Abstract
Introduction:
Abnormalities in biological rhythms (BR) may have a role in the pathophysiology of Bipolar Disorders (BD). The objective of this study is to validate the Italian version of the Biological Rhythms Interview of Assessment in Neuropsychiatry (BRIAN), a useful tool in studying BR, and measure its accuracy in discriminating BD.
Methods:
44 outpatients with DSM-IV-TR diagnosis of BD and 38 controls balanced for sex and age were consecutively recruited. The discriminant validity of BRIAN for the screening of BD and its test re-test reliability in two evaluations were assessed.
Results:
BD patients scored 22.22±11.19 in BRIAN against 7.13±5.6 of the control group (P<0.0001). BRIAN showed a good accuracy to screen between BD non-BD at cutoff 16, a sensitivity was 68.2 and specificity was 92.5. The test-retest stability measured using Pearson’s coefficient found very high r values for each section and the total score, thus indicating a correlation at the two times of statistical significance in all measures. Cohen’s Kappa varied from 0.47 in the sociality section to 0.80 in the sleep section, with a total K mean of 0.65.
Conclusion:
The results show that the Italian version of BRIAN has good discriminant validity in detecting BD from healthy controls and shows good test-retest reliability. The study suggests the possibility of developing mixed screening tools by introducing items on dysregulation of biological rhythms to the usual measures of mood.
Keywords: Biological rhythms, bipolar disorders, BRIAN, Italian screening, validation.
1. INTRODUCTION
The course of bipolar disorder is, by definition, cyclical and characterized by episodes of depression and (hypo)mania with or without mixed features, with – or without - interepisodic euthymia [1]. As the mood switch involves a change of biological rhythms, with changes in sleeping patterns constituting perhaps the most relevant one, it was thought that abnormalities in biological rhythms might have a role in the pathophysiology of the disease [2]. From these considerations, the literature reports a relationship between biological rhythm disturbances and treatment and the onset, maintenance and remission of bipolar episodes [3]. There is also evidence about the relevance of dys-regulation of hormones and neurotransmitters that command biological rhythms in bipolar disorders [4-8]. Physiological and behavioral timekeeping processes are frequently found abnormal in bipolar disorders, thus a vulnerability to alterations in biological rhythms may play a certain role in the course of the disease [9]. Differences in the course of bipolar disorders may also be caused by genetic differences concerning regulation of biological rhythms [10]. Moreover, biological rhythm impairment has been associated with poor functioning and quality of life [11].
Thus, circadian rhythms are related to bipolar disorders in three different ways: (1) by considering its etiological/triggering role, (2) as a very reliable early warning sign of relapse, very useful in psychoeducation [12], and (3) its modification –by means of psychological or drug interventions - may have a therapeutic effect.
The Biological Rhythms Interview of Assessment in Neuropsychiatry (BRIAN) is an 18-items interviewer-administered instrument which aims to investigate four main areas related to circadian rhythm disturbance, namely: sleep, activities, social rhythms and eating patterns. Items are rated using a 4-point scale, (1)= no difficulty, (2)= mild difficulty, (3)= moderate difficulty, and (4) =severe difficulty. The BRIAN scores thus range from 1 to 72, where the higher scores suggest severe circadian rhythm disturbance [13]. To date, the scale is available in Portuguese, Spanish and English. Hereby we aim to validate the Italian version of this tool.
2. METHOD
2.1. Study Sample
44 euthymic (Young Mania Rating Scale (YMRS)<6, Hamilton Depression Rating Scales (HDRS)<8 for a period of at least one month before inclusion) outpatients with a DSM-IV-TR diagnosis of bipolar disorder and 38 control subjects balanced for sex and age were recruited. The comparison group was recruited from the general population within the catchment area of Cagliari, Italy. The test-retest reliability measure was carried out in half (N=41) of the sample recruited randomly out of the original sample after stratification by sex and diagnosis.
Diagnosis was conducted according to the “Advanced Neuropsychiatric Tools and Assessment Schedule” (ANTAS) [14] a semi-structured clinical interview derived in part from the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) non-patient version (SCID-I/NP) [15]. The control subjects were screened using the same interview to exclude current or lifetime psychiatric disorders. Controls had no first-degree relatives with bipolar disorder or other psychiatric disorders.
