Abstract
Objective: Malaria is an infectious disease commonplace in tropical countries. For many years, major antimalarial drugs consisted of natural products, but since 1930s these drugs have been largely replaced with a series of synthetic drugs. This article tries to briefly indicate that some plants which previously were used to treat malaria, as a result of deficiencies of synthetic drugs, have revived into useful products once more. It also attempts to describe some tests which can be used to evaluate plant extracts for antimalarial activity.
Materials and Methods: By referring to some recent literatures, data were collected about plants used for the treatment of malaria, evaluation of plant extracts for antimalarial activity, modes of action of natural antimalarial agents, and recent research on antimalarial plants in Iran and other countries.
Results and Conclusion: There is an urgent need for the development of new treatments for malaria. Many countries have a vast precedence in the use of medicinal plants and the required knowledge spans many centuries. Although malaria is controlled in Iran, some researchers tend to study malaria and related subjects. In vitro biological tests for the detection of antimalarial activities in plant extracts are currently available. It is vital that the efficacy and safety of traditional medicines be validated and their active constituents be identified in order to establish reliable quality control measures.
Key Words: Antimalarial plants, Malaria, Natural Products
Introduction
Malaria is an infectious disease commonplace in tropical countries with the majority of their population still relying on the use of plant extracts to combat the ravages of the disease. It has been estimated that currently some 1,600 million people live where they can be exposed to malaria and that 400 million people live in countries where malaria is endemic (Phillipson and O’Neill, 1987 ▶). In 1982, it was calculated that approximately 215 million people were chronically infected and that some 150 million new cases were reported each year. The causing agents are 4 species of Plasmodium, viz. P. falciparum, P. malariae, P. ovale and P. vivax. The latter three species are less dangerous than P. falciparum but they persist in the liver and relapses can occur many years after primary infection. However, it is P. falciparum that is the cause of malignant tertiary malaria, which is life threatening.
For many years, quinine remained the major antimalarial drug, but from 1930s this natural product was largely replaced by a series of synthetic drugs including 8-aminoquinolines (e.g. primaquine), 4-aminoquinolines (e.g. chlooquine, amodiaquine) and folic acid synthesis inhibitors (e.g. proguanil, pyrimethamine). By the mid 1950s, it was confidently expected that malaria would be eradicated worldwide, but by the mid 1960s this confidence was undermined because of the problems of resistance (Phillipson and O’Neill, 1987 ▶). The vector mosquito developed resistance to potent insecticides such as DDT and certain strains of P. falciparum became resistant to chloroquine treatment. By the early 1980s, several strains of P. falciparum had become multi-drug resistant and today chloroquine resistance is widespread in S. E. Asia, S. America and E. Africa. With increase in international travel, the problem of malaria does not belong solely to the tropical countries (Phillipson and O’Neill, 1987 ▶).
Chemotherapeutic agents will continue to be in demand for the complete management of malaria and the issue of resistance means that discovering new antimalarial drugs is an urgent priority. In addition to the need for the development of new antimalarial drugs, it is essential to establish the efficacy and safety of traditional medicinal plants which are used to fight the disease. The purpose of this article is to briefly describe some plants that are used to treat malaria, to describe some test systems which can be used to evaluate plant extracts for antimalarial activity, and to consider some of the ongoing related researches.
