Abstract
Background
The benefit of statin use after acute ST-segment elevation myocardial infarction (STEMI) has been well established, however, the influence of the timing of statin administration has not been elucidated. The objective of this study focused on early clinical outcomes after percutaneous coronary intervention (PCI).
Methods
This analysis of the Korea Working Group on Myocardial Infarction registry (KorMI) study included 3,584 STEMI patients (mean age, 63 ± 13 years; male, 2,684, 74.9%) undergoing PCI from January 2008 to June 2009. Rates of major adverse cardiac events (MACE: all-cause death, recurrent MI, and target lesion revascularization) were compared among patients grouped according to statin therapy timing: I, both during and after hospitalization (n = 2,653, 74%); II, only during hospitalization (n = 309, 8.6%); III, only after discharge (n = 157, 4.4%); and IV, no statin therapy (n = 465, 13%). Mean follow-up duration was 234 ± 113 days.
Results
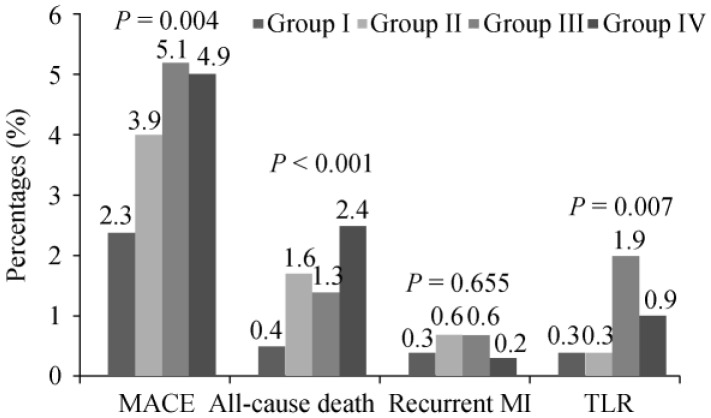
Multivariate factors of statin use during hospitalization included prior statin use, multiple diseased vessels, final thrombolysis in myocardial infarction flow grade III, and low-density lipoprotein cholesterol level. At 6-month follow-up, groups III and IV had the highest MACE rates (2.3%, 3.9%, 5.1%, and 4.9% for groups I-IV, respectively, P = 0.004). After adjusting for confounders, groups II-IV had a higher MACE risk than group I [hazard ratio (HR): 3.20, 95% confidence interval (95%CI): 1.31–7.86, P = 0.011; HR: 3.84, 95%CI: 1.47–10.02, P = 0.006; and HR: 3.17, 95%CI: 1.59–6.40, P = 0.001; respectively].
Conclusions
This study, based on the national registry database, shows early and continuous statin therapy improvs early outcomes of STEMI patients after PCI in real-world clinical practice.
Keywords: Statins, Acute myocardial infarction, Treatment outcome
1. Introduction
Statins, the 3-hydroxy-3-methylglutaryl coenzyme A (HMG Co-A) reductase inhibitors, reduce the risk of recurrent coronary events and improve survival in patients after acute myocardial infarction (AMI).[1] Statin use in pa-tients undergoing percutaneous coronary intervention (PCI) appears beneficial in terms of early and intermediate-term mortality;[2] statin therapy initiated at discharge significantly reduces 1-year mortality after primary angioplasty for ST-segment elevation myocardial infarction (STEMI);[3] and statin discontinuation in first-AMI survivors is associated with higher all-cause mortality when compared with non-users.[4] However, lipid-lowering medications remain underutilized in real-world practice, and the impact of timing patterns of statin use on survival after AMI is unknown. This study assessed whether timing of statin use, i.e., during hospitalization and/or after discharge or no use, influences early outcomes after acute STEMI, particularly in patients undergoing PCI.
