Abstract
Patients with invasive giant prolactinoma suffer from a constellation of symptoms including headache, blurred vision, lethargy, and sexual dysfunction. Cabergoline, a potent dopamine agonist, is a known medication prescribed for the treatment of invasive giant prolactinoma. Here, we report a case of invasive giant prolactinoma in a 52-year-old Saudi male with dramatic response to cabergoline treatment clinically, biochemically, and radiologically.
Keywords: pituitary tumor, giant prolactinoma, cabergoline
Introduction
Pituitary adenomas are benign tumors of the pituitary gland, with lactotroph adenoma (prolactinoma) being the major subtype, accounting for 44% of known cases.1 Microprolactinomas are less than 1 cm in diameter, and tend to occur more in females, where macroadenomas measures more than 1 cm with male predominance. On the other hand, invasive giant prolactinoma is subset of macroadenoma, defined as tumors >4 cm, >1000 ng/mL prolactin levels and with clinical symptoms of hyperprolactinemia or mass effect.1 Giant prolactinoma is a rare tumor with male preponderance.2,3 Massively extended prolactinoma has been reported in a case of a 49-year-old male, whose tumor was locally aggressive extending through the inferior petrosal sinus to emerge within the internal jugular vein, with serum prolactin level above 100,000 mU/L and was only partially responsive to bromocriptine treatment.4
With regards to cabergoline, it is a long acting dopamine receptor agonist with high affinity for D2 receptors. Dopamine agonists reduce the size of prolactinomas by inducing a reduction in cell volume (via an early inhibition of secretory mechanism, and a late inhibition of gene transcription and PRL synthesis), as well as causing perivascular fibrosis and partial cell necrosis.5 It has been demonstrated that cabergoline is safe and effective for treatment of invasive giant prolactinomas, even when administered in relatively high doses for longer duration.6 Adverse effects associated with high doses of dopamine agonists are uncommon but includes cerebrospinal fluid leakage,7 chiasmal herniation, and pituitary apoplexy.8 In view of the potent agonist effect of cabergoline against 5HT2B receptor, it has been associated with mitral valve insufficiency in high doses prescribed for Parkinson’s disease.9 In this report, we describe the case of a 52-year-old Saudi male with giant prolactinoma and its dramatic response to dopamine agonist (cabergoline).
Case Report
A 52-year-old Saudi male presented to the emergency department with complains of headache and decreased bilateral vision for 10 days. He previously sought medical advice in Jordan, where he fully investigated and was found to have high serum prolactin levels and a radiographically documented large sellar mass. He was offered surgery but refused and instead came to seek for second opinion. History revealed generalized fatigability, lethargy, decrease libido, and constipation for 5 years. He also noted weight gain despite having undergone bariatric surgery more than 10 years ago.
He reported no history of gynecomastia, galactorrhea, hearing loss, or nasal discharge. No history of seizure disorder, personality changes, or altered levels of consciousness. Medical family history was unremarkable.
On physical examination, patient was conscious, coherent, and ambulatory. He was morbidly obese (body mass index = 45 kg/m2). Vital signs were stable. Thyroid examination was normal. Perimetry examination showed bilateral superior quadrantanopia with full range of extra ocular muscle movements. Systemic examination was unremarkable. Laboratory investigations showed hyperprolactinemia at (prolactin = 125,347.0 mIU/L; normal value = 86–324 mIU/L). Other pituitary work-ups showed central hypogonadism, secondary hypothyroidism, and adrenal insufficiency. Magnetic resonance imaging (MRI) was done and revealed a giant intra-sellar solid mass with intra-tumoral cyctic degeneration invading the sphenoid and bilateral cavernous sinuses with clivus approaching the posterior nasal spaces and the right pterygoid plate. Compression effect over the optic chiasm was also noted.
The patient was eventually diagnosed with invasive giant prolactinoma with apoplexy. He was started on cabergoline 0.25 mg twice weekly, thyroxin 50 mcg daily, testosterone 250 mg IM injection every 3 weeks, hydrocortisone 10 mg a.m. and 5 mg p.m., and vitamin D 50,000 IU weekly for 8 weeks then monthly. After 3 days post-treatment, prolactin levels dropped to 48,986.0 (86–324 mIU/L), with subsequent improvements in vision and headache. The patient was discharged and was advised to continue on the same regimen. Follow-up was done 5 months later and revealed decreased prolactin levels (9983 mIU/L) as compared to previous results. ACTH stimulation test was normal. Hydrocortisone was discontinued. Perimetry test showed normal results. Table 1 shows the effect of cabergoline at a dose of 0.25 mg twice weekly over 5 months (September 2013), with the latest results including MRI images before and after treatment (Fig. 1) as well as after 13 months (Fig. 2). However, this has resulted in CSF rhinorrhoea.