Plants used for the treatment of malaria
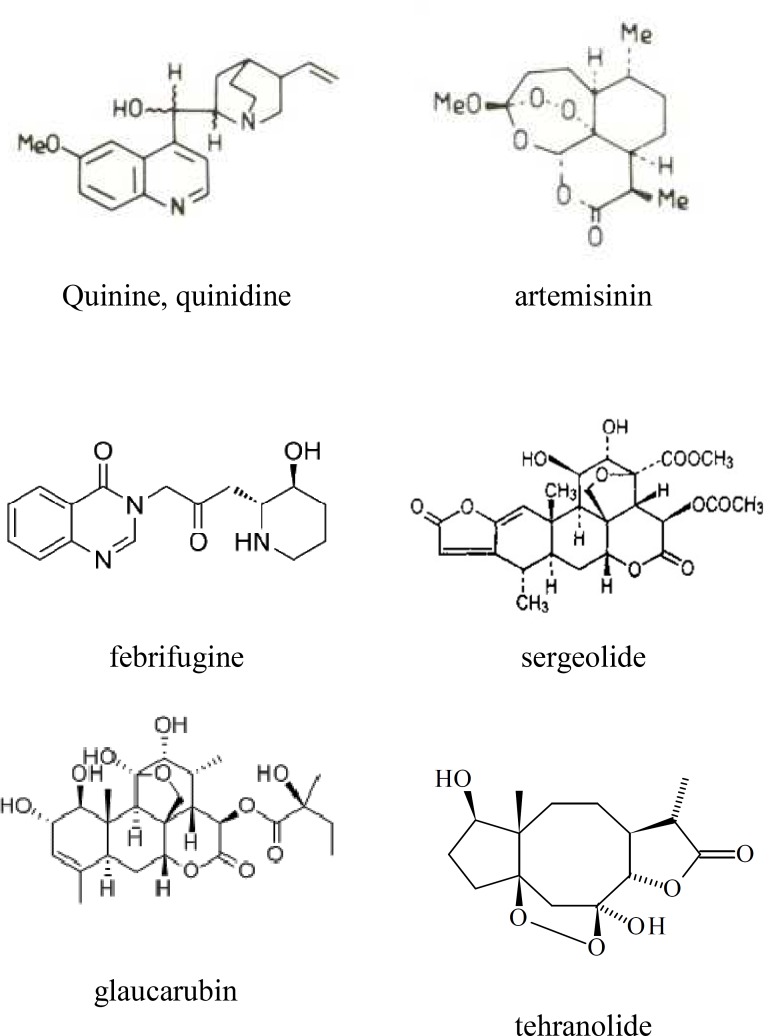
Cinchona species are well known for their antimalarial properties and the constituent alkaloid quinine is still acknowledged as an effective drug. Perhaps the less widely known stereoisomer quinidine (Figure 1) is at least as potent as, and possibly more potent than quinine (White, 1985 ▶). The Chinese traditional treatment of malaria includes the use of Artemisia annua (Compositae) and its active compound, artemisinin, which are currently under considerable interest. (Figure 1) (Phillipson and O’Neill, 1987 ▶). Artemisinin has a higher chemotherapeutic index than chloroquine and is effective in chloroquine-resistant strains of human malaria (Warhurst, 1985 ▶). Another species used as an antimalarial drug in Chinese traditional medicine is Dichroea febrifuga (Saxifragaceae) (Anonymous, 1975 ▶). The active principle, febrifugine (Fig. 1) has been used clinically against P. vivax and P. ovale but its liver toxicity makes it unacceptable as a useful antimalarial drug (Steck, 1972 ▶). The use of plants for the treatment of malaria extends to at least three continents including several countries in Africa (Sofowora, 1980 ▶), Americas (Lewis and Elwin-Lewis, 1971 ▶) and Asia (Chopra et al., 1956 ▶). The NAPRALERT natural product database lists species from 152 genera which have folklore reputations for antimalarial properties. It is important that using modern biological techniques plants with these traditional representations are investigated in order to establish their safety and efficacy, and to determine their value as sources of new antimalarial drugs.
Figure1.
Some examples of antimalarial natural products
Evaluation of plant extracts for antimalarial activity
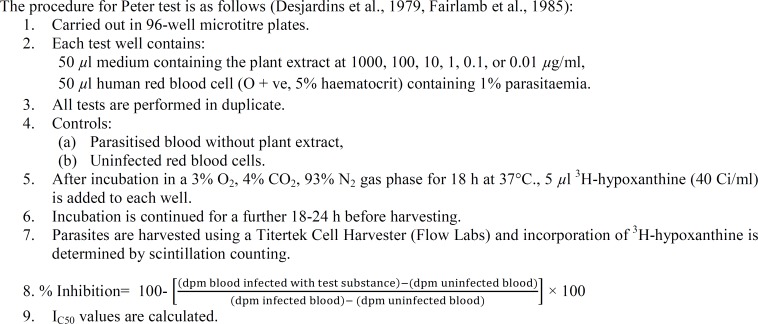
It is only in recent years that good in vitro tests have been established for antimalarial activity. However, previous expensive, time-consuming in vivo testing is still required, even for initial screening purposes. The largest published study for the assessment of plant extracts was reported by Phillipson and O’Neill (Phillipson and O’Neill, 1987 ▶). Some 600 plants representing around 126 families were extracted and their extracts tested for their in vitro activities against P. gallinaceum in chickens and P. chatemerium and P. lophurae in ducklings. Species from over 30 genera yielded extracts which were active against these avian malarias. However, the ability of such tests to predict activity against human malaria is not confirmed yet. Nevertheless, a number of noteworthy observations were made. Particularly, several species of Simaroubaceae which are used in traditional medicine in Africa, Americas and Asia, gives extracts which are active against avian malaria. The most significant advance in antimalarial testing followed the development of a method for the continuous in vitro culture of the human malaria parasite, P. falciparum (Trager and Jensen, 1976 ▶). In 1979, Desjardins et al. described a technique for the quantitative assessment of in vitro anti-P. falciparum activity. The test has since been modified (Fairlamb et al., 1985 ▶), but still relies on the ability to inhibit the incorporation of 3H-hypoxanthine into plasmodia. Further details of the in vitro test are given in Figure 2.
