Abstract
Under normal conditions, food intake and energy expenditure are balanced by a homeostatic system that maintains stability of body fat content over time. However, this homeostatic system can be overridden by the activation of ‘emergency response circuits’ that mediate feeding responses to emergent or stressful stimuli. Inhibition of these circuits is therefore permissive for normal energy homeostasis to occur, and their chronic activation can cause profound, even life-threatening, changes in body fat mass. This Review highlights how the interplay between homeostatic and emergency feeding circuits influences the biologically defended level of body weight under physiological and pathophysiological conditions.
Whether to eat, what to eat, when to eat and how much to eat in any one meal are decisions that each of us is intimately familiar with and that we are capable of making with little conscious effort. As these decisions can be influenced by a nearly limitless number of variables, day-to-day energy intake tends to vary both between and within individuals1. However, in normal individuals, body weight and body fat content are typically quite stable over time2,3 owing to a biological process termed ‘energy homeostasis’ that matches energy intake to expenditure over long periods of time. The energy homeostasis system comprises neurons in the mediobasal hypothalamus and other brain areas4 that are a part of a neurocircuit that regulates food intake in response to input from humoral signals that circulate at concentrations proportionate to body fat content4-6.
The robust efficiency with which the energy homeostasis system works in normal-weight humans and animal models seems to be at odds with the very high prevalence of overweight and obesity in Westernized societies7. Also common are disorders characterized by anorexia and progressive loss of body mass (‘wasting illness’) that importantly contribute to the mortality of cancer and other diseases8. Little is known regarding mechanisms underlying these disorders, but recently identified neurocircuits, which are referred to here as ‘emergency feeding circuits’, may play a part. Some of these emergency circuits are designed to increase plasma glucose levels (partly by increased feeding) when they are activated9, whereas others prevent feeding when to do so is maladaptive (for example, under conditions of trauma, illness or threats from the environment)8. A key point is that activation of these emergency circuits can potentially override normal control of energy homeostasis irrespective of whether these circuits function to increase or decrease food intake. The goals of this Review are to describe how food intake is governed by the energy homeostasis system and how it is altered in times of stress, and to consider how pathological activation of emergency response circuits can cause disorders of body weight.
The energy homeostasis system
First proposed by Kennedy10 some 60 years ago, energy homeostasis is achieved by a system whereby circulating signals inform the brain of available energy stores (a process referred to as ‘adiposity negative feedback’) and, in response, the brain makes corrective adjustments to food intake. (The energy homeostasis system also regulates energy expenditure, a topic that has recently been reviewed in REFS 11,12.) The best-studied humoral mediator of adiposity negative feedback is the adipocyte hormone leptin. Leptin is secreted from adipose tissue13, circulates in proportion to body fat stores14, enters the brain in proportion to its plasma level15 and acts on key neurons that regulate energy balance16,17. Moreover, leptin administration directly into the brain reduces food intake and body weight18,19, although conversely, reduced or impaired neuronal leptin signalling promotes hyperphagia and weight gain13,20.
The pancreatic hormone insulin is also implicated in energy homeostasis. Like leptin, insulin circulates in proportion to body fat21 and acts in the brain to reduce food intake22; conversely, reduced neuronal insulin signalling causes a mild expansion of body fat mass23. Although both hormones are implicated in this adiposity negative feedback control system, the feeding effect of leptin is quantitatively much greater than that of insulin.
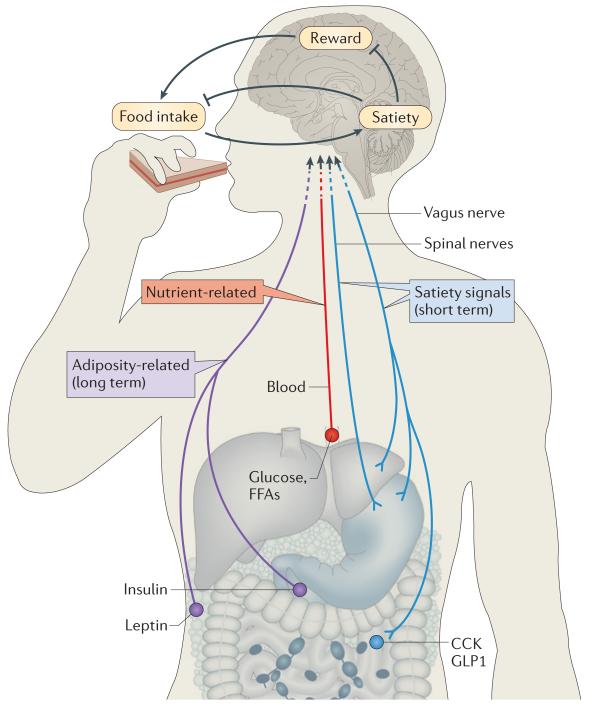
Beyond adiposity negative feedback signals, numerous hormonal and nutrient-related signals can potently influence feeding. Among these are gut peptides that are involved in the perception of satiety and hence participate in the termination of individual meals. Putative satiety signals include peptide YY3-36 (PYY3-36)24, glucagon-like peptide 1 (GLP1)25 and cholecystokinin (CCK)26. The gastric hormone ghrelin27, conversely, is secreted before meal onset and can stimulate feeding. Food intake can also be inhibited by other endogenous mediators, including pro-inflammatory cytokines (such as interleukin-6 and tumour necrosis factor-α) and nutrients themselves (for example, glucose and free fatty acids28) (FIG. 1).
Figure 1. CNS regulation of energy homeostasis.
The CNS integrates input from long-term energy stores (for example, leptin) and short-term meal-related signals (nutrients and gut-derived satiety signals) to regulate food intake and energy expenditure in a manner that maintains stable body fat stores over time. Positive energy balance induced by overfeeding inhibits the rewarding properties of food while enhancing meal-induced satiety, thereby reducing food intake. In response to energy deprivation, CNS adaptive responses are engaged that both increase the rewarding properties of food and reduce the response to satiety signals, collectively resulting in increased food consumption until deficient fat stores are replenished. CCK, cholecystokinin; FFAs, free fatty acids; GLP1, glucagon-like peptide 1. Modified from Marx, J. Cellular warriors at the battle of the bulge. Science 299, 846-849 (2003)170. Reprinted with permission from AAAS.
Satiety perception
Whereas the decision to eat (meal initiation) is influenced by many external factors, the amount eaten (meal size) is primarily determined by internal signals. Among the most important internal signals are peptides such as CCK and GLP1 that are secreted from the gastrointestinal tract in response to food ingestion26,29. Satiety information is conveyed by these peptides, as well as by neural signals generated by gastric distension, to the CNS through afferent fibres of the vagus nerve that project from the gut to the nucleus of the solitary tract (NTS) in the caudal hindbrain. Satiety peptides trigger food intake inhibition that is profound but short-lived, and they do not reliably cause sustained weight loss with repeated dosing. Illustrating this point is a study in rats in which serial injections of CCK were administered at the onset of each meal over a period of days30. Although CCK consistently decreased meal size, its impact on body weight was minimal because of a compensatory increase in meal frequency, such that the total amount of calories consumed was not substantially affected30.
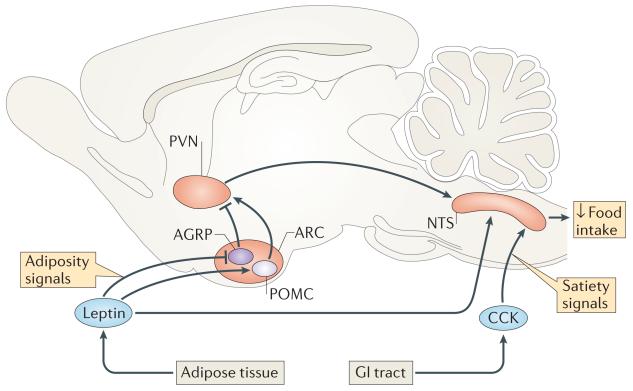
Buried within this observation is a fundamental axiom regarding how the energy homeostasis system works: adiposity negative feedback reduces food intake in part by increasing brain responsiveness to satiety signals31, an effect that is mediated by neuronal input from leptin and insulin32,33. Weight loss lowers the plasma levels of these hormones, which reduces the satiating effect of food (by reducing the response to satiety signals) and thereby increases meal size. Consistent with this concept is evidence that leptin reduces food intake by enhancing the response to satiety signals32,34,35 and thereby decreases meal size36,37, whereas deficient brain leptin signalling reduces the responsiveness to CCK, which leads to an increase in meal size31,38,39. This interaction between leptin and satiety signals seems to involve the activation of leptin receptors in both the hindbrain (on NTS neurons themselves40) and the forebrain (on neurons in the hypothalamic arcuate nucleus (ARC) that project directly or indirectly to the NTS41). The key point is that this interaction enables the amount of food consumed during individual meals to be adjusted to compensate for changes in body fat mass35,42 (FIG. 2).
Figure 2. Integration of long-term homeostatic and short-term satiety signals.
A model describing homeostatic control of body adiposity proposes that regulation of food intake on a meal-to-meal basis is adjusted in response to changes in body fat content. Through actions in both the forebrain and hindbrain, the adiposity negative feedback signal leptin enhances responsiveness to gut-derived satiety signals such as cholecystokinin (CCK), which are released upon food ingestion. In addition to direct effects on hindbrain areas such as the nucleus of the solitary tract (NTS), leptin stimulates pro-opiomelanocortin (POMC) neurons but inhibits neurons that express agouti-related protein (AGRP) and neuropeptide Y (labelled as just AGRP) in the hypothalamic arcuate nucleus (ARC). These neurons project to second-order neurons in adjacent hypothalamic nuclei, including the paraventricular nucleus (PVN) and lateral hypothalamic area (not shown), which, in turn, project to the NTS, where satiety signals are processed. Satiety signals activate vagal afferents that terminate in the NTS to promote the termination of a meal. The NTS response to the satiety response is amplified both by direct input to the NTS from leptin and indirectly through the action of leptin in the hypothalamus. Consequently, reduced leptin action (for example, following weight loss) increases meal size by reducing the hindbrain response to satiety signals. GI, gastrointestinal. Figure from REF. 4, Nature Publishing Group.
Food reward
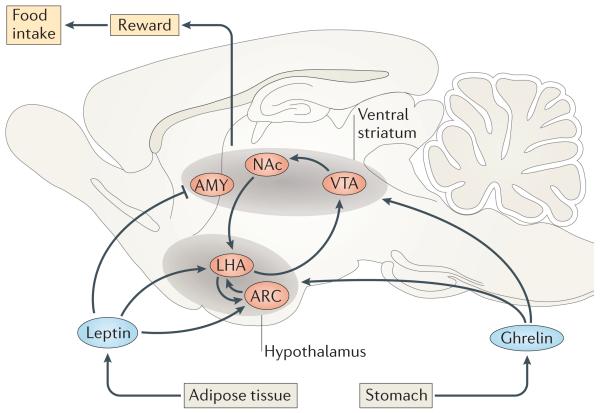
That palatability is a crucial determinant of the decision to eat, and that highly palatable foods can trigger eating at times when food would not otherwise be consumed, comes as no surprise. This type of feeding has been described as ‘non-homeostatic’ (REF. 43), because it can occur in the absence of the need to replenish depleted fuel stores. However, we disagree with this characterization because regulation of food reward is in fact integral to how energy homeostasis is achieved44. First, reduced perception of food reward seems to be an inherent aspect of satiety, a concept that has recently been developed based on findings from rodent studies45 and that is supported by brain imaging studies in humans46,47. Second, a fasting-induced increase in food intake (‘re-feeding hyperphagia’) is associated with an increase in both the amount of work an animal will do to obtain food (a measure of the motivation to eat) and the ability of food to condition place preference (a measure of learning driven by food’s reinforcing properties), and both of these responses are blunted by intracerebroventricular administration of leptin or insulin48,49. Stated more simply, weight loss induced by fasting or caloric restriction stimulates a compensatory hyperphagia in part by increasing the rewarding properties of food, and this effect is mediated by reduced neuronal input from adiposity negative feedback signals. Clinical evidence in support of this assertion includes the finding that leptin administration reduces food intake in humans with congenital leptin deficiency. This effect is associated with decreases not only in the subjective experience of food reward but also in the activation of brain areas that are associated with reward (that is, the ventral striatum) in response to food-related stimuli50 (FIG. 3).
