Abstract
North American optometry and ophthalmology faculty members and vision science librarians were surveyed online (14% response rate) about teaching evidence-based practice (EBP). Similar to studies of other health care programs, all five EBP steps (Ask, Acquire, Appraise, Apply, Assess) were taught to varying degrees. Optometry and ophthalmology EBP educators may want to place further emphasis on (1) the Apply and Assess steps, (2) faculty- and student-generated questions and self-assessment in clinical settings, (3) online teaching strategies, (4) programmatic integration of EBP learning objectives, and (5) collaboration between faculty members and librarians.
INTRODUCTION
Evidence-based medicine was first developed for physicians in the early 1990s 1. Since then, other health care providers have integrated this concept into their disciplines, and the phrase has broadened to evidence-based practice (EBP) 2–6.
Optometrists and ophthalmologists provide eye and vision care. Optometry educators are increasingly recognizing the importance of EBP in optometric education. North American EBP competencies for optometrists can be found in accreditation standards and educational competency statements 7, 8. Curricula are changing to incorporate EBP knowledge and skill development at both the undergraduate and continuing education levels 2, 9–11. Articles in the optometric literature address EBP's nature, value, and role in the profession as well as barriers to and deficits in its current use in the profession 2. EBP literature in ophthalmology education predates that in optometric education 12–15. As a result, ophthalmology may be further ahead than optometry in adopting and integrating EBP into its educational programs.
EBP is normally taught by both faculty members and librarians, although their differing expertise likely informs what, who, and how they teach 16–23. Surveying ophthalmology and optometry programs can provide useful insights for vision science librarians and faculty members who are interested in introducing EBP training into or enhancing it in their programs. The results should allow comparison of vision-related EBP education in optometry and ophthalmology with that employed by other health care professions. This study is the first to survey both librarians and faculty members regarding educational practices with respect to EBP education.
METHODS
Measures
After obtaining institutional ethics clearance, online surveys (Appendix A and Appendix B, online only) were developed, tested, and administered in 2011 for two North American cohorts: (1) optometry and ophthalmology faculty members and (2) vision science librarians. The survey content was developed based on a literature review 16, 17, 19, 20, 24–29, a previous unpublished survey by the first author, the knowledge and experience of the research team members, and consultations with several vision science librarians. The surveys were pilot-tested using a group of local health sciences or medical librarians and optometry faculty members.
The surveys contained twenty-seven Likert-scale or open-text survey questions that addressed teaching EBP. Questions sought information on respondents' demographics, teaching or learning methods and assessment, and institutional characteristics. Likert-scale questions were either four points (e.g., frequency) or six points (e.g., agreement). Twenty-four of the survey questions were the same for the faculty members and librarians (although six questions contained slight wording differences to fit the unique roles and responsibilities of the respondent groups). A chi-squared test was used to examine differences between cohorts that might emerge because of their differing expertise. In many academic institutions, librarians are faculty members, but for the purpose of this study, the authors separated the two groups to gain a functional perspective.
Sample
Potential survey participants were identified through purposeful and snowball sampling using Internet searches, email queries, and word of mouth. Canadian and US optometry and ophthalmology faculty members involved in teaching EBP were identified by searching the websites of schools and colleges offering doctor of optometry programs and medical schools and facilities offering ophthalmology programs. Vision science librarians were identified through the Association of Vision Science Librarians (AVSL) and/or through websites of institutions offering optometry or medical programs. The websites of 20 optometry and 103 ophthalmology schools or programs were searched, and potential respondents were identified for each site.
Potential respondents were sent a preliminary email to ascertain if they taught EBP and if not, were requested to pass the email on to the appropriate person. Potential participants were asked to respond to the preliminary email. The email addresses of all initial potential participants who did not respond to the preliminary email plus the email addresses of suggested participants formed the final survey participant list. The email addresses of potential participants who indicated that they did not teach EBP or did not want to participate were taken off the list. This list was forwarded to the University of Waterloo Survey Research Centre, who implemented the online survey. Participants were told the study wanted to explore if and how optometry and ophthalmology programs taught their students the EBP process.
