
Inclusion criteria
Study design
We considered study designs in the following order: overviews of systematic reviews and systematic reviews, randomised controlled trials, cluster-randomised controlled trials, quasi-randomised controlled trials, controlled before-and-after studies, and interrupted time-series analyses.
Setting
Primary health care/community.
Population
Adults (≥18 years) with low levels of PA or increased risk of, or diagnosis of, disease for which physical activity may be a protective factor, e.g. cardiovascular disease, and type 2 diabetes.
Intervention
Organised follow-up over a period of 10–14 weeks, individually or in groups, given within a local organisation or by a single health professional (excluding general practitioners), starting with individual goal-setting and aiming to support increased PA.
Comparisons
1) Advice (with or without written information) about PA from health professionals without organised follow-up outside the office, 2) usual care, and 3) no treatment.
Outcomes
The primary outcome was PA behaviour, e.g. frequency, duration, intensity, achievement of pre-set goals, or indications of PA, e.g. energy expenditure, aerobic capacity.
Language
There were no language restrictions for the literature search. Publications in other languages than English or Scandinavian have been translated if judged relevant.
Literature searches
We searched MEDLINE, EMBASE, Cochrane Database of Systematic Reviews, Cochrane Central Register, DARE and HTA (via Centre for Reviews and Dissemination), Cinahl, PsychINFO, Sociological Abstracts, and Social Science citation Index up to October 2011. In addition, we searched manually in a) reference lists of relevant systematic reviews identified in the electronic search, b) reference lists of included publications, c) the following journals that most commonly publish papers that could potentially match our inclusion criteria (publication dates were January 2009 – February 2012): American Journal of Preventive Medicine, BMC Family Practice, BMC Public Health, European Journal of Public Health, Preventive Medicine, Scandinavian Journal of Primary Health Care, and Scandinavian Journal of Public Health, and d) reference lists of relevant protocols identified in c). The search was updated by a search in MEDLINE in June 2012. The search strategy for the 2012 search is available in Additional file 1.
Two authors (ED and GEV, ED and VU or ED and RCB) independently screened titles and abstracts and assessed retrieved full texts against a set of pre-determined inclusion criteria. Discrepancies were solved by consensus or by a third person. There was no need to contact authors to provide additional data.
Data extraction and analysis
The first author (ED) extracted study characteristics (study design, population, intervention(s), comparison(s), and outcome(s)) and study results (descriptive discrete or continuous data, effect measures and effect estimates) using a pre-designed data extraction form. One other author (GEV, VU or RCB) verified the extracted data against the full text articles. Risk of bias at study level was assessed according to the Cochrane Handbook [15] and independently by two authors. If consensus was not reached a third person was consulted. The GRADE approach [16] was used to rate our confidence in the effect estimate for each outcome in each comparison. The interventions were categorized according to main content, and in each category effect measures and effect estimates were described for each comparison. When several outcome measures were reported, we chose the measure(s) that best reflected total physical activity.
Results
We did not find overviews of systematic reviews or systematic reviews that matched our inclusion criteria. We found 14 primary studies that met our inclusion criteria (Figure 1), all of which were randomised controlled trials [17-30]. Study characteristics and risk of bias ratings for the included studies are presented in Table 1.
Figure 1.
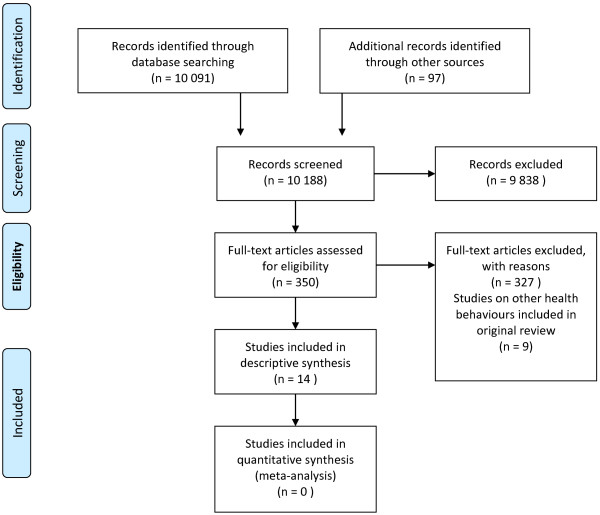
PRISMA flow diagram showing literature retrieval and study selection.
Table 1.