Figure 2.
determination of in vitro anti-Plasmodium falciparum activity in plant extracts.
Guidelines for antimalarial screening of drugs were established by WHO (WHO, 1973 ▶) and four stages were described. Primary screening establishes whether compounds are active against malaria parasites whereas secondary screening sets out to further qualify and quantify antiparasitic activity and to determine safety and comparative activities of analogues. The purpose of tertiary screening is to study non-human and human parasites in primates other than man prior to the fourth stage of the clinical testing. In assessing the activity of plant extracts for the presence of compounds with antimalarial activity, the techniques of primary and secondary screening as outlined by Peters (1987) can be utilized. For initial screening, both in vivo and in vitro techniques may be employed (Phillipson, 1991 ▶).
Preliminary experiments have been performed in order to determine whether this test would serve to evaluate the activity of crude extracts from plants (O'Neill et al., 1985 ▶). Ethanolic extracts of Artemisia annua and of A. vulgaris were prepared and the former was shown to contain artemisinin, which was absent from the latter. The IC50 values obtained on the basis of tenfold dilution followed by twofold dilutions within narrow ranges of concentration proved to be 3.9 µg/ml and 250 µg/ml, respectively. Hence, the in vitro test discriminated between species of the same genus in which the antimalarial compound, artemisinin, was present in only one of the two species.
Crude extracts of three species of Simaroubaceae, namely Brucea javanica and Simaba cedron, both of which are used in traditional medicine for the treatment of malaria, and of Ailanthus alitissima, were prepared for evaluation by the in vivo test. Sequential fractionation using solvents of different polarity resulted in petroleum ether, methanol, and aqueous extracts; the methanol extracts were subsequently partitioned between chloroform and water. The three species yielded active extracts and in each case the activity was concentrated in the chloroformic fraction (O'Neill et al., 1985 ▶). The ability of the in vitro test to detect active compounds in relatively crude fractions has been further demonstrated by assessing the activity of B. javanica fractions obtained from polyamide columns (O'Neill et al., 1985 ▶). Clearly, an in vitro test against multi-drug resistant P. falciparum that can be used for the evaluation of crude extracts of plants, has considerable value for the assessment of plants used in traditional medicine for the treatment of malaria.
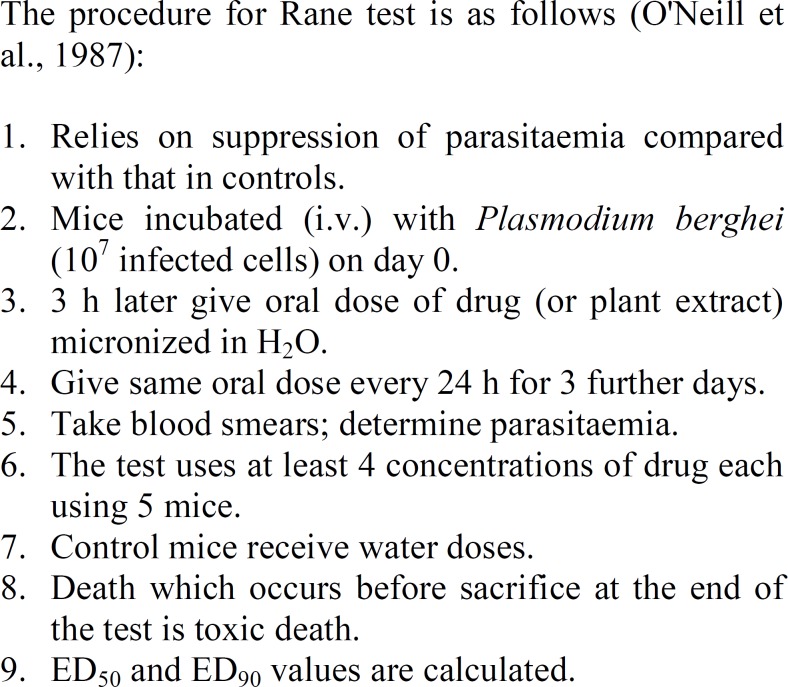
Extracts and isolated constituents selected on the basis of in vitro testing should be further studied for their in vivo antimalarial activity. Several in vivo test systems are available but their major drawback is that the used plasmodia are species which do not parasitize humans. P. falciparum is a selective human parasite. Nevertheless, useful information regarding in vivo antimalarial activity can be obtained by assessing the activity against rodent infections. In particular, the 4-day suppression of parasitaemia test against P. berghei infections in mice has been used to evaluate plant extracts (Fandeur et al., 1985 ▶, O'Neill et al., 1987 ▶). An outline of the procedure used in the evaluation is given in Figure 3.