The study was approved by the Università Europea del Mediterraneo Onlus Ethics Committee and was carried out in compliance with the Helsinki Declaration of 1975 (the Evaluation, Support and Prevention Unit). All subjects contacted were informed about the study and when they decided to participate they signed a consensus form.
2.2. Assessment and Instruments
The clinical researchers were trained beforehand in the use of the study tools. One clinical researcher recorded the socio-demographic and clinical variables of each patient, administered the Italian version of the Young Mania Rating Scale (YMRS) [16], the 17-items Hamilton Depression Rating Scale (HDRS-17) [17] and the Global Assessment Functioning (GAF) scale [18] to confirm the stability of the patient's condition and overall functioning. She also recorded all the medication prescribed to the patient for each visit. Finally, a second researcher administered the BRIAN. Interviewers administering the BRIAN and the GAF, HDRS and YMRS were blinded to each other.
2.3. BRIAN
The BRIAN was developed by the Bipolar Disorders Program & INCT Translational Medicine and by the Hospital de Clínicas de Porto Alegre, Universidade Federal do Rio Grande do Sul, Porto Alegre, Brazil. It is an interviewer-administered instrument designed for use by a trained clinician; the time frame studied refers to the last 14 days before assessment. The 18 items evaluating sleep, activities, social rhythm and eating patterns were probed for discriminant, content and construct validity. All items were rated using a 4-point scale scored 1 = not at all, 2 = seldom, 3 = sometimes, 4 =often, or in some items 1 =never, 2 = seldom, 3 = often, 4 =always. The global score was obtained when the scores of each item were added up. The score may be regrouped in five specific sections scoring sleep, activity, sociality, eating habits and rhythms.
The original version was translated into Italian to English, back translated and approved by two English native speakers working as researchers in the field of bipolar disorder.
A more detailed description of the instrument is shown in the original paper by Giglio et al. [12]. The Italian version is included in the current paper as an Appendix.
2.4. Psychometrics and Statistical Analysis
Statistical analysis was performed using SPSS for Windows – Version 11.0 (SPSS Inc., Chicago, IL, USA). The accuracy of the BRIAN score in discriminating between cases and controls (discriminant validity) was measured comparing mean BRIAN scores in the two groups with one-way ANOVA. Sensitivity and specificity of BRIAN at cutoff 20 was also carried out. The test re-test reliability of the BRIAN total score and the BRIAN sections (Sleep, Activity, Sociality, Eating, Rythms) was measured comparing to and t1 (1 week later) using both the correlation coefficient of Pearson and Cohen’s kappa value.
3. RESULTS
44 bipolar patients (25 BD I, 19 BD II) and 38 healthy controls were included in the study (Table 1). The mean age of the sample was 44.61 + 12.64 without differences between cases and controls regarding the distribution by sex.
Table 1.
Characteristics of the sample and concurrent validity of the BRIAN.
| Variable | Descrictive Statistics |
|---|---|
| N (%) sample | 80 (100%) |
|
Age (years) Bipolar (44) Not Bipolar (38) |
mean ± sd = 44.61 ± 12.64 45.21 + 13.18 43.95±12.01 BP vs nBP F=0.20, df 1,80,81, P=0.604 |
|
Gender Male Female |
32 (39.0%) – 16 Bipolar Disorders (42.1%) 50 (61.0%) – 22 Bipolar Disorders (57.89%) BP vs nBP Χ2=0.28, 1df, P=0.595 |
|
DSM-IV Diagnosis Bipolar Disorder I Bipolar Disorder II No Diagnosis |
25 (30.5%) 19 (23.2%) 38 (46.3%) |
| Brian Bipolar Brian non Bipolar | 22.22±11.19 7.13±5.6 F=56.75, df 1,80,81, P<0.0001 |
The bipolar sample included 16 men (42.1%) and this rate was similar (16 men, 36.4%) in the control group. In the Bipolar Sample, 25 subjects were diagnosed as Bipolar I (30.5% of the whole sample) and 19 (23.3%) as Bipolar II (Table 1).