Figure 3. Integration of homeostatic and reward-related inputs.
Homeostatic signals modulate the perception of food reward (for example, the hedonic value and the motivation to work for food). Mesolimbic dopaminergic neurons in the ventral tegmental area (VTA) project to the nucleus accumbens (NAc) and other brain areas to heighten the reward value of palatable food. Neurons in the lateral hypothalamic area (LHA) integrate reward-related input from the NAc with information related to energy homeostasis from arcuate nucleus (ARC) neurons. In turn, LHA neurons project to and influence the mesolimbic dopaminergic system while also influencing satiety perception through projections to the hindbrain (not shown). Weight loss lowers plasma insulin and leptin levels while increasing plasma ghrelin levels. Working in concert, these responses increase the rewarding properties of food and hence the motivation to eat through either direct effects in the ventral striatum or indirect effects in the hypothalamus through the LHA. Conversely, following periods of positive energy balance, body weight is returned to its biologically defended level through both a decrease in the rewarding properties of food and an increased response to input from satiety signals. AMY, amygdala.
The homeostatic regulation of food reward is the subject of recent reviews51,52. Briefly, brain reward circuits that process information related to food reward (for example, the hedonic value of and motivation to work for food) are influenced by metabolic and hormonal signals that communicate information regarding the status of energy stores to the CNS. These reward circuits include mesolimbic dopaminergic neurons in the ventral tegmental area (VTA) that project to the nucleus accumbens (NAc) and other forebrain areas53. With its supply of fibres from hypothalamic areas such as the ARC, as well as from reward-processing areas such as the NAc, the lateral hypothalamic area (LHA) is proposed to integrate reward-related input with information related to energy homeostasis53. In turn, LHA neurons project to and influence the mesolimbic dopamine system54 as well as hindbrain areas such as the NTS that regulate satiety. To summarize, the energy homeostasis system functions through powerful and coordinated influences over the perception of satiety on the one hand and of food reward on the other.
Energy homeostasis neurocircuitry
Our understanding of the neurocircuitry of energy homeostasis has rapidly grown over the past decade. Among the most-studied and best-understood neuronal subpopulations are those that co-express neuropeptide Y (NPY), agouti-related protein (AGRP; an antagonist of melanocortin signalling) and GABA16,55; these neurons are henceforth referred to as AGRP neurons. AGRP neurons are situated in the ARC and they stimulate feeding when they are activated56. Consistent with a role in energy homeostasis, AGRP neurons are inhibited by both insulin and leptin57-59, whereas they are activated by ghrelin60. In leptin-deficient ob/ob mice, these neurons are strongly activated, and this effect has been functionally linked to the pronounced hyperphagia in these mice55,61.
Adjacent to AGRP cells in the ARC are neurons that express pro-opiomelanocortin (POMC) and release α-melanocyte stimulating hormone (α-MSH), which inhibits food intake by binding to and activating neuronal melanocortin receptors. Unlike AGRP neurons, POMC neurons are stimulated by leptin62,63 and they are inhibited in leptin-deficient states62. However, caution is warranted when generalizing the role of POMC neurons, as several distinct subsets have been reported, some of which are leptin-responsive64, whereas others are responsive to insulin. Surprisingly, whereas leptin depolarizes and increases firing of POMC cells, insulin has the opposite effect64. Nevertheless, insulin and leptin activate overlapping signal transduction and transcriptional cascades in POMC neurons65, and the functional significance of the effects of these hormones on membrane potential is unknown. Still other POMC neuronal subsets are activated by ascending serotonergic input66 or by glutamatergic neurons located in the ventromedial hypothalamic nucleus (VMN)67, whereas they are inhibited by GABAergic input from AGRP neurons57.
Weight loss activates AGRP neurons, which inhibits POMC neurons, and these effects are triggered at least in part by reduced leptin signalling. It is therefore somewhat surprising that only a mild obesity phenotype results when leptin receptors are deleted from both POMC and AGRP neurons67-69, whereas pan-hypothalamic leptin receptor deletion recapitulates the severe obesity and hyperphagia phenotype of mice lacking leptin receptors altogether70. These and other observations support the hypothesis that although leptin can act directly on leptin receptors expressed by POMC and AGRP neurons, these neurons can also be regulated through indirect effects mediated by leptin-responsive neurons that are situated upstream.
Although ARC neurons remain a major research focus, leptin clearly influences energy balance through effects in other brain areas both within the hypothalamus (for example, the VMN71) and outside the hypothalamus (for example, the VTA72,73 and NTS40,74). With respect to neuronal subtypes that are important in leptin action, a role has been suggested for hypothalamic GABAergic neurons (which are typically detected by the expression of the vesicular GABA transporter (also known as vesicular inhibitory amino acid transporter)). Deletion of leptin receptors from GABAergic neurons causes a much more pronounced obesity phenotype75 than that induced by leptin receptor deletion from AGRP and/or POMC cells69,76. A caveat to these observations is that GABAergic neurons constitute a majority of hypothalamic leptin-responsive cell types (including, for example, AGRP neurons), and hence leptin receptor deletion from these cells has a greater effect than that which would be expected in a more select neuronal subpopulation. In this context, it is of interest that some GABAergic neurons also synthesize nitric oxide, and leptin receptor deletion from neurons that express neuronal nitric oxide synthase (nNOS) causes severe hyperphagia and obesity77. These leptin-responsive GABAergic neurons are found in both the ARC and dorsomedial nucleus (DMN), and in response to leptin, they are hypothesized to inhibit downstream neurocircuits that are ‘hardwired’ to drive feeding (perhaps including AGRP neurons).
Recent observations point to an important and specific role for GABA originating in AGRP neurons in the control of feeding behaviour. Deletion of GABA signalling (by deletion of the vesicular GABA transporter) from AGRP neurons results in mice characterized by a lean phenotype that are resistant to diet-induced obesity (DIO)78. Perhaps more importantly, GABAergic projections from AGRP neurons tonically inhibit a subset of neurons in the parabrachial nucleus (PBN) that, when activated, trigger profound anorexia79,80. These PBN neurons, discussed in greater detail below, are marked by expression of calcitonin and calcitonin gene-related peptide (CGRP), and their activation after the ablation of AGRP neurons induces potentially fatal anorexia in mice81.
Identification of neural circuits for feeding
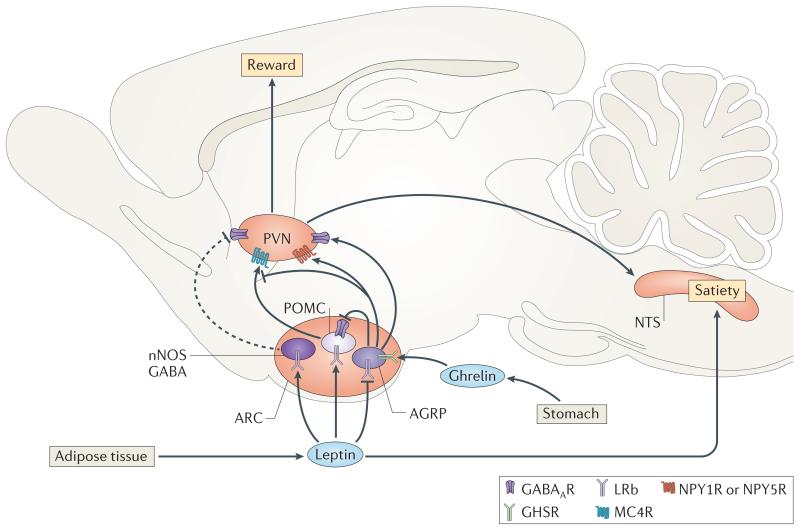
The combination of mouse genetics with optogenetics or DREADD (designer receptor exclusively activated by a designer drug) technology has enabled investigation into the feeding effects induced by activating or inhibiting defined neuronal subsets in live, conscious adult mice82,83. For example, studies using optogenetic as well as pharmacogenetic (DREADD-mediated) strategies show that AGRP neuron activation is sufficient to rapidly and potently stimulate feeding84-86. Moreover, this voracious feeding response occurs irrespective of nutritional state (that is, in well-fed mice), time of day and without training, and instead primarily depends on the level of AGRP neuron activity84. Activation of these neurons also increases both the motivation to work for food (as assessed by a progressive ratio test or lever pressing) and food-seeking behaviour86, whereas selective inhibition of AGRP neurons reduces feeding84. Thus, hyperphagia associated with reduced leptin signalling (for example, in ob/ob or db/db mice, fasting and uncontrolled insulin-deficient diabetes mellitus (uDM))87-89 probably involves activation of AGRP neurons (FIG. 4).
Figure 4. Neurocircuits involved in the homeostatic regulation of feeding.
Neurons in the hypothalamic arcuate nucleus (ARC) and nucleus of the solitary tract (NTS) sense and respond to peripheral energy signals to promote energy homeostasis. Neuropeptides such as neuropeptide Y (NPY) and neurotransmitters such as GABA, among others, are released onto downstream neurons including those in the paraventricular nucleus (PVN). In the PVN, oxytocin and other neurons tonically inhibit feeding and, during energy deficit, are inhibited by orexigenic input from the ARC, thereby stimulating feeding. The same agouti-related protein (AGRP) neurons (which co-express GABA and NPY) that are involved in short-term feeding also contribute to long-term energy balance through the release of AGRP, an inverse agonist of melanocortin receptor 4 (MC4R) and, through GABA release, inhibit neighbouring pro-opiomelanocortin (POMC) neurons. POMC neurons are stimulated by input from leptin, and the release of α-melanocyte stimulating hormone (α-MSH) activates MC4R, thereby inhibiting food intake. In addition, recent evidence also implicates leptin-responsive GABAergic neurons that express neuronal nitric oxide synthase (nNOS) in the regulation of energy homeostasis. These neurons are found in the ARC and dorsomedial nucleus (not shown) and are hypothesized (dashed line) to inhibit downstream neurocircuits that drive feeding. Collectively, this input is relayed to the PVN and lateral hypothalamic area (not shown) and integrated to modulate the rewarding properties of food and the response to satiety signals. GABAAR, type A GABA receptor; GHSR, growth hormone secretagogue receptor (ghrelin receptor); LRb, leptin receptor; NPY1R, NPY receptor type 1.
Recent research has shed light on the respective roles of the three mediators contained within AGRP neurons: AGRP, NPY and GABA. Using DREADD technology in three different mouse models, Lowell and colleagues tested the individual contributions made by GABA, NPY or AGRP to feeding induced by AGRP neuron activation90. They found that the presence of either GABA or NPY is sufficient to rapidly stimulate feeding upon AGRP neuron activation. Although AGRP release alone failed to increase food intake in the short term, it did so effectively over a longer time interval90. Although the time course of their effects can differ, release of any of the three mediators contained within AGRP neurons is sufficient to comparably and potently stimulate feeding.
