Abstract
OBJECTIVE:
To evaluate the applicability of the London Chest Activity of Daily Living (LCADL) scale in patients on the waiting list for lung transplantation.
METHODS:
This was a cross-sectional study, conducted between May and September of 2010, involving 26 male and female patients on the waiting list for lung transplantation and treated at the Pulmonary Rehabilitation Program in the Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, located in the city of Porto Alegre, Brazil. We evaluated the patients using the six-minute walk test (6MWT) and pulmonary function tests. We also obtained the LCADL scores, as well as the modified Borg scale scores for sensation of dyspnea and leg fatigue. Cronbach's alpha coefficient was used to determine the internal consistency of the LCADL scale. Linear regression analysis was used in order to identify associations between the total LCADL score (expressed as a percentage) and the variables studied.
RESULTS:
According to the LCADL scale results, 69% of the patients reported that the performance of their activities of daily living was significantly impaired by their dyspnea. The internal consistency of the LCADL scale was 0.89. After adjusting for age and FEV1, we found that the total LCADL scale score showed statistically significant negative associations with the six-minute walk distance (β = −0.087; p < 0.001) and the six-minute walk work (β = −0.285; p < 0.001).
CONCLUSIONS:
Our findings suggest that the LCADL scale is a useful tool for assessing patients on the waiting list for lung transplantation.
Keywords: Activities of daily living, Lung transplantation, Dyspnea
Abstract
OBJETIVO:
Avaliar a aplicabilidade da escala London Chest Activity of Daily Living (LCADL), em pacientes em lista de transplante pulmonar.
MÉTODOS:
Estudo transversal com 26 pacientes em lista de espera para transplante de pulmão, de ambos os sexos, entre maio e setembro de 2010 tratados no Programa de Reabilitação Pulmonar, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, em Porto Alegre, RS. Todos os pacientes foram submetidos ao teste de caminhada de seis minutos (TC6) e a teste de função pulmonar e foram obtidos os escores das escalas LCADL e de Borg modificada para dispneia e fadiga das pernas. O teste alfa de Cronbach foi utilizado para verificar a consistência interna da escala LCADL. A análise de regressão linear foi utilizada para identificar associações entre o escore total em porcentagem da escala LCADL e as variáveis estudadas.
RESULTADOS:
Segundo os resultados da LCADL, 69% dos pacientes indicaram que suas atividades de vida diária são muito comprometidas pela dispnéia. A consistência interna da escala LCADL foi de 0,89. Houve associações negativas estatisticamente significativas entre o escore total da escala LCADL e distância percorrida no TC6 (β = −0,087; p < 0,001) e trabalho realizado no TC6 (β = −0,285; p < 0,001), quando os dados foram ajustados por idade e VEF1.
CONCLUSÕES:
Esses achados sugerem que a escala LCADL é um instrumento útil para avaliar o desempenho funcional dos pacientes em listas de transplante pulmonar.
Introduction
The prevalence of respiratory diseases has increased substantially in recent years, and respiratory diseases have come to play a major role in the morbidity and mortality profiles of the population. A public health problem, COPD ranked fourth among the leading causes of death worldwide in 2006, and by 2020, it is estimated that it will be the third leading cause of mortality worldwide.( 1 , 2 )
In chronic lung disease patients who have severe progressive impairment and a high level of inactivity, lung transplantation is recommended as an essential therapeutic intervention, being an effective treatment option.( 3 ) The most common indications for this intervention are emphysema (in 36%), idiopathic pulmonary fibrosis (in 20%), and cystic fibrosis (in 16%).( 4 ) In transplantation candidates, assessment of their level of physical activity is an important tool for quantifying the impact of the disease on their activities of daily living (ADL).( 5 )
The six-minute walk distance (6MWD) is also considered a good marker of functional capacity in ADL, and the use of the six-minute walk test (6MWT) is recommended in the assessment of patients with exercise-induced lung disease or cardiovascular disease, given that it provides an overall analysis of the respiratory, cardiac, and metabolic systems.( 6 ) Another way of assessing the functional status of a patient is to use scales or questionnaires.( 7 ) The use of questionnaires or scales has shown the impact that the disease has on the level of physical activity and the quality of life of chronic disease patients, indirectly reflecting the degree to which the disease interferes with their ADL.( 8 ) Currently, there are few validated scales to investigate the impairment of functional capacity in chronic lung disease patients, especially in severely impaired patients who are candidates for lung transplantation.( 9 )
The London Chest Activity of Daily Living (LCADL) scale is a tool aimed at assessing the level of dyspnea during ADL. It has four domains: self-care; household activities; physical activity; and leisure activities.( 8 , 10 ) The LCADL scale, which is considered an inexpensive and user-friendly instrument, can be a feasible clinical tool for assessment and monitoring of dyspnea-related functional impairment in chronic lung disease patients, as well as for pre- and post-intervention assessment. Although this instrument has been validated for use in COPD patients, there are few studies evaluating the use of this scale in lung disease patients already on the waiting list for lung transplantation. The objective of the present study was to evaluate the applicability of the LCADL scale in patients on the waiting list for lung transplantation by assessing the psychometric properties of the scale and the relationship between the scale scores and the 6MWT results.