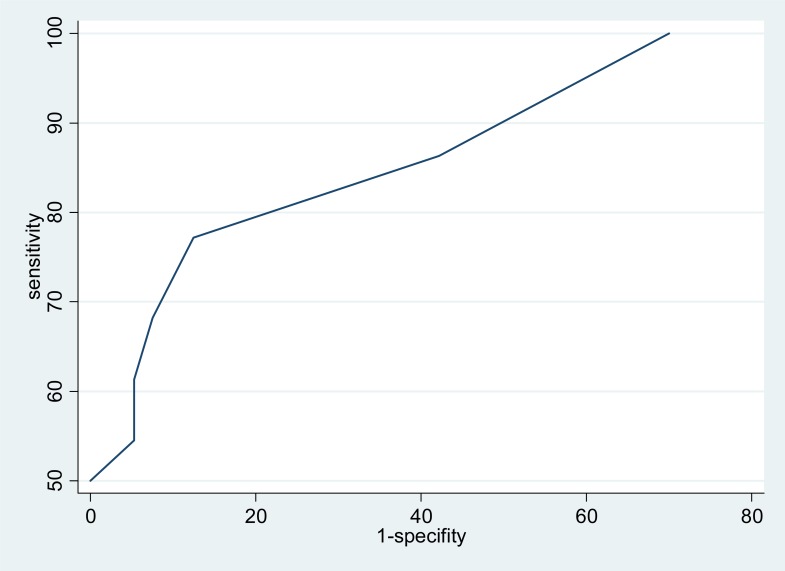
Bipolar Patients scored 22.22±11.19 in BRIAN against 7.13±5.6 in the control group (F=56.75, df 1,80,81, p<0.0001). BRIAN showed good accuracy in screening between BD and non-BD with quite good performance in specificity, for example at cutoff 16, with a sensitivity of 68.2, specificity was excellent (92.5). Table 2 shows the performance of BRIAN as a screening tool for Bipolar Disorders at different cutoff points. Fig. (1) translates these results into a ROC Curve.
Table 2.
Accuracy of BRIAN as screener for Bipolar Disorder.
| Cutoff | Sensitivity | 1-Specificity | Specificity | VPP | VPN |
|---|---|---|---|---|---|
| 4 | 100 | 70 | 30 | 60 | 100 |
| 8 | 86.3 | 42.2 | 57.8 | 70.7 | 78.5 |
| 12 | 77.2 | 12.5 | 87.5 | 87.12 | 77.7 |
| 16 | 68.2 | 7.5 | 92.5 | 91.1 | 72.5 |
| 18 | 61.3 | 5.3 | 94.7 | 93.1 | 66.6 |
| 20 | 54.5 | 5.3 | 94.7 | 92.3 | 64.3 |
| 28 | 50 | 0 | 100 | 100 | 54.8 |
Fig. (1).
ROC curve.
Test-retest stability was measured in half of the sample randomly recruited after stratification by diagnosis and sex (8 Male; age 44.83, 19 Bipolar). It was found by using both the correlation coefficient of Pearson and Cohen’s kappa value. Table 2 shows the K values (with standard error) and the r values. The Pearson r values were found very high in each section and in the total score, thus indicating a correlation between the two scores with statistical significance in all measures. The K value varied from 0.47 in the sociality section to 0.80 in the sleep section. The K of the total BRIAN Score was 0.65.
DISCUSSION
The Italian version of the BRIAN is a valid and reliable tool with psychometric properties equivalent to the original tool and has a good test-retest reliability measured with K statistics.
Moreover, the results of the present study suggest that the Italian version of the BRIAN shows an interesting discriminant validity in screening for bipolar disorder. The high discriminant validity allows the obtaining of an excellent performance using the BRIAN as a screening tool at the cutoff of 20. From this perspective, we must consider that a screener can really be useful if it does not generate false positives and thus is capable of producing a high predictive value of a negative. In fact, if the test is inexpensive, noninvasive and easy to apply, it can lead to a second evaluation only on positives with a more accurate diagnostic tool, or if another screener is available, one that is equally inexpensive and easy to apply but with complementary performance (with high sensitivity and low specificity), they can be administered simultaneously. We must therefore take into account that the predictive value of negative evidence we found at a cutoff of 20 is noteworthy. It is to be underscored that the BRIAN was not conceived or initially tested as a screening tool, but even then it showed acceptable screening properties.