RESULTS
Survey response
Seven of the 460 distributed surveys were returned due to email address errors or extended out-of-office notices, leaving a potential sample of 453 people (328 faculty members and 125 librarians). Sixty-six surveys were returned with 4 being significantly incomplete (2 faculty members and 2 librarians), leaving 62 complete surveys (14% response rate). The respondents included 34 faculty members (11%) and 28 librarians (24%).
Fifty (81%) of the respondents indicated they taught at least some of the 5-step EBP process as defined by Straus and Prasad (Ask, Acquire, Appraise, Apply, Assess) 30, 31, and 12 (19%) indicated they did not teach any of the steps. This article reports on the 50 completed surveys from respondents who taught the EBP process (24 faculty members and 26 librarians). The survey was not designed to determine whether the respondents came from the same or differing institutions.
Faculty member respondents were primarily optometrists (75%) who provided clinical care (88%) and had more than 16 years of teaching experience and taught in optometry programs (79%). Most librarian respondents had a master of library and information science degree (92%), more than 13 years of teaching experience, and taught in more than 1 type of health care program (92%).
Respondents obtained EBP training via 1 or more methods, including through self-directed learning (86%), from courses outside a degree program (50%), in a graduate degree program (20%), or in their professional training (18%).
Generally, 80% of respondents worked in professional programs affiliated with a college or university. Sixty-six percent of the respondents described their libraries as multidisciplinary health sciences or discipline-specific.
Instruction of evidence-based practice (EPB) steps
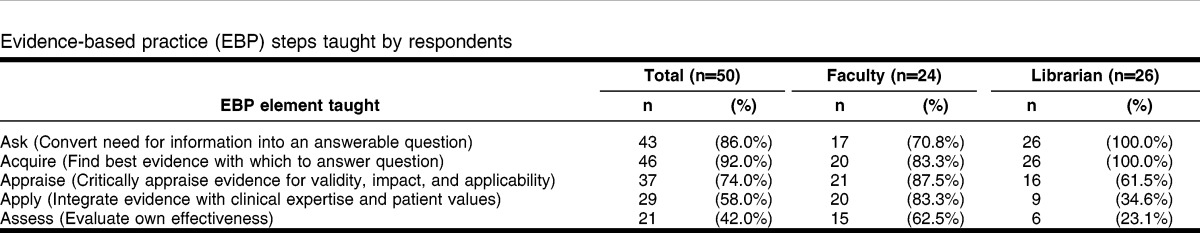
All 5 steps of the EBP process were taught but to varying degrees among the respondent cohorts (Table 1), based on frequency-based responses. All librarian respondents taught Ask and Acquire, with decreasing proportions teaching Appraise, Apply, and Assess. Overall, Assess was taught by the smallest proportion of all respondents (42%). Faculty member respondents were more likely to teach the steps Apply (83% versus 35%) and Assess (63% versus 23%) than librarians (χ2≤8.0, P≤0.01).
Table 1.
Evidence-based practice (EBP) steps taught by respondents
Learner type and duration taught
The librarian and faculty member respondents taught a variety of learners. Using frequency-based responses, in decreasing order, the top 4 types of learners receiving EBP instruction were other faculty members (52%), optometry students (50%), medical students (48%), and non-ophthalmology residents or fellows (46%). Twenty four percent of respondents taught ophthalmology residents. The statistically significant instructor-cohort differences among respondents were that optometry students were more likely to receive instruction from faculty members (88%) than librarians (15%) (χ2 = 29.6, P<0.01), while medical students, non-ophthalmology residents or fellows, and graduate students were more likely to receive instruction from librarians (77%, 77%, 58%, respectively) than faculty members (17%, 13%, 21%, respectively) (χ2≤7.06, P≤0.01). The number of hours of EBP instruction, using a yes/no response, was 10 hours or less (31%), 11–20 hours (27%), and more than 20 hours (43%).