Figure 3.
Determination of in vivo antimalarial activity against Plasmodium berghei infections in mice.
Mode of action of natural antimalarial agent
The effectiveness of any chemotherapeutic agent is dependent upon a favorable therapeutic ratio, i.e. the drug must kill or inhibit the parasite but have little or no toxicity to the host. Although a large number of natural products have been shown to be able to inhibit the growth of one or more species of protozoa, very few are proved to be selectivity toxic to the parasite. Selectivity depends on differences in biochemistry between the parasite and the host; such a drug can operate on a biochemical target in the parasite that is either absent, or significantly different in the host. However, the mode of action of many natural products with antiprotozoal activities is, at present, unknown and it is possible that some of these may act on biochemical targets unique to protozoa (Wright, 2009 ▶).
Recent research on antimalarial plants
The most significant recent development in naturally occurring antimalarial drugs is arguably the identification of artemisinin (Figure 1) as the active component of the plant Artemisia annua, which is used in traditional medicine as an antimalarial agent (Pillipson and O’Neill, 1987 ▶). This unique sesquiterpene contains an endoperoxide group that appears to be an essential requirement for its activity. It is particularly active in vivo against chloroquine-resistant P. falciparum and is reported to have relatively low toxicity. However, in the usual dose of 0.6 mg/day for 3 days, the average recurrence rate is more than 10% (Phillipson and O’Neill, 1987 ▶). Due to its highly lipophilic nature, there are inherent problems with its administration as a drug and several derivatives have been prepared, including arthemeter (methyldihydroartemisinin) and sodium artesunate (sodium dihyroartemisinin hemisuccinate). Artemisinin and its two derivatives have been used clinically for the treatment of cerebral malaria in an area where chloroquine resistance was endemic and the cure rate was greater than 90% (Li et al., 1982 ▶). The mode of action is not primarily at the level of nucleic acid synthesis but it appears to inhibit protein synthesis (Gu et al., 1983 ▶).
Like most naturally-occurring therapeutic agents, artemisinin exists in the plant in very small concentration. Chinese workers were unable to find artemisinin in about 30 other Artemisia species. In another attempt, a group at the Walter Reed Army Institute of Research studied some 70 species and did not find artemisinin in any of them (Klayman, 1993 ▶).
It is often argued by protagonists of herbal medicine that the total plant extract contains a mixture of substances which act synergistically and hence it is better for a patient to take the whole plant or an extract rather than a single isolated active ingredient. In this context, it is interesting to note that some flavonoids, which do not possess in vitro activity against P. falciparum, cause a significant reduction in the IC50 value of artemisinin when it is assessed for its ability to inhibit the incorporation of 3H-hypoxanthine (Elford et al., 1987 ▶). These flavonoids have little effect on the activity of chloroquine under the same test conditions. It is possible that flavonoids, which are present in A. annua, may significantly alter the clinical potential of artemisinin in the treatment of chloroquine–resistant malaria. Although endoperoxides appear to be rare as natural products, it is noteworthy that investigation of another antimalarial plant, Artabotrys hexapetalus (Annonaceae), has revealed that its active principle, yingzhausu A (Figure 1), also contains an endoperoxide (Xiao, 1983 ▶). Another component containing an endoperoxide is tehranolide and is identified in Artemisia diffusa from Iran (Rustaiyan et al., 1989 ▶).
It is demonstrated that crude extracts of A. diffusa inhibits the growth of P. berghei in vivo in mice. The microscopic examination of Giemsa stained slides showed a virtual absence of all blood-stage of murine malaria treated with three concentrations of herbal extracts including 27, 2.7 and 0.27 mg/ml. These observations suggest that the active constituents in the extract may be cytotoxic for P. berghei, thereby inhibiting their development to the erythrocytic stage.
The results specifically indicated the inhibitory effects of the A. diffusa crude extracts and the fraction which contains sesquiterpene lactones including tehranolide, on the developmental stages of P. berghei by decreasing parasitaemia (Rustaiyan et al., 2009 ▶).