Methods
This was a cross-sectional study involving patients treated at the Pulmonary Rehabilitation Program in the Pereira Filho Ward of the Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, located in the city of Porto Alegre, Brazil. All male and female patients who were on the waiting list for lung transplantation between May and September of 2010 and who gave written informed consent were included in the study. Patients who had cognitive or motor limitations, as well as those who had had respiratory infection in the three weeks before the assessment, were excluded from the study.
The version of the LCADL scale used in the present study has been validated for use in Brazil.( 8 ) The LCADL scale consists of 15 questions divided into four domains: self-care; household activities; physical activity; and leisure activities. Each question in each domain is scored by patients on a 0-5 scale, with 5 representing the greatest dyspnea-related impairment in ADL. The total score can range from 0 to 75 points, with higher values translating to greater limitation in ADL. In addition, the LCADL scale has a multiple-choice question, i.e., question 16, which refers to specific information about dyspnea-related impairment in ADL in any situation and to which patients are required to answer "Quite a bit", "Slightly", or "Not at all". The LCADL scale, which was administered as an interview by the same researcher, was interpreted on the basis of its total score (expressed as a percentage).
The 6MWT was performed in accordance with the American Thoracic Society recommendations,( 11 ) considering reference equations for healthy adults.( 12 ) The six-minute walk work (6MWW) was calculated by multiplying distance walked by body weight (in kg).( 13 ) Before and after the 6MWT, patients were assessed for their perception of dyspnea and leg fatigue with the modified Borg scale.
All pulmonary function tests were carried out in accordance with the technical standards and the acceptability and reproducibility criteria of the American Thoracic Society/European Respiratory Society.( 14 ) Flow-volume curves were obtained with a Koko spirometer (Ferraris Respiratory, Louisville, CO, USA). The parameter used to assess pulmonary function was FEV1. Results are reported as a percentage of predicted reference values.( 15 )
Statistical analysis was performed as described below. The variables were assessed for distribution by using the Kolmogorov-Smirnov test. Continuous variables are expressed as means and 95% CIs, and categorical variables are expressed as absolute and relative frequencies. Bivariate and multivariate linear regression analyses were performed to identify possible associations between the LCADL scale results and the covariates of interest (6MWD, 6MWW, age, FEV1, and the Borg scale scores). Initially, all covariates that had a p < 0.10 in the univariate analysis were included in the multivariate model. The next step was to exclude the covariates that were found to have critical p values (values that were not significant) one by one. This step was repeated until all variables remaining in the model had a p < 0.05. The internal consistency of the LCADL scale was measured with Cronbach's alpha coefficient, which investigates specific correlations between total and domain scores. For the purpose of calculating this coefficient, values of p ≥ 0.70 are considered adequate.( 16 ) In addition, the proportion of patients with minimum and maximum scores (floor/ceiling effect) was calculated.
The study was approved by the local research ethics committee (Protocol no. 3293/10) in May of 2010.
Results
The present study included 26 subjects, 10 (38%) of whom were male. The mean age was 48 ± 14 years. The characteristics of the sample are shown in Table 1.