Settings
The 50 respondents taught EBP in a variety of settings. Using frequency-based responses, the top 4 EBP teaching settings were: small classrooms (64%), seminar rooms (60%), offices (54%), and clinics (52%). The significant instructor-cohort setting differences were that faculty members (79%) were more likely than librarians (27%) to teach in clinics (χ2 = 13.7, P = 0.01), while librarians (77%) were more likely than faculty members (8%) to teach in computer labs (χ2 = 26.4, P = 0.01).
Teaching methods
Most often, respondents employed lectures (72%); individualized instruction (68%); print or electronic tutorials, handouts, and guides (64%); small group case-based learning (62%); and live demonstrations of tools, resources, and processes (62%), according to frequency-based responses. There were several significant instructor-cohort method differences. Relative to faculty members, librarians were more likely to employ tutorials, handouts, and guides (print or online information modules, exercise sheets, or collections of resources around a specific topic) (89% versus 38%); live demonstrations (92% versus 29%); and practical sessions (hands-on computer lab exercises) (77% versus 33%) (χ2≥0.62, P≤0.01). Faculty members were significantly more likely than librarians to utilize case discussions (63% versus 23%) and to teach in the course of patient care (67% versus 12%) (χ2≥8.0, P≤0.01).
Teaching tools and aids
Respondents used anytime (asynchronous) more frequently than live (synchronous) web-based tools with the most prevalent tools being course management software (54%), online tutorials and modules (44%), and email (30%). The top 4 teaching aids developed were EBP resource lists (50%), search strategy worksheets (42%), question development sheets (38%), and EBP subject guides (34%). Librarian respondents were more likely than faculty members to use search strategy worksheets (63% versus 21%) and subject specific guides (54% versus 13%) (χ2≥8.49, P≤0.01).
Assessment strategies
To assess student learning, the 4 most commonly reported assessment strategies using frequency-based responses were final exam questions (54%), EBP worksheets (42%), critical appraisal exercises (42%), and case reports (40%). Significantly more faculty members than librarians reported using case study reports (58% versus 23%) and observations of the students' the clinical practices (63% versus 12%) (χ2≥6.5, P≤0.01). Librarians (58%) were more likely than faculty members (17%) to use library research assignments involving self-assessment of literature searching skills (χ2 = 9.0, P≤0.01). Of interest is that only 26% of all respondents used a critically appraised topic (CAT) report as an assessment method. A CAT is a 1-page summary of a patient-stimulated EBP learning effort that includes the clinical question, the bottom line, an evidence summary, comments, and citations.
Collaboration and teaching support
Frequency-based questions were used to ascertain collaboration levels and activities. More respondents collaborated with faculty members (72%) than librarians (56%), with significantly more librarians (77%) than faculty members (33%) collaborating with librarians (χ2 = 9.62, P = 0.01). When asked about engaging with colleagues to teach EBP, significantly more librarians than faculty members collaborated by discussing teaching strategies and assessment outside class (73% versus 25%), teaching a section of the course alone (77% versus 21%), or co-teaching in the classroom (62% versus 8%), laboratory or clinic (23% versus 0) (χ2≥6.3, P≤0.01). These options were not mutually exclusive. In response to a yes/no question, both faculty members and librarians used campus teaching support mechanisms, such as instructional technologies services (25%) and teaching support services (10%), in a limited way.
Integration of EBP into program
EBP training was embedded into the learning environment through a variety of strategies. According to frequency-based questions, the 4 most common avenues employed for all respondents were in courses (80%), via individual consults (80%), by continuing education courses (54%), and as program milestones or other form of graduation requirements (34%). None of the cohort differences were statistically significant.
The level of EBP integration into programmatic curricula varied. Indicators of EBP integration most often took the form of EBP-related learning objectives in courses (68%). Less often, EBP was a programmatic milestone requirement (40%); incorporated into the programmatic mission, goals, and objectives (40%); or part of clinic experience learning objectives (36%).
DISCUSSION
The findings of this study suggest that training for optometry students and ophthalmology residents should address all five steps of the EBP process. Ophthalmology residents may actually receive relatively more EBP training than optometry students, because studies indicate that EBP training normally starts during undergraduate medical school 16, 22, 23. Librarian respondents were most likely to report teaching the earlier EBP steps, while faculty members reported teaching across the five steps. This result might reflect the need for clinician-based activity to inform teaching and assessment especially in the Apply step. Librarian involvement in these types of activities would likely be limited. The final Assess step was taught the least frequently by both groups; its absence may reflect time constraints, a lack of teaching methods, or the assumption that it occurs automatically. Unfortunately, in the absence of this final step, students might not learn how to review and refine their EBP process, making them less efficient at and reflective about the process.