As artemisinin is a complex molecule, much effort has been put into synthesizing compounds based on the 1,2,4-trioxane ring of artemisinin. Many compounds have been produced from artemisinin, some of which have promising in vivo activities in animal models (Wright. 2009 ▶). A number of mono- and bicyclic endoperoxides were prepared and tested for antimalarial activity in search of a simplified analogue of the 5-oxygen-substitued 1,2,4-trioxane ring structure of the naturally occurring antimalarial artemisinin (Figure 2). The compounds were assayed in an in vitro system for antimalarial activity against chloroquine-susceptible and chloroquine-resistant strains and their antimalarial activity against P. falciparum (Rustaiyan et al., 2009 ▶).
Species of Simaroubaceae are used pantropically for the treatment of malaria in vivo. The antimalarial activity has been demonstrated for a number of quassinoids, which are bitter upon tasting, biosynthetically degraded triterpenes and are characteristic of the family (Fandeur et al., 1985 ▶, Chan et al, 1986 ▶, Guru et al., 1983 ▶, Pavanand et al., 1986 ▶, Trager and Polonsky, 1981 ▶, O'Neill et al., 1986 ▶). Bruceantin, simalikalactone D, glaucarubinone, soularubinone, and sergeolide have been demonstrated to be markedly active against P. falciparum in vitro. Sergeolide reduced virulence in P. berghei-infected mice when administered subcutaneously at 0.26 mg/Kg/day but its high toxicity, with a LD50 of 1.8 mg/Kg, is indicative of its unsuitability for the curative treatment of malaria (Fandeur et al., 1985 ▶).
A series of 14 quassinoids tested for in vitro antimalarial activity were all active, having IC50 values below 0.41 µg/ml and 10 of them possessed IC50 values less than 0.02 µg/ml (O’Neill et al., 1986). Under the same test condition, chloroquin diphosphate had an IC50 value of 0.21µg/ml. The presence and nature of the ester function at C-15 is of importance for in vitro antiplasmodial activity. Glaucarubin is about three times more active than chaparrin (Figure 1), whereas glaucarubinone is about twice as potent as halocanthone, and bruceanthin is more than three times more active than brusatol (Figure 1). The A ring substitution pattern is also crucial for activity e.g. glaucarubinone having an α, β-unsaturated keto function in ring A is over 10 times more active than glaucarubin (Figure 1). Highly active quassinoids may possess either a C-20/C-11 or a C-20/C-13 oxygen bridge (Figure 1). The nature of the C-15 ester function, the A ring substitution, and the oxygen bridge from C-20 to either C-11 or C-13 appear to be crucial for in vitro antimalarial activity, and in these respects there are similarities in the structural requirements needed for antileukemic activity. It has observed that for five quassinoids tested, the in vitro antimalarial activities paralleled their antileukemic activities. However, in a study with fourteen quassinoids, it was noted that in vitro antimalarial activity did not parallel the in vivo P-388 lymphocytic leukemia optimal test to control survival values or optimal doses reported previously (Phillipson and O’Neill, 1987 ▶).
The mechanism of action of quassinoids against Plasmodium spp. is not understood and warrants further studies. The interesting results reported to date indicate that these compounds require more detailed investigation, particularly in order to exploit differences in specificity between their antiplasmodial and cytotoxic activities.
Research on antimalarial plants in Iran
Except for identification of tehranolide in Artemisia diffusa and its antimalarial effect, (described above (Rustaiyan et al., 1989 ▶)), some other works are (Table 1).
Table 1.
Research on antimalarial plants in Iran.
| Author | Plant | Plasmodium | Effect |
|---|---|---|---|
| Hakiminia, 2004 | Cichorium intybus | P. berghei | Doses 0.07 and 0.1 mg/kg were the most effective and provided 0 of parasitaemia in 4th day |
| Esmaeili et al., 2009 | Glycyrrhiza glabra | P. falciparum and P. berghei | antiplasmodial activity |
| Rustaiyan et al., 2009 | Artemisia diffusa | P. berghei | decreasing parasitaemia, inhibit the growth |
| Nahrevanian et al., 2010 | Artemisia khorasanica | P. berghei | successfully tested |
| Ramazaniet al., 2010a | Artemisia annua and A. absinthium | P. bergei | reduced parasitaemia in mice by 94.28% and 83.28% |
| Ramazani et al., 2010b |
Prosopis juliflora,
Boerhavia elegans and Solanum surattense |
P. falciparum
chloroquine-resistant and sensitive strains |
IC50 [less than or equal to] 50 µg/ml |
| Ramazani et al., 2010b |
Prosopis juliflora,
Boerhavia elegans and Solanum surattense |
P. berghei | good antiplasmodial activity |
In vitro and in vivo antiplasmodial tests were carried out on selected plants traditionally used in Iran. Thirty-two plants were extracted with methanol and tested for their in vitro (pLDH assay) activity against Plasmodium falciparum, in vivo activity against P. berghei, and assessed for any cytotoxicity against the human cancer cell line MCF7 and the normal cell MDBK. Extracts from four plants, Buxus hyrcana, Erodium oxyrrhnchum, Glycyrrhiza glabra, and Ferula oopoda were found to have significant antiplasmodial activity (IC50 ranging from 4.7 to 26.6 g/ml). G. glabra showed antiplasmodial activity and has selectivity for P. falciparum and P. berghei when tested on mammalian cells (Esmaeili et al., 2009 ▶).