Study characteristics and risk of bias ratings in the included studies
| Study location | Design overall risk of bias✝ | Participants longest follow-up | Intervention and duration | Comparison | Physical activity outcomes | Measured by |
|---|---|---|---|---|---|---|
| Isaacs 2007 [17] England |
RCT Unclear3,4,5,7 |
943 adults 40–74 years 3 months |
Supervised PA in groups |
Advice |
Minutes of PA/week |
Questionnaire on 7-day leisure time activities, walking, occupational activity and work in the home [48] |
| Energy expenditure, kcal/kg/week | ||||||
| 1) strength, fitness | ||||||
| 2) walks led by instructor | ||||||
| Duration: 10 weeks | ||||||
| Park 2011 [18] South Korea |
RCT Unclear1,2,3,4,5 |
45 older adults ≥ 65 years Post-treatment |
Supervised PA in groups |
No treatment |
MET-adjusted minutes of PA/week |
International Physical Activity Questionnaire [49] |
| Duration: 12 weeks | ||||||
| Elley 2003 [19] New Zealand |
Cluster-RCT Unclear2,3,4 |
878 adults 40–79 years 9 months |
Referral to local resources w/follow-up |
Advice |
Energy expenditure, kcal/kg/week |
Auckland Heart Study Physical Activity Questionnaire [50] |
| Duration: 12 weeks | ||||||
| Fortier 2011 [20] Canada |
RCT Low3 |
120 adults 18–69 years 3 months |
Referral to local resources w/follow-up |
Advice |
Minutes of moderate PA/day |
Godin Leisure-Time Exercise Questionnaire [51]; accelerometer [52] |
| PA score | ||||||
| Duration: 12 weeks | ||||||
| Harrison 2004 [21] England |
RCT Low4 |
545 adults ≥ 18 years 9 months |
Referral to local resources w/follow-up |
Advice |
Number of participants who met PA goal (90 min/week) |
Adapted 7-Day Physical Activity Recall Questionnaire [53] |
| Duration: 12 weeks | ||||||
| Stevens 1998 [22] England |
RCT Unclear2,3,4,5,7 |
714 adults 45–74 years 4 months |
Referral to local resources w/follow-up |
Advice |
Level of PA last 4 weeks |
Adapted 7-Day Physical Activity Recall Questionnaire [53] |
| Duration: 10 weeks | ||||||
| Armit 2009 [23] Australia |
RCT Low2,4 |
136 adults 50–70 years 3 months |
1) Referral to local resources w/follow-up |
Advice |
Number of participants who met PA goal (150 min/week) |
Active Australia Physical Activity Questionnaire [54] |
| 2) Self-organised PA w/follow-up | ||||||
| Duration: 12 weeks | ||||||
| Taylor 1998 [24] England |
RCT Unclear2,3,4,5 |
142 adults 40–70 years 6 months |
Referral to local resources w/follow-up |
No treatment |
Minutes of PA/week |
7-Day Physical Activity Recall Questionnaire [53] |
| Energy expenditure, kcal/kg/day | ||||||
| Duration: 10 weeks | ||||||
| Bjørk Petersen 2012 [25] Denmark |
RCT Unclear1,3,4 |
655 adults ≥ 18 years Post-treatment |
Self-organised PA w/follow-up |
Advice |
Minutes of PA/week |
International Physical Activity Questionnaire [49]; ergometer [55,56] |
| Increased level of PA | ||||||
| Duration: 12 weeks | ||||||
| Aerobic capacity | ||||||
| Harland 1999 [26] England |
RCT Low2,3 |
209 adults 40–64 years§ 9 months |
Self-organised PA w/follow-up |
Advice |
PA score |
National Fitness Survey Questionnaire [57] |
| - level of PA | ||||||
| Duration: 12 weeks | ||||||
| - occasions with PA | ||||||
| Baker 2008 [27] Scotland |
RCT Unclear1,3 |
79 adults 18–65 years Post-treatment |
Self-organised PA w/follow-up |
No treatment |
Number of steps/day |
Pedometer [58] |
| Duration: 12 weeks | ||||||
| Green 2002 [28] USA |
RCT Low3 |
316 adults 18–65 years 3 months |
Self-organised PA w/follow-up |
No treatment |
PA score |
Physician Assessment and Counselling for Exercise [59] |
| Duration: 12 weeks | ||||||
| Kirkwood 2007 [29] Scotland |
RCT High1,2,3,4,5 |
34 adult women 30–50 years Post-treatment |
Self-organised PA w/follow-up |
No treatment |
Energy expenditure, kcal/kg/day |
Accelerometer [60] |
| Duration: 12 weeks | ||||||
| Kolt 2007 [30] New Zealand |
RCT Unclear2,3,4,5 |
186 older adults ≥ 65 years 9 months |
Self-organised PA w/follow-up |
No treatment |
Minutes of PA/week |
Auckland Heart Study Physical Activity Questionnaire [50] |
| Duration: 12 weeks |
Legend: PA = physical activity; ✝domains where risk of bias was rated as low, unclear or high at study level: 1sequence generation, 2allocation concealment, 3blinding of participants and personnel, 4blinding of outcome assessment, 5incomplete outcome data, 6selective outcome reporting, 7other potential threats to validity; §data for Group 3 used.
Participants and settings
Ten studies were conducted in primary health care [17,19-24,26,28,30] and four in community settings [18,25,27,29]. Twelve studies involved persons with low levels of physical activity, and two studies included persons with high blood pressure [18,24]. The studies included 5,002 participants in total, with a median of 67% female participants. Mean or median age varied between 44 and 74 years, reported in 9 studies [17-20,24,25,27,28,30]. The proportion of participants with ≥ 12 years of education varied between 27 and 75%, median 60%, reported in 9 studies [17-20,22,23,25,26,30]. The proportion of participants with white/European origin varied between 73 and 97%, median 95%, reported in 7 studies [17,19-23,28]. The proportion of persons who was offered, but declined participation in the studies varied between 38% and 86%. Demographic data were not reported for these persons.
Interventions
The main content of the interventions was categorised as referral to supervised group PA [17,18], referral to local resources with follow-up [19-24], and self-organised PA with follow-up [23,25-30]. Total participant contact time over 10–12 weeks generally varied between one and four hours, except for the supervised group PA which varied between 20 and 36 hours. The interventions were mainly delivered by exercise specialists. Fidelity to the intervention protocol was reported in one study only [20] and ranged between 77 and 84%.
Referral to supervised group PA
The intervention was given 2–3 times/week for 10 weeks [17] or 12 weeks [18]. Each session lasted about an hour and involved indoor exercises to improve strength and aerobic capacity [17,18] or walks led by an instructor [17].
Referral to local resources with follow-up
The interventions comprised referral to an exercise specialist with follow-up 3–6 times over 12 weeks [20,23]; referral to an exercise specialist at a local centre with follow-up 3 times over 12 weeks [19], or at the end of the intervention [21,22]; referral to a local centre with subsidised access to a gym and follow-up twice over 10 weeks [24]. One of the studies [23] based the follow-up consultations on stages-of-change theory [31] and motivational interviewing [32].