The respondents in this survey reported similar approaches to educators in other disciplines in terms of teaching settings 16, 19, 20, 24, 27 and the use of multiple teaching methods 19, 24, 27. Lectures, with or without interactive methods 16, 19, 20, 24, 27, 32–34, were most commonly used; however, this method has been shown not to change practice behavior in postgraduate education 35. The majority of respondents also used individual consultation, although less frequently. This approach has been shown to be a good way to introduce, reinforce, and master EBP skills 24, 32, 36, 37. Results suggest that individual consultation needs to be introduced or expanded if the integration of EBP into clinical practice for optometry and ophthalmology is to be achieved.
Over half the respondents taught EBP in clinical settings, and this finding aligns with the growing recognition that EBP instruction should be clinically based, so that the questions coming out of clinical interactions are asked and answered 24. Answering patient-specific questions arising during clinical care has been shown to increase knowledge and change clinical decisions among residents 24 as well as medical students 38. Expanding teaching of EBP in the clinical setting should be encouraged. Only 27% of librarian respondents taught in clinics. Other studies note that the presence and participation of librarians in rounds and morning reports helps learners with developing questions, developing search strategies, and finding clinical evidence 17, 39–41. Utilizing librarians in clinical settings is an opportunity that could be expanded by optometry and ophthalmology programs.
While the use of CAT reports is well documented in the literature as a method to help novices learn to ask a clinical question, review the literature, and summarize the best available research evidence on the subject 18, 30, 42–44, only just over one-quarter of respondents employed CATs as an instructional method. This assessment strategy was not one of the top four strategies used by respondents. More optometry and ophthalmology educators may want to explore the use of CATs, because patient-focused, self-directed, and personalized learning in the clinical setting should lead to a greater chance of having the EBP behaviors integrated into future practice 5, 24, 26, 36, 38, 42. Beyond the use of course management systems, other web-based teaching tools such as online tutorials or modules and videos could be explored by educators. These web-based tools 16, 31, 33, 42, 45–49 were used by few respondents but can be as effective as standard lectures for gaining knowledge and changing attitudes 50.
The most common assessment strategies used were final exam questions, EBP worksheets, critical appraisal exercises, and case reports. This is consistent with other disciplines 18–20, 27, 42–44, 47, 51, 52. Assessment is often organized around a series of assignments and reports that focus on the various steps of EBP 20, 21, 25, 26. Active application of the process (the “shows how” level of Miller's pyramid) 53 has been assessed using clinical vignettes and standardized patients 27, 54–56 and is being used by some respondents. This is another avenue of exploration or expansion because of its value for assessing the Apply and Assess steps.
Integration of EBP into curriculum and programmatic goals or competencies occurred primarily at the level of the individual course rather than the program. While other health care professions talk about the integration of EBP into the curriculum, the degree of formal integration is unreported and requires further study.
Limitations of this study include the small number of respondents, particularly among faculty members and more specifically ophthalmology faculty members. Therefore, the findings might not reflect EBP instruction in North American optometry schools and ophthalmology programs. In institutions where librarians are faculty members, their status as faculty members rather than professional staff members might influence what EBP steps are taught and assessed. Another limitation is that our sampling technique might have incorrectly identified or missed individuals who were responsible for EBP education.
CONCLUSION
The findings of this survey-based study provide the first indication of EBP educational practices used by faculty members and librarians training optometry students and ophthalmology residents in North America. Optometry and ophthalmology educators may want to increase their emphasis on the Apply and Assess EBP steps to ensure that application and improvement of the EBP process are ingrained in students before they become practitioners. Some of these educators may want to enhance their use of: (1) faculty- and student-generated questions and self-assessment in the clinical setting, (2) online teaching strategies with assistance from teaching support services on campus, (3) greater integration of EBP learning objectives at a programmatic level, and (4) increasing collaboration.
