Abstract
Purpose
Lower urinary tract symptoms are numerous, but the specific impact of each of these symptoms on the quality of life (QoL) has not been evaluated in community-dwelling men. An assessment of these symptoms and their effects on QoL was the focus of this study.
Methods
We performed a cross-sectional study with 373 men aged >50 years from a community setting. Patients completed the International Prostate Symptom Score questionnaire, which includes questions on each of the specific urinary symptoms and a question addressing health-related QoL that are graded from 0 to 5. We used the Pearson correlation test to assess the impact of each symptom on QoL.
Results
Nocturia (58.9%) was the most prevalent urinary symptom. The mean score was 0.9±1.4 for incomplete emptying, 1.0±1.5 for frequency, 0.9±1.3 for intermittency, 0.8±1.3 for urgency, 1.0±1.5 for weak stream, 0.5±1.0 for straining, and 2.0±1.6 for nocturia. Nocturia and frequency were the only symptoms associated with poorer QoL, with nocturia showing a stronger association.
Conclusions
Nocturia affects 50% of community dwelling men aged >50 years, and is the lower urinary tract symptom with the greatest negative impact on QoL.
Keywords: Epidemiology, Lower urinary tract symptoms, Nocturia, Prostatic hyperplasia, Quality of life
INTRODUCTION
Lower urinary tract symptoms (LUTS) comprise a spectrum of storage, voiding, and postmicturition issues that may be caused by different conditions. They are prevalent in elderly men, in whom the most common cause of such symptoms is benign prostatic hyperplasia (BPH). LUTS have a negative impact on the quality of life (QoL) of patients with BPH and other diseases [1,2,3]. However, little is known about their impact on the QoL in men from a community setting. Moreover, the specific impact of each urinary symptom on QoL is also unknown.
The most widely employed tool for the evaluation of LUTS is the International Prostate Symptom Score (IPSS), which is a questionnaire that includes seven questions, each evaluating a specific symptom, and a QoL question regarding satisfaction with urinary function. The IPSS has been used extensively for assessing LUTS in patients with BPH and other urological conditions [4]. The impact of each isolated symptom on QoL has not been well established, especially in patients without BPH and outside the clinical setting [5,6,7,8]. It is necessary to establish the impact of each specific symptom on QoL because patients with low total IPSS may have a severe, isolated symptom that negatively affects QoL [9]. Moreover, different treatment strategies may be developed based on the predominant symptoms in each patient. In this study, we evaluated the impact of each specific urinary symptom on QoL in community-dwelling men.
MATERIALS AND METHODS
After approval from both the Institutional Review Board and Ethics Committee, we performed a cross-sectional study including men aged >50 years from a community setting. To conduct the survey, three interviewers were trained to use the IPSS questionnaire that is composed of 7 questions on urinary symptoms, each graded from 0 to 5. Each question independently evaluates a specific lower urinary tract symptom, including sensation of incomplete emptying, urinary frequency, intermittency, urgency, weak stream, straining, and nocturia. Patients are considered to have a specific symptom when they have an IPSS≥2. The total IPSS can range from 0 to 35, with higher scores indicating greater symptom severity. In addition, there is an independent eighth question that assessed QoL as the health-related QoL (HRQoL), which allowed patients to rate themselves as delighted, pleased, mostly satisfied, mixed, mostly dissatisfied, unhappy, or terrible with respect to their urinary condition. The HRQoL score ranges from 0 to 6, with higher scores indicating poorer QoL. Validity of the IPSS has previously been demonstrated [4].
Participants were randomly selected from a large city in Brazil. Exclusion criteria were patients with a history of overactive bladder (OAB) syndrome, bladder pain syndrome, chronic pelvic pain syndrome, or any medical condition that could be directly related to LUTS (not only BPH). Patients with a history of radical prostatectomy, acute or uncompensated chronic diseases, alcoholism or drug addiction, or neurological and psychiatric diseases were also excluded. Among 624 men, 373 were eligible and agreed to participate. All participants signed an informed consent form after proper explanation and did not receive any financial incentive for their participation. Thereafter, they completed a health and socio-demographic questionnaire and the IPSS, including the question addressing HRQoL.