The purpose of next research was to study five Artemisia species from Iran for their in vitro and in vivo antimalarial property and detection of artemisinin in the active. Dried plants were extracted by 80% ethanol, and total extracts were investigated for antiplasmodial property and artemisinin content by TLC, HPLC, and 1H-NMR techniques. Two plants (A. annua L. and Artemisia absinthium L.) showed good antiplasmodial activity against multidrug resistant and sensitive strain of P. falciparum. A. absinthium and A. annua at concentrations of 200 mg/kg for 4 days reduced parasitaemia in mice infected with P. bergei by 94.28% and 83.28%, respectively, but they could not detect artemisinin in all plants studied in this research. The antiplasmodial property of these two herbs is possibly related to essential oils that present in high amounts in their extracts (Ramazani et al., 2010a ▶).
Antiplasmodial activities of extracts of Boerhavia elegans and Solanum surattense are reported for the first time. The crude ethanolic extracts were tested for in vitro antiplasmodial activity against two strains of Plasmodium falciparum: K1 (chloroquine-resistant strain) and CY27 (chloroquine-sensitive strain), using the parasite lactate dehydrogenase (pLDH) assay. The antiplasmodial activity of the extracts was also assessed in the 4-day suppressive antimalarial assay in mice inoculated with P. berghei. Crude ethanolic extracts showed good antiplasmodial activity and were further fractionated by partitioning in water and dichloromethane. Often plant species assayed, three species: B. elegans, S. surattense and Prosopis juliflora showed promising antiplasmodial activity in vitro (IC50 [less than or equal to] 50 µg/ml) and in vivo with no toxicity. The dichloromethane fraction of three extracts revealed stronger antiplasmodial activity than the total extracts (Ramazani et al., 2010b ▶).
The aerial parts of Iranian flora A. khorasanica were collected at flowering stage from Khorassan Province, northeastern Iran in 2008. Toxicity of herbal extracts was assessed on mice, and its antimalarial efficacy was investigated on infected P. berghei animals. The herbal extract was successfully tested in vivo for its antiplasmodial activity through artemisinin composition, which is widely used as a standard malaria treatment. Although, this study confirmed less antimalarial effects of A. khorssanica against murine malaria in vivo, but there are some evidences on improving the infection using this medication (In vivo antimalarial effects of Iranian flora Artemisia khorassanica against Plasmodium berghei and pharmacochemistry of its natural components (Nahrevanian et al., 2010 ▶).
Antimalarial activity of Cichorium intybus against P. berghei infections in mice (modified Peter’s method) was evaluated, too. Doses 0.07 and 0.1 mg/kg were the most effective and eliminated parasitaemia in the fourth day. Chloroquine was used as a positive control (Hakiminia, 2004 ▶).
Conclusion
There is an urgent need for the development of novel drugs to treat malaria. Biological investigations into plants used traditionally for primary health care are one obvious way in which searching for new leading compounds should concentrate. Many countries have vast experience in the use of medicinal plants and the required knowledge spans many centuries. In vitro biological tests for the detection of antimalarial activity in plant extracts are currently available and some measure of specificity of action can be obtained by monitoring their cytotoxicity in mammalian cells (O'Neill et al., 1986 ▶, Keene et al., 1986 ▶). The biological activities of several compounds isolated from species of the Simaroubaceae have provided interesting leads which require further investigation (O'Neill et al., 1986 ▶, O'Neill et al., 1987 ▶). It is vital that the efficacy and safety of traditional medicines be validated and their active constituents be identified so that reliable quality controls can be established.