Self-organised PA with follow-up
The interventions comprised use of pedometers and follow-up by an exercise specialist 3 times over 12 weeks [23], by e-mail 3 times over 12 weeks [25], or at the end of the intervention [27]; information about local facilities and activities and follow-up 6 times over 12 weeks [26]; self-help materials and follow-up 3 times over 12 weeks [28]; a ‘TeleWalk’ programme and follow-up 8 times over 12 weeks [30]; one consultation with specific advice to reach 60 minutes of brisk walking/day and individualised follow-up by postal mail, e-mail or phone [29]. The follow-up consultations were based on stages-of-change theory [31] in one study [28], on stages-of-change theory [31] and motivational interviewing [32,33] in three studies [23,26,30], and on the theory of planned behaviour [34] in one study [25].
Comparisons
The interventions were compared to written or oral advice [17,20-23,25,26], usual care [19], or no treatment [18,24,27-30]. Because usual care does not exclude advice, we combined the categories written or oral advice and usual care into one category: advice. There were a total of 39 comparisons in the included studies: 9 concerning supervised group PA [17,18], 16 concerning referral to local resources with follow-up [19-24], and 14 concerning self-organised PA with follow-up [23,25-30].
Outcomes and follow-up periods
Primary outcomes
Our primary outcome, physical activity, was measured in several ways in the included studies, as described in Table 1. All outcomes except minutes of moderate PA/day and energy expenditure (measured by accelerometer [20,29]) and aerobic capacity (ergometer test [25]) were self-reported by questionnaire. Data concerning psychometric properties of questionnaires were reported in one study only [28]. Harm was not reported in any of the studies.
Follow-up periods in the studies
The follow-up periods were described from baseline in all studies. The length of follow-up varied from immediately post-intervention to nine months post intervention (Table 1).
Effects of interventions
Due to clinical heterogeneity of measurements of the primary outcome, data were synthesised descriptively. As described earlier, PA was operationalised in several different ways and mainly measured by different self-report questionnaires, which would make pooled effect estimates difficult to interpret.
Supervised group PA
The effect estimates for the 9 comparisons concerning supervised group PA are presented in Table 2. Significant differences favoring the intervention group were reported for two outcomes where we rated our confidence in the effect estimates as low [17]. For the remaining seven comparisons non-significant results were reported. We rated our confidence in these effect estimates as low for six outcomes and as very low for one outcome. About 85% of the participants were reported to adhere to all or parts of the intervention to which they were referred.
Table 2.
Effect estimates for the comparisons concerning supervised group PA
| Study | Outcome | Participants (studies) | Comparison | Effect measure | Follow-up period/s | Effect estimate | Quality of the documentation |
|---|---|---|---|---|---|---|---|
| Isaacs [17] Strength, fitness |
Minutes of PA/week |
305 (1) |
Advice |
% change from BL (95% CI) |
Post-treatment |
−13% (−29, 8) |
Low1,2 |
| 610 (1) |
3 months |
7% (−6, 22) |
Low1,2 |
||||
| Energy expenditure kcal/kg/week |
305 (1) |
% change from BL (95% CI) |
Post-treatment |
−7% (−24, 14) |
Low1,2 |
||
| 610 (1) |
3 months |
7% (−6, 23) |
Low1,2 |
||||
| Isaacs [17] Walks |
Minutes of PA/week |
305 (1) |
Advice |
% change from BL (95% CI) |
Post-treatment |
19% (−4, 48) |
Low1,2 |
| 610 (1) |
3 months |
17% (3, 34) |
Low1,2 |
||||
| Energy expenditure kcal/kg/week |
305 (1) |
% change from BL (95% CI) |
Post-treatment |
18% (−4, 45) |
Low1,2 |
||
| 610 (1) |
3 months |
19% (4, 36) |
Low1,2 |
||||
| Park [18] | MET-adjusted minutes of PA/week | 40 (1) | No treatment | Mean diff, p-value | Post-treatment | 1050, ns | Very low1,3 |
Legend: PA = physical activity; MET = metabolic equivalent of task, BL = baseline, ns = not significant; 1unclear risk of bias at study level, 2only one study, 3only one small study.
Referral to local resources with follow-up
The effect estimates for the 16 comparisons concerning referral to local resources with follow-up are presented in Table 3. Significant differences to the advantage of the intervention group were reported for four outcomes where we rated our confidence in the effect estimates as moderate for two outcomes [20,21] and as low for two outcomes [19,22]. For the remaining 12 comparisons non-significant results were reported. We rated our confidence in the effect estimates as low for six outcomes and as very low for six outcomes. Between 25% and 100% were reported to participate in all or parts of the intervention to which they were referred.
Table 3.