IBM SPSS ver. 20.0 (IBM Co., Armonk, NY, USA) was used to analyze the collected data. All data were descriptive and based on frequencies. Results were described as mean±standard deviation. The Pearson Correlation test was used to assess the correlation of each specific urinary symptom with the HRQoL score. Statistical significance was set at P<0.05.
RESULTS
The study group had a mean age of 61.1±8.8 years and a mean IPSS of 7.8±6.5. Demographic data are summarized in Table 1. Nocturia (58.9%) was the most prevalent urinary symptom, followed by frequency (35.9%), weak stream, incomplete emptying, intermittency, urgency, and straining (Fig. 1). The mean score for each isolated symptom was 0.9±1.4 for incomplete emptying, 1.0±1.5 for frequency, 0.9±1.3 for intermittency, 0.8±1.3 for urgency, 1.0±1.5 for weak stream, 0.5±1.0 for straining, and 2.0±1.6 for nocturia (Fig. 2).
Table 1.
Demographic data (n=373)
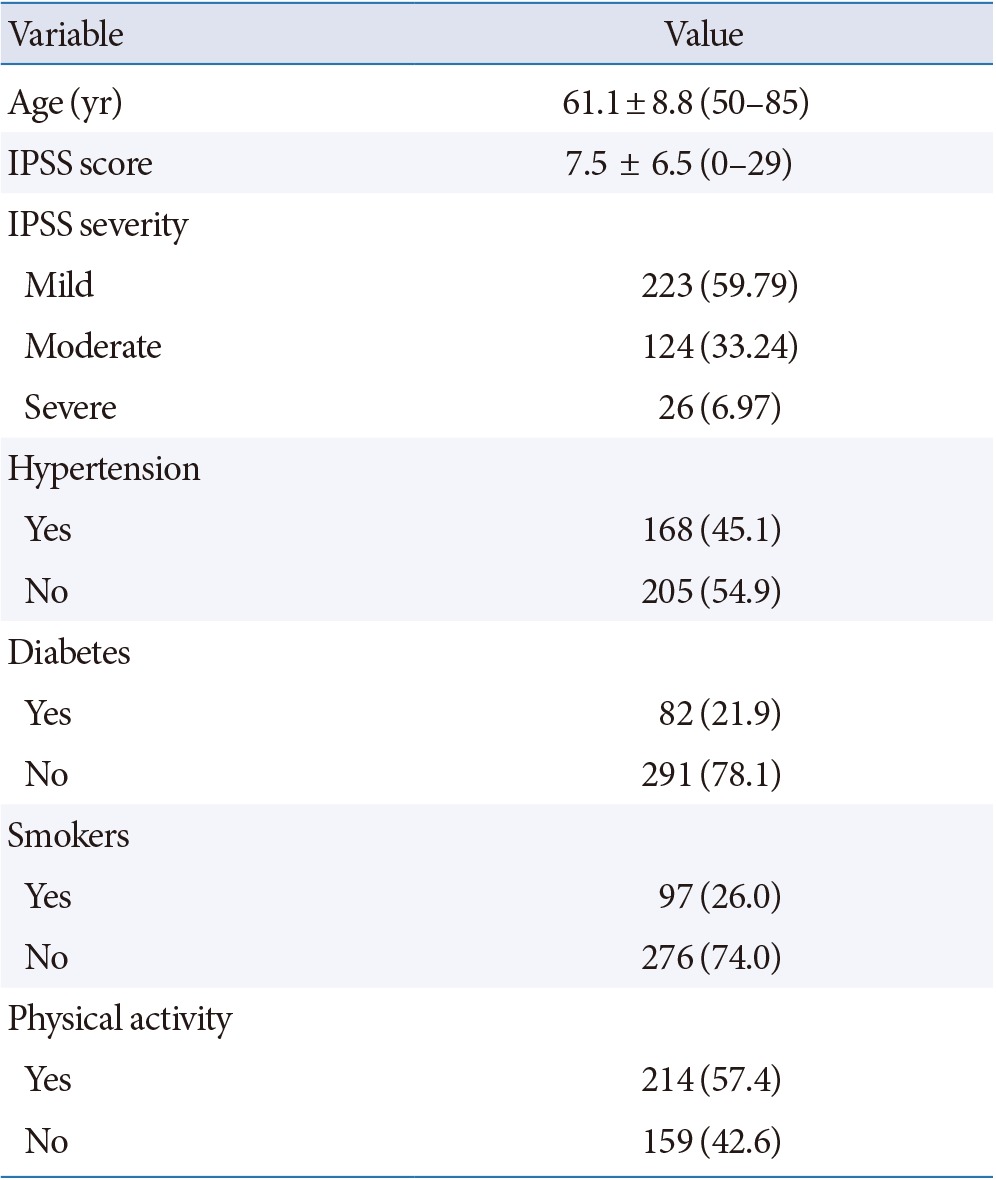
Values are presented as mean ± standard deviation (range) or number (%).
IPSS, International Prostate Symptom Score.
Fig. 1.
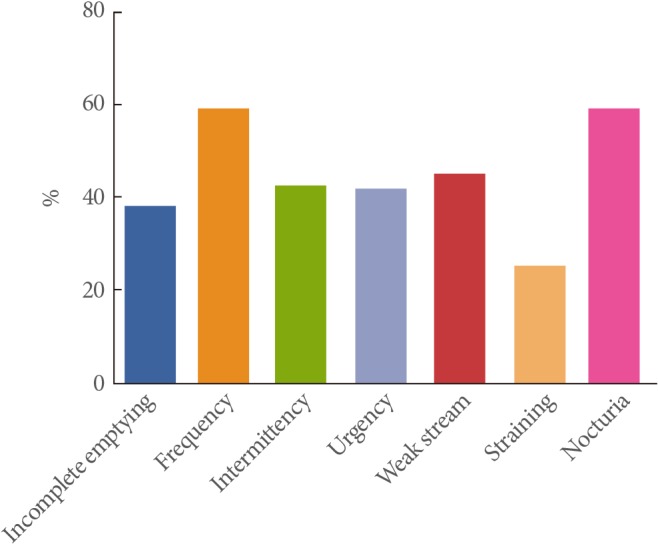
Prevalence rate of each lower urinary tract symptom.
Fig. 2.
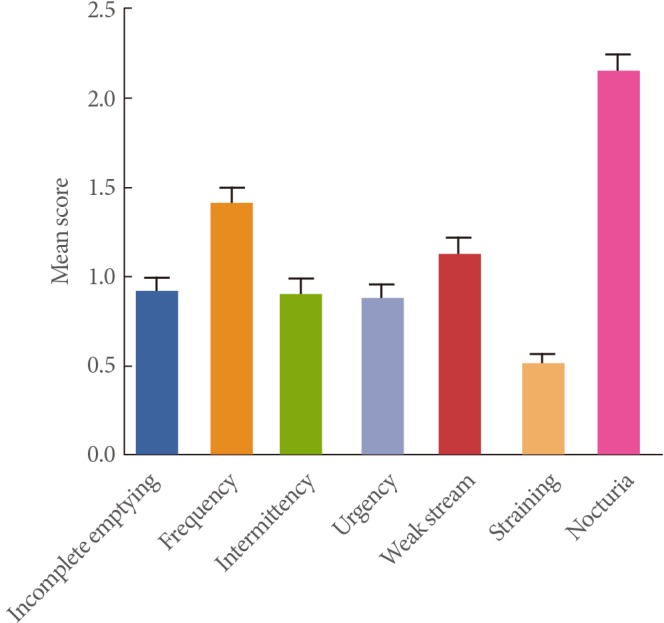
Mean score of each lower urinary tract symptom.