Although stimulation and inhibition of POMC neurons using either optogenetics or DREADDs in mice reduces and increases food intake, respectively84,85, these effects do not occur rapidly. Thus, POMC cells may primarily participate in long-term rather than short-term control of feeding84,85. This observation fits with the delayed onset of feeding induced by local release of AGRP alone90, as AGRP acts by inhibiting neuronal melanocortin receptors. The observation also implies that the inhibition of POMC neurons by AGRP neuron activation (through type A GABA (GABAA) receptors)57 does not explain the associated acute stimulation of food intake.
Studies to identify a ‘feeding circuit’ activated by AGRP neurons have thus far focused on the hypothalamic paraventricular nucleus (PVN) on the basis of evidence that photoactivation of AGRP axons in this brain area mimics the feeding effect of activating AGRP neurons in the ARC85. The relevant PVN neurons (which are characterized by the expression of single-minded homologue 1 (SIM1)) seem to be inhibited by input from AGRP neurons, as activation of these PVN neurons reduces food intake and reverses the hyperphagic effect of AGRP neuron activation, including effects on both food seeking and willingness to work for food85. Conversely, electrolytic lesioning of the PVN (like AGRP neuron activation) has long been known to induce hyperphagic obesity91.
Melanocortin receptor 4 (MC4R) mediates many of the feeding effects of both AGRP and POMC neurons. The importance of this receptor in energy homeostasis was first established by the obese phenotype of MC4R-knockout mice92. Subsequent studies found that MC4R mutation is the most common cause of monogenic obesity in humans93,94, accounting for up to 6% of early-onset or severe adult obesity cases95. The PVN has been implicated as a key site for the inhibitory effect of MC4R signalling on food intake, as MC4Rs are abundantly expressed in this brain area96, the PVN is heavily innervated by both AGRP and POMC neurons97and food intake is reduced by administration of MC4R agonists directly into the PVN98. Furthermore, re-expression of MC4Rs in SIM1 (that is, PVN) neurons rescues hyperphagia in MC4R-null mice99, whereas regulation of energy expenditure by MC4R is mediated by sympathetic preganglionic neurons100.
Among several distinct subsets of PVN neurons that are likely to participate in the control of food intake are those that express oxytocin and seem to be components of the pathway activated by leptin. Following either systemic or central administration, oxytocin reduces food intake and body weight in obese as well as lean animals101-104. This effect is mediated in part by projections to the NTS, where oxytocin release seems to enhance the hindbrain response to gut-derived satiety signals such as CCK, leading to the consumption of smaller meals105. In support of this concept, leptin-responsive oxytocin neurons in the PVN project to the NTS, and leptin-induced anorexia requires oxytocin signalling106,107. Conversely, mice108 or humans109-111 with genetic disruptions in SIM1 as well as individuals with Prader–Willi syndrome112 are characterized both by the loss of PVN oxytocin neurons and by severe hyperphagia and obesity. This PVN–NTS oxytocin circuit therefore exemplifies how leptin-responsive hypothalamic neurons can inhibit feeding by enhancing the hindbrain response to satiety signals, although (as noted above) leptin can also reduce meal size through direct effects in the NTS40. Moreover, mice lacking either oxytocin113 or its receptor114 exhibit only a modest, late-onset obesity phenotype, and oxytocin neuron activation does not reduce food intake after a fast85. Thus, the importance of oxytocin neurons in energy homeostasis and obesity pathogenesis awaits further study.
Emergency circuits that stimulate feeding
An emerging concept in the neurobiology of food intake is that neurocircuits exist that are normally inhibited, but when activated in response to emergent or stressful stimuli they can override the homeostatic control of energy balance. Understanding how these circuits interact with the energy homeostasis system is fundamental to understanding the control of food intake and may bear on the pathogenesis of disorders at both ends of the body weight spectrum.
Hypoglycaemia
Although reduced food intake accompanies most stressful stimuli, inadequate delivery of glucose to the brain, termed ‘neuroglucopenia’ (also known as ‘glucoprivation’), is an exception. The response to hypoglycaemia exemplifies how the emergency created by neuroglucopenia activates neurocircuits that drive feeding along with wide-ranging neuroendocrine and autonomic ‘counter-regulatory’ responses that together function to raise blood glucose levels9,115. Components of the response include: suppression of insulin secretion; secretion of counter-regulatory hormones such as glucagon and adrenaline that function in a coordinated manner with the activation of the hypothalamus–pituitary-adrenal (HPA) axis; and increased sympathetic nervous system outflow to liver, islet and adrenal tissue. The net effect of these responses is to raise serum glucose levels by stimulating glucose production while inhibiting glucose uptake in peripheral tissues115-118 (BOX 1).
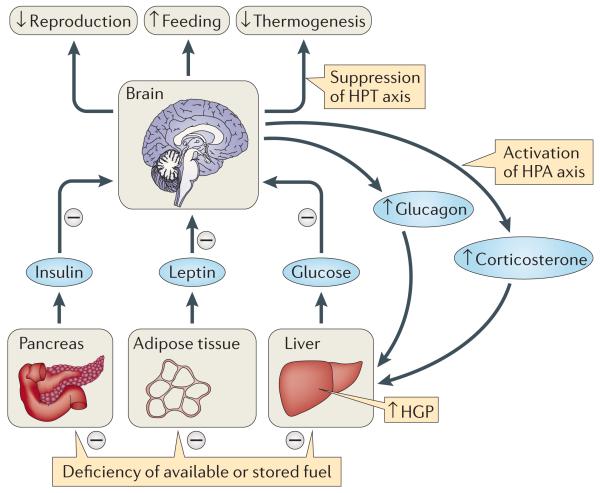
Box 1. Behavioural, autonomic and neuroendocrine responses to current or pending energy deficiency.
In response to conditions of either acute energy deficiency (for example, hypoglycaemia) or chronic energy deficiency (for example, leptin deficiency), the brain initiates a shared set of behavioural, autonomic and neuroendocrine responses that are designed to increase the availability of fuel to the CNS while also conserving fuel stores. Among the responses are increases in both feeding and hepatic glucose production (HGP), with the latter effect mediated in part by increased plasma levels of glucagon and corticosterone (through activation of the hypothalamus–pituitary–adrenal (HPA) axis). At the same time, the body conserves energy by inhibiting energy-expensive processes such as growth and reproduction while reducing metabolic rate through the suppression of the hypothalamus–pituitary–thyroid (HPT) axis. These various responses are elicited by both hypoglycaemia and uncontrolled insulin-deficient diabetes mellitus (uDM) despite the fact that blood glucose levels are low in the former and high in the latter. Thus, one cause of hyperglycaemia in uDM is the pathological activation of the same responses that are also observed in hypoglycaemia, presumably in response to deficient leptin input to the brain.
Consistent with this hypothesis, central leptin infusion restores euglycaemia in rats and mice with uDM135-138. Similarly, the behavioural, autonomic and neuroendocrine responses that are observed in hypoglycaemia and uDM are also elicited in other leptin-deficient conditions (for example, fasting and in ob/ob mice); again, these responses are ameliorated by administering leptin directly into the brain61,133. Thus, conditions associated with central leptin deficiency are characterized by both hyperphagia and raised HGP, presumably reflecting activation of some of the same neurocircuits that are involved in the counter-regulatory response to neuroglucopenia.
In summary, the CNS monitors signals that are pertinent to both immediately available fuel (for example, glucose) and the status of fuel stores (for example, leptin), with deficiency of either hypothesized to activate the same neurocircuitry. The result is a potent increase in both feeding and HGP until blood glucose (and leptin) levels have risen sufficiently to turn off the response.
Information regarding glucose availability is conveyed to the brain from multiple sources, including the hepatic portal vein and glucose-sensing neurons in both the hindbrain119 and forebrain120, including the hypothalamus. Glucose-responsive neurons can either increase or decrease their firing rate as local glucose concentrations rise, with the former termed ‘glucose-excited’ and the latter referred to as ‘glucose-inhibited’ neurons121. These glucose-sensing neurons then project to integrative centres that are located in the hindbrain and the hypothalamus, with VMN neurons being strongly implicated in efferent responses that act to raise plasma glucose levels. Although the neurocircuitry that mediates glucose counter-regulation remains poorly understood, both limbs of the autonomic nervous system are potently activated in an organ-specific manner. Parasympathetic outflow increases through neurons in the dorsal motor nucleus of the vagus that supply pancreatic islets, and sympathetic outflow increases through the intermedio lateral cell column of the spinal cord to stimulate glucose production by the liver and to activate the adrenal medulla while also stimulating pancreatic islets122. Thus, glucopenia-induced glucagon secretion is stimulated by the activation of both parasympathetic and sympathetic neurons supplying the islet.
A potent and sustained increase in food intake also accompanies these responses (termed ‘neuroglucopenic feeding’ (also known as ‘glucoprivic feeding’)), and this increase is so robust that it overrides control exerted by the energy homeostasis system. Stated differently, neuroglucopenia stimulates feeding irrespective of body fuel stores or plasma levels of leptin or insulin123 and, consequently, obesity can result from repeated bouts of neuroglucopenia over a prolonged period. Indeed, the flawed notion that excess insulin is a cause of obesity stems in part from the early observation that pathological weight gain can be induced by repeated administration of insulin at doses sufficient to cause hypoglycaemia124. However, this effect results from neuroglucopenic feeding rather than from insulin itself.
From a teleological perspective, the notion that neuroglucopenic feeding should override the energy homeostasis system is logical in that maintaining stable body fat stores over time is of little use if plasma glucose levels are too low to support brain function. Thus, hyperphagic feeding is sustained until glucopenia has resolved, at which point the energy homeostasis system can re-engage to offset any increase in body fat mass sustained in the process of restoring euglycaemia.
A role for NPY in neuroglucopenic feeding has been suggested, as this response is blunted in NPY-deficient mice125 and ARC NPY-containing neurons (AGRP neurons) are activated by neuroglucopenia126. However, these neurons do not seem to be required for neuroglucopenic feeding127,128, as hypoglycaemia induces hyperphagia in mice even after AGRP neurons have been ablated127. Hindbrain catecholamine neurons that project to the PVN may also drive neuroglucopenic feeding119, as destruction of these neurons selectively blocks this feeding response but leaves fasting-induced feeding responses intact129. These and other findings suggest that neuroglucopenic feeding can be induced by any of several components of a distributed neuronal system, at least some of which are distinct from neurocircuits that drive hyperphagia after a fast.
Diabetic hyperphagia
Type 1 diabetes is a human disease caused by autoimmune destruction of insulin-secreting pancreatic β-cells. In the absence of insulin treatment, profound hyperglycaemia is accompanied by progressive weight loss because insulin deficiency impairs fat storage in adipose tissue. In the absence of insulin therapy, the resultant depletion of body fat causes deficiency of leptin as well as insulin130. Recent experiments in rodent models of uDM, in which hyperglycaemia is induced using the β-cell toxin streptozotocin (STZ), have begun to change our thinking about mechanisms underlying diabetic hyperphagia.
In addition to severe weight loss, hyperglycaemia and ketosis, uDM is accompanied by hyperphagia and many of the same neuroendocrine and autonomic responses that are induced by neuroglucopenia (BOX 1). These responses include increased plasma levels of glucagon, catecholamines and corticosterone that collectively act to increase hepatic glucose production115,131. Moreover, sympathetic outflow to thermogenic brown adipose tissue is reduced in both neuroglucopenia and uDM, and the reproductive, growth and thyroid axes are inhibited in both conditions as well. Therefore, in uDM, hyperglycaemia seems to be driven by many of the same behavioural, autonomic and neuroendocrine responses that are elicited by neuroglucopenia9,132.