References
- Anonymous . Herbal Pharmacology in the people republic of China. Washington: National Academy of Sciences; 1975. [Google Scholar]
- Chan KL, O'Neill MJ, Phillipson JD, Warhurst DC. Plants as sources of antimalarial drugs. Part 3- Eurycoma longifolia. Planta Med. 1986;52:105. doi: 10.1055/s-2007-969091. [DOI] [PubMed] [Google Scholar]
- Chopra RN, Nayar SL, Chpra IC. Glossary of Indian Medicinal Plants. New Delhi: Council of Scientific and Industrial Research; 1956. [Google Scholar]
- Desjardins RE, Canfield CJ, Haynes JD, Chulay JD. Quantitative assessment of antimalarial activity in vitro by a semiautomated microdilution technique. Antimicrob Agents Chemother. 1979;16:710–718. doi: 10.1128/aac.16.6.710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elford BC, Roberts MF, Phillipson JD, Wilson RJ. Potentiation of the antimalarial activity of qinghaosu by methoxylated flavones. Trans R Soc Trop Med Hyg. 1987;81:434–436. doi: 10.1016/0035-9203(87)90161-1. [DOI] [PubMed] [Google Scholar]
- Esmaeili S, Naghibi F, Mosaddegh M, Sahranavard S, Ghafari S, Abdullah NR. Screening of antiplasmodial properties among some traditionally used Iranian plants. J Ethnopharmacol. 2009;121:400–404. doi: 10.1016/j.jep.2008.10.041. [DOI] [PubMed] [Google Scholar]
- Fairlamb AH, Warhurst DC, Peters W. An improved technique for the cultivation of Plasmodium falciparum in vitro without daily medium change. Ann Trop Med Parasitol. 1985;79:379–384. doi: 10.1080/00034983.1985.11811935. [DOI] [PubMed] [Google Scholar]
- Fandeur T, Moretti C, Polonsky J. In vitro and in vivo assessement of the antimalarial activity of sergeolide. Planta Med. 1985;51:20–23. doi: 10.1055/s-2007-969382. [DOI] [PubMed] [Google Scholar]
- Gu HM, Warhurst DC, Peters W. Rapid action of Qinghaosu and related drugs on incorporation of [3H]isoleucine by Plasmodium falciparum in vitro. Biochem Pharmacol. 1983;32:2463–2466. doi: 10.1016/0006-2952(83)90002-3. [DOI] [PubMed] [Google Scholar]
- Guru PY, Warhurst DC, Harris A, Phillipson JD. Antimalarial activity of bruceantin in vitro. Ann Trop Med Parasitol. 1983;77:433–735. doi: 10.1080/00034983.1983.11811732. [DOI] [PubMed] [Google Scholar]
- Hakiminia Gh. Antimalarial activity of Cichorium intybus. [Dissertation] Tehran, Iran: Shahid Beheshti University of Medical Sciences; 2004. [Google Scholar]
- Keene AT, Harris A, Phillipson JD, Warhurst DC. In vitro amoebicidal testing of natural products; Part I. Methodology. Planta Med. 1986;52:278–285. [PubMed] [Google Scholar]
- Kepler JA, Philip A, Lee YW, Musallam HA, Carroll FI. Endoperoxides as potential antimalarial agents. J Med Chem. 1987;30:1505–1509. doi: 10.1021/jm00391a039. [DOI] [PubMed] [Google Scholar]
- Klayman DL. Artemisia annua. In: Kinghorn AD, Balandrin MF, editors. Human Medicinal Agents from Plants. Washington: American Chemical Society; 1993. p. 243. [Google Scholar]
- Lewis WH, Elwin-Lewis MPF. Medical Botany. New York: Wiley; 1971. [Google Scholar]
- Li GQ, Guo XB, Jin R, Wang ZC, Jian HX, Li ZY. J Tradit Chin Med. 1982 Clinical studies on treatment of cerebral malaria with qinghaosu and its derivatives;2:125–130. [PubMed] [Google Scholar]
- Nahrevanian H, Esmaeili B, Kazemi M, Nazem H, Amini M. In vivo antimalarial effects of Iranian flora Artemisia khorassanica against Plasmodium berghei and pharmacochemistry of its natural components. Iranian J Parasitol. 2010;5:6–19. [PMC free article] [PubMed] [Google Scholar]
- O'Neill MJ, Bray DH, Boardman P, Chan KL, Phillipson JD, Warhurst DC, Peters W. Plants as sources of antimalarial drugs, Part 4: Activity of Brucea javanica fruits against chloroquine-resistant Plasmodium falciparum in vitro and against Plasmodium berghei in vivo. J Nat Prod. 1987;50:41–48. doi: 10.1021/np50049a007. [DOI] [PubMed] [Google Scholar]