Effect estimates for the comparisons concerning referral to local resources with follow-up
| Study | Outcome | Participants (studies) | Comparison | Effect measure | Follow-up period/s | Effect estimate | Quality of the documentation |
|---|---|---|---|---|---|---|---|
| Elley [19] |
Energy expenditure kcal/kg/week |
878 (1) |
Advice |
Mean change diff (96% CI) |
9 months |
9.38 (3.96, 14.81) |
Low1,5 |
| Fortier [20] |
Minutes of moderate PA/day |
120 (1) |
Advice |
Mean diff, p-value |
Post-treatment |
−1.8, ns |
Low3 |
| |
|
120 (1) |
|
|
3 months |
−1.6, ns |
Low3 |
| |
PA score |
120 (1) |
|
Mean diff, p-value |
Post-treatment |
5.5, p = 0.01 |
Moderate1 |
| |
|
120 (1) |
|
|
3 months |
0.9, ns |
Low3 |
| Harrison [21] |
Number of participants who met PA goal (90 min/week) |
330 (1) |
Advice |
OR (95% CI) |
3 months |
1.67 (1.08, 2.60) |
Moderate1 |
| |
|
312 (1) |
|
|
9 months |
1.49 (0.86, 2.57) |
Low3 |
| Stevens [22] |
Level of PA last 4 weeks |
314 (1) |
Advice |
Mean diff (95% CI) |
4 months |
1.52 (1.14,1.95) |
Low1,4 |
| Armit [23] |
Number of participants who met PA goal (150 min/week) |
91 (1) |
Advice |
OR (95% CI) |
Post-treatment |
2.07 (0.86, 5.02) |
Low3 |
| |
|
91 (1) |
|
|
3 months |
1.14 (0.47, 2.76) |
Low3 |
| Taylor [24] |
Minutes of PA/week |
67 (1) |
No treatment |
Mean diff, p-value |
1 month |
66, ns |
Very low2,6 |
| |
|
67 (1) |
|
|
3 months |
- 23, ns |
Very low2,6 |
| |
|
67 (1) |
|
|
6 months |
- 4, ns |
Very low2,6 |
| |
Energy expenditure kcal/kg/day |
67 (1) |
|
Mean diff, p-value |
1 month |
0.7, ns |
Very low2,6 |
| |
|
67 (1) |
|
|
3 months |
0.1, ns |
Very low2,6 |
| 67 (1) | 6 months | 0.2, ns | Very low2,6 |
Legend: PA = physical activity, ns = not significant; 1only one study, 2only one small study, 3only one study an wide confidence interval, 4unclear risk of bias at study level, 5unclear risk of bias at study level + only 35% got the intervention, 6 unclear risk of bias at study level + incomplete data.
Self-organised PA with follow-up
The effect estimates for the 14 comparisons concerning self-organised PA with follow-up are presented in Table 4. Significant differences favoring the intervention group were reported for nine of the fourteen outcomes measured. We rated our confidence in the effect estimates as moderate for five outcomes [23,26-28], as low for three outcomes [25,30], and as very low for one outcome [29]. For the remaining five comparisons non-significant results were reported. We rated our confidence in the effect estimates as low for these outcomes. Between 66% and 77% were reported to participate in all or parts of the intervention to which they were referred.
Table 4.
Effect estimates for the comparisons concerning self-organised PA with follow-up.
| Study | Outcome | Participants (studies) | Comparison | Effect measure | Follow-up period/s | Effect estimate | Quality of the documentation |
|---|---|---|---|---|---|---|---|
| Armit [23] |
Number of participants who met PA goal (150 min/week) |
91 (1) 91 (1) |
Advice |
OR (95% CI) |
Post-treatment 3 months |
1.03 (0.41, 2,62) 2.39 (1.01, 5.64) |
Low2 Moderate1 |
| Bjørk Petersen [25] |
Minutes of PA/week |
655 (1) |
Advice |
Median diff, p-value |
Post-treatment |
120, p = 0.30 |
Low1,3 |
| Increased level of PA |
365 (1) |
% diff, p-value |
Post-treatment |
10.3, p < 0.01 |
Low1,3 |
||
| Aerobic capacity |
655 (1) |
Median diff, p-value |
Post-treatment |
- 0.7 p = 0.21 |
Low1,3 |
||
| Harland [26] |
Level of PA |
166 (1) 179 (1) |
Advice |
% diff (95% CI) |
Post-treatment 9 months |
19% (6, 32) 8% (−5, 21) |
Moderate1 Low2 |
| Occasions with PA |
172 (1) 171 (1) |
% diff (95% CI) |
Post-treatment 9 months |
16% (4, 29) 8% (−5, 20) |
Moderate1 Low2 |
||
| Baker [27] |
Number of steps/day |
79 (1) |
No treatment |
Mean change diff, p-value |
Post-treatment |
3 022, p < 0.001 |
Moderate1 |
| Green [28] |
PA score |
256 (1) |
No treatment |
Mean diff, p-value |
3 months |
0.39, p = 0.049 |
Moderate1 |
| Kirkwood [29] |
Energy expenditure kcal/kg/day |
37 (1) |
No treatment |
Mean diff (95% CI) |
Post-treatment |
294 (68, 520) |
Very low4,5 |
| Kolt [30] | Minutes of PA/week | 175 (1) 165 (1) | No treatment | Mean diff, p-value | Post-treatment 9 months | 48.9, p = 0.02 74.9, p = 0.05 | Low1,3 Low1,3 |
Legend: PA = physical activity; 1only one study, 2only one study and wide confidence interval, 3unclear risk of bias at study level, 4only one small study, 5high risk of bias at study level.
Discussion
The results of this systematic review show effects in favour of self-organised PA with follow-up (compared to both advice and no treatment) and referral to local resources with follow-up of PA (compared to advice) in some of the comparisons where we rated our confidence in the effect estimates as moderate. However, the results indicated no difference between intervention and control groups for the majority of comparisons. Follow-up in the studies was mainly short-term with the longest follow-up 9 months post-intervention. We rated our confidence in the effects estimates as low or very low in most comparisons, both for results in favour of the intervention and results indicating little or no difference between groups. This indicates considerable uncertainty concerning effects of organised follow-up during 10–14 weeks of PA.