Virtually all of these responses are also present in fasting133 and ob/ob mice134, both of which, like uDM, are characterized by leptin deficiency. Together, these observations suggest that the brain response to leptin deficiency recapitulates the response that is induced by hypoglycaemia, a concept that seems paradoxical in that plasma glucose levels are high in both uDM and ob/ob mice and low in fasting and hypoglycaemia. However, this view is consistent with a model in which the CNS response to a deficiency of immediately available fuel (for example, glucose) overlaps with the CNS response to depletion of stored body fuel (as reflected by deficient leptin signalling). That is, the response to a deficiency of currently available fuel involves the same neuro circuits that respond to a pending fuel deficiency; in each case, the response functions to raise blood glucose levels and thereby ensure an adequate supply of fuel to the brain. This concept is consistent with the observation that intracerebroventricular leptin administration ameliorates each of these responses in rats and mice with leptin deficiency induced by STZ-DM135-138, whereas restoring neuronal glucose availability reverses these conditions in neuroglucopenia. These observations support a model in which plasma glucose levels provide the brain with a crucial signal of immediately available fuel, whereas plasma leptin levels signal the amount of stored fuel (in the form of adipose tissue) and that deficiency of either triggers essentially the same brain response. This modification of the ‘selfish brain hypothesis’ (REF. 139) has interesting potential implications for obesity pathogenesis, and these are discussed below.
Implications for obesity pathogenesis
In normal-weight individuals, the energy homeostasis system robustly defends against both weight loss and weight gain140,141. The homeostatic response to weight loss has important clinical implications in that it explains how weight lost by dietary and/or lifestyle intervention tends to be regained over time in obese humans142,143. Conversely, available data from studies in rodents144 as well as humans145,146 show that the energy homeostasis system also protects against pathological weight gain. Specifically, when weight is increased by involuntary (or ‘forced’) overfeeding, a dramatic reduction in caloric intake occurs that is sustained until body weight returns to its pre-intervention level145. From this observation, we infer that obesity does not arise simply from the passive accumulation of excess body fat but rather is a state in which the defended level of body fat has increased141. Indeed, overweight individuals defend their increased body fat stores as robustly as lean individuals145,147-149. Consistent with this view, the main challenge confronting successful obesity treatment is that voluntary weight loss is resisted by homeostatic responses that eventually promote the recovery of lost weight.
One possible explanation for the biological defence of increased body fat mass involves the phenomenon of leptin resistance. This hypothesis has its origin in the observations that leptin levels are increased in obese individuals14 and that the ability of leptin to reduce food intake and body weight is blunted in most obese animals and humans18,150-152. However, leptin resistance is a term that should be used cautiously, as a reduced behavioural or metabolic response to leptin can occur even when the response of cells and tissues to leptin is entirely normal (for example, when the underlying defect lies downstream of neurons that respond directly to leptin). Nevertheless, evidence suggests that in rodent models of DIO, both the ability of leptin to cross the blood-brain barrier and its capacity to activate neuronal leptin receptor signalling are impaired153.
Although the cause of obesity-associated leptin resistance is unknown, inflammation, gliosis and injury affecting hypothalamic neurons may have a role154-158. Inflammation and gliosis are detected in the rat or mouse ARC within the first few days of exposure to a high-fat diet, well before obesity develops159, and these effects could favour weight gain by impairing the response of key neurons to insulin and leptin. In this scenario, input from leptin would need to be increased for ‘normal’ energy homeostasis to occur (for example, maintenance of neutral energy balance and stable body fat mass over time), and expansion of fat stores is the body’s only way to increase plasma leptin levels. Accordingly, body fat mass will increase until input from leptin (combined with other adaptive changes, such as the increased energy cost associated with increased body weight) increases sufficiently to create a new steady state in which body weight is once again stabilized, albeit at a raised level.
Consistent with this hypothesis, experimental activation of hypothalamic inflammatory pathways (such as inhibitor of nuclear factor-κB kinase-(IKKβ)–nuclear factor-κB (NF-κB) signalling) promotes hyperphagia and weight gain, predisposes to DIO and blunts the anorectic effects of insulin and leptin160. Conversely, interventions that reduce hypothalamic inflammation can reduce food intake and body weight, and improve hypothalamic insulin and leptin sensitivity157,160.
A recent study suggests that hypothalamic inflammation induced by high-fat feeding involves neuronal injury — the basis of which remains unknown — which in turn triggers an associated reactive gliosis (the recruitment and activation of microglia and astrocytes)159. In its early stages, this gliosis may be neuroprotective, but with prolonged exposure to a high-fat diet, permanent damage to or loss of neurons involved in energy homeostasis (that is, POMC neurons) can occur159,161. Additional research is needed to assess the causal nature of the relationship between hypothalamic inflammation, gliosis and neuron injury and the pathogenesis of DIO, and to determine whether these responses are reversible and/or can be blocked by therapeutic intervention.
Regardless of the underlying mechanism, reduced neuronal leptin sensitivity seems to trigger adaptive responses that are by and large the same as those induced by neuroglucopenia (BOX 1). The predicted result is not only the biological defence of an increased level of body fat mass among obese, leptin-resistant individuals but also the defence of increased blood glucose levels and an associated impairment in glucose tolerance. Thus, if the brain leptin signal is not effectively transmitted to key hypothalamic neurocircuits, increases in glycaemia as well as food intake will occur until a new steady state is reached, one that is marked by delivery of leptin as well as glucose in amounts sufficient to silence the adaptive response.
The neurobiology of stress-induced anorexia
Reduced food intake is common to many types of stress — whether being chased by a predator, in response to trauma or illness, or following exposure to noxious substances. As the need to maintain body fat stores would seem to be of secondary importance under such circumstances, anorexia effectively overrides control of feeding by the energy homeostasis system. It is as if an ‘off switch’ has been turned on, ensuring that feeding does not occur until the threat has passed.
Palmiter and colleagues81 have recently identified a subset of neurons situated in the PBN that may function as one such off switch for feeding. The PBN is a relay station that receives both visceral and gustatory information and plays a part in protection against the consumption of unfamiliar or potentially toxic substances. In normal rodents, this protection manifests as neophobia (for example, avoidance of a novel taste or food until its post-ingestive consequences are determined) and conditioned taste aversion (CTA)162. Thus, when confronted with a novel-tasting food with no previously known gustatory association, little is consumed until the consequences of doing so are known, and foods that elicit an aversive experience will be avoided in the future. These responses are presumed to have survival value because they protect against the consumption of potentially harmful foods162.
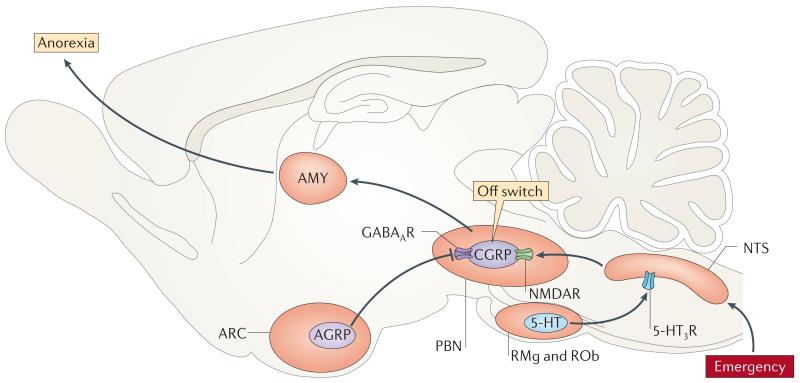
Lithium chloride and lipopolysaccharide (LPS) are agents that, when administered to rodents, mimic the consumption of chemical and bacterial toxins, respectively. As such, each induces anorexia and can support CTA formation. The PBN is implicated in these responses as both lithium chloride and LPS activate PBN neurons, and lesions of the PBN prevent CTA formation163,164. Contained within the PBN are CGRP-expressing neurons that project to the amygdala and are implicated as mediators of anorexia that is induced by stressful stimuli81. The activity of these neurons increases in response to input from ascending projections from the caudal hindbrain, although conversely, they are tonically inhibited by GABAergic input from AGRP neurons79-81. Using a combination of viral and genetic approaches, a recent study showed that these PBN CGRP neurons are activated by both lithium chloride and LPS81, and that activation of these neurons in unstressed mice (using either optogenetics or DREADD technology) causes feeding to decrease or even to cease altogether. With repeated stimulation, animals continue to exhibit anorexia even when they are threatened with death from starvation79-81 (FIG. 5).
Figure 5. Activation of emergency neurocircuits that inhibit feeding.
Neurocircuits exist that, when activated, can override the homeostatic control of food intake. Recent work from the Palmiter laboratory suggests that calcitonin gene-related peptide (CGRP) neurons expressed in the parabrachial nucleus (PBN) are an ‘off switch’ that can trigger anorexia in the context of emergency conditions (that is, illness, trauma or injury). The activity of this neurocircuit is constrained by inhibitory GABAergic input from agouti-related protein (AGRP) neurons in the arcuate nucleus (ARC), but this inhibition can be overcome in response to trauma, illness or stress. Some PBN neurons express NMDA receptors (NMDARs) that are activated by glutamatergic input from neurons in the rostral nucleus of the solitary tract (NTS), which in turn are regulated by serotonergic input from neurons located in the raphe magnus (RMg) and raphe obscurus (ROb). The net effect of activating this circuit is to activate CGRP neurons and thereby inhibit feeding. AMY, amygdala; GABAAR, type A GABA receptor; 5-HT, 5-hydroxytryptamine (serotonin); 5-HT3R, 5-HT3 receptor.
Perhaps most importantly, the anorexia induced by lithium chloride and LPS is blocked when PBN CGRP neurons are inhibited81, whereas inhibition of these neurons has no effect on intake in normal, unstressed animals; the latter finding fits with evidence that under usual conditions, these neurons are already inhibited, at least in part by GABAergic input from AGRP neurons. Taken together, these findings suggest that one function of neurons in energy homeostasis circuits (for example, AGRP neurons) is to inhibit neurons in emergency feeding circuits (for example, CGRP neurons). However, when faced with a stress that is sufficient to override this inhibition, feeding ceases until the stress has passed.
Implications for disease states
Wasting illness is common not only in cancer but also in chronic infectious, inflammatory and other disorders. In these conditions, wasting is a major cause of morbidity and mortality8, and insight into its pathogenesis has proven elusive despite decades of study. Empirically, wasting can be considered a state in which the energy homeostasis system does not function properly, as food intake remains low irrespective of the amount of weight lost165. Furthermore, weight loss in normal individuals is typified by the preferential depletion of body fat, with relative sparing of lean mass, whereas wasting illness is characterized as cachexia, which is defined as progressive weight loss without sparing of lean mass.
With this background, the identification and characterization of CGRP neurons by the Palmiter group raises an important question: does chronic activation of this or a similar endogenous ‘off switch’ for feeding drive the pathogenesis of wasting illness in diseases such as cancer? Perhaps certain tumours (or the body’s response to tumour cells) might result in the production of factors that activate CGRP neurons in the PBN, thereby causing inexorable, unrelenting weight loss that completely overrides the energy homeostasis system. If this hypothesis is correct, silencing these neurons should improve the wasting disorder or even induce its remission. We view testing of this hypothesis as an important scientific priority.
Summary and conclusions
That robust and powerful systems ensure that the body’s ongoing energy demands are met comes as no surprise. At the same time, carrying either too much or too little body fat can be maladaptive. To address these competing needs, the energy homeostasis system evolved to enable animals to match energy intake to energy expenditure over long time intervals and thereby ensure stability in the amount of body energy stored as fat. However, under pathological conditions, activation of an unrelated set of neurocircuits can override control exerted by the energy homeostasis system, leading to common and potentially serious disorders at either end of the body weight spectrum.