Electronic Content
Acknowledgments
Erin Harvey, Statistics and Actuarial Science, University of Waterloo, provided statistical analysis.
Footnotes
Supplemental Appendix A and Appendix B are available with the online version of this journal.
REFERENCES
- 1.Evidence-Based Medicine Working Group (November 1992) Evidence-based medicine: a new approach to teaching the practice of medicine. JAMA. 1992 Nov 4;268(17):2420–5. doi: 10.1001/jama.1992.03490170092032. [DOI] [PubMed] [Google Scholar]
- 2.Anderton PJ. Implementation of evidence-based practice in optometry. Clin Exp Optom. 2007 Jul;90(4):238–43. doi: 10.1111/j.1444-0938.2007.00153.x. [DOI] [PubMed] [Google Scholar]
- 3.Hoge MA, Tondora J, Stuart GW. Training in evidence-based practice. Psychiatr Clin North Am. 2003 Dec;26(4):851–65. doi: 10.1016/s0193-953x(03)00066-2. [DOI] [PubMed] [Google Scholar]
- 4.Moch SD, Cronje RJ, Branson J. Part 1. undergraduate nursing evidence-based practice education: envisioning the role of students. J Prof Nurs. 2010 Jan;26(1):5–13. doi: 10.1016/j.profnurs.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 5.Thomas A, Saroyan A, Dauphinee WD. Evidence-based practice: a review of theoretical assumptions and effectiveness of teaching and assessment interventions in health professions. Adv Health Sci Educ Theory Pract. 2011 May;16:253–76. doi: 10.1007/s10459-010-9251-6. [DOI] [PubMed] [Google Scholar]
- 6.Kronenfeld M, Stephenson PL, Nail-Chiwetalu B, Tweed EM, Sauers EL, McLeod TCV, Guo R, Trahan H, Alpi KM, Hill B, Sherwill-Navarro P, Allen MP, Stephenson PL, Hartman LM, Burnham J, Fell D, Kronenfeld M, Pavlick R, MacNaughton EW, Nail-Chiwetalu B, Ratner NB. Review for librarians of evidence-based practice in nursing and the allied health professions in the United States. J Med Lib Assoc. 2007 Oct;95(4):394–407. doi: 10.3163/1536-5050.95.4.394. DOI: http://dx.doi.org/10.3163/1536-5050.95.4.394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Association of Schools and Colleges of Optometry. Attributes of students graduating from schools and colleges of optometry [Internet] The Association; 2011 [cited 5 Nov 2012]. < http://www.opted.org/files/2011_AttributesReport.pdf>. [Google Scholar]
- 8.Competence Committee of Canadian Examiners in Optometry. Competency-based performance standards for the Canadian standard assessment in optometry [Internet] The Association; 2005 [cited 15 Dec 2012]. < http://docs.ceo-eco.org/dm/cache/documents/CSAOdocs/CBPS_Document.pdf>. [Google Scholar]
- 9.Adams AJ. The role of research, evidence and education in optometry: a perspective. Clin Exp Optom. 2007 Jul;90(4):232–7. doi: 10.1111/j.1444-0938.2007.00149.x. [DOI] [PubMed] [Google Scholar]
- 10.Adams AJ. Whither goes evidence-based optometry. Optom Vis Sci. 2008 Jul;85(4):219–20. doi: 10.1097/OPX.0b013e3181719a7a. [DOI] [PubMed] [Google Scholar]
- 11.Keller PR. The evidence in evidence-based practice. why the confusion. Clin Exp Optom. 2012 Nov;95(6):618–20. doi: 10.1111/j.1444-0938.2012.00804.x. [DOI] [PubMed] [Google Scholar]
- 12.Burnier MN. The evaluation of scientific information in medicine. Can J Ophthalmol. 2004 Feb;39(1):5–6, 9. doi: 10.1016/s0008-4182(04)80046-2. [DOI] [PubMed] [Google Scholar]
- 13.Coleman AL. Applying evidence-based medicine in ophthalmic practice. Am J Ophthalmol. 2002 Oct;134(4):599–601. doi: 10.1016/s0002-9394(02)01652-5. [DOI] [PubMed] [Google Scholar]