Table 1.
Laboratory work-ups before and after cabergoline treatment.
| HORMONE | INITIAL (MAY 2013) | SEPTEMBER 2013 | FEBRUARY 2014 |
|---|---|---|---|
| Prolactin (mIU/L) | 125347 (86–324) | 9983 | 11635 |
| FSH (IU//L) | 2.3 IU/L | 2.8 | 3.0 |
| LH (IU/L) | 3.1 lU/L | 3.3 | 6.6 |
| TSH (mIU/L) | 0.41 (0.270–4.200) | 1.5 | 0.43 |
| Total Testosterone | 3.55 (6.70–25.70) | 12.3 | 16.8 |
| FT4 (pmol/L) | 10.3 (12.0–22.0) | 13.2 on treatment | 13.7 |
| FT3 (pmol/L) | 2.4 (3.1–6.8) | 2.7 | 3.7 |
| ACTH (pmol/L) | 2.2 (1.6–13.9) | 6.8 | 7.2 |
| Cortisol (nmol/L) | 27 nmol/l | 141–546–671 (SST) normal | 46–679 |
Note: Data presented as actual values (normal values).
Figure 1.
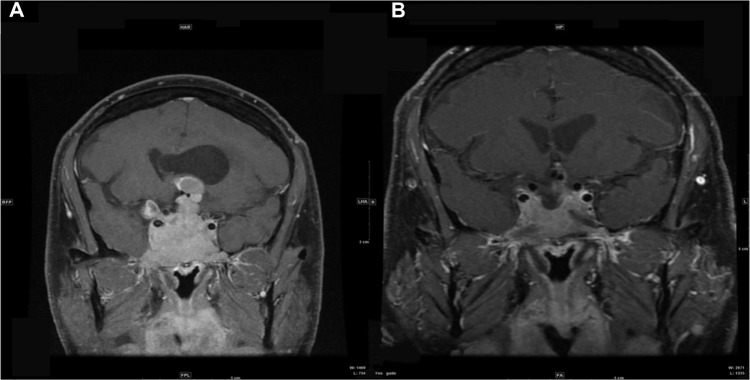
MRI pituitary before (A) and 6 months after (B) cabergoline treatment.
Figure 2.
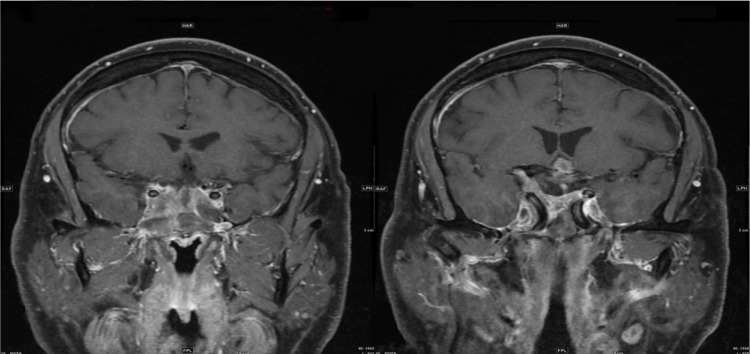
MRI 13 months after treatment.
Discussion
Treatment of invasive giant prolactinoma using cabergoline has been observed to provide excellent outcomes in treating an extensive prolactinoma with locoregional spread and visual field compromise, starting with 0.25 mg/week and increased to 1 mg/week, with serum prolactin decreasing to 192 ng/mL at 8 months from an initial level of 1592 ng/mL.10 Other cases reported that treatment with cabergoline for 18 months markedly reduced tumor size with normalization of adrenal function and visual field improvement.11
In our case, significant improvements (as shown in Table 1 and MRI images) were observed from an initial dose of 0.25 mg of cabergoline twice weekly. Also, patient showed dramatic improvement in visual field symptoms as early as day 3 from cabergoline treatment. He was maintained on 100 mcg of thyroxin with good clinical and biochecmial response as well as testosterone 250 mg injection every 3 weeks with remarkable improvement in his sexual function. CSF rhinorrhea was treated with reduction the cabergoline dose to once weekly then once every other week in order to allow tumor re-expansion and stop the leak with some success that followed by endoscopic nasal surgery to repair the fistula using muscle grafts, which was successful in sealing the leak.