We identified 14 studies including more than 5,000 participants. These studies assessed three different types of intervention; however, all evaluated the effect of organised follow-up aimed at increasing PA. Given this data material, we would have expected to arrive at clearer conclusions. The main reason for the lack of clarity and strength in the documentation may be the wide variation in outcomes combined with a lack of consensus on how to measure them. Several different constructs were used for the primary outcome, PA, such as amount of PA per week, number of persons who achieved a set goal of PA, number of steps per day, and energy expenditure. These constructs, in turn, were measured and reported in 14 different ways; mainly by self-report (see Table 1). A consequence of this is that the confidence in the effect estimates is reduced because none of them were reproduced or confirmed by others. In addition, the documentation for each outcome is based on relatively few events which in many cases lead to wide confidence intervals comprising the possibility of large benefit, no difference, and potential harm from the intervention. We believe that the large number of non-significant findings and our low confidence in the results in this review is a direct result of the lack of consensus regarding the main outcomes in PA and how to measure them.
We proposed in the protocol for the present systematic review that meta-analysis with a random-effects model be used to synthesise effect data across studies. Our decision in the course of the review to synthesise effect data descriptively was based primarily on our judgement that methodological diversity in the way the primary outcome was measured in the included studies would introduce heterogeneity that could potentially affect the results of meta-analyses. In particular, this would apply to potential systematic bias due to unknown responsiveness of the questionnaires that were used to assess effects of interventions, which may lead to exacerbation of the bias by a random-effects meta-analysis [15]. Measurement properties of 85 versions of physical activity questionnaires were assessed in a recent systematic review [35], the results showing that most questionnaires lacked information on content validity and that only a few had sufficient construct validity and reliability. Interestingly, only two of the questionnaires were found to be tested for responsiveness [35], a property that is important when evaluating intervention effects [36]. Similar results were reported for 13 physical activity questionnaires for the elderly [37].
Surely, synthesising the data descriptively will not make the problem disappear – the same uncertainty regarding bias introduced by methodological diversity in the measurement of PA persists. One possible solution to the problem of wide variation in outcomes that is increasingly discussed and applied is the establishment of “core outcome sets” in clinical trials [38,39]. A core outcome set (COS) is an agreed and standardised collection of outcomes that should be reported in all trials within a specific research area [39]. It does not preclude use of other outcomes, but defines a minimum set of outcomes that should always be measured and reported. In the case of PA, objectively measured outcomes, e.g. motion sensors like pedometers and accelerometers would preferably be included [40]. To date, the OMERACT (Outcome Measures in Rheumatology) collaboration appears to have the longest history of developing such outcome sets [41]. Briefly, OMERACT works in interactive consensus processes with three criteria for endorsement of a measure: truth, discrimination, and feasibility [41]. Guidance on Delphi techniques to arrive at consensus on core outcomes suggests the involvement of patients, clinicians, researchers, and facilitators [42]. A related issue that would preferably be incorporated in such work concerns the time points for follow-up in evaluations of interventions to increase physical activity. Study designs should reflect existing knowledge regarding the acquisition and maintenance of behaviour change.
Participants in the included studies appear to have been predominantly of European origin, well educated, and in the upper range of the adult life-span. We do not have demographic data for those who declined participation in the studies. Generalisation may therefore be limited to the above mentioned population.
The content of interventions in the included studies appears to match the options offered in healthy lifestyle centres, i.e. follow-up on self-organised PA, referral to local resources, and supervised group PA. Studies were included where the length of interventions matches one period in healthy lifestyle centres, which is the basic offer in Norway. In reality, it is more common than not that a second (or third) period is offered on the basis of the motivational health conversation that concludes the first (or second) period. It may be unrealistic to achieve stable behaviour change in 12 weeks [43] and the practice in healthy lifestyle centres to offer more than one period is probably a reflection of this. Therefore, the results of this systematic review may only correspond to the basic offer of a 12 week period in healthy lifestyle centres. During our study selection and inclusion process we identified several studies that evaluated longer interventions, e.g. six months e.g. [44] or 12 months e.g. [45]. We did not, however, come across studies that evaluated interventions that corresponded to the flexibility offered in healthy lifestyle centres.
Reported adherence to all or parts of the interventions indicated substantial variation among the studies evaluating referral to local resources (25-100%), and somewhat less variation among the studies evaluating self-organised PA with follow-up (66-77%). This makes it difficult to attempt to assess whether total participant contact time would have had any influence on the results because planned contact time does not necessarily equal actual contact time. A recent systematic review of levels and predictors of uptake and adherence to exercise referral schemes reported that levels of adherence ranged from 12% to 93% and that the pooled level across three randomised controlled trials was 43% (95% CI 32% to 54%). Substantial heterogeneity was reported, possibly reflecting differences in methods of defining adherence [12]. Our data, from a different sample of studies, seem to support the results reported by Pavey and co-workers [12].
The strengths of this systematic review include the systematic literature search and use of methods to minimise bias, e.g. independent study selection and assessment of risk of bias by several authors and according to pre-determined criteria. A limitation of the present systematic review is that potentially effective interventions using new information and communication technologies alone were not evaluated. Interventions that are Web-based e.g. [46] and mobile phone based e.g. [47] are increasingly used to support health behaviour change. Such interventions were excluded from our review because they typically lack personal motivational health conversations at the beginning and end of programmes, and personal follow-up. However, personal phone calls, e-mail or text messages are already used for follow-up during the programme period in healthy living centres and further integration of information and communication technologies may offer new possibilities in program administration.
Conclusions
The results of this systematic review indicate that referral to local resources with follow-up and self-organised physical activity with follow up during 12 weeks may have positive effects on the amount of physical activity achieved by sedentary adults in the short and medium term. We rated our confidence in the effect estimates as low or very low in most comparisons, both for results in favour of the intervention and results indicating little or no difference between groups. This indicates considerable uncertainty concerning effects of organised follow-up during 10–14 weeks on PA. The diversity concerning both the conceptualisation and operationalisation of PA as well as the lack of documentation of responsiveness for all but a few of available questionnaires that measure PA represent major methodological problems in this research area. The adoption of “core sets” of outcomes and planning of time points for follow-up according to behaviour change theory may therefore result in considerable improvements of the internal validity of future research results.