2. Methods
2.1. Study population
This study is based on a database collected by the national registry study of the Korea Working Group on Myocardial Infarction (KorMI). KorMI is a prospective, multi-center registry study designed to characterize the clinical characteristics and prognosis of AMI in Korean patients. All 52 cardiology centers in Korea were invited to participate in the KorMI study, with support from the Korean Society of Cardiology in January 2008. At participating sites, consecutive patients admitted with AMI were asked to register as part of this study. The study protocol was reviewed and approved by the institutional review board at each participating center. Detailed data were obtained on the demographics of patients, treatment in the emergency room, catheterization findings, and the clinical outcome during their hospital stay. Data were collected at each institution; a study coordinator or doctor entered the data into a password-protected, web-based, computerized database program provided by the KorMI committee.
A total of 7,732 patients with AMI were enrolled in the KorMI registry from January 2008 to June 2009. Of these patients, 3,584 patients were included in this study using the following criteria: newly diagnosed STEMI; hospital admission within 7 days of symptom onset; age > 20 years (mean age: 63 ± 13 years); all patients underwent PCI; and patients experiencing in-hospital mortality were excluded (n = 347). Patients were stratified into four groups according to the mode of statin usage and regardless of statin dosage or class as follows: Group I, statin therapy both during hospitalization and after discharge (n = 2,653, 74%); Group II, only during hospitalization (n = 309, 8.6%); Group III, only after discharge (n = 157, 4.4%); and Group IV, no statin therapy (n = 465, 13%).
2.2. Study outcome
The outcome of this study was a 6-month composite of major adverse cardiac events (MACE) including all-cause death, recurrent MI, and target lesion revascularization (TLR). MI was defined as typical ischemic chest pain, ST-segment or T-wave abnormalities with a creatinine kinase-MB level ≥ 2 times the reference value. TLR was defined as surgical or percutaneous re-intervention driven by significant (> 50%) luminal narrowing within a stent or within 5 mm proximal or distal to a stent in the presence of angina symptoms, or objective evidence of ischemia. Only the first MACE was considered as the MACE of a patient.
2.3. Statistical analysis
Data were analyzed with SPSS for Windows, release 17.0 (SPSS Inc., Chicago, IL, USA). All descriptive data are expressed as mean ± SD. Comparisons of continuous and categorical variables between groups were analyzed by t test (2-sided) and Chi-square test, respectively. P < 0.05 were considered statistically significant. Long-term mortality was estimated using Kaplan-Meier techniques, and the impact of statin therapy as a time-dependent covariate on patient outcome was evaluated with the Cox proportional hazards regression model. Univariate Cox regression analysis was performed to evaluate the influence of variables on 6-month MACE. Multivariate logistic regression analysis was used to adjust for all MACE-associated variables with a P < 0.20 on univariate analysis.
3. Results
Mean follow-up duration was 234 ± 113 days. Among baseline characteristics, age, diabetes mellitus (DM), total cholesterol (TC), low-density lipoprotein cholesterol (LDL-C), prior PCI, Killip class > 1, left ventricular ejection fraction (LVEF) < 45%, systolic and diastolic blood pressure (BP), and prior statin use were significantly different among the four groups (Table 1). Statin use during hospitalization was influenced by prior statin use, disease severity, and several laboratory findings. Angiographic findings were not significantly different among the four groups, except for the rate of achievement of final Thrombolysis In the Myocardial Infarction (TIMI) flow grade III (Table 2). Table 3 shows differences in medication use among the four groups during hospitalization and after discharge. Statins were less frequently dispensed in more severely diseased patients not taking other medications. On multivariate logistic regression analysis, statin use during hospitalization appeared to be influenced by several factors, including prior statin use, multiple diseased vessels, TIMI flow grade III after PCI, and LDL-C level (Table 4).
Table 1. Baseline characteristics.