Conclusion
In summary, our case illustrates the efficacy of cabergoline in treating invasive giant prolactinoma and reversing patient’s symptoms. Moreover, it is considered to be a safe medication as it causes no significant adverse effects apart from CSF rhinorrhea, which was managed successfully.
Footnotes
Author Contributions
Conceived and designed the experiments: SA, MHA. Analyzed the data: SA, MHA. Wrote the first draft of the manuscript: SA, MHA. Contributed to the writing of the manuscript: SA, MHA. Agree with manuscript results and conclusions: SA, MHA. Jointly developed the structure and arguments for the paper: SA, MHA. Made critical revisions and approved final version: SA, MHA. Both authors reviewed and approved of the final manuscript.
ACADEMIC EDITOR: Athavale Nandkishor, Associate Editor
FUNDING: Authors disclose no funding sources.
COMPETING INTERESTS: Authors disclose no potential conflicts of interest.
This paper was subject to independent, expert peer review by a minimum of two blind peer reviewers. All editorial decisions were made by the independent academic editor. All authors have provided signed confirmation of their compliance with ethical and legal obligations including (but not limited to) use of any copyrighted material, compliance with ICMJE authorship and competing interests disclosure guidelines and, where applicable, compliance with legal and ethical guidelines on human and animal research participants.
REFERENCES
- 1.Siddiqui A, Chew N, Miszkiel K. Unusual orbital invasion by a giant prolactinoma. Br J Radiol. 2008;81:259–62. doi: 10.1259/bjr/98771490. [DOI] [PubMed] [Google Scholar]
- 2.Shrivastava RK, Arginteanu MS, King WA, Post KD. Giant prolactinomas: clinical management and long-term follow up. J Neurosurg. 2002;97:299–306. doi: 10.3171/jns.2002.97.2.0299. [DOI] [PubMed] [Google Scholar]
- 3.Corsello SM, Ubertini G, Altomare M, et al. Giant prolactinomas in men: efficacy of cabergoline treatment. Clin Endocrinol. 2003;58:662–70. doi: 10.1046/j.1365-2265.2003.01770.x. [DOI] [PubMed] [Google Scholar]
- 4.Davis JRE, Sheppard MC, Heath DA. Giant invasive prolactinoma: a case report and review of nine further cases. (New Series).Q J Med. 1990;74(275):227–38. [PubMed] [Google Scholar]
- 5.Bevan JS, Webster J, Burke CW, Scanlon MF. Dopamine agonists and pituitary tumor shrinkage. Endocr Rev. 1992;13:220–40. doi: 10.1210/edrv-13-2-220. [DOI] [PubMed] [Google Scholar]
- 6.Clayton RN, Webb J, Heath DA, Dunn PJS, Rolfe EB, Hockley AD. Dramatic and rapid shrinkage of a massive invasive prolactinoma with bromocriptine: a case report. Clin Endocrinol. 1985;22:573–81. doi: 10.1111/j.1365-2265.1985.tb02992.x. [DOI] [PubMed] [Google Scholar]
- 7.Shimon I, Benbassat C, Hadani M. Effectiveness of long-term cabergoline treatment for giant prolactinoma: study of 12 men. Eur J Endocrinol. 2007;156:225–31. doi: 10.1530/EJE-06-0646. [DOI] [PubMed] [Google Scholar]
- 8.Leong KS, Foy PM, Swift AC, Atkin SL, Hadden DR, MacFarlane IA. CSF rhinorrhoea following treatment with dopamine agonists for massive invasive prolactinomas. Clin Endocrinol. 2002;52:43–9. doi: 10.1046/j.1365-2265.2000.00901.x. [DOI] [PubMed] [Google Scholar]
- 9.Pinero A, Marcos-Alberca P, Fortes J. Cabergoline-related severe restrictive mitral regurgitation. New Engl J Med. 1997;337:581–8. doi: 10.1056/NEJM200511033531822. [DOI] [PubMed] [Google Scholar]
- 10.Dutta D, Ghosh S, Mukhopadhyay S, Chowdhury S. Rapid reduction with cystic transformation of invasive giant prolactinoma following short-term low dose cabergoline. Indian J Endocrinol Metab. 2012;16(6):1048–51. doi: 10.4103/2230-8210.103041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rahmanian M, Meybodi HA, Larijani B, Mohajeri-Tehran M. Giant prolactinoma: case report and review of literature. J Diabetes Metab Disord. 2013;12:3. doi: 10.1186/2251-6581-12-3. [DOI] [PMC free article] [PubMed] [Google Scholar]