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
ED participated in the design, study selection, data extraction and synthesis of the review. ED also hand searched journals and drafted the manuscript. GEV participated in the design, study selection, data extraction and synthesis of the review and helped draft the manuscript. VU participated in the study selection, data extraction, and synthesis. RCB participated in the study selection and data extraction. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Example of search strategy. Search strategy for Ovid MEDLINE®. Note that the strategy comprises search terms to identify studies concerning physical activity, diet, smoking, and alcohol use.
Contributor Information
Eva Denison, Email: Eva.Denison@nokc.no.
Gunn E Vist, Email: GunnElisabeth.Vist@nokc.no.
Vigdis Underland, Email: Vigdis.Underland@nokc.no.
Rigmor C Berg, Email: Rigmor.Berg@nokc.no.
Acknowledgements
We thank Malene Gundersen and Mariann Mathisen who carried out the literature searches in the electronic data bases.
References
- World Health Organization. Global status report on noncommunicable diseases 2010. Geneva: WHO Press; 2011. [Google Scholar]
- U.S. Department of Health and Human Services. 2008 Physical Activity Guidelines for Americans. Washington D.C: Office of Disease Prevention and Health Promotion; 2008. [Google Scholar]
- World Health Organization. Global Recommendations on Physical Activity for Health. Geneva: WHO Press; 2010. [PubMed] [Google Scholar]
- van Doorslaer E, Masseria C, Koolman X. Inequalities in access to medical care by income in developed countries. CMAJ. 2006;174:177–183. doi: 10.1503/cmaj.050584. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Etz R, Cohen D, Woolf S, Summers Holtrop J, Donahue K, Isaacson N, Stange K, Ferrer R, Olson A. Bridging primary care practices and communities to promote healthy behaviors. Am J Prev Med. 2008;35:S390–S397. doi: 10.1016/j.amepre.2008.08.008. [DOI] [PubMed] [Google Scholar]
- Summers Holtrop J, Dosh S, Torres T, Thum Y. The community health educator referral liaison (CHERL). A primary care practice role for promoting healthy behaviors. Am J Prev Med. 2008;35:S365–S372. doi: 10.1016/j.amepre.2008.08.012. [DOI] [PubMed] [Google Scholar]
- Ferrer R, Mody-Baily P, Jaén C, Gott S, Araujo S. A medical assistant-based program to promote healthy behaviors in primary care. Ann Fam Med. 2009;7:504.512. doi: 10.1370/afm.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams N. Promoting physical activity in primary care. BMJ. 2011;343:d6615. doi: 10.1136/bmj.d6615. [DOI] [PubMed] [Google Scholar]
- BHF National Centre for Physical Activity and Health. [ http://www.bhfactive.org.uk/sites/Exercise-Referral-Toolkit]
- Bull F, Milton K. A process evaluation of a “physical activity pathway” in the primary care setting. BMC Public Health. 2010;10:463. doi: 10.1186/1471-2458-10-463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orrow G, Kinmonth A-L, Sanderson S, Sutton S. Effectiveness of physical activity promotion based inprimary care: systematic review and meta-analysis of randomised controlled trials. BMJ. 2012;344:e1389. doi: 10.1136/bmj.e1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pavey T, Taylor A, Fox K, Hillsdon M, Anokye N, Campbell J, Foster C, Green C, Moxham T, Mutrie N, Searle J, Trueman P, Taylor R. Effect of exercise referral schemes in primary care on physical activity and improving health outcomes: systematic review and meta-analysis. BMJ. 2011;343:d6462. doi: 10.1136/bmj.d6462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Norwegian Directorate of Health. Health Promotion – achieving good health for all. Oslo: The Norwegian Directorate of Health; 2010. [Google Scholar]
- Denison E, Vist GE, Underland V, Berg RC. Effects of organized follow-up of behaviour that may increase risk of disease in adults. Oslo: Norwegian Knowledge Centre for the Health Services, Report 12–2012; 2012. In Norwegian. [PubMed] [Google Scholar]
- Higgins JPT, Green S, editor. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011] ▪: The Cochrane Collaboration; 2011. [ www.cochrane-handbook.org] [Google Scholar]
- Guyatt G, Oxman A, Akl E, Kunz R, Vist G, Brozek J, Norris S, Falck-Ytter Y, Glasziou P, deBeer H, Jaeschke R, Rind D, Meerpohl J, Dahm P, Schünemann H. GRADE guidelines: 1. Introduction – GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64:383–394. doi: 10.1016/j.jclinepi.2010.04.026. [DOI] [PubMed] [Google Scholar]
- Isaacs AJ, Critchley JA, Tai SS, Buckingham K, Westley D, Harridge SD, Smith C, Gottlieb JM. Exercise Evaluation Randomised Trial (EXERT): a randomised trial comparing GP referral for leisure centre-based exercise, community-based walking and advice only. Health Technol Assess. 2007;11:1–165. doi: 10.3310/hta11100. [DOI] [PubMed] [Google Scholar]
- Park YH, Song M, Cho BL, Lim JY, Song W, Kim SH. The effects of an integrated health education and exercise program in community-dwelling older adults with hypertension: a randomized controlled trial. Patient Educ Couns. 2011;82:133–137. doi: 10.1016/j.pec.2010.04.002. [DOI] [PubMed] [Google Scholar]