The results are of interest because of the well-known difficulties in research in developing accurate screeners for bipolar disorder due to the several existing biases which include memory biases, perception of hypomania as a non-pathological state and others [1]. In particular, current screening tools show good sensitivity but low specificity. From this point of view the BRIAN could be highly complementary to questionnaires such as the Mood Disorder Questionnaire (MDQ) and Hypomania Checklist-32 (HCL-32) and its use associated with a clinical questionnaire (more sensitive but less specific) could make the screening very effective.
In all cases the result was so good as to suggest extending the possibility of using a scale of biological rhythms as screening for bipolar disorder or introducing some items on biological rhythms into well-known clinical screeners such as the MDQ [19] or HCL-32 [20].
From this point of view we must consider that this study was conducted by comparing patients with bipolar disorder to people without psychiatric diagnoses. In practice, a screening tool should be able to discriminate especially among people with different pathologies. From this perspective it must be considered that the disturbances of biological rhythms have recently been reported not only in bipolar disorders but also in other psychiatric disorders such as major depression, stress related disorders, autism and schizophrenia [21-24]. However, it has been highlighted in recent literature that the weight of the dysregulation of biological rhythms in bipolar disorder is higher than in other disorders and can be described as a kind of characteristic of these disorders [25, 26]. Even on the level of genetic determinants a justification for the association between dysregulation of biological rhythms and bipolar syndromes has been found [27]. If it is thus evident that the screening of biological rhythm dysregulation can divide people with bipolar disorder from people without a psychiatric diagnosis, it follows that this can occur during a screening of the general population.
However, the extent of biological rhythm dysregulation has never been introduced as a possible screening tool at the speculative level. In the light of these psychometric results it would be interesting to design a tool that that combines the features of mixed measurement of hyperactivity and hyperergia typical of most known screens, such as the MDQ and HCL, with the measurement of biological rhythms. Test-retest reliability probably adds some new data to the first validation study. The study indicates that the total BRIAN score and the BRIAN sub-section scores reach a good correlation in the two measures (t0 and t1) measured by means of Pearson’s correlation factor. The test re-test reliability for each section showed a K agreement from sufficient to good. Sufficient (K from 0.40 to 0.60) was shown for Sociality and Activity sections; Good (K from 0.60 to 0.80) was shown for Sleep, Eating, Rhythm sections and total score.
The study of the regulation of biological rhythms is becoming increasingly important in the field of bipolar disorders. The circadian time keeping process is responsible for controlling sleep patterns. The role of Melatonin secretion in this control is well-known and is today the objective of several studies that may contribute to better understanding the physiopathological process of bipolar disorders as the genetic component and may suggest newer therapeutic pathways [8]. Bipolar subjects, regardless of the mood state, experience a wide variety of disruptions of biological rhythms and sleep disorders [19]. A decreasing amount of deep sleep per night comes just before the onset of a manic episode and may come before a depressive episode [28]. Therefore, the decrease in sleep has been identified as a predictor of manic episodes [28]. Psychoeducational programs have shown that preventing disruptions in the circadian sleep cycle is important in maintaining a regular sleep schedule [11].
LIMITATION
Amongst the limitations we must consider the preliminary nature of the data, the limited sample size and the fact that the current study was designed to validate the Italian version of the BRIAN, not to test its screening properties. Screening performances need to be measured in target populations of future screening studies (ie: community samples), and/or clinical samples including euthymic patients with major depressive disorder because a differential diagnosis between bipolar depression and unipolar depression is often the most important issue in this area in clinical practice. The results must be considered an innovative preliminary report suggesting a new perspective in the development of screening tools, it can be complementary to those explored so far.
CONCLUSION
Due to the relevance of monitoring biological rhythms with a valuable and reproducible instrument, BRIAN can be a useful tool both in research and clinical practice with bipolar patients. The Italian version was shown to have good psychometric proprieties. The results also show that BRIAN has good discriminant validity in detecting BD from healthy controls and shows good test-retest reliability. The study suggests the possibility of developing mixed screening tools by introducing items on biological rhythm dysregulation into the usual measures of mood
Table 3.