A key goal underlying efforts to delineate energy homeostasis neurocircuits is to facilitate the discovery of effective new therapeutic modalities, but little progress has been made in this effort to date. Bariatric surgery can effectively induce and sustain weight loss, but the underlying mechanisms remain poorly understood. Possibilities include both neural mechanisms (for example, activation of a ‘gut–brain’ axis by re-routing or accelerating the flow of intestinal nutrients) and humoral mechanisms (for example, markedly increasing the secretion of satiety-inducing gut peptides)166, but how these or other such effects ultimately lower the defended level of body fat mass remains unclear.
Options for medical therapy increased following the US Food and Drug Administration approval of both lorcaserin (Belviq), a 5-hydroxytryptamine (serotonin) 2C agonist, and Qsymia, a drug that combines phentermine (an adrenergic agonist) with the anticonvulsant topiramate. Lorcaserin-induced weight loss is probably mediated at least in part by activation of POMC neurons167 and, although the drug’s safety profile is favourable, efficacy is modest168. Qsymia is a somewhat more potent weight loss agent169, but how topiramate affects energy homeostasis neurocircuitry is unknown. Clearly, there is ample room for improvement where treatment of obesity and other weight disorders is concerned, and efforts to delineate energy homeostasis and stress-responsive neurocircuitry have great potential to move the field forward. Recent technological advances offer exciting new tools with which to accomplish these goals and obtain information that will inform strategies for more effective approaches to the treatment of these common and debilitating disorders.
Acknowledgements
This work was supported by a US National Institute of Diabetes and Digestive and Kidney Diseases Grant to M.W.S (DK090320, DK083042, and DK052989) and G.J.M. (DK089053), the US National Institutes of Health (NIH) funded Nutrition Obesity Research Center (DK035816) and Diabetes Research Center (DK17047) at the University of Washington and a NIH Diabetes and Metabolism training Grant (F32 DK097859; T32 DK0007247).
Glossary
- Energy homeostasis
The biological process by which the body maintains body fat stores by balancing energy intake with energy expenditure over time.
- Anorexia
A disorder that is characterized by a reduction in energy intake and accompanied weight loss.
- Adiposity negative feedback signals
Hormones that circulate in direct proportion to body fat and convey the state of total energy stores to the CNS.
- Satiety
The state of feeling full to the point of satisfaction after the consumption of food.
- Neuropeptide
A small protein-like molecule that is used by neurons to communicate with each other, often in a paracrine manner.
- Optogenetics
A technique that uses light to control the activity of specific neurons in living tissue.
- DREADD
(Designer receptor exclusively activated by a designer drug). G protein-coupled receptors that are modified for activation by binding to inert small molecules that are used to non-invasively control neuronal signalling.
- Neurotransmitters
Chemical messengers that are released by the end of a nerve fibre, causing an impulse to be passed from once cell to another.
- Leptin resistance
A state in which the body is no longer responsive to the anorexic effect of exogenous leptin.
- Conditioned taste aversion
(CTA). A learned response of an animal to avoid repeated ingestion of certain foods that cause nausea or sickness.
- Cachexia
A condition that is characterized by anorexia, weight loss and disproportionate wasting of muscle and adipose tissue.
Footnotes
Competing interests statement
The authors declare no competing interests.
References
- 1.Edholm OG. Energy balance in man studies carried out by the Division of Human Physiology, National Institute for Medical Research. J. Hum. Nutr. 1977;31:413–431. [PubMed] [Google Scholar]
- 2.Edholm OG, Fletcher JG, Widdowson EM, McCance RA. The energy expenditure and food intake of individual men. Br. J. Nutr. 1955;9:286–300. doi: 10.1079/bjn19550040. [DOI] [PubMed] [Google Scholar]
- 3.Bray GA, Flatt JP, Volaufova J, Delany JP, Champagne CM. Corrective responses in human food intake identified from an analysis of 7-d food-intake records. Am. J. Clin. Nutr. 2008;88:1504–1510. doi: 10.3945/ajcn.2008.26289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Schwartz MW, et al. Central nervous system control of food intake. Nature. 2000;404:661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- 5.Morton GJ, Cummings DE, Baskin DG, Barsh GS, Schwartz MW. Central nervous system control of food intake and body weight. Nature. 2006;443:289–295. doi: 10.1038/nature05026. This comprehensive review provides a new conceptual understanding of how energy homeostasis is achieved.
- 6.Saper CB, Chou TC, Elmquist JK. The need to feed: homeostatic and hedonic control of eating. Neuron. 2002;36:199–211. doi: 10.1016/s0896-6273(02)00969-8. [DOI] [PubMed] [Google Scholar]
- 7.Nguyen DM, El-Serag HB. The epidemiology of obesity. Gastroenterol. Clin. North Am. 2010;39:1–7. doi: 10.1016/j.gtc.2009.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Braun TP, Marks DL. Pathophysiology and treatment of inflammatory anorexia in chronic disease. J. Cachexia Sarcopenia Muscle. 2010;1:135–145. doi: 10.1007/s13539-010-0015-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ritter RC, Slusser P. 5-Thio-D-glucose causes increased feeding and hyperglycemia in the rat. Am. J. Physiol. 1980;238:E141–E144. doi: 10.1152/ajpendo.1980.238.2.E141. This study provides evidence that the hindbrain is important in responding to neuroglucopenia.
- 10.Kennedy G. The role of depot fat in the hypothalamic control of food intake in the rat. Proc. R. Soc. Lond. B. 1953;140:578–592. doi: 10.1098/rspb.1953.0009. [DOI] [PubMed] [Google Scholar]
- 11.Gao Q, Horvath TL. Neurobiology of feeding and energy expenditure. Annu. Rev. Neurosci. 2007;30:367–398. doi: 10.1146/annurev.neuro.30.051606.094324. [DOI] [PubMed] [Google Scholar]
- 12.Rosenbaum M, Leibel RL. Adaptive thermogenesis in humans. Int. J. Obes. (Lond.) 2010;34(Suppl. 1):47–55. doi: 10.1038/ijo.2010.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Y, et al. Positional cloning of the mouse obese gene and its human homologue. Nature. 1994;372:425–432. doi: 10.1038/372425a0. This study describes the mapping and sequencing of the gene that encodes the hormone leptin.
- 14.Considine RV, et al. Serum immunoreactive-leptin concentrations in normal-weight and obese humans. N. Engl. J. Med. 1996;334:292–295. doi: 10.1056/NEJM199602013340503. [DOI] [PubMed] [Google Scholar]
- 15.Schwartz MW, Peskind E, Raskind M, Boyko EJ, Porte D., Jr. Cerebrospinal fluid leptin levels: relationship to plasma levels and to adiposity in humans. Nature Med. 1996;2:589–593. doi: 10.1038/nm0596-589. [DOI] [PubMed] [Google Scholar]
- 16.Baskin DG, Breininger JF, Schwartz MW. Leptin receptor mRNA identifies a subpopulation of neuropeptide Y neurons activated by fasting in rat hypothalamus. Diabetes. 1999;48:828–833. doi: 10.2337/diabetes.48.4.828. [DOI] [PubMed] [Google Scholar]
- 17.Elmquist JK, Bjorbaek C, Ahima RS, Flier JS, Saper CB. Distributions of leptin receptor mRNA isoforms in the rat brain. J. Comp. Neurol. 1998;395:535–547. [PubMed] [Google Scholar]
- 18.Campfield LA, Smith FJ, Guisez Y, Devos R, Burn P. Recombinant mouse OB protein: evidence for a peripheral signal linking adiposity and central neural networks. Science. 1995;269:546–549. doi: 10.1126/science.7624778. [DOI] [PubMed] [Google Scholar]
- 19.Halaas JL, et al. Physiological response to long-term peripheral and central leptin infusion in lean and obese mice. Proc. Natl Acad. Sci. USA. 1997;94:8878–8883. doi: 10.1073/pnas.94.16.8878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lee G-H, et al. Abnormal splicing of the leptin receptor in diabetic mice. Nature. 1996;379:632–635. doi: 10.1038/379632a0. [DOI] [PubMed] [Google Scholar]
- 21.Bagdade JD, Bierman EL, Porte D., Jr. The significance of basal insulin levels in the evaluation of the insulin response to glucose in diabetic and nondiabetic subjects. J. Clin. Invest. 1967;46:1549–1557. doi: 10.1172/JCI105646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Woods SC, Lotter EC, McKay LD, Porte D., Jr. Chronic intracerebroventricular infusion of insulin reduces food intake and body weight of baboons. Nature. 1979;282:503–505. doi: 10.1038/282503a0. An early study demonstrating that insulin is an adiposity signal that acts in the brain of non-human primates to regulate food intake and body weight.