| Variable | Pattern of statin therapy use |
P | |||
| Group I | Group II | Group III | Group IV | ||
| (n = 2,653) | (n = 309) | (n = 157) | (n = 465) | ||
| Age, yrs | 62 ± 13 | 63 ± 12 | 64 ± 14 | 66 ± 13 | < 0.001 |
| Male | 2,010 (76) | 213 (69) | 119 (76) | 342 (74) | 0.071 |
| Risk factor (%) | |||||
| Hypertension | 1,194 (46) | 149 (49) | 77 (50) | 204 (45) | 0.439 |
| Diabetes mellitus | 599 (23) | 92 (30) | 30 (20) | 123 (27) | 0.007 |
| Current smoker | 1,260 (49) | 129 (44) | 76 (50) | 195 (44) | 0.048 |
| Lipid profile | |||||
| TC, mg/dL | 188 ± 44 | 178 ± 46 | 181 ± 45 | 168 ± 41 | < 0.001 |
| Triglycerides, mg/dL | 133 ± 102 | 133 ± 98 | 133 ± 135 | 116 ± 108 | 0.016 |
| HDL-C, mg/dL | 44 ± 13 | 44 ± 17 | 45 ± 17 | 43 ± 13 | 0.124 |
| LDL-C, mg/dL | 121 ± 38 | 112 ± 39 | 115 ± 34 | 103 ± 35 | < 0.001 |
| Prior PCI | 100 (4) | 23 (7) | 6 (4) | 18 (4) | 0.022 |
| Prior angina pectoris | 94 (4) | 10 (3) | 3 (2) | 10 (2) | 0.335 |
| Prior CABG | 6 (0.2) | 0 | 0 | 1 (0.2) | 0.789 |
| Prior stroke | 153 (6) | 22 (7) | 3 (2) | 27 (6) | 0.147 |
| CHF NYHA class > 2 | 16 (0.6) | 4 (1.3) | 2 (1.3) | 5 (1.1) | 0.358 |
| Killip class > 1 | 744 (31) | 100 (35) | 37 (26) | 172 (41) | < 0.001 |
| LVEF < 45% | 363 (15) | 43 (19) | 18 (13) | 86 (23) | 0.002 |
| Systolic BP | 129 ± 29 | 125 ± 31 | 124 ± 25 | 119 ± 31 | < 0.001 |
| Diastolic BP | 79 ± 18 | 77 ± 19 | 76 ± 17 | 73 ± 20 | < 0.001 |
| Prior statin use | 154 (6) | 18 (6) | 3 (2) | 15 (3) | 0.028 |
Results are presented as mean ± SD or n (%). Patterns of statin therapy use: Group I, statin therapy both during hospitalization and after discharge; Group II, only during hospitalization; Group III, only after discharge; and Group IV, no statin therapy. BP: blood pressure; CABG: coronary artery bypass graft; CHF: congestive heart failure; HDL-C: high-density lipoprotein-cholesterol; LDL-C: low-density lipoprotein-cholesterol; LVEF: left ventricular ejection fraction; NYHA: New York Heart Association; PCI: percutaneous coronary intervention; TC: total cholesterol.
Table 2. Angiographic findings.
| Variable | Pattern of statin therapy use |
P | |||
| Group I | Group II | Group III | Group IV | ||
| (n = 2,653) | (n = 309) | (n = 157) | (n = 465) | ||
| > 1 Diseased vessel | 1,363 (53) | 168 (56) | 71 (48) | 224 (53) | 0.511 |
| Infarct related artery | 0.412 | ||||
| Left anterior descending | 1,341 (52) | 155 (52) | 76 (52) | 199 (47) | |
| Left circumflex | 271 (11) | 33 (11) | 22 (15) | 49 (12) | |
| Right coronary | 934 (36) | 107 (36) | 47 (32) | 167 (39) | |
| Left main | 30 (1) | 5 (2) | 2 (1) | 9 (2) | |
| Lesion type C | 1,065 (48) | 128 (51) | 58 (46) | 147 (43) | 0.132 |
| Stent length > 30 mm | 554 (23) | 50 (20) | 26 (20) | 84 (22) | 0.644 |
| Stent diameter ≤ 3.0 mm | 523 (22) | 48 (19) | 27 (21) | 72 (19) | 0.57 |
| Final TIMI 3 flow | 2,171 (92) | 223 (86) | 123 (92) | 308 (83) | < 0.001 |
Results are presented as n (%). Patterns of statin therapy use: Group I, statin therapy both during hospitalization and after discharge; Group II, only during hospitalization; Group III, only after discharge; and Group IV, no statin therapy. TIMI: Thrombolysis In Myocardial Infarction.