Test-retest reliability of BRIAN.
| Section | K (ES) | 95% K | r Pearson (40df) | P | Mean t0 | Mean t1 | T -test |
|---|---|---|---|---|---|---|---|
| Sleep | 0.80(0.13) | 0.55-1.63 | 0.88 | <0.0001 | 4.42±3.88 | 4.09±3.92 | 11.83 |
| Activity | 0.54 (0.18) | 0.19-0.90 | 0.93 | <0.0001 | 4.26±4.44 | 3.85±4.49 | 9.79 |
| Sociality | 0.47(0.19) | 0.09-0.90 | 0.87 | <0.0001 | 2.02±2.60 | 1.85±2.55 | 11.26 |
| Eating | 0.68(0.12) | 0.45-0.91 | 0.85 | <0.0001 | 2.42±2.87 | 1.85±2.23 | 10.23 |
| Rhythm | 0.76 (0.15) | 0.45-1.07 | 0.35 | 0.045 | 2.40±1.24 | 2.57±1.15 | 1.72 |
| Total Score | 0.65 (0.13) | 0.37-0.90 | 0.93 | <0.0001 | 15.54±11.4 | 14.23±11.56 | 16.78 |
ACKNOWLEDGEMENTS
Declared none.
AUTHOR’S CONTRIBUTIONS
MGC and FC participated in the design of the study, in the analysis of the data and drafted the manuscript. MFM, EP, MP and RM participated in acquisition of data and critical revision of the manuscript. FK and EV participated in the analysis of the data and drafted the manuscript. All authors read and approved the final manuscript.
CONFLICT OF INTEREST
The authors confirm that this article content has no conflict of interest.
REFERENCES
- 1.Carta MG, Angst J. Epidemiological and clinical aspects of bipolar disorders: controversies or a common need to redefine the aims and methodological aspects of surveys. Clin Pract Epidemiol Ment Health. 2005;1(1):4. doi: 10.1186/1745-0179-1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jones S, Benca RM. Sleep and Biological Rhythms Abnormalities in the Pathophysiology of Bipolar Disorders in Bipolar Disorders.Chapter 10. Basic Mechanisms and Therapeutic Implications. In: Jair C Soares, Allan H., editors. 189-208 CRC Press Print ISBN: 978-0-8493-9897-1 eBook. 2007. pp. 978–1-4200-2115-8. [Google Scholar]
- 3.Li J, Lu WQ, Beesley S, Loudon AS, Meng QJ. Lithium impacts on the amplitude and period of the molecular circadian clockwork. PLoS One. 2012;7(3):e33292. doi: 10.1371/journal.pone.0033292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dallaspezia S, Benedetti F. Melatonin. circadian rhyhms.and the clock genes in bipolar disorder. Curr Psychiatry Rep . 2009;11(6):488–93. doi: 10.1007/s11920-009-0074-1. [DOI] [PubMed] [Google Scholar]
- 5.Ellenbogen MA, Hodgins S, Linnen AM, Ostiguy CS. Elevated daytime cortisol levels: a biomarker of subsequent major affective disorder?. J Affect Disord. 2011;132(1-2):265–9. doi: 10.1016/j.jad.2011.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Carta MG, Bhat KM, Preti A. GABAergic neuroactive steroids: a new frontier in bipolar disorders?. Behav Brain Funct. 2012;8:61. doi: 10.1186/1744-9081-8-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hardoy MC, Serra M, Carta MG, Contu P, Pisu MG, Biggio G. Increased neuroactive steroid concentrations in women with bipolar disorder or major depressive disorder. J Clin Psychopharmacol. 2006;26(4):379–84. doi: 10.1097/01.jcp.0000229483.52955.ec. [DOI] [PubMed] [Google Scholar]
- 8.Lanfumey L, Mongeau R, Hamon M. Biological rhythms and melatonin in mood disorders and their treatments. Pharmacol Ther. 2013;138(2):176–84. doi: 10.1016/j.pharmthera.2013.01.005. [DOI] [PubMed] [Google Scholar]
- 9.Harvey AG. Sleep and circadian functioning: critical mechanisms in the mood disorders?. Annu Rev Clin Psychol. 2011;7:297–319. doi: 10.1146/annurev-clinpsy-032210-104550. [DOI] [PubMed] [Google Scholar]
- 10.McCarthy MJ, Nievergelt CM, Kelsoe JR, Welsh DK. A survey of genomic studies supports association of circadian clock genes with bipolar disorder spectrum illnesses and lithium response. PLoS One. 2012;7(2):e32091. doi: 10.1371/journal.pone.0032091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Giglio LM, Magalhães PV, Kapczinski NS, Walz JC, Kapczinski F. Functional impact of biological rhythm disturbance in bipolar disorder. J Psychiatr Res. 2010;44(4):220–3. doi: 10.1016/j.jpsychires.2009.08.003. [DOI] [PubMed] [Google Scholar]