- 14.Lee AG, Boldt HC, Golnik KC, Arnold AC, Oetting TA, Beaver HA, Olson RJ, Carter K. Using the journal club to teach and assess competence in practice-based learning and improvement: a literature review and recommendation for implementation. Surv Ophthalmol. 2005 Nov–Dec;50(6):542–8. doi: 10.1016/j.survophthal.2005.08.002. [DOI] [PubMed] [Google Scholar]
- 15.Wormald R. Bridging the gap to evidence-based eye care. Community Eye Health. 2004 Oct;17(51):40–1. [PMC free article] [PubMed] [Google Scholar]
- 16.Lynn VA. Foundations of database searching: integrating evidence-based medicine into the medical curriculum. Med Ref Serv Q. 2010 Apr;29(2):121–31. doi: 10.1080/02763861003723176. [DOI] [PubMed] [Google Scholar]
- 17.Hatala R, Keitz SA, Wilson MC, Guyatt G. Beyond journal clubs: moving toward an integrated evidence-based medicine curriculum. J Gen Intern Med. 2006 May;21(5):538–41. doi: 10.1111/j.1525-1497.2006.00445.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Haines SJ, Nicholas JS. Teaching evidence-based medicine to surgical subspecialty residents. J Am Coll Surg. 2003 Aug;197(2):285–9. doi: 10.1016/S1072-7515(03)00114-5. [DOI] [PubMed] [Google Scholar]
- 19.Finkel ML, Brown HA, Gerber LM, Supino PG. Teaching evidence-based medicine to medical students. Med Teach. 2003Mar;25(2):202–4. doi: 10.1080/0142159031000092634. [DOI] [PubMed] [Google Scholar]
- 20.Burns HK, Foley SM. Building a foundation for an evidence-based approach to practice: teaching basic concepts to undergraduate freshman students. J Prof Nurs. 2005 Nov–Dec;21(6):351–7. doi: 10.1016/j.profnurs.2005.10.001. [DOI] [PubMed] [Google Scholar]
- 21.Shlonsky A, Stern SB. Reflections on the teaching of evidence-based practice. Res Soc Work Pract. 2007 Sep;17(5):603–11. [Google Scholar]
- 22.MacEachern M, Townsend W, Young K, Rana G. Librarian integration in a four-year medical school curriculum: a timeline. Med Ref Serv Q. 2012;31(1):105–14. doi: 10.1080/02763869.2012.641856. [DOI] [PubMed] [Google Scholar]
- 23.Maggio LA, Tannery NH, Chen HC, ten Cate O, O'Brien B. Evidence-based medicine training in undergraduate medical education: a review and critique of the literature published 2006–2011. Acad Med. 2013 Jul;88(7):1022–8. doi: 10.1097/ACM.0b013e3182951959. [DOI] [PubMed] [Google Scholar]
- 24.Schilling LM, Steiner JF, Lundahl K, Anderson RJ. Residents' patient-specific clinical questions: opportunities for evidence-based learning. Acad Med. 2005 Jan;80(1):51–6. doi: 10.1097/00001888-200501000-00013. [DOI] [PubMed] [Google Scholar]
- 25.Brancato VC. An innovative clinical practicum to teach evidence-based practice. Nurse Educ. 2006 Sep–Oct;31(5):195–9. doi: 10.1097/00006223-200609000-00004. [DOI] [PubMed] [Google Scholar]
- 26.Cayley WE., Jr Evidence-based medicine medical students: introducing EBM in a primary care rotation. Wis Med J. 2005 Apr;104(3):34–7. [PubMed] [Google Scholar]
- 27.Holloway R, Nesbit K, Bordley D, Noyes K. Teaching and evaluating first and second year medical students' practice of evidence-based medicine. Med Educ. 2004 Aug;38(8):868–78. doi: 10.1111/j.1365-2929.2004.01817.x. [DOI] [PubMed] [Google Scholar]
- 28.Jack BA, Roberts KA, Wilson RW. Developing the skills to implement evidence based practice—a joint initiative between education and clinical practice. Nurse Educ Pract. 2003 Jun;3(2):112–8. doi: 10.1016/S1471-5953(02)00108-7. [DOI] [PubMed] [Google Scholar]