Table 3. Medications during hospitalization and after discharge.
| Variable | Pattern of statin therapy use |
P | |||
| Group I | Group II | Group III | Group IV | ||
| (n = 2,653) | (n = 309) | (n = 157) | (n = 465) | ||
| During hospitalization | |||||
| Aspirin | 2,641 (100) | 307 (99) | 143 (99) | 424 (98) | 0.001 |
| Clopidogrel | 2,631 (100) | 306 (99) | 142 (99) | 423 (98) | 0.061 |
| Beta-blocker | 2,183 (82) | 248 (80) | 93 (59) | 313 (67) | < 0.001 |
| ACEI | 1,916 (72) | 196 (63) | 79 (50) | 262 (56) | < 0.001 |
| ARB | 486 (18) | 63 (22) | 31 (20) | 85 (18) | 0.526 |
| After discharge | |||||
| Aspirin | 2,682 (99) | 183 (61) | 156 (99) | 371 (80) | < 0.001 |
| Clopidogrel | 2,362 (89) | 170 (55) | 143 (91) | 330 (71) | < 0.001 |
| Beta-blocker | 2,155 (81) | 145 (47) | 119 (76) | 280 (60) | < 0.001 |
| ACEI | 1,780 (67) | 115 (37) | 86 (55) | 226 (49) | < 0.001 |
Results are presented as n (%). Patterns of statin therapy use: Group I, statin therapy both during hospitalization and after discharge; Group II, only during hospitalization; Group III, only after discharge; and Group IV, no statin therapy. ACEI: angiotensin-converting-enzyme inhibitors; ARB: angiotensin II receptor blockers.
Table 4. The factors associated with statin use during hospitalization (Multivariate analysis).
| Variable | Exp (β) | 95% CI |
P | |
| Lower | Upper | |||
| Prior statin use | 0.052 | 0.007 | 0.408 | 0.005 |
| > 1 diseased vessel | 1.524 | 1.110 | 2.092 | 0.009 |
| Lesion type C | 1.345 | 0.972 | 1.861 | 0.074 |
| Final TIMI 3 flow | 0.392 | 0.232 | 0.664 | < 0.001 |
| LDL-C (mg/dL) | 1.013 | 1.003 | 1.022 | 0.010 |
Age, sex, history of diabetes mellitus and hypertension, current smoking, lipid profile, LVEF, prior statin use, > 1 diseased vessel, Lesion type C, stent length and stent diameter, Final TIMI 3 flow were used as covariates in the model. LDL-C: low-density lipoprotein-cholesterol; LVEF: left ventricular ejection fraction; TIMI: thrombolysis in myocardial infarction.
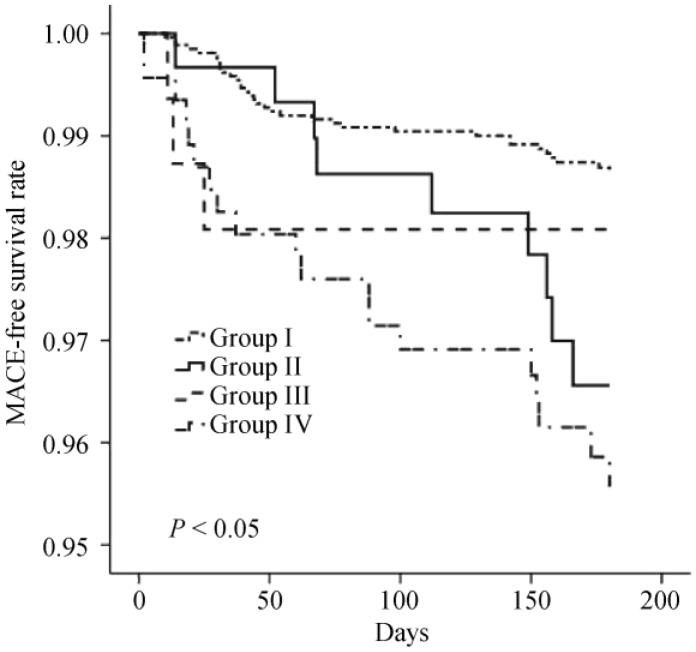
At 6-month follow-up, Groups III and IV had higher MACE rates (2.3%, 3.9%, 5.1%, and 4.9% for Groups I-IV, respectively, P = 0.004), (Figure 1). Patients on statin medication during and/or after hospitalization had better clinical outcomes than statin-naïve patients at the six month follow-up (Figure 2). After adjusting for other MACE-associated factors, Cox-proportional hazard analysis revealed significantly increased MACE risks for Groups II-IV as compared with Group I [II: hazard ratio (HR): 3.20, 95% confidence interval (95% CI): 1.31–7.86, P = 0.011; III: HR: 3.84, 95% CI: 1.47–10.02, P = 0.006; and IV: HR: 3.17, 95% CI: 1.59–6.40, P = 0.001; respectively] (Table 5). Also, relative risk of MACE development in patients who discontinued statin at discharge was similar to that of patients who had not used statins (3.20 and 3.17 in Groups II and IV, respectively).
