Abstract
Historically, the lack of melanocytes in the vaginal and cervical mucus membranes has deterred the findings of primary melanomas. Mainly due to its rarity, difficulty to diagnose, and poor prognosis, there has been no absolute agreement on comprehensive treatment so far. In this case report, we present a case of a 46-year-old woman with primary malignant melanoma of uterine cervix. She underwent neo-adjuvant chemotherapy initially followed by a radical hysterectomy. After adjuvant concurrent chemo-radiation, the patient has been followed up for 24 months. So far, she has not shown any symptoms or signs of recurrence. Further studies with more cases based on variable combinations of treatment regimen have been on the way.
Keywords: Malignant melanoma, uterine cervix, neo-adjuvant chemotherapy, chemo-radiation
Introduction
Malignant melanoma, a common neoplasm of the mucous membranes and skin, makes up 2% of all newly diagnosed cancers (1,2). In the women, 3% to 7% of all cases develop within genital tract and mostly found in the vulva and vagina. On the other hands, primary malignant melanoma of the uterine cervix is extremely rare with an incidence five times lower than primary vaginal or vulva cases. In fact, only 80 cases have been reported (3-5).
Mainly due to its rarity and difficulty to diagnose, there has been no absolute agreement on comprehensive treatment so far. Radical hysterectomy coupled with regional lymphadenectomy and/or concurrent chemo-radiation therapies are generally recommended and the prognosis is usually poor and unpredictable. Our aim is to present the new treatment combination and to give a new way to establish a standard treatment.
Case report
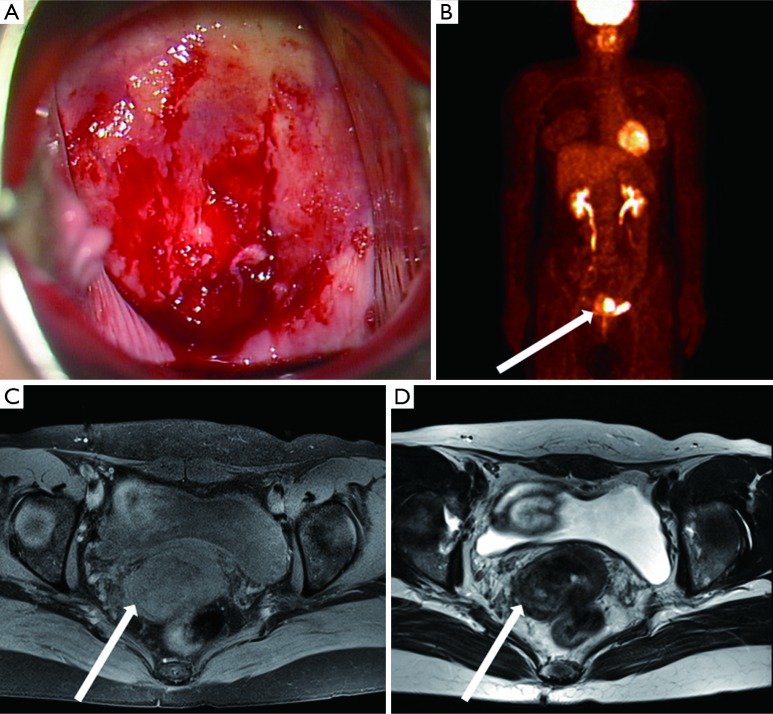
A 46-year-old woman visited the gynecology clinic of Korea University Medical Centre with approximately one month’s history of postcoital vaginal bleeding. She had two normal vaginal deliveries and undergone a laparoscopic unilateral salpingo-oophorectomy in 2009 mainly for tubo-ovarian abscess with noting of note in her and her family medical history. One year ago, she took a cervical cytology test and the result was negative for malignancy. On our pelvic examination, the uterine cervix showed a consistent hardness, slightly increasing size, and easy-touch bleeding surface. First, cervical cytology examinations (Thin Prep® PAP Test, Hologic, Inc., Marlborough, MA, USA) and human papillomavirus (HPV) DNA test (Hybrid Capture 2 High-Risk HPV DNA Test, Qiagen, Netherlands) were taken but the results were negative. Multiple blunt biopsies were taken as the next step. The histological examination revealed the existence of a malignant melanoma cell in cervix and immunohistochemistry showed positive reaction for human melanoma black 45 (HMB45) and S-100 protein. For the detection of primary focus, gynecologic oncologists and dermatologists did systemic examinations, however, no suspicious lesion as the primary focus was observed. On recto-vaginal examination, the involvement of cancer mass to both parametrium was not detected. However, magnetic resonance image (MRI) showed a 5 cm × 4 cm sized cancer mass with the possibility of parametrial invasions. Positron emission tomography-computed tomography (PET-CT) also showed intense hyper-metabolic lesions in cervix and lymph nodes (LNs) of both internal iliac areas, suggesting malignancies with metastatic LNs (Figure 1). The clinical diagnosis made for this patient was International Federation of Gynecology and Obstetrics (FIGO) stage IB2.
Figure 1.
Several diagnostic imaging studies of primary malignant melanoma of uterine cervix. (A) Colposcopic finding of malignant melanoma with hard consistency and easy-touch bleeding; (B) PET-CT with round hyper-metabolic image; (C) T1 weighted transverse image; (D) T2 weighted transverse image (white solid arrow: malignant melanoma). PET-CT, positron emission tomography-computed tomography.
Considering the poor prognosis of malignant melanoma, our multidisciplinary groups decided to take more aggressive treatments consisting of radical hysterectomy following neo-adjuvant chemotherapy and adjuvant concurrent chemo-radiation. Initially, two cycles of cisplantin (CDDP) 20 mg/m2 and dacarbazine (DTIC) 250 mg/m2 were administered with 2-week interval as neo-adjuvant chemotherapies and then, she underwent radical hysterectomy, right salpingo-oophorectomy, and pelvic lymphadenectomy. Final pathology showed spindle-shaped malignant melanoma cells in cervix and uterine myometrium (Figure 2). The resection margin showed the involvement of parametrium and one invasion out of three left pelvic LNs was also found. As planned, four cycles of CDDP 20 mg/m2 and DTIC 250 mg/m2 were administered at every 4 weeks interval and concurrently, whole pelvis was treated with daily 200 cGy in 25 fractions up to total 5,000 cGy with external beam radiation therapy, followed by 350 cGy with high dose rate brachytherapy.
Figure 2.
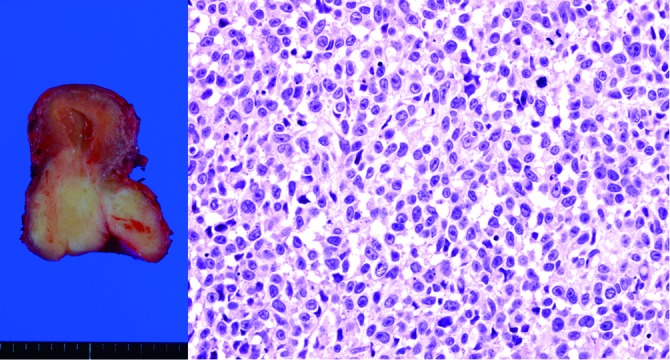
Horizontal section