Table 1. Characteristics of the sample of patients on the waiting list for lung transplantation. a .
| Variable | Result |
| BMI, kg/m2 | 23.8 ± 30.2 |
| FEV1, % of predicted | 35.1 ± 17.4 |
| FVC, % of predicted | 43. 8 ± 14.9 |
| FVC/FEV1 | 0.67 ± 0.23 |
| 6MWD, m | 331.4 ± 118.7 |
| 6MWW, m/kg | 101.9 ± 30.2 |
: body mass index;
: six-minute walk distance;
: six-minute walk work.
Values expressed as mean ± SD.
In the sample as a whole, 14 (54%) and 12 (46%) of the patients had obstructive and restrictive lung disease, respectively. The patients included in the present study had the following diagnoses: pulmonary fibrosis, 13 (50%); COPD, 4 (15%); cystic fibrosis, 2 (8%); bronchiectasis, 3 (12%); and others, 4 (15%).
The mean total LCADL score (expressed as a percentage) was 36%. In the sample as whole, 16 patients achieved a total LCADL score above 50%. In 69% of the cases, the answer to the qualitative question on the LCADL scale, i.e., question 16, which refers to the level of dyspnea-related impairment in ADL, was "Quite a bit".
The overall alpha value was 0.89, and the alpha values for each domain ranged from 0.72 to 0.94. There was no floor or ceiling effect.
In the univariate analysis, the 6MWD, the modified Borg scale scores, and the 6MWW showed significant associations with the total LCADL score (expressed as a percentage; Table 2).
Table 2. Univariate analysis of the total score on the London Chest Activity of Daily Living scale (expressed as a percentage).
| Variable | β | 95% CI | p | |
| Age, years | 0.226 | − 0.222 to 0.674 | 0.323 | |
| Diagnosis | ||||
| COPD | 0.000 | |||
| Pulmonary fibrosis | − 16.325 | − 34.000 to 1.351 | 0.070 | |
| Cystic fibrosis | − 8.244 | − 26.362 to 9.874 | 0.372 | |
| Bronchiectasis | − 9.658 | − 30.574 to 11.259 | 0.365 | |
| Others | − 10.746 | − 27.024 to 5.532 | 0.196 | |
| FEV1, % of predicted | 0.373 | − 0.001 to 0.741 | 0.005 | |
| 6MWD, m | − 0.079 | − 0.132 to − 0.027 | 0.002 | |
| Modified Borg scale score | − 0.056 | − 2.461 to 2.349 | 0.964 | |
| 6MWW, m/kg | − 0.348 | − 0.563 to − 0.133 | 0.002 |
: six-minute walk distance
: six-minute walk work
In the multivariate analysis, the 6MWD (Figure 1) and the 6MWW showed a significant inverse association with the total LCADL score (expressed as a percentage; Table 3).
Figure 1. Relationship between the total score on the London Chest Activity of Daily Living scale (expressed as a percentage) and the six-minute walk distance (6MWD). (β = −0.103; p < 0.001).
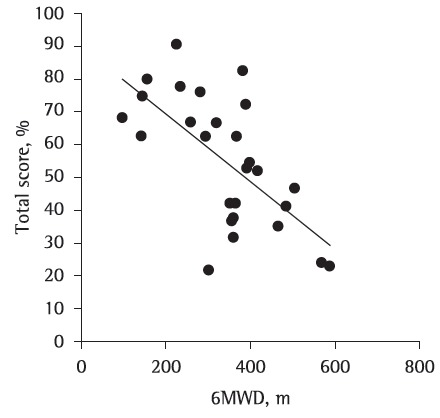
Table 3. Multivariate analysis of the total score on the London Chest Activity of Daily Living scale (expressed as a percentage).
| Variable | β | 95% CI | p |
| 6MWD, m | 0.087 | − 0.128 to − 0.046 | < 0.001 |
| 6MWW, m/kg | 0.285 | − 0.448 to − 0.123 | < 0.001 |
: six-minute walk distance
: six-minute walk work
Discussion
The objective of the present study was to evaluate the applicability of the LCADL scale in patients on the waiting list for lung transplantation. This instrument was found to have good reliability and to be associated with the 6MWD and the 6MWW. Our data showed that the total LCADL score was inversely associated with these parameters in the study population. Higher scores on the LCADL scale translated to lower 6MWD and lower 6MWW.