Figure 1. Clinical outcomes at 6-month follow up.
Patterns of statin therapy use: Group I, statin therapy both during hospitalization and after discharge; Group II, only during hospitalization; Group III, only after discharge; and Group IV, no statin therapy. MACE: major adverse cardiac events; MI: myocardial infarction; TLR: target lesion revascularization.
Figure 2. MACE-free survival curves according to pattern of statin use.
Patterns of statin therapy use: Group I, statin therapy both during hospitalization and after discharge; Group II, only during hospitalization; Group III, only after discharge; and Group IV, no statin therapy. MACE: major adverse cardiac events.
Table 5. Prognostic value of the pattern of statin therapy use for total adverse events at 6-month follow up.
| Grouping | Hazard ratio (95% CI) |
|||
| Unadjusted | P | Adjusted | P | |
| Group I | 1 | 1 | ||
| Group II | 3.19 (1.21–8.42) | 0.019 | 3.2 (1.31–7.86) | 0.011 |
| Group III | 4.77 (1.71–13.28) | 0.003 | 3.84 (1.47–10.02) | 0.006 |
| Group IV | 3.71 (1.71–8.0) | 0.001 | 3.17 (1.59–6.40) | 0.001 |
Adjusted for age, gender, Killip class > I, blood pressures, left ventricular ejection fraction < 45%, and co-morbidities (previous myocardial infarction, angina pectoris, heart failure, hypertension, diabetes, smoking history, increased lipid levels, stroke, and peripheral vascular disease), medications before and after discharge, reperfusion therapies (primary percutaneous coronary intervention, thrombolytic therapy, and overall percutaneous coronary intervention), angiographic findings (multivessel disease, target vessel, lesion type C, and stent insertion), and complications. Patterns of statin therapy use: Group I, statin therapy both during hospitalization and after discharge; Group II, only during hospitalization; Group III, only after discharge; and Group IV, no statin therapy.
4. Discussion
It is known that statin therapy has early benefit on vascular cellular responses through pleiotropic mechanisms beyond its LDL-C lowering effects[5] including endothelial function improvement,[6] antithrombotic effects,[7] mobilization of bone marrow progenitor cells,[8] cardiac remodeling prevention,[9] antiarrhythmic effects,[10] and reduction of ischemia-reperfusion injury.[11] In a previous study performed by Celik, et al.[12] using TIMI frame count method, prior high-dose statin use at least six months before PCI in AMI patients had beneficial effects on coronary blood flow, possibly by improving microvascular dysfunction. In a randomized clinical trial, Stenestrand, et al.[13] showed that early initiation of statin treatment in AMI patients is associated with reduced 1-year mortality. In our study, early and prolonged statin use (Group I) was associated with significantly lower 6-month MACE rate than that of other groups with statin use only during hospitalization or after discharge, or without statin use (2.3% vs. 4.9%). Despite the compelling scientific and clinical trial evidence that early initiation of statins reduces mortality in patients after AMI,[13],[14] this life-saving therapy continues to be underutilized in real-world practice. In the present study, statin non-users or those discontinuing statin use also tended not to use or discontinue cardioprotective drugs, such as aspirin, clopidogrel, β-blockers, and ACEI. One could posit that the latter observation might be explained by the differences in baseline characteristics between groups, including older age, higher Killip class, high rate of ejection fraction below 45% and low systolic, diastolic BP. However, the relative large percentage (17.4%) of STEMI patients not on statins during their hospitalization and of those who discontinued statin at discharge (8.6%) cannot be fully explained by these baseline differences. Because statins are relatively safe drugs with relatively low rates of complications,[15] there do not seem to be potential contraindications or life-threatening conditions that would justify avoiding or discontinuing statins in all groups. The paradoxical underuse of statins among the highest-risk patients might be explained by the so called “risk-treatment mismatch”, i.e., a progressive decline in medication prescription with increased baseline cardiovascular risk and future probability of death in the real world. In other words, clinicians seem to avoid prescribing medications to patients perceived to have a short life expectancy.