- 23.Bruning JC, et al. Role of brain insulin receptor in control of body weight and reproduction. Science. 2000;289:2122–2125. doi: 10.1126/science.289.5487.2122. [DOI] [PubMed] [Google Scholar]
- 24.Batterham RL, et al. Gut hormone PYY3-36 physiologically inhibits food intake. Nature. 2002;418:650–654. doi: 10.1038/nature00887. [DOI] [PubMed] [Google Scholar]
- 25.Turton MD, et al. A role for glucagon-like peptide-1 in the central regulation of feeding. Nature. 1996;379:69–72. doi: 10.1038/379069a0. [DOI] [PubMed] [Google Scholar]
- 26.Gibbs J, Young RC, Smith GP. Cholecystokinin decreases food intake in rats. J. Comp. Physiol. Psychol. 1973;84:488–495. doi: 10.1037/h0034870. [DOI] [PubMed] [Google Scholar]
- 27.Tschop M, Smiley DL, Heiman ML. Ghrelin induces adiposity in rodents. Nature. 2000;407:908–913. doi: 10.1038/35038090. [DOI] [PubMed] [Google Scholar]
- 28.Lam TK. Neuronal regulation of homeostasis by nutrient sensing. Nature Med. 2010;16:392–395. doi: 10.1038/nm0410-392. [DOI] [PubMed] [Google Scholar]
- 29.Strubbe JH, Woods SC. The timing of meals. Psychol. Rev. 2004;111:128–141. doi: 10.1037/0033-295X.111.1.128. [DOI] [PubMed] [Google Scholar]
- 30.West DB, Fey D, Woods SC. Cholecystokinin persistently suppresses meal size but not food intake in free-feeding rats. Am. J. Physiol. 1984;246:R776–R787. doi: 10.1152/ajpregu.1984.246.5.R776. [DOI] [PubMed] [Google Scholar]
- 31.McMinn JE, Sindelar DK, Havel PJ, Schwartz MW. Leptin deficiency induced by fasting impairs the satiety response to cholecystokinin. Endocrinology. 2000;141:4442–4448. doi: 10.1210/endo.141.12.7815. [DOI] [PubMed] [Google Scholar]
- 32.Barrachina MD, Martinez V, Wang L, Wei JY, Tache Y. Synergistic interaction between leptin and cholecystokinin to reduce short-term food intake in lean mice. Proc. Natl Acad. Sci. USA. 1997;94:10455–10460. doi: 10.1073/pnas.94.19.10455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Figlewicz DP, Stein LJ, West D, Porte D, Jr, Woods SC. Intracisternal insulin alters sensitivity to CCK-induced meal suppression in baboons. Am. J. Physiol. 1986;250:R856–R860. doi: 10.1152/ajpregu.1986.250.5.R856. [DOI] [PubMed] [Google Scholar]
- 34.Emond M, Schwartz GJ, Ladenheim EE, Moran TH. Central leptin modulates behavioral and neural responsivity to CCK. Am. J. Physiol. 1999;276:R1545–R1549. doi: 10.1152/ajpregu.1999.276.5.R1545. [DOI] [PubMed] [Google Scholar]
- 35.Williams DL, Baskin DG, Schwartz MW. Evidence that intestinal glucagon-like peptide-1 plays a physiological role in satiety. Endocrinology. 2009;150:1680–1687. doi: 10.1210/en.2008-1045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hulsey MG, Lu H, Wang T, Martin RJ, Baile CA. Intracerebroventricular (i.c.v.) administration of mouse leptin in rats: behavioral specificity and effects on meal patterns. Physiol. Behav. 1998;65:445–455. doi: 10.1016/s0031-9384(98)00180-2. [DOI] [PubMed] [Google Scholar]
- 37.Kahler A, et al. Chronic administration of OB protein decreases food intake by selectively reducing meal size in male rats. Am. J. Physiol. 1998;275:R180–R185. doi: 10.1152/ajpregu.1998.275.1.R180. [DOI] [PubMed] [Google Scholar]
- 38.McLaughlin CL, Baile CA. Decreased sensitivity of Zucker obese rats to the putative satiety agent cholecystokinin. Physiol. Behav. 1980;25:543–548. doi: 10.1016/0031-9384(80)90119-5. [DOI] [PubMed] [Google Scholar]
- 39.Morton GJ, et al. Leptin regulates insulin sensitivity via phosphatidylinositol-3-OH kinase signaling in mediobasal hypothalamic neurons. Cell. Metab. 2005;2:411–420. doi: 10.1016/j.cmet.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 40.Grill HJ, et al. Evidence that the caudal brainstem is a target for the inhibitory effect of leptin on food intake. Endocrinology. 2002;143:239–246. doi: 10.1210/endo.143.1.8589. [DOI] [PubMed] [Google Scholar]
- 41.Morton GJ, et al. Leptin action in the forebrain regulates the hindbrain response to satiety signals. J. Clin. Invest. 2005;115:703–710. doi: 10.1172/JCI200522081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Barrera JG, Sandoval DA, D’Alessio DA, Seeley RJ. GLP-1 and energy balance: an integrated model of short-term and long-term control. Nature Rev. Endocrinol. 2011;7:507–516. doi: 10.1038/nrendo.2011.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berthoud HR. Homeostatic and non-homeostatic pathways involved in the control of food intake and energy balance. Obesity. 2006;14(Suppl. 5):197S–200S. doi: 10.1038/oby.2006.308. [DOI] [PubMed] [Google Scholar]
- 44.Figlewicz DP. Adiposity signals and food reward: expanding the CNS roles of insulin and leptin. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2003;284:R882–R892. doi: 10.1152/ajpregu.00602.2002. This is one of the first reviews to describe the role of the adiposity hormones in the regulation of the reward system.
- 45.Dossat AM, Lilly N, Kay K, Williams DL. Glucagon-like peptide 1 receptors in nucleus accumbens affect food intake. J. Neurosci. 2011;31:14453–14457. doi: 10.1523/JNEUROSCI.3262-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Mehta S, et al. Regional brain response to visual food cues is a marker of satiety that predicts food choice. Am. J. Clin. Nutr. 2012;96:989–999. doi: 10.3945/ajcn.112.042341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nijs IM, Muris P, Euser AS, Franken IH. Differences in attention to food and food intake between overweight/obese and normal-weight females under conditions of hunger and satiety. Appetite. 2010;54:243–254. doi: 10.1016/j.appet.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 48.Figlewicz DP, Sipols AJ. Energy regulatory signals and food reward. Pharmacol. Biochem. Behav. 2010;97:15–24. doi: 10.1016/j.pbb.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fulton S, Woodside B, Shizgal P. Modulation of brain reward circuitry by leptin. Science. 2000;287:125–128. doi: 10.1126/science.287.5450.125. [DOI] [PubMed] [Google Scholar]
- 50.Farooqi IS, et al. Leptin regulates striatal regions and human eating behavior. Science. 2007;317:1355. doi: 10.1126/science.1144599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Berthoud HR, Lenard NR, Shin AC. Food reward, hyperphagia, and obesity. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2011;300:R1266–R1277. doi: 10.1152/ajpregu.00028.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stice E, Figlewicz DP, Gosnell BA, Levine AS, Pratt WE. The contribution of brain reward circuits to the obesity epidemic. Neurosci. Biobehav. Rev. 2012;37:2047–2058. doi: 10.1016/j.neubiorev.2012.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Kelley AE, Baldo BA, Pratt WE, Will MJ. Corticostriatal-hypothalamic circuitry and food motivation: integration of energy, action and reward. Physiol. Behav. 2005;86:773–795. doi: 10.1016/j.physbeh.2005.08.066. [DOI] [PubMed] [Google Scholar]
- 54.Leinninger GM, et al. Leptin acts via leptin receptor-expressing lateral hypothalamic neurons to modulate the mesolimbic dopamine system and suppress feeding. Cell. Metab. 2009;10:89–98. doi: 10.1016/j.cmet.2009.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Hahn TM, Breininger JF, Baskin DG, Schwartz MW. Coexpression of Agrp and NPY in fasting-activated hypothalamic neurons. Nature Neurosci. 1998;1:271–272. doi: 10.1038/1082. [DOI] [PubMed] [Google Scholar]
- 56.Hagan MM, et al. Long-term orexigenic effects of AgRP-(83—132) involve mechanisms other than melanocortin receptor blockade. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000;279:R47–R52. doi: 10.1152/ajpregu.2000.279.1.R47. [DOI] [PubMed] [Google Scholar]
- 57.Cowley MA, et al. Leptin activates anorexigenic POMC neurons through a neural network in the arcuate nucleus. Nature. 2001;411:480–484. doi: 10.1038/35078085. A groundbreaking study identifying POMC neurons in the ARC as being leptin-responsive and under GABA inhibition.
- 58.Spanswick D, Smith MA, Groppi VE, Logan SD, Ashford ML. Leptin inhibits hypothalamic neurons by activation of ATP-sensitive potassium channels. Nature. 1997;390:521–525. doi: 10.1038/37379. [DOI] [PubMed] [Google Scholar]
- 59.Spanswick D, Smith MA, Mirshamsi S, Routh VH, Ashford ML. Insulin activates ATP-sensitive K+ channels in hypothalamic neurons of lean, but not obese rats. Nature Neurosci. 2000;3:757–758. doi: 10.1038/77660. [DOI] [PubMed] [Google Scholar]
- 60.Cowley MA, et al. The distribution and mechanism of action of ghrelin in the CNS demonstrates a novel hypothalamic circuit regulating energy homeostasis. Neuron. 2003;37:649–661. doi: 10.1016/s0896-6273(03)00063-1. [DOI] [PubMed] [Google Scholar]
- 61.Schwartz MW, et al. Specificity of leptin action on elevated blood glucose levels and hypothalamic neuropeptide Y gene expression in ob/ob mice. Diabetes. 1996;45:531–535. doi: 10.2337/diab.45.4.531. [DOI] [PubMed] [Google Scholar]
- 62.Schwartz MW, et al. Leptin increases hypothalamic pro-opiomelanocortin mRNA expression in the rostral arcuate nucleus. Diabetes. 1997;46:2119–2123. doi: 10.2337/diab.46.12.2119. [DOI] [PubMed] [Google Scholar]
- 63.Fan W, Boston BA, Kesterson RA, Hruby VJ, Cone RD. Role of melanocortinergic neurons in feeding and the agouti obesity syndrome. Nature. 1997;385:165–168. doi: 10.1038/385165a0. This paper was one of the first to identify the melanocortin system and the MC4R in the control of feeding behaviour.
- 64.Williams KW, et al. Segregation of acute leptin and insulin effects in distinct populations of arcuate proopiomelanocortin neurons. J. Neurosci. 2010;30:2472–2479. doi: 10.1523/JNEUROSCI.3118-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hill JW, et al. Direct insulin and leptin action on pro-opiomelanocortin neurons is required for normal glucose homeostasis and fertility. Cell. Metab. 2010;11:286–297. doi: 10.1016/j.cmet.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sohn JW, et al. Serotonin 2C receptor activates a distinct population of arcuate pro-opiomelanocortin neurons via TRPC channels. Neuron. 2011;71:488–497. doi: 10.1016/j.neuron.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sohn JW, Elmquist JK, Williams KW. Neuronal circuits that regulate feeding behavior and metabolism. Trends Neurosci. 2013;36:504–512. doi: 10.1016/j.tins.2013.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gautron L, Elmquist JK. Sixteen years and counting: an update on leptin in energy balance. J. Clin. Invest. 2011;121:2087–2093. doi: 10.1172/JCI45888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.van de Wall E, et al. Collective and individual functions of leptin receptor modulated neurons controlling metabolism and ingestion. Endocrinology. 2008;149:1773–1785. doi: 10.1210/en.2007-1132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Ring LE, Zeltser LM. Disruption of hypothalamic leptin signaling in mice leads to early-onset obesity, but physiological adaptations in mature animals stabilize adiposity levels. J. Clin. Invest. 2010;120:2931–2941. doi: 10.1172/JCI41985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Dhillon H, et al. Leptin directly activates SF1 neurons in the VMH, and this action by leptin is required for normal body-weight homeostasis. Neuron. 2006;49:191–203. doi: 10.1016/j.neuron.2005.12.021. [DOI] [PubMed] [Google Scholar]
- 72.Fulton S, et al. Leptin regulation of the mesoaccumbens dopamine pathway. Neuron. 2006;51:811–822. doi: 10.1016/j.neuron.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 73.Hommel JD, et al. Leptin receptor signaling in midbrain dopamine neurons regulates feeding. Neuron. 2006;51:801–810. doi: 10.1016/j.neuron.2006.08.023. [DOI] [PubMed] [Google Scholar]
- 74.Hayes MR, et al. Endogenous leptin signaling in the caudal nucleus tractus solitarius and area postrema is required for energy balance regulation. Cell. Metab. 2010;11:77–83. doi: 10.1016/j.cmet.2009.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vong L, et al. Leptin action on GABAergic neurons prevents obesity and reduces inhibitory tone to POMC neurons. Neuron. 2011;71:142–154. doi: 10.1016/j.neuron.2011.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Balthasar N, et al. Leptin receptor signaling in POMC neurons is required for normal body weight homeostasis. Neuron. 2004;42:983–991. doi: 10.1016/j.neuron.2004.06.004. [DOI] [PubMed] [Google Scholar]
- 77.Leshan RL, Greenwald-Yarnell M, Patterson CM, Gonzalez IE, Myers MG., Jr. Leptin action through hypothalamic nitric oxide synthase-1-expressing neurons controls energy balance. Nature Med. 2012;18:820–823. doi: 10.1038/nm.2724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Tong Q, Ye CP, Jones JE, Elmquist JK, Lowell BB. Synaptic release of GABA by AgRP neurons is required for normal regulation of energy balance. Nature Neurosci. 2008;11:998–1000. doi: 10.1038/nn.2167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Wu Q, Boyle MP, Palmiter RD. Loss of GABAergic signaling by AgRP neurons to the parabrachial nucleus leads to starvation. Cell. 2009;137:1225–1234. doi: 10.1016/j.cell.2009.04.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Wu Q, Clark MS, Palmiter RD. Deciphering a neuronal circuit that mediates appetite. Nature. 2012;483:594–597. doi: 10.1038/nature10899. An excellent paper identifying the PBN as an integration centre of visceral toxicity via hindbrain glutamatergic signals and GABAergic homeostatic feeding circuits.