Carpes et al.( 8 ) showed that the LCADL scale correlated with the 6MWD in COPD patients. When we compared the LCADL scores with the different diagnoses of patients, we found no significant differences. However, we observed that COPD patients had higher scores on the LCADL scale than did those with other diagnoses. The lack of significance in the differences among the different diagnoses might be due to a lack of power for this analysis.
Recent studies have reported a negative correlation between movement intensity during ADL in COPD patients in the self-care domain and the total LCADL score.( 17 ) The reported results suggest that lower movement intensity during ADL translates to a higher total score on the LCADL scale, indicating greater functional impairment in ADL. When we evaluated the association between the 6MWW and the LCADL scores, we also found it to be significant. One group of authors( 13 ) proposed that functional performance during exercise would be better expressed by the product of 6MWD and body weight than by the analysis of 6MWD alone, because subjects perform specific work when walking, given that they transport their own body over a given distance over a given time.
In the present study, the LCADL scale was found to have high internal consistency (alpha), with the overall alpha value being 0.90 and the alpha values for each domain ranging from 0.72 to 0.94. Previous studies have demonstrated that the LCADL scale has high internal consistency when administered to COPD patients. One study( 18 ) reported an alpha value of 0.98, which demonstrates that the LCADL scale is a valid measure of dyspnea during ADL. Another study( 10 ) showed that the Brazilian Portuguese-language version of the LCADL scale is reproducible, having an alpha value of 0.86.
In the present study, 69% of the patients in the sample achieved a total LCADL score (expressed as a percentage) above 50%, i.e., they showed severe dyspnea-related limitation in their ADL. A recent study has suggested the use of a cut-off point of 50%, with a score equal to or greater than 50% indicating severe dyspnea-related limitation in ADL.( 19 ) In addition, we should take into account that most of the study sample reported that dyspnea significantly affects their ADL, which leads us to believe that dyspnea can impose major restrictions on these patients. The presence of dyspnea has been considered a severe limitation to physical and social activities, having a direct impact on the quality of life of patients with chronic obstructive or restrictive respiratory disease and leading to a marked increase in morbidity and mortality.( 20 )
In the univariate analysis, the modified Borg scale score (dyspnea) showed no significant association with the total LCADL score (expressed as a percentage). This finding might be associated with the fact that the Borg scale has poor reproducibility, which has been reported in other studies, given the difficulty that patients have in classifying their level of dyspnea because of desensitization.( 21 ) In this sense, the LCADL scale can be a useful and user-friendly tool for assessing patients on the waiting list for lung transplantation, especially those experiencing significant impairment in ADL, in whom dyspnea is an incapacitating symptom, even for routine activities.( 7 , 18 )
The FEV1 was not significantly associated with the total LCADL score (expressed as a percentage). One explanation for this finding is that, although FEV1 provides a useful description of the severity of the disease-related pulmonary changes, it does not systematically assess the impact that the disease has on the patients' ability to perform their ADL because of dyspnea.( 18 , 22 )
Age also showed no association with the LCADL scale results. These findings can be attributed to the fact that functional classification scales are more strongly related to patient symptoms and clinical status, neither of which are directly related to age.( 19 , 23 ) One explanation for the lack of association between the LCADL scale results and patient age in the present study is the fact that the sample did not include older patients. One group of authors( 24 ) found a strong negative correlation between age and functional capacity, which is evidence that physical aspects are more impaired by advancing age than are mental aspects.
One limitation of the present study is the small sample size. However, despite the limited number of patients, it was possible to determine that the LCADL scale behaves appropriately with regard to psychometric properties, as well as being strongly associated with the 6MWD and the 6MWW, which are objective measures.
In conclusion, the LCADL scale proved to have instrumental reliability, as well as being correlated with conventional objective measures of the level of physical activity. The fact that the LCADL scale performed well in patients on the waiting list for lung transplantation suggests that this instrument can be a valid and feasible tool to assess dyspnea during ADL.
Footnotes
Financial support: None
Study carried out in the Department of Physical Therapy, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, Brazil.