- 29.Fineout-Overholt E, Johnston L. Teaching EBP: implementation of evidence: moving from evidence to action. Worldviews Evid Based Nurs. 2006;3(4):194–200. doi: 10.1111/j.1741-6787.2006.00070.x. [DOI] [PubMed] [Google Scholar]
- 30.Straus SE, Glaziou P, Richardson SW, Haynes RB. Evidence based medicine: how to practice and teach it. 4th ed. Toronto, ON, Canada: Churchill Livingstone; 2011. [Google Scholar]
- 31.Prasad K. Fundamentals of evidence-based medicine: basic concepts in easy language. New Delhi, India: Meeta Publishers; 2007. [Google Scholar]
- 32.Bookstaver PB, Rudisill CN, Rebecca Bickley A, McAbee C, Miller AD, Piro CC, Schulz R. An evidence-based medicine elective course to improve student performance in advanced pharmacy practice experiences. Am J Pharm Educ. 2011 Feb;75(1):9. doi: 10.5688/ajpe7519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pitkala KH, Mantyranta T, Strandberg TE, Makela M, Vanhanen H, Varonen H. Evidence-based medicine—how to teach critical scientific thinking to medical undergraduate students. Med Teach. 2000 Jan;22(1):22–6. [Google Scholar]
- 34.Potomkova J, Mihal V, Zapletalova J, Subova D. Integration of evidence-based practice in bedside teaching paediatrics supported by e-learning. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2010 Mar;154(1):83–7. doi: 10.5507/bp.2010.014. [DOI] [PubMed] [Google Scholar]
- 35.Coomarasamy A, Khan K. What is the evidence that postgraduate teaching in evidence based medicine changes anything? a systematic review. BMJ. 2004 Oct 30;329(7473):1017–9. doi: 10.1136/bmj.329.7473.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bradt P, Moyer V. How to teach evidence-based medicine. Clin Perinatol. 2003 Jun;30(2):419–33. doi: 10.1016/s0095-5108(03)00019-8. [DOI] [PubMed] [Google Scholar]
- 37.Elnicki DM, Kolarik R, Bardella I. Third-year medical students' perceptions of effective teaching behaviors in a multidisciplinary ambulatory clerkship. Acad Med. 2003 Aug;78(8):815–9. doi: 10.1097/00001888-200308000-00016. [DOI] [PubMed] [Google Scholar]
- 38.McGinn T, Seltz M, Korenstein D. A method for real-time, evidence-based general medical attending rounds. Acad Med. 2002 Nov;77(11):1150–2. doi: 10.1097/00001888-200211000-00019. [DOI] [PubMed] [Google Scholar]
- 39.Duggar DC, Christopher KA, FitzGerald L, Wood RT. Does providing onsite immediate access to electronic resources using a laptop and wireless network improve resident participation in morning report. J Hosp Lib. 2008 Nov;8(4):411–7. [Google Scholar]
- 40.Skhal KJ. A full revolution: offering 360 degree library services to clinical clerkship students. Med Ref Serv Q. 2008 Fall;27(3):249–59. doi: 10.1080/02763860802198788. [DOI] [PubMed] [Google Scholar]
- 41.Weaver D. Enhancing resident morning report with “daily learning packages.”. Med Ref Serv Q. 2011;30(4):402–10. doi: 10.1080/02763869.2011.609077. [DOI] [PubMed] [Google Scholar]
- 42.Aronoff SC, Evans B, Fleece D, Lyons P, Kaplan L, Rojas R. Integrating evidence based medicine into undergraduate medical education: combining online instruction with clinical clerkships. Teach Learn Med. 2010 Jul;22(3):219–23. doi: 10.1080/10401334.2010.488460. [DOI] [PubMed] [Google Scholar]