- 81.Carter ME, Soden ME, Zweifel LS, Palmiter RD. Genetic identification of a neural circuit that suppresses appetite. Nature. 2013;503:111–114. doi: 10.1038/nature12596. In this paper, the authors identify a neural circuit that suppresses appetite.
- 82.Kramer RH, Mourot A, Adesnik H. Optogenetic pharmacology for control of native neuronal signaling proteins. Nature Neurosci. 2013;16:816–823. doi: 10.1038/nn.3424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Packer AM, Roska B, Hausser M. Targeting neurons and photons for optogenetics. Nature Neurosci. 2013;16:805–815. doi: 10.1038/nn.3427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Aponte Y, Atasoy D, Sternson SM. AGRP neurons are sufficient to orchestrate feeding behavior rapidly and without training. Nature Neurosci. 2011;14:351–355. doi: 10.1038/nn.2739. The first use of optogenetics in the field of energy balance, examining the effect of AGRP neuronal activation on feeding.
- 85.Atasoy D, Betley JN, Su HH, Sternson SM. Deconstruction of a neural circuit for hunger. Nature. 2012;488:172–177. doi: 10.1038/nature11270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Krashes MJ, et al. Rapid, reversible activation of AgRP neurons drives feeding behavior in mice. J. Clin. Invest. 2011;121:1424–1428. doi: 10.1172/JCI46229. Another pioneering study using DREADD technology to manipulate neurons involved in energy homeostasis.
- 87.White JD, Kershaw M. Increased hypothalamic neuropeptide Y expression following food deprivation. Mol. Cell Neurosci. 1990;1:41–48. doi: 10.1016/1044-7431(90)90040-b. [DOI] [PubMed] [Google Scholar]
- 88.Sipols AJ, Baskin DG, Schwartz MW. Effect of intracerebroventricular insulin infusion on diabetic hyperphagia and hypothalamic neuropeptide gene expression. Diabetes. 1995;44:147–151. doi: 10.2337/diab.44.2.147. [DOI] [PubMed] [Google Scholar]
- 89.Wilding JP, et al. Increased neuropeptide-Y messenger ribonucleic acid (mRNA) and decreased neurotensin mRNA in the hypothalamus of the obese (ob/ob) mouse. Endocrinology. 1993;132:1939–1944. doi: 10.1210/endo.132.5.7682936. [DOI] [PubMed] [Google Scholar]
- 90.Krashes MJ, Shah BP, Koda S, Lowell BB. Rapid versus delayed stimulation of feeding by the endogenously released AgRP neuron mediators GABA, NPY, and AgRP. Cell. Metab. 2013;18:588–595. doi: 10.1016/j.cmet.2013.09.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Leibowitz SF, Hammer NJ, Chang K. Hypothalamic paraventricular nucleus lesions produce overeating and obesity in the rat. Physiol. Behav. 1981;27:1031–1040. doi: 10.1016/0031-9384(81)90366-8. [DOI] [PubMed] [Google Scholar]
- 92.Huszar D, et al. Targeted disruption of the melanocortin-4 receptor results in obesity in mice. Cell. 1997;88:131–141. doi: 10.1016/s0092-8674(00)81865-6. [DOI] [PubMed] [Google Scholar]
- 93.Vaisse C, Clement K, Guy Grand B, Froguel P. A frameshift mutation in human MC4R is associated with a dominant form of obesity. Nature Genet. 1998;20:113–114. doi: 10.1038/2407. [DOI] [PubMed] [Google Scholar]
- 94.Yeo GS, et al. A frameshift mutation in MC4R associated with dominantly inherited human obesity. Nature Genet. 1998;20:111–112. doi: 10.1038/2404. [DOI] [PubMed] [Google Scholar]
- 95.Farooqi IS, et al. Clinical spectrum of obesity and mutations in the melanocortin 4 receptor gene. N. Engl. J. Med. 2003;348:1085–1095. doi: 10.1056/NEJMoa022050. [DOI] [PubMed] [Google Scholar]
- 96.Mountjoy KG, Mortrud MT, Low MJ, Simerly RB, Cone RD. Localization of the melanocortin-4 receptor (MC4-R) in neuroendocrine and autonomic control circuits in the brain. Mol. Endocrinol. 1994;8:1298–1308. doi: 10.1210/mend.8.10.7854347. [DOI] [PubMed] [Google Scholar]
- 97.Cowley MA, et al. Integration of NPY, AGRP, and melanocortin signals in the hypothalamic paraventricular nucleus: evidence of a cellular basis for the adipostat. Neuron. 1999;24:155–163. doi: 10.1016/s0896-6273(00)80829-6. [DOI] [PubMed] [Google Scholar]
- 98.Giraudo SQ, Billington CJ, Levine AS. Feeding effects of hypothalamic injection of melanocortin 4 receptor ligands. Brain Res. 1998;809:302–306. doi: 10.1016/s0006-8993(98)00837-3. [DOI] [PubMed] [Google Scholar]
- 99.Balthasar N, et al. Divergence of melanocortin pathways in the control of food intake and energy expenditure. Cell. 2005;123:493–505. doi: 10.1016/j.cell.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 100.Rossi J, et al. Melanocortin-4 receptors expressed by cholinergic neurons regulate energy balance and glucose homeostasis. Cell. Metab. 2011;13:195–204. doi: 10.1016/j.cmet.2011.01.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Arletti R, Benelli A, Bertolini A. Influence of oxytocin on feeding behavior in the rat. Peptides. 1989;10:89–93. doi: 10.1016/0196-9781(89)90082-x. [DOI] [PubMed] [Google Scholar]
- 102.Arletti R, Benelli A, Bertolini A. Oxytocin inhibits food and fluid intake in rats. Physiol. Behav. 1990;48:825–830. doi: 10.1016/0031-9384(90)90234-u. [DOI] [PubMed] [Google Scholar]
- 103.Olson BR, et al. Oxytocin and an oxytocin agonist administered centrally decrease food intake in rats. Peptides. 1991;12:113–118. doi: 10.1016/0196-9781(91)90176-p. [DOI] [PubMed] [Google Scholar]
- 104.Morton GJ, et al. Peripheral oxytocin suppresses food intake and causes weight loss in diet-induced obese rats. Am. J. Physiol. Endocrinol. Metab. 2012;302:E134–E144. doi: 10.1152/ajpendo.00296.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Blevins JE, Ho JM. Role of oxytocin signaling in the regulation of body weight. Rev. Endocr. Metab. Disord. 2013;14:311–329. doi: 10.1007/s11154-013-9260-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Blevins JE, Eakin TJ, Murphy JA, Schwartz MW, Baskin DG. Oxytocin innervation of caudal brainstem nuclei activated by cholecystokinin. Brain Res. 2003;993:30–41. doi: 10.1016/j.brainres.2003.08.036. [DOI] [PubMed] [Google Scholar]
- 107.Blevins JE, Schwartz MW, Baskin DG. Evidence that paraventricular nucleus oxytocin neurons link hypothalamic leptin action to caudal brainstem nuclei controlling meal size. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004;287:R87–R96. doi: 10.1152/ajpregu.00604.2003. [DOI] [PubMed] [Google Scholar]
- 108.Kublaoui BM, Gemelli T, Tolson KP, Wang Y, Zinn AR. Oxytocin deficiency mediates hyperphagic obesity of Sim1 haploinsufficient mice. Mol. Endocrinol. 2008;22:1723–1734. doi: 10.1210/me.2008-0067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Bonnefond A, et al. Loss-of-function mutations in SIM1 contribute to obesity and Prader-Willi-like features. J. Clin. Invest. 2013;123:3037–3041. doi: 10.1172/JCI68035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Holder JL, Jr, Butte NF, Zinn AR. Profound obesity associated with a balanced translocation that disrupts the SIM1 gene. Hum. Mol. Genet. 2000;9:101–108. doi: 10.1093/hmg/9.1.101. [DOI] [PubMed] [Google Scholar]
- 111.Ramachandrappa S, et al. Rare variants in single-minded 1 (SIM1) are associated with severe obesity. J. Clin. Invest. 2013;123:3042–3050. doi: 10.1172/JCI68016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Swaab DF, Purba JS, Hofman MA. Alterations in the hypothalamic paraventricular nucleus and its oxytocin neurons (putative satiety cells) in Prader-Willi syndrome: a study of five cases. J. Clin. Endocrinol. Metab. 1995;80:573–579. doi: 10.1210/jcem.80.2.7852523. [DOI] [PubMed] [Google Scholar]
- 113.Camerino C. Low sympathetic tone and obese phenotype in oxytocin-deficient mice. Obesity. 2009;17:980–984. doi: 10.1038/oby.2009.12. [DOI] [PubMed] [Google Scholar]
- 114.Takayanagi Y, et al. Oxytocin receptor-deficient mice developed late-onset obesity. Neuroreport. 2008;19:951–955. doi: 10.1097/WNR.0b013e3283021ca9. [DOI] [PubMed] [Google Scholar]
- 115.Beall C, Ashford ML, McCrimmon RJ. The physiology and pathophysiology of the neural control of the counterregulatory response. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2012;302:R215–R223. doi: 10.1152/ajpregu.00531.2011. [DOI] [PubMed] [Google Scholar]
- 116.Gerich JE, et al. Prevention of human diabetic ketoacidosis by somatostatin. Evidence for an essential role of glucagon. N. Engl. J. Med. 1975;292:985–989. doi: 10.1056/NEJM197505082921901. [DOI] [PubMed] [Google Scholar]
- 117.Garber AJ, et al. The role of adrenergic mechanisms in the substrate and hormonal response to insulin-induced hypoglycemia in man. J. Clin. Invest. 1976;58:7–15. doi: 10.1172/JCI108460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Rizza RA, Cryer PE, Gerich JE. Role of glucagon, catecholamines, and growth hormone in human glucose counterregulation. Effects of somatostatin and combined α- and β-adrenergic blockade on plasma glucose recovery and glucose flux rates after insulin-induced hypoglycemia. J. Clin. Invest. 1979;64:62–71. doi: 10.1172/JCI109464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ritter S, Li AJ, Wang Q, Dinh TT. Minireview: the value of looking backward: the essential role of the hindbrain in counterregulatory responses to glucose deficit. Endocrinology. 2011;152:4019–4032. doi: 10.1210/en.2010-1458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.McCrimmon RJ, Sherwin RS. Hypoglycemia in type 1 diabetes. Diabetes. 2010;59:2333–2339. doi: 10.2337/db10-0103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Routh VH. Glucose-sensing neurons: are they physiologically relevant? Physiol. Behav. 2002;76:403–413. doi: 10.1016/s0031-9384(02)00761-8. [DOI] [PubMed] [Google Scholar]
- 122.Watts AG, Donovan CM. Sweet talk in the brain: glucosensing, neural networks, and hypoglycemic counterregulation. Front. Neuroendocrinol. 2010;31:32–43. doi: 10.1016/j.yfrne.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Dryden S, Pickavance L, Henderson L, Williams G. Hyperphagia induced by hypoglycemia in rats is independent of leptin and hypothalamic neuropeptide Y. (NPY) Peptides. 1998;19:1549–1555. doi: 10.1016/s0196-9781(98)00106-5. [DOI] [PubMed] [Google Scholar]
- 124.Russell-Jones D, Khan R. Insulin-associated weight gain in diabetes—causes, effects and coping strategies. Diabetes Obes. Metab. 2007;9:799–812. doi: 10.1111/j.1463-1326.2006.00686.x. [DOI] [PubMed] [Google Scholar]
- 125.Sindelar DK, et al. Neuropeptide Y is required for hyperphagic feeding in response to neuroglucopenia. Endocrinology. 2004;145:3363–3368. doi: 10.1210/en.2003-1727. [DOI] [PubMed] [Google Scholar]