[16],[17] However, another main cause of non-use or discontinuation of statins is likely the insurance system. Hoogerbrugge, et al.[18] previously identified unfavorable insurance status as the most relevant nonclinical factor associated with less use of costly services, such as treatment with statins. In our study, TC and LDL-C levels were significantly different between Group I and other groups. Because the Korean insurance system allows use of statins only based on TC and LDL-C levels, low levels of these parameters are likely responsible for statin non-use or discontinuation.
Daskalopoulou, et al.[4] in their large, observational, population-based study reported that statin discontinuation in first-AMI survivors was associated with higher all-cause mortality when compared with non-users. In the latter study, patients received 90 days of statin after AMI, and statin discontinuation was evaluated at 90 days after AMI. De Luca, et al.[19] reported that statin therapy initiation at discharge was associated with a significant reduction in 1-year mortality after primary angioplasty for STEMI. However, the impact of timing patterns of statin use during hospitalization and after discharge after AMI remained unclear. Moreover, comparison between statin-naïve patients and those who followed several patterns of statin use had not been studied well. In our study, after adjusting for compounding factors (Table 5), relative risk of MACE development in patients who discontinued statins at discharge was higher than that in patients continuing statin use after discharge (HR of 3.2 for Group II relative to Group I). In addition, relative risk of MACE was similar between the statin-discontinuation group and the statin-naïve group (HR 3.20 in Group II vs. 3.17 in Group IV). Non-use of statin therapy after AMI appears to be associated with higher mortality than any other pattern of statin administration (Figure 1). This finding is consistent with those of clinical studies showing that the beneficial effects of statins are rapidly lost and often transiently reversed when statins are acutely discontinued.[20] In a previous study using data from the National Registry of Myocardial Infarction 4, patients who continued or newly started statin treatment had a decreased risk of in-hospital mortality; however, discontinuation of statins was associated with a higher risk of in-hospital mortality (compared with no statin use).[21] In patients with non-ST-segment elevation AMI discontinuation during the first 24 h was associated with a 2-fold risk when compared with continuation of statin treatment.[22] On the other hand, data from the Treating New Targets study suggested that short-term discontinuation of statin therapy in patients with stable cardiac conditions may not substantially increase the risk of acute coronary syndromes.[23] However, neither of these studies showed the relative long-term (six months) impact of statin discontinuation at discharge in unstable post-STEMI patients treated with PCI compared with various modes of statin use.
Our study underscores the clinical importance of statin therapy during hospitalization and after discharge in STEMI patients, in particular, those who underwent PCI. The discontinuation of statins in post-STEMI patients was associated with a high rate of MACE. This result appears to be driven not by the lipid-lowering effects of statins, but by reversal of statin pleiotropic effects after their discontinuation. The reasons for not using or discontinuing statins in the real world appear secondary to risk-treatment mismatch, and in large part, to the inappropriate health insurance system. Therefore, physicians need to recognize the benefit of statin use and should be very careful with statin discontinuation at patient discharge, especially in post-STEMI patients. Also remedial action of the health insurance system, now only focused on TC and LDL-C, is needed.