- 43.Burneo JG, Jenkins ME. Teaching evidence-based clinical practice to neurology and neurosurgery residents. Clin Neurol Neurosurg. 2007 Jun;109(5):418–21. doi: 10.1016/j.clineuro.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 44.Rugh JD, Hendricson WD, Glass BJ, Hatch JP, Deahl ST, 2nd, Guest G, Ongkiko R, Gureckis K, Jones AA, Rose WF, Gakunga P, Stark D, Steffensen B. Teaching evidence-based practice at the University of Texas Health Science Center at San Antonio dental school. Tex Dent J. 2011 Feb;128(2):187–90. [PubMed] [Google Scholar]
- 45.Jeffery KM, Maggio L, Blanchard M. Making generic tutorials content specific: recycling evidence-based practice (EBP) tutorials for two disciplines. Med Ref Serv Q. 2009 Spring;28(1):1–9. doi: 10.1080/02763860802615872. [DOI] [PubMed] [Google Scholar]
- 46.Bradley P, Oterholt C, Herrin J, Nordheim L, Bjorndal A. Comparison of directed and self-directed learning in evidence-based medicine: a randomised controlled trial. Med Educ. 2005 Oct;39(10):1027–35. doi: 10.1111/j.1365-2929.2005.02268.x. [DOI] [PubMed] [Google Scholar]
- 47.Cook DA, Dupras DM. Teaching on the web: automated online instruction and assessment of residents in an acute care clinic. Med Teach. 2004;26(7):599–603. doi: 10.1080/01421590400004932. [DOI] [PubMed] [Google Scholar]
- 48.Kaneshiro KN, Emmett TW, London SK, Ralston RK, Richwine MW, Skopelja EN, Brahmi FA, Whipple E. Use of an audience response system in an evidence-based mini-curriculum. Med Ref Serv Q. 2008 Fall;27(3):284–301. doi: 10.1080/02763860802198861. [DOI] [PubMed] [Google Scholar]
- 49.Genes N, Parekh S. Bringing journal club to the bedside in the form of a critical appraisal blog. J Emerg Med. 2010 Oct;39(4):504–5. doi: 10.1016/j.jemermed.2008.10.011. [DOI] [PubMed] [Google Scholar]
- 50.Davis J, Crabb S, Rogers E, Zamora J, Khan K. Computer-based teaching is as good as face to face lecture-based teaching of evidence based medicine: a randomized controlled trial. Med Teach. 2008;30(3):302–7. doi: 10.1080/01421590701784349. [DOI] [PubMed] [Google Scholar]
- 51.Mottonen M, Tapanainen P, Nuutinen M, Rantala H, Vainionpaa L, Uhari M. Teaching evidence-based medicine using literature for problem solving. Med Teach. 2001 Jan;23(1):90–1. doi: 10.1080/01421590150214645. [DOI] [PubMed] [Google Scholar]
- 52.Temple C. L. F, Ross DC. Acquisition of evidence-based surgery skills in plastic surgery residency training. J Surg Educ. 2011 May–Jun;68(3):167–71. doi: 10.1016/j.jsurg.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 53.Miller G. The assessment of clinical skills competence performance. Acad Med. 1990 Sep;65(9):S63–S67. doi: 10.1097/00001888-199009000-00045. [DOI] [PubMed] [Google Scholar]
- 54.Rutten GMJ, Harting J, Rutten STJ, Bekkering GE, Kremers SPJ. Measuring physiotherapists' guideline adherence by means of clinical vignettes: a validation study. J Eval Clin Pract. 2006 Oct;12(5):491–500. doi: 10.1111/j.1365-2753.2006.00699.x. [DOI] [PubMed] [Google Scholar]
- 55.Shah R, Edgar D, Evans BJW. Measuring clinical practice. Ophthalmic Physiol Opt. 2007 Mar;27(2):113–25. doi: 10.1111/j.1475-1313.2006.00481.x. [DOI] [PubMed] [Google Scholar]
- 56.Waxman KT. The development of evidence-based clinical simulation scenarios: guidelines for nurse educators. J Nurs Educ. 2010 Jan;49(1)):29–35. doi: 10.3928/01484834-20090916-07. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