- Elley CR, Kerse N, Arroll B, Robinson E. Effectiveness of counselling patients on physical activity in general practice: cluster randomised controlled trial. BMJ. 2003;326:793. doi: 10.1136/bmj.326.7393.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortier MS, Hogg W, O'Sullivan TL, Blanchard C, Sigal RJ, Reid RD, Boulay P, Doucet E, Bisson E, Beaulac J, Culver D. Impact of integrating a physical activity counsellor into the primary health care team: physical activity and health outcomes of the Physical Activity Counselling randomized controlled trial. Appl Physiol Nutr Metab. 2011;36:503–514. doi: 10.1139/h11-040. [DOI] [PubMed] [Google Scholar]
- Harrison R, Roberts C, Elton P. Does primary care referral to an exercise programme increase physical activity 1 year later? A randomized controlled trial. J Public Health. 2004;27:25–32. doi: 10.1093/pubmed/fdh197. [DOI] [PubMed] [Google Scholar]
- Stevens W, Hillsdon M, Thorogood M, McArdle D. Cost-effectiveness of a primary care based physical activity intervention in 45–74 year old men and women: a randomised controlled trial. Br J Sports Med. 1998;32:236–241. doi: 10.1136/bjsm.32.3.236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Armit C, Brown W, Marshall A, Ritchie C, Trost S, Green A, Bauman A. Randomized trial of three strategies to promote physical activity in general practice. Prev Med. 2009;48:156–163. doi: 10.1016/j.ypmed.2008.11.009. [DOI] [PubMed] [Google Scholar]
- Taylor A, Doust J, Webborn N. Randomised controlled trial to examine the effects of a GP exercise referral programme in Hailsham, East Sussex, on modifiable coronary heart disease risk factors. J Epidemiol Community Health. 1998;52:595–601. doi: 10.1136/jech.52.9.595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjørk Petersen C, Severin M, Wolff Hansen A, Curtis T, Grønbæk M, Schurmann Tolstrup J. A population-based randomized controlled trial of the effect of combining a pedometer with an intervention toolkit on physical activity among individuals with low levels of physical activity or fitness. Prev Med. 2012;54:125–130. doi: 10.1016/j.ypmed.2011.12.012. [DOI] [PubMed] [Google Scholar]
- Harland J, White M, Drinkwater C, Chinn D, Farr L, Howel D. The Newcastle exercise project: a randomised controlled trial of methods to promote physical activity in primary care. BMJ. 1999;319:828–832. doi: 10.1136/bmj.319.7213.828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker G, Gray S, Wright A, Fitzsimons C, Nimmo M, Lowry R, Mutrie N. The effect of a pedometer-based community walking intervention "Walking for Wellbeing in the West" on physical activity levels and health outcomes: a 12-week randomized controlled trial. Intl J Behav Nutr Phys Act. 2008;5:44. doi: 10.1186/1479-5868-5-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green B, McAfee T, Hindmarsch M, Madsen L, Caplow M, Buist D. Effectiveness of telephone support in increasing physical activity levels in primary care patients. Am J Prev Med. 2002;22:177–183. doi: 10.1016/s0749-3797(01)00428-7. [DOI] [PubMed] [Google Scholar]
- Kirkwood L, Aldujaili E, Drummond S. Effects of advice on dietary intake and/or physical activity on body composition, blood lipids and insulin resistance following a low-fat, sucrose-containing, high-carbohydrate, energy restricted diet. Int J Food Sci Nutr. 2007;58:383–397. doi: 10.1080/09637480701252336. [DOI] [PubMed] [Google Scholar]
- Kolt S, Shofield G, Kerse N, Garret N, Oliver M. Effect of telephone counseling on physical activity for low-active older people in primary care: a randomized, controlled trial. J Am Geriatr Soc. 2007;55:986–992. doi: 10.1111/j.1532-5415.2007.01203.x. [DOI] [PubMed] [Google Scholar]
- Prochaska J, Redding C, Evers K. In: Health behavior and health education. Theory, research, and practice. 4. Glanz K, Rimer B, Viswanath K, editor. San Francisco: Jossey Bass; 2008. The transtheoretical model and stages of change; pp. 97–121. [Google Scholar]
- Scales R, Miller J. Motivational techniques for improving compliance with an exercise program: skills for primary care clinicians. Curr Sports Med Rep. 2003;2:166–177. doi: 10.1249/00149619-200306000-00010. [DOI] [PubMed] [Google Scholar]
- Miller W, Rollnick S. Motivational interviewing: preparing people to change addictive behaviour. London: Gilford Press; 1991. [Google Scholar]
- Montaño D, Kasprzyk D. In: Health behavior and health education. Theory, research, and practice. 4. Glanz K, Rimer B, Viswanath K, editor. San Francisco: Jossey Bass; 2008. Theory of reasoned action, theory of planned behavior, and the integrated behavioral model; pp. 67–96. [Google Scholar]
- van Poppel M, Chinapaw M, Mokkink L, van Mechelen W, Terwee C. Physical activity questionnaires for adults. A systematic review of measurement properties. Sports Med. 2010;40:565–600. doi: 10.2165/11531930-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Terwee C, Mokkink L, van Poppel M, Chinapaw M, van Mechelen W, de Vet H. Qualitative attributes and measurement properties of physical activity questionnaires. Sports Med. 2010;40:525–537. doi: 10.2165/11531370-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Forsén L, Waaler Loland N, Vuillemin A, Chinapaw M, van Poppel M, Mokkink L, van Mechelen W, Terwee CB. Self-administered physical activity questionnaires for the elderly. Sports Med. 2010;40:601–623. doi: 10.2165/11531350-000000000-00000. [DOI] [PubMed] [Google Scholar]