Our study has several limitations. This study is limited by the large differences in baseline clinical characteristics among groups studied (such as age, previous medical history, lipid profiles, Killip class, LVEF, BP, rates of prior statin use), the lack of differentiation of statin properties according to class (lipophilic or hydrophilic) or dosage (high vs. low), its non-randomized, non-controlled design, and the inability to adjust for all confounders. Also, we could not confirm whether patients who were prescribed statins at hospital discharge continued using them throughout long-term follow-up. Because this study was based on registry data and data collection was voluntary at each participating center, the follow-up data were partially incomplete.
In conclusion, this study suggested that early and continuous use of statins improved early outcomes in acute STEMI survivors who underwent PCI in real-world clinical practice. This study was valuable since it was based on the national registry database, including a large sample size, multicenter design, and prospective data collection.
References
- 1.Prevention of cardiovascular events and death with pravastatin in patients with coronary heart disease and a broad range of initial cholesterol levels. The Long-Term Intervention with Pravastatin in Ischaemic Disease (LIPID) Study Group. N Engl J Med. 1998;339:1349–1357. doi: 10.1056/NEJM199811053391902. [DOI] [PubMed] [Google Scholar]
- 2.Krumholz HM, Anderson JL, Bachelder BL, et al. ACC/AHA 2008 performance measures for adults with ST-elevation and non-ST-elevation myocardial infarction: a report of the American College of Cardiology/American Heart Association Task Force on Performance Measures (Writing Committee to develop performance measures for ST-elevation and non-ST-elevation myocardial infarction): developed in collaboration with the American Academy of Family Physicians and the American College of Emergency Physicians: endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation, Society for Cardiovascular Angiography and Interventions, and Society of Hospital Medicine. Circulation. 2008;118:2596–2648. doi: 10.1161/CIRCULATIONAHA.108.191099. [DOI] [PubMed] [Google Scholar]
- 3.De Luca G, Suryapranata H, Zijlstra F, et al. Statin therapy and mortality in patients with ST-segment elevation myocardial infarction treated with primary angioplasty. Neth Heart J. 2004;12:271–278. [PMC free article] [PubMed] [Google Scholar]
- 4.Daskalopoulou SS, Delaney JA, Filion KB, et al. Discontinuation of statin therapy following an acute myocardial infarction: a population-based study. Eur Heart J. 2008;29:2083–2091. doi: 10.1093/eurheartj/ehn346. [DOI] [PubMed] [Google Scholar]
- 5.Kadota S, Matsuda M, Izuhara M, et al. Long-term effects of early statin therapy for patients with acute myocardial infarction treated with stent implantation. J Cardiol. 2008;51:171–178. doi: 10.1016/j.jjcc.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 6.Wassmann S, Faul A, Hennen B, et al. Rapid effect of 3-hydroxy-3-methylglutaryl coenzyme a reductase inhibition on coronary endothelial function. Circ Res. 2003;93:e98–e103. doi: 10.1161/01.RES.0000099503.13312.7B. [DOI] [PubMed] [Google Scholar]
- 7.Sanguigni V, Pignatelli P, Lenti L, et al. Short-term treatment with atorvastatin reduces platelet CD40 ligand and thrombin generation in hypercholesterolemic patients. Circulation. 2005;111:412–419. doi: 10.1161/01.CIR.0000153810.81187.7D. [DOI] [PubMed] [Google Scholar]
- 8.Suzuki G, Iyer V, Cimato T, et al. Pravastatin improves function in hibernating myocardium by mobilizing CD133+ and cKit+ bone marrow progenitor cells and promoting myocytes to reenter the growth phase of the cardiac cell cycle. Circ Res. 2009;104:255–264. doi: 10.1161/CIRCRESAHA.108.188730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liao Y, Zhao H, Ogai A, et al. Atorvastatin slows the progression of cardiac remodeling in mice with pressure overload and inhibits epidermal growth factor receptor activation. Hypertens Res. 2008;31:335–344. doi: 10.1291/hypres.31.335. [DOI] [PubMed] [Google Scholar]