- 126.Sergeyev V, Broberger C, Gorbatyuk O, Hokfelt T. Effect of 2-mercaptoacetate and 2-deoxy-D-glucose administration on the expression of NPY, AGRP, POMC, MCH and hypocretin/orexin in the rat hypothalamus. Neuroreport. 2000;11:117–121. doi: 10.1097/00001756-200001170-00023. [DOI] [PubMed] [Google Scholar]
- 127.Luquet S, Phillips CT, Palmiter RD. NPY/AgRP neurons are not essential for feeding responses to glucoprivation. Peptides. 2007;28:214–225. doi: 10.1016/j.peptides.2006.08.036. [DOI] [PubMed] [Google Scholar]
- 128.Corrin SE, McCarthy HD, McKibbin PE, Williams G. Unchanged hypothalamic neuropeptide Y concentrations in hyperphagic, hypoglycemic rats: evidence for specific metabolic regulation of hypothalamic NPY. Peptides. 1991;12:425–430. doi: 10.1016/0196-9781(91)90080-9. [DOI] [PubMed] [Google Scholar]
- 129.Ritter S, Bugarith K, Dinh TT. Immunotoxic destruction of distinct catecholamine subgroups produces selective impairment of glucoregulatory responses and neuronal activation. J. Comp. Neurol. 2001;432:197–216. doi: 10.1002/cne.1097. [DOI] [PubMed] [Google Scholar]
- 130.Havel PJ, et al. Marked and rapid decreases of circulating leptin in streptozotocin diabetic rats: reversal by insulin. Am. J. Physiol. 1998;274:R1482–R1491. doi: 10.1152/ajpregu.1998.274.5.R1482. [DOI] [PubMed] [Google Scholar]
- 131.American Diabetes Association Standards of medical care in diabetes—2011. Diabetes Care. 2011;34(Suppl. 1):11–61. doi: 10.2337/dc11-0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Kumaresan P, Turner CW. Effect of alloxan on feed consumption and on replacement therapy with graded levels of insulin in rats. Proc. Soc. Exp. Biol. Med. 1966;122:526–527. doi: 10.3181/00379727-122-31180. [DOI] [PubMed] [Google Scholar]
- 133.Ahima RS, et al. Role of leptin in the neuroendocrince response to fasting. Nature. 1996;382:250–252. doi: 10.1038/382250a0. [DOI] [PubMed] [Google Scholar]
- 134.Bray GA, Fisler J, York DA. Neuroendocrine control of the development of obesity: understanding gained from studies of experimental animal models. Front. Neuroendocrinol. 1990;11:128–181. [Google Scholar]
- 135.Fujikawa T, Chuang JC, Sakata I, Ramadori G, Coppari R. Leptin therapy improves insulin-deficient type 1 diabetes by CNS-dependent mechanisms in mice. Proc. Natl Acad. Sci. USA. 2010;107:17391–17396. doi: 10.1073/pnas.1008025107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.German JP, et al. Leptin activates a novel CNS mechanism for insulin-independent normalization of severe diabetic hyperglycemia. Endocrinology. 2011;152:394–404. doi: 10.1210/en.2010-0890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Hidaka S, et al. Chronic central leptin infusion restores hyperglycemia independent of food intake and insulin level in streptozotocin-induced diabetic rats. FASEB J. 2002;16:509–518. doi: 10.1096/fj.01-0164com. [DOI] [PubMed] [Google Scholar]
- 138.Lin CY, Higginbotham DA, Judd RL, White BD. Central leptin increases insulin sensitivity in streptozotocin-induced diabetic rats. Am. J. Physiol. Endocrinol. Metab. 2002;282:E1084–E1091. doi: 10.1152/ajpendo.00489.2001. [DOI] [PubMed] [Google Scholar]
- 139.Peters A, et al. The selfish brain: competition for energy resources. Neurosci. Biobehav. Rev. 2004;28:143–180. doi: 10.1016/j.neubiorev.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 140.Schwartz MW, Niswender KD. Adiposity signaling and biological defense against weight gain: absence of protection or central hormone resistance? J. Clin. Endocrinol. Metab. 2004;89:5889–5897. doi: 10.1210/jc.2004-0906. [DOI] [PubMed] [Google Scholar]
- 141.Ryan KK, Woods SC, Seeley RJ. Central nervous system mechanisms linking the consumption of palatable high-fat diets to the defense of greater adiposity. Cell. Metab. 2012;15:137–149. doi: 10.1016/j.cmet.2011.12.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Knowler WC, et al. 10-year follow-up of diabetes incidence and weight loss in the Diabetes Prevention Program Outcomes Study. Lancet. 2009;374:1677–1686. doi: 10.1016/S0140-6736(09)61457-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Safer DJ. Diet, behavior modification, and exercise: a review of obesity treatments from a long-term perspective. South Med. J. 1991;84:1470–1474. [PubMed] [Google Scholar]
- 144.Hagan MM, et al. Role of the CNS melanocortin system in the response to overfeeding. J. Neurosci. 1999;19:2362–2367. doi: 10.1523/JNEUROSCI.19-06-02362.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Sims EA, et al. Experimental obesity in man. Trans. Assoc. Am. Physicians. 1968;81:153–170. [PubMed] [Google Scholar]
- 146.Deriaz O, Fournier G, Tremblay A, Despres JP, Bouchard C. Lean-body-mass composition and resting energy expenditure before and after long-term overfeeding. Am. J. Clin. Nutr. 1992;56:840–847. doi: 10.1093/ajcn/56.5.840. [DOI] [PubMed] [Google Scholar]
- 147.Diaz EO, Prentice AM, Goldberg GR, Murgatroyd PR, Coward WA. Metabolic response to experimental overfeeding in lean and overweight healthy volunteers. Am. J. Clin. Nutr. 1992;56:641–655. doi: 10.1093/ajcn/56.4.641. [DOI] [PubMed] [Google Scholar]
- 148.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N. Engl. J. Med. 1995;332:621–628. doi: 10.1056/NEJM199503093321001. [DOI] [PubMed] [Google Scholar]
- 149.Sims EA, et al. Endocrine and metabolic effects of experimental obesity in man. Recent Prog. Horm. Res. 1973;29:457–496. doi: 10.1016/b978-0-12-571129-6.50016-6. [DOI] [PubMed] [Google Scholar]
- 150.Farooqi IS, et al. Effects of recombinant leptin therapy in a child with congenital leptin deficiency. N. Engl. J. Med. 1999;341:879–884. doi: 10.1056/NEJM199909163411204. A seminal study showing leptin replacement can correct metabolic and endocrine abnormalities in humans with congenital leptin deficiency.
- 151.El-Haschimi K, Pierroz DD, Hileman SM, Bjorbaek C, Flier JS. Two defects contribute to hypothalamic leptin resistance in mice with diet-induced obesity. J. Clin. Invest. 2000;105:1827–1832. doi: 10.1172/JCI9842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Heymsfield SB, et al. Recombinant leptin for weight loss in obese and lean adults: a randomized, controlled, dose-escalation trial. JAMA. 1999;282:1568–1575. doi: 10.1001/jama.282.16.1568. [DOI] [PubMed] [Google Scholar]
- 153.Myers MG, Jr., Leibel RL, Seeley RJ, Schwartz MW. Obesity and leptin resistance: distinguishing cause from effect. Trends Endocrinol. Metab. 2010;21:643–651. doi: 10.1016/j.tem.2010.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Xu H, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J. Clin. Invest. 2003;112:1821–1830. doi: 10.1172/JCI19451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Weisberg SP, et al. Obesity is associated with macrophage accumulation in adipose tissue. J. Clin. Invest. 2003;112:1796–1808. doi: 10.1172/JCI19246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Hotamisligil GS. Inflammation and metabolic disorders. Nature. 2006;444:860–867. doi: 10.1038/nature05485. [DOI] [PubMed] [Google Scholar]
- 157.Posey K, et al. Hypothalamic proinflammatory lipid accumulation, inflammation, and insulin resistance in rats fed a high-fat diet. Am. J. Physiol. Endocrinol. Metab. 2008;296:E1003–E1012. doi: 10.1152/ajpendo.90377.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.De Souza CT, et al. Consumption of a fat-rich diet activates a proinflammatory response and induces insulin resistance in the hypothalamus. Endocrinology. 2005;146:4192–4199. doi: 10.1210/en.2004-1520. [DOI] [PubMed] [Google Scholar]
- 159.Thaler JP, et al. Obesity is associated with hypothalamic injury in rodents and humans. J. Clin. Invest. 2012;122:153–162. doi: 10.1172/JCI59660. A notable study postulating that neuronal injury due to high-fat feeding underlies the development of obesity.
- 160.Zhang X, et al. Hypothalamic IKKβ/NF-κB and ER stress link overnutrition to energy imbalance and obesity. Cell. 2008;135:61–73. doi: 10.1016/j.cell.2008.07.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Thaler JP, Guyenet SJ, Dorfman MD, Wisse BE, Schwartz MW. Hypothalamic inflammation: marker or mechanism of obesity pathogenesis? Diabetes. 2013;62:2629–2634. doi: 10.2337/db12-1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Reilly S. The parabrachial nucleus and conditioned taste aversion. Brain Res. Bull. 1999;48:239–254. doi: 10.1016/s0361-9230(98)00173-7. [DOI] [PubMed] [Google Scholar]
- 163.Reilly S, Trifunovic R. Lateral parabrachial nucleus lesions in the rat: aversive and appetitive gustatory conditioning. Brain Res. Bull. 2000;52:269–278. doi: 10.1016/s0361-9230(00)00263-x. [DOI] [PubMed] [Google Scholar]
- 164.Reilly S, Trifunovic R. Lateral parabrachial nucleus lesions in the rat: neophobia and conditioned taste aversion. Brain Res. Bull. 2001;55:359–366. doi: 10.1016/s0361-9230(01)00517-2. [DOI] [PubMed] [Google Scholar]
- 165.Grossberg AJ, Scarlett JM, Marks DL. Hypothalamic mechanisms in cachexia. Physiol. Behav. 2010;100:478–489. doi: 10.1016/j.physbeh.2010.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Stefater MA, Wilson-Perez HE, Chambers AP, Sandoval DA, Seeley RJ. All bariatric surgeries are not created equal: insights from mechanistic comparisons. Endocr. Rev. 2012;33:595–622. doi: 10.1210/er.2011-1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Berglund ED, et al. Serotoni. 2C receptors in pro-opiomelanocortin neurons regulate energy and glucose homeostasis. J. Clin. Invest. 2013;123:5061–5070. doi: 10.1172/JCI70338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Smith SR, et al. Multicenter, placebo-controlled trial of lorcaserin for weight management. N. Engl. J. Med. 2010;363:245–256. doi: 10.1056/NEJMoa0909809. [DOI] [PubMed] [Google Scholar]
- 169.Gadde KM, et al. Effects of low-dose, controlled-release, phentermine plus topiramate combination on weight and associated comorbidities in overweight and obese adults (CONQUER): a randomised, placebo-controlled, phase 3 trial. Lancet. 2011;377:1341–1352. doi: 10.1016/S0140-6736(11)60205-5. [DOI] [PubMed] [Google Scholar]
- 170.Marx J. Cellular warriors at the battle of the bulge. Science. 2003;299:846–849. doi: 10.1126/science.299.5608.846. [DOI] [PubMed] [Google Scholar]