Contributor Information
Jocimar Prates Muller, Vale do Rio dos Sinos University, São Leopoldo, Brazil, Coordinator. Department of Physical Therapy, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, Brazil. Universidade do Vale do Rio dos Sinos – UNISINOS, Vale do Rio dos Sinos University – São Leopoldo, Brazil.
Patrícia Ayres Guterres Gonçalves, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Department of Physical Therapy, Porto Alegre, Brazil. Department of Physical Therapy, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, Brazil.
Fabrício Farias da Fontoura, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, Brazil. Pulmonary Rehabilitation Program, Pereira Filho Ward, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, Brazil.
Rita Mattiello, Pontifical Catholic University of Rio Grande do Sul, Biomedical Research Institute, Porto Alegre, Brazil. Biomedical Research Institute, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil.
Juliessa Florian, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, Brazil. Pulmonary Rehabilitation Program, Pereira Filho Ward, Complexo Hospitalar Santa Casa de Misericórdia de Porto Alegre, Porto Alegre, Brazil.
References
- 1.Wehrmeister FC, Knorst M, Jardim JR, Macedo EC, Noal RB, Martínez-Mesa J, et al. Pulmonary rehabilitation programs for patients with COPD. J Bras Pneumol. 2011;37(4):544–555. doi: 10.1590/s1806-37132011000400017. http://dx.doi.org/10.1590/S1806-37132011000400017 [DOI] [PubMed] [Google Scholar]
- 2.Garcia-Aymerich J, Serra Pons I, Mannino DM, Maas AK, Miller DP, Davis KJ. Lung function impairment, COPD hospitalisations and subsequent mortality. Thorax. 2011;66(7):585–590. doi: 10.1136/thx.2010.152876. http://dx.doi.org/10.1136/thx.2010.152876 [DOI] [PubMed] [Google Scholar]
- 3.Ahmad S, Shlobin OA, Nathan SD. Pulmonary complications of lung transplantation. Chest. 2011;139(2):402–411. doi: 10.1378/chest.10-1048. http://dx.doi.org/10.1378/chest.10-1048 [DOI] [PubMed] [Google Scholar]
- 4.Cardoso PF. New perspectives in lung transplantation: from conventional preservation to ex vivo lung perfusion and lung reconditioning. J Bras Pneumol. 2009;35(11):1057–1059. doi: 10.1590/s1806-37132009001100001. [DOI] [PubMed] [Google Scholar]
- 5.Rogers D, Prasad SA, Doull I. Exercise testing in children with cystic fibrosis. J R Soc Med. 2003;96(Suppl 43):23–29. [PMC free article] [PubMed] [Google Scholar]
- 6.Pitta F, Troosters T, Spruit MA, Probst VS, Decramer M, Gosselink R. Characteristics of physical activities in daily life in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2005;171(9):972–977. doi: 10.1164/rccm.200407-855OC. http://dx.doi.org/10.1164/rccm.200407-855OC [DOI] [PubMed] [Google Scholar]
- 7.Bausewein C, Farquhar M, Booth S, Gysels M, Higginson IJ. Measurement of breathlessness in advanced disease: a systematic review. Respir Med. 2007;101(3):399–410. doi: 10.1016/j.rmed.2006.07.003. http://dx.doi.org/10.1016/j.rmed.2006.07.003 [DOI] [PubMed] [Google Scholar]
- 8.Carpes MF, Mayer AF, Simon KM, Jardim JR, Garrod R. The Brazilian Portuguese version of the London Chest Activity of Daily Living scale for use in patients with chronic obstructive pulmonary disease. J Bras Pneumol. 2008;34((3):143–151. doi: 10.1590/s1806-37132008000300004. http://dx.doi.org/10.1590/S1806-37132008000300004 [DOI] [PubMed] [Google Scholar]