Of the urinary symptoms, only nocturia and frequency correlated with the HRQoL score, with nocturia having the strongest association (r=0.40; 95% CI, 0.31-0.47; P<0.001 and r=0.12; 95% CI, 0.01-0.21; P=0.003, respectively). Fig. 3 is the graphical representation of the correlation of each lower urinary tract symptom with the HRQoL score.
Fig. 3.
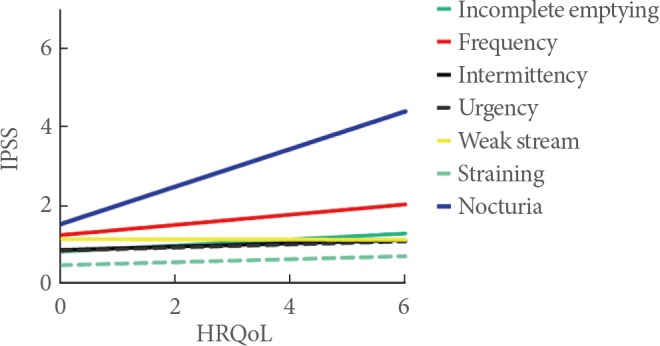
Correlation between each lower urinary tract symptom and quality of life. IPSS, International Prostate Symptom Score; HRQoL, health-related quality of life.
DISCUSSION
We evaluated the impact of each urinary symptom on QoL in community-dwelling men aged >50 years. Nocturia was the most prevalent symptom with the greatest negative impact on QoL, followed by frequency. Urinary symptoms were assessed with the IPSS questionnaire because it is a simple and universally applicable tool for the quick estimation of LUTS and the related QoL [10].
In our study, we found a high prevalence of LUTS in community-dwelling men, which is in accordance with previously reported results [1,3,11,12,13,14]. Nocturia was the most common symptom (58.9%), followed by frequency (35.9%), and weak urinary stream (27.7%). It is known that the incidence of nocturia increases with aging and the prevalence rate of 2 or more voids per night may exceed 50% in older individuals [1,3]. Nocturia is defined by the International Continence Society as the need to awaken one or more times at night to void [15]. However, many studies considered nocturia to be 2 or more voids per night, based on the fact that 1 void per night does not significantly affect QoL [13]. Therefore, in our study, we considered nocturia to be 2 or more voids per night when analyzing the prevalence of nocturia.
Some studies have already demonstrated an association between nocturia and poorer HRQoL in men with BPH. Van Dijk et al. [8] reported that among the symptoms assessed by the IPSS questionnaire, nocturia, urgency, and weak stream were associated with poorer QoL. Storage symptoms such as urgency, increased frequency, and nocturia reportedly have a greater impact on QoL than voiding symptoms [16]. In our study, only nocturia and frequency had a negative impact on the QoL in community-dwelling men.
Urgency is another symptom that negatively impacts QoL [16], mainly in studies on OAB [17,18]. Contrary to these findings, we could not demonstrate a significant correlation between urgency and QoL in men from a community setting. We believe that this could be attributed to the assessment method; the current study utilized an item of the IPSS questionnaire, which is not an adequate instrument to accurately assess OAB.In studies on patients with OAB, more complete and specific questionnaires were developed to evaluate urgency, which led to a better understanding of the impact of urgency on QoL. Furthermore, the impact of LUTS on QoL may differ among populations [16,19].