- Clarke M. Standardising outcomes for clinical trials and systematic reviews. Trials. 2007;8:39. doi: 10.1186/1745-6215-8-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williamson P, Altman D, Blazeby J, Clarke M, Devane D, Gargon E, Tugwell P. Developing core outcome sets for clinical trials: issues to consider. Trials. 2012;13:132. doi: 10.1186/1745-6215-13-132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warren J, Ekelund U, Besson H, Mezzani A, Geladas N, Vanhees L. Assessment of physical activity - a review of methodologies with reference to epidemiological research: a report of the exercise physiology section of the European Association of Cardiovascular Prevention and Rehabilitation. Eur J Cardiovasc Prev Rehabil. 2010;17:127. doi: 10.1097/HJR.0b013e32832ed875. [DOI] [PubMed] [Google Scholar]
- Tugwell P, Boers M, Brooks P, Simon L, Strand V, Idzerda L. OMERACT: an international initiative to improve outcome measurement in rheumatology. Trials. 2007;8:38. doi: 10.1186/1745-6215-8-38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinha I, Smyth R, Williamson P. Using the delphi technique to determine which outcomes to measure in clinical trials: recommendations for the future based on a systematic review of existing studies. PLoS Med. 2011;8:e1000393. doi: 10.1371/journal.pmed.1000393. doi:10.1371/journal.pmed.1000393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Health and Clinical Excellence. Behaviour change at population, community, and individual levels. London: NICE Public Health Guidance 6; 2007. [Google Scholar]
- Lee L, Arthur A, Avis M. Evaluating a community-based walking intervention for hypertensive older people in Taiwan: A randomized controlled trial. Prev Med. 2007;44:160–166. doi: 10.1016/j.ypmed.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Kinmonth A-L, Wareham N, Hardeman W, Sutton S, Prevost T, Williams K, Ekelund U, Spiegelhalter D, Griffin S. Efficacy of a theory-based behavioural intervention to increase physical activityin an at-risk group in primary care (ProActive UK): a randomized trial. Lancet. 2008;371:41–48. doi: 10.1016/S0140-6736(08)60070-7. [DOI] [PubMed] [Google Scholar]
- Davies C, Spence J, Vandelanotte C, Caperchione C, Mummery K. Meta-analysis of internet-delivered interventions to increase physical activity levels. Int J Behav Nutr Phys Act. 2012;9:52. doi: 10.1186/1479-5868-9-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buchholz S, Wilbur J, Ingram D, Fogg L. Physical activity text messaging interventions in adults: a systematic review. Worldviews Evid Based Nurs. 2013;10:163–173. doi: 10.1111/wvn.12002. [DOI] [PubMed] [Google Scholar]
- Hillsdon M, Thorogood M, White I, Foster C. Advising people to take more exercise is ineffective: a randomised trial of physical activity promotion in primary care. Int J Epidemiol. 2002;31:808–815. doi: 10.1093/ije/31.4.808. [DOI] [PubMed] [Google Scholar]
- Craig C, Marshall A, Sjöström M, Bauman A, Booth M, Ainsworth B, Pratt M, Ekelund U, Yngve A, Sallis J, Oja P. International physical activity questionnaire: 12-country reliability and validity. Med Sci Sports Exer. 2003;35:1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB. [DOI] [PubMed] [Google Scholar]
- Arrol B, Jackson R, Beaglehole R. Validation of a three-month physical activity recall questionnaire with a seven-day food intake and physical activity diary. Epidemiology. 1991;2:296–299. doi: 10.1097/00001648-199107000-00011. [DOI] [PubMed] [Google Scholar]
- Godin G, Shepard R. A simple method to assess exercise behavior in the community. Can J Appl Sport Sci. 1985;10:141–146. [PubMed] [Google Scholar]
- Welk G, Schaben J, Morrow J. Reliability of accelerometry-based activity monitors: a generalizability study. Med Sci Sports Exerc. 2004;36:1637–1645. [PubMed] [Google Scholar]
- Taylor C, Coffey T, Berra K. Seven-day recall activity and self-report compared to a direct measure of physical activity. Am J Epidemiol. 1984;120:818–824. doi: 10.1093/oxfordjournals.aje.a113954. [DOI] [PubMed] [Google Scholar]
- Brown W, Burton N, Marshall A, Miller Y. Reliability and validity of a modified self-administered version of the Active Australia physical activity survey in a sample of mid-age women. Public Health. 2008;32:535–541. doi: 10.1111/j.1753-6405.2008.00305.x. [DOI] [PubMed] [Google Scholar]
- Andersen L. A maximal cycle exercise protocol to predict maximal oxygen uptake. Scand J Med Sci Sports. 1995;5:143–146. doi: 10.1111/j.1600-0838.1995.tb00027.x. [DOI] [PubMed] [Google Scholar]
- Åstrand P-O, Rodahl K. In: Textbook of work physiology. 3. Provenzano M, editor. New York: McGraw Hill; 1986. Physiological bases of exercise. Evaluation of physical performance of the baisi of tests; pp. 354–390. [Google Scholar]
- Sports Council, Health Education Council. Allied Dunbar national fitness survey: main findings. Northampton: Sports Council, Health Education Council; 1992. [Google Scholar]
- Ryan C, Grant P, Tigbe W. The validity and reliability of a novel activity monitor as a measure of walking. Br J Sports Med. 2006;40:779–784. doi: 10.1136/bjsm.2006.027276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick K, Sallis J, Long B, Calfas K, Wooten W, Heath G. A new tool for encouraging activity: Project PACE. Physician Sports Med. 1994;22:45–55. doi: 10.1080/00913847.1994.11947706. [DOI] [PubMed] [Google Scholar]
- Haymes E, Byrnes W. Walking and running energy expenditure estimated by Caltrac and indirect calorimetry. Med Sci Sports Exerc. 1993;25:1365–1369. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Example of search strategy. Search strategy for Ovid MEDLINE®. Note that the strategy comprises search terms to identify studies concerning physical activity, diet, smoking, and alcohol use.