- 9.Vilaró J, Gimeno E, Sánchez Férez N, Hernando C, Díaz I, Ferrerc M, et al. Daily living activity in chronic obstructive pulmonary disease: validation of the Spanish version and comparative analysis of 2 questionnaires [Article in Spanish] Med Clin (Barc) 2007;129(9):326–332. doi: 10.1157/13109543. http://dx.doi.org/10.1157/13109543 [DOI] [PubMed] [Google Scholar]
- 10.Pitta F, Probst VS, Kovelis D, Segretti NO, Mt Leoni A, Garrod R, et al. Validation of the Portuguese version of the London Chest Activity of Daily Living Scale (LCADL) in chronic obstructive pulmonary disease patients. Rev Port Pneumol. 2008;14(1):27–47. [PubMed] [Google Scholar]
- 11.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 12.Enright PL, Sherrill DL. Reference equations for the six-minute walk in healthy adults. Pt 1Am J Respir Crit Care Med. 1998;158(5):1384–1387. doi: 10.1164/ajrccm.158.5.9710086. [DOI] [PubMed] [Google Scholar]
- 13.Teixeira PJ, Costa CC, Berton DC, Versa G, Bertoletti O, Canterle DB. O trabalho de caminhada dos seis minutos não se correlaciona com o grau de obstrução do fluxo aéreo em doentes portadores de Doença Pulmonar Obstrutiva Crónica (DPOC) Rev Port Pneumol. 2006;12(3):241–253. [PubMed] [Google Scholar]
- 14.Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. General considerations for lung function testing. Eur Respir J. 2005;26(1):153–161. doi: 10.1183/09031936.05.00034505. http://dx.doi.org/10.1183/09031936.05.00034505 [DOI] [PubMed] [Google Scholar]
- 15.Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal maximal expiratory flow-volume curve with growth and aging. Am Rev Respir Dis. 1983;127(6):725–734. doi: 10.1164/arrd.1983.127.6.725. [DOI] [PubMed] [Google Scholar]
- 16.Streiner DL, Norman GR, editors. Health Measurement Scales. New York: Oxford University Press; 2003. [Google Scholar]
- 17.Hernandes NA, Teixeira Dde C, Probst VS, Brunetto AF, Ramos EM, Pitta F. Profile of the level of physical activity in the daily lives of patients with COPD in Brazil. J Bras Pneumol. 2009;35(10):949–956. doi: 10.1590/s1806-37132009001000002. [DOI] [PubMed] [Google Scholar]
- 18.Garrod R, Bestall JC, Paul EA, Wedzicha JA, Jones PW. Development and validation of a standardized measure of activity of daily living in patients with severe COPD: the London Chest Activity of Daily Living scale (LCADL) Respir Med. 2000;94(6):589–596. doi: 10.1053/rmed.2000.0786. http://dx.doi.org/10.1053/rmed.2000.0786 [DOI] [PubMed] [Google Scholar]
- 19.Simon KM. Atividade de vida diária e índice de mortalidade "BODE" em indivíduos portadores de doença pulmonar obstrutiva crônica [dissertation] Uberlândia: Centro Universitário do Triângulo; 2006. [Google Scholar]
- 20.Martinez JA, Pádua AI, Terra J., Filho Dispnéia. Medicina (Ribeirão Preto) 2004;37:199–207. [Google Scholar]
- 21.Velloso M, Costa CP, Ozeki CM. Métodos de mensuração da dispnéia: uma revisão da literatura. Conscientiae Saúde. 2002;1:35–39. http://dx.doi.org/10.5585/conssaude.v1i0.166 [Google Scholar]
- 22.American Thoracic Society Pulmonary rehabilitation-1999. Pt 1Am J Respir Crit Care Med. 1999;159(5):1666–1682. doi: 10.1164/ajrccm.159.5.ats2-99. [DOI] [PubMed] [Google Scholar]
- 23.Cunha TM, Cota RM, Souza BK, Oliveira BG, Ribeiro AL, Sousa LA. Correlação entre classe funcional e qualidade de vida em usuários de marcapasso cardíaco. Rev Bras Fisioter. 2007;11(5):341–345. http://dx.doi.org/10.1590/S1413-35552007000500003 [Google Scholar]
- 24.Santos PR. Relação do sexo e da idade com nível de qualidade de vida em renais crônicos hemodialisados. Rev Assoc Med Bras. 2006;52(5):356–392. doi: 10.1590/s0104-42302006000500026. http://dx.doi.org/10.1590/S0104-42302006000500026 [DOI] [PubMed] [Google Scholar]