- O'Neill MJ, Bray DH, Boardman P, Phillipson JD, Warhurst DC, Peters W, Suffness M. Plants as sources of antimalarial drugs: in vitro antimalarial activities of some quassinoids. Antimicrob Agents Chemother. 1986;30:101–104. doi: 10.1128/aac.30.1.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neill MJ, Bray DH, Boardman P, Phillipson JD, Warhurst DC. Plants as sources of antimalarial drugs. Part 1. In vitro test method for the evaluation of crude extracts from plants. Planta Med. 1985;51:394–398. doi: 10.1055/s-2007-969529. [DOI] [PubMed] [Google Scholar]
- Pavanand K, Nutakul W, Dechatiwongse T, Yoshihira K, Yongvanitchit K, Scovill JP, Flippen-Anderson JL, Gilardi R, George C, Kanchanapee P, Webster HK. In vitro antimalarial activity of Bruceajavanica against multi-drug resistant Plasmodiumfalciparum. Planta Med. 1986;52:108–111. [PubMed] [Google Scholar]
- Peters W. Chemotharapy and Drug Resistance in Malaria. London: Academic Press; 1987. [Google Scholar]
- Phillipson JD. Assays for antimalarial and amoebicidal activities. In: Hostettmann K, Dey PM, Harborne JB, editors. Methods in Plant Biochemistry. Vol. 6. London: Academic Press; 1991. p. 138. [Google Scholar]
- Phillipson JD, O’Neill MJ. Antimalarial and amoebicidal natural products. In: Hostettmann K, Lea PJ, editors. Biologically Active Natural Products. Oxford: Clarendon Press; 1987. pp. 49–64. [Google Scholar]
- Ramazani A, Sardari S, Zakeri S, Vaziri B. In vitro antiplasmodial and phytochemical study of five Artemisia species from Iran and in vivo activity of two species. Parasitology Res. 2010;107:593–599. doi: 10.1007/s00436-010-1900-4. [DOI] [PubMed] [Google Scholar]
- Ramazani A, Zakeri S, Sardari S, Khodakarim N, Djadid ND. In vitro and in vivo anti-malarial activity of Boerhavia elegans and Solanum surattense. Malaria J. 2010:124. doi: 10.1186/1475-2875-9-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rustaiyan A, Nahrevanian H, Kazemi M. A new antimalarial agent; effect of extracts of Artemisia diffusa against Plasmodium berghei. Pharmacognosy Magazine. 2009;4:1–7. [Google Scholar]
- Rustaiyan A, Sigari H, Jakupovic J, Grenz M. A sesquiterpene lactone from Artemisia diffusa. Phytochem. 1989;28:2723–2725. [Google Scholar]
- Sofowora A. The present status of knowledge of the plants used in traditional medicine in Western Africa: a medical approach and a chemical evaluation. J Ethnopharmacol. 1980;2:109–118. doi: 10.1016/0378-8741(80)90004-5. [DOI] [PubMed] [Google Scholar]
- Steck EA. The Chemotherapy of Protozoan Diseases. Washington: Walter Reed Army Institute of Research; 1972. [Google Scholar]
- Trager W, Jensen JB. Human malaria parasites in continuous culture. Science. 1976;193:673–675. doi: 10.1126/science.781840. [DOI] [PubMed] [Google Scholar]
- Trager W, Polonsky J. Antimalarial activity of quassinoids against chloroquine-resistant Plasmodium falciparum in vitro. Am J Trop Med Hyg. 1981;30:531–537. doi: 10.4269/ajtmh.1981.30.531. [DOI] [PubMed] [Google Scholar]
- Wright CW. Antiprotozoal Natural Products. In: Evans EC, editor. Trease and Evans Pharmacognosy. 16th ed. Edinburgh: Saunders; 2009. pp. 428–434. [Google Scholar]
- Warhurst DC. New drugs and their potential use against drug-resistant malaria. Ann Ist Super Sanita. 1985;21:327–336. [PubMed] [Google Scholar]
- White NJ. Clinical pharmacokinetics of antimalarial drugs. Clin Pharmacokinet. 1985;10:187–215. doi: 10.2165/00003088-198510030-00001. [DOI] [PubMed] [Google Scholar]
- WHO . WHO special programme for Research and Training in Tropical Diseases. Geneva: WHO; 1973. [Google Scholar]
- Xiao P. Recent developments on medicinal plants in China. J Ethnopharmacol. 1983;7:95–109. doi: 10.1016/0378-8741(83)90083-1. [DOI] [PubMed] [Google Scholar]