- 12.Colom F, editor. . ISBN - 10: 0521683688 ISBN 13: 9780521683685. Colombia : Cambridge University Press 2010; Psychoeducation Manual for Bipolar Disorder. [Google Scholar]
- 13.Giglio LM, Magalhães PV, Andreazza AC , et al. Development and use of a biological rhythm interview. J Affect Disord. 2009;118(1-3):161–5. doi: 10.1016/j.jad.2009.01.018. [DOI] [PubMed] [Google Scholar]
- 14.Carta MG, Aguglia E, Bocchetta A , et al. The use of antidepressant drugs and the lifetime prevalence of major depressive disorders in Italy. Clin Pract Epidemiol Ment Health. 2010;6:94–100. doi: 10.2174/1745017901006010094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.First MB, Spitzer R, Gibbon M, editors. Structured clinical interview for DSM-IV Axis I Disorders. Washington DC.: Am Psychiat Press Inc.; 1997. In Biometrics Research Deparment Ed. [Google Scholar]
- 16.Young RC, Biggs JT, Ziegler VE, Meyer DA. A rating scale for mania: reliability. validity and sensitivity. Br J Psychiatry. 1978;133:429–35. doi: 10.1192/bjp.133.5.429. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiat. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.American Psychiatric Association. Diagnostic and Statistical manual for Mental Disorders. 4th Edition (DSM IV) Global Assessment of Functioning Scale (GAF). Washington DC:: American Psychiatric Press; 1994. American Psychiatric Association. [Google Scholar]
- 19.Hirschfeld RMA, Williams JBW, Spitzer RL , et al. Development and validation of a screening instrument for bipolar spectrum disorder: the Mood Disorder Questionnaire. Am J Psychiatry. 2000;157(11):1873–75. doi: 10.1176/appi.ajp.157.11.1873. [DOI] [PubMed] [Google Scholar]
- 20.Angst J, Meyer TD, Adolfsson R , et al. Hypomania: a transcultural perspective. World Psychiatry. 2010;9(1):41–9. doi: 10.1002/j.2051-5545.2010.tb00268.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lamont EW, Legault-Coutu D, Cermakian N, Boivin DB. The role of circadian clock genes in mental disorders. Dialog Clin Neurosci. 2007;9:33–42. doi: 10.31887/DCNS.2007.9.3/elamont. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McClung CA. Circadian genes. rhythms and the biology of mood disorders. Pharmacol Ther. 2007;114:222–232. doi: 10.1016/j.pharmthera.2007.02.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bourgeron T. The possible interplay of synaptic and clock genes in autism spectrum disorders. Cold Spring Harbor Symposium on Quantum Biology. 2007:645–54. doi: 10.1101/sqb.2007.72.020. [DOI] [PubMed] [Google Scholar]
- 24.Carta MG, Balestrieri M, Murru A, Hardoy MC. Adjustment Disorder epidemiology diagnosis and treatment. Clin Pract Epidemiol Ment Health. 2009;5:15. doi: 10.1186/1745-0179-5-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robillard R, Naismith SL, Hickie IB. Recent advances in sleep-wake cycle and biological rhythms in bipolar disorder. Curr Psychiatry Rep. 2013;15(10):402. doi: 10.1007/s11920-013-0402-3. [DOI] [PubMed] [Google Scholar]
- 26.Benedetti F, Sorretti A, Colombo C, Campori E, Barbini B, di Bella D. Influence of a functional polymorphism within the promoter of the serotonin transporter gene on the effects of total sleep deprivation in bipolar depression. Am J Psych. 1999;156:1450–2. doi: 10.1176/ajp.156.9.1450. [DOI] [PubMed] [Google Scholar]
- 27.Prasko J. Bright light therapy. Neuro Endocrinol Lett. 2008;29 (Suppl 1 ):33–64. [PubMed] [Google Scholar]
- 28.Benazzi F. A prediction rule for diagnosing hypomania. Prog europsychopharmacol Biol Psychiatry. 2009;33(2):317–22. doi: 10.1016/j.pnpbp.2008.12.007. [DOI] [PubMed] [Google Scholar]