- 10.Tang Q, Huang J, Qian H, et al. Antiarrhythmic effect of atorvastatin on autoimmune myocarditis is mediated by improving myocardial repolarization. Life Sci. 2007;80:601–608. doi: 10.1016/j.lfs.2006.11.045. [DOI] [PubMed] [Google Scholar]
- 11.Di Napoli P, Taccardi AA, Grilli A, et al. Chronic treatment with rosuvastatin modulates nitric oxide synthase expression and reduces ischemia-reperfusion injury in rat hearts. Cardiovasc Res. 2005;66:462–471. doi: 10.1016/j.cardiores.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 12.Celik T, Kursaklioglu H, Iyisoy A, et al. The effects of prior use of atorvastatin on coronary blood flow after primary percutaneous coronary intervention in patients presenting with acute myocardial infarction. Coron Artery Dis. 2005;16:321–326. doi: 10.1097/00019501-200508000-00010. [DOI] [PubMed] [Google Scholar]
- 13.Stenestrand U, Wallentin L. Early statin treatment following acute myocardial infarction and 1-year survival. JAMA. 2001;285:430–436. doi: 10.1001/jama.285.4.430. [DOI] [PubMed] [Google Scholar]
- 14.Lenderink T, Boersma E, Gitt AK, et al. Patients using statin treatment within 24 h after admission for ST-elevation acute coronary syndromes had lower mortality than non-users: a report from the first Euro Heart Survey on Acute Coronary Syndromes. Eur Heart J. 2006;27:1799–1804. doi: 10.1093/eurheartj/ehl125. [DOI] [PubMed] [Google Scholar]
- 15.Armitage J. The safety of statins in clinical practice. Lancet. 2007;370:1781–1790. doi: 10.1016/S0140-6736(07)60716-8. [DOI] [PubMed] [Google Scholar]
- 16.Lee DS, Tu JV, Juurlink DN, et al. Risk-treatment mismatch in the pharmacotherapy of heart failure. JAMA. 2005;294:1240–1247. doi: 10.1001/jama.294.10.1240. [DOI] [PubMed] [Google Scholar]
- 17.Ko DT, Mamdani M, Alter DA. Lipid-lowering therapy with statins in high-risk elderly patients: the treatment-risk paradox. JAMA. 2004;291:1864–1870. doi: 10.1001/jama.291.15.1864. [DOI] [PubMed] [Google Scholar]
- 18.Hoogerbrugge N, van Domburg R, van der Zwet E, et al. High fat intake in hyperlipidaemic patients is related to male gender, smoking, alcohol intake and obesity. Neth J Med. 2001;59:16–22. doi: 10.1016/s0300-2977(01)00119-x. [DOI] [PubMed] [Google Scholar]
- 19.De Luca G, Suryapranata H, Ottervanger JP, et al. Impact of statin therapy at discharge on 1-year mortality in patients with ST-segment elevation myocardial infarction treated with primary angioplasty. Atherosclerosis. 2006;189:186–192. doi: 10.1016/j.atherosclerosis.2005.11.028. [DOI] [PubMed] [Google Scholar]
- 20.Cubeddu LX, Seamon MJ. Statin withdrawal: clinical implications and molecular mechanisms. Pharmacotherapy. 2006;26:1288–1296. doi: 10.1592/phco.26.9.1288. [DOI] [PubMed] [Google Scholar]
- 21.Fonarow GC, Wright RS, Spencer FA, et al. Effect of statin use within the first 24 hours of admission for acute myocardial infarction on early morbidity and mortality. Am J Cardiol. 2005;96:611–616. doi: 10.1016/j.amjcard.2005.04.029. [DOI] [PubMed] [Google Scholar]
- 22.Spencer FA, Fonarow GC, Frederick PD, et al. Early withdrawal of statin therapy in patients with non-ST-segment elevation myocardial infarction: National Registry of Myocardial Infarction. Arch Intern Med. 2004;164:2162–2168. doi: 10.1001/archinte.164.19.2162. [DOI] [PubMed] [Google Scholar]
- 23.McGowan MP. There is no evidence for an increase in acute coronary syndromes after short-term abrupt discontinuation of statins in stable cardiac patients. Circulation. 2004;110:2333–2335. doi: 10.1161/01.CIR.0000145118.55201.15. [DOI] [PubMed] [Google Scholar]