The relatively small number of patients in our study compared with that in other community-based studies may be a limitation of our study. However, our purpose was mainly to assess the impact of each symptom on QoL, rather than determine the prevalence of LUTS in the general population [20]. Moreover, our sample was large enough to produce significant findings. Although hypertension, diabetes, smoking, and physical activity can be linked to LUTS, these factors are not usually the main causes of urinary disorders in most patients. Men with severe arterial hypertension (and secondary chronic heart failure) or uncontrolled diabetes are more prone to developing LUTS. However, no such cases were identified in our population, thus preventing a more detailed evaluation. Another limitation of our study is that mood disorders (anxiety and depression) and hormone levels (andropause syndrome) were not considered, which may have had some impact on our findings.
The present study corroborates the understanding of nocturia as a symptomatic urinary disorder rather than a symptom of some other condition. Although the clinical significance of nocturia has been difficult to quantify, it has been increasingly recognized because of associations with several aspects of HRQoL as well as increased morbidity and mortality [13,21]. The understanding of nocturia as the symptom with the greatest impact on QoL may facilitate the development of specific treatment strategies for this condition, which could lead to better improvements in patient health.
Nocturia is a prominent component of LUTS in community-dwelling men aged >50 years, with the greatest negative impact on QoL. This finding may be important in the evaluation and development of treatment strategies for LUTS in elderly men.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Bosch JL, Weiss JP. The prevalence and causes of nocturia. J Urol. 2010;184:440–446. doi: 10.1016/j.juro.2010.04.011. [DOI] [PubMed] [Google Scholar]
- 2.Angalakuditi M, Seifert RF, Hayes RP, O'Leary MP, Viktrup L. Measurement properties of the benign prostatic hyperplasia impact index in tadalafil studies. Health Qual Life Outcomes. 2010;8:131. doi: 10.1186/1477-7525-8-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim SO, Choi HS, Kim YJ, Kim HS, Hwang IS, Hwang EC, et al. Impact of nocturia on health-related quality of life and medical outcomes study sleep score in men. Int Neurourol J. 2011;15:82–86. doi: 10.5213/inj.2011.15.2.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Badía X, Garcia-Losa M, Dal-Re R. Ten-language translation and harmonization of the International Prostate Symptom Score: developing a methodology for multinational clinical trials. Eur Urol. 1997;31:129–140. doi: 10.1159/000474438. [DOI] [PubMed] [Google Scholar]
- 5.Yoshimura K, Arai Y, Ichioka K, Terada N, Matsuta Y, Okubo K. Symptom-specific quality of life in patients with benign prostatic hyperplasia. Int J Urol. 2002;9:485–490. doi: 10.1046/j.1442-2042.2002.00503.x. [DOI] [PubMed] [Google Scholar]
- 6.Ushijima S, Ukimura O, Okihara K, Mizutani Y, Kawauchi A, Miki T. Visual analog scale questionnaire to assess quality of life specific to each symptom of the International Prostate Symptom Score. J Urol. 2006;176:665–671. doi: 10.1016/j.juro.2006.03.031. [DOI] [PubMed] [Google Scholar]
- 7.Batista-Miranda JE, Molinuevo B, Pardo Y. Impact of lower urinary tract symptoms on quality of life using Functional Assessment Cancer Therapy scale. Urology. 2007;69:285–288. doi: 10.1016/j.urology.2006.09.054. [DOI] [PubMed] [Google Scholar]
- 8.Van Dijk MM, Wijkstra H, Debruyne FM, De La Rosette JJ, Michel MC. The role of nocturia in the quality of life of men with lower urinary tract symptoms. BJU Int. 2010;105:1141–1146. doi: 10.1111/j.1464-410x.2009.08969.x. [DOI] [PubMed] [Google Scholar]
- 9.Sountoulides P, van Dijk MM, Wijkstra H, de la Rosette JJ, Michel MC. Role of voiding and storage symptoms for the quality of life before and after treatment in men with voiding dysfunction. World J Urol. 2010;28:3–8. doi: 10.1007/s00345-009-0480-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McVary KT, Roehrborn CG, Avins AL, Barry MJ, Bruskewitz RC, Donnell RF, et al. Update on AUA guideline on the management of benign prostatic hyperplasia. J Urol. 2011;185:1793–1803. doi: 10.1016/j.juro.2011.01.074. [DOI] [PubMed] [Google Scholar]
- 11.Blanker MH, Bohnen AM, Groeneveld FP, Bernsen RM, Prins A, Ruud Bosch JL. Normal voiding patterns and determinants of increased diurnal and nocturnal voiding frequency in elderly men. J Urol. 2000;164:1201–1205. [PubMed] [Google Scholar]
- 12.Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S, et al. Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of the EPIC study. Eur Urol. 2006;50:1306–1314. doi: 10.1016/j.eururo.2006.09.019. [DOI] [PubMed] [Google Scholar]
- 13.Boongird S, Shah N, Nolin TD, Unruh ML. Nocturia and aging: diagnosis and treatment. Adv Chronic Kidney Dis. 2010;17:e27–e40. doi: 10.1053/j.ackd.2010.04.004. [DOI] [PubMed] [Google Scholar]
- 14.Coyne KS, Sexton CC, Thompson CL, Milsom I, Irwin D, Kopp ZS, et al. The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from the Epidemiology of LUTS (EpiLUTS) study. BJU Int. 2009;104:352–360. doi: 10.1111/j.1464-410X.2009.08427.x. [DOI] [PubMed] [Google Scholar]
- 15.Abrams P, Cardozo L, Fall M, Griffiths D, Rosier P, Ulmsten U, et al. The standardisation of terminology of lower urinary tract function: report from the Standardisation Sub-committee of the International Continence Society. Neurourol Urodyn. 2002;21:167–178. doi: 10.1002/nau.10052. [DOI] [PubMed] [Google Scholar]
- 16.Masumori N, Tanaka Y, Takahashi A, Itoh N, Ogura H, Furuya S, et al. Lower urinary tract symptoms of men seeking medical care--comparison of symptoms found in the clinical setting and in a community study. Urology. 2003;62:266–272. doi: 10.1016/s0090-4295(03)00252-8. [DOI] [PubMed] [Google Scholar]
- 17.Wang Y, Xu K, Hu H, Zhang X, Wang X, Na Y, et al. Prevalence, risk factors, and impact on health related quality of life of overactive bladder in China. Neurourol Urodyn. 2011;30:1448–1455. doi: 10.1002/nau.21072. [DOI] [PubMed] [Google Scholar]
- 18.Coyne KS, Sexton CC, Kopp ZS, Ebel-Bitoun C, Milsom I, Chapple C. The impact of overactive bladder on mental health, work productivity and health-related quality of life in the UK and Sweden: results from EpiLUTS. BJU Int. 2011;108:1459–1471. doi: 10.1111/j.1464-410X.2010.10013.x. [DOI] [PubMed] [Google Scholar]
- 19.Sagnier PP, MacFarlane G, Teillac P, Botto H, Richard F, Boyle P. Impact of symptoms of prostatism on level of bother and quality of life of men in the French community. J Urol. 1995;153(3 Pt 1):669–673. doi: 10.1097/00005392-199503000-00033. [DOI] [PubMed] [Google Scholar]
- 20.Andersson SO, Rashidkhani B, Karlberg L, Wolk A, Johansson JE. Prevalence of lower urinary tract symptoms in men aged 45-79 years: a population-based study of 40 000 Swedish men. BJU Int. 2004;94:327–331. doi: 10.1111/j.1464-410X.2004.04930.x. [DOI] [PubMed] [Google Scholar]
- 21.Asplund R. Mortality in the elderly in relation to nocturnal micturition. BJU Int. 1999;84:297–301. doi: 10.1046/j.1464-410x.1999.00157.x. [DOI] [PubMed] [Google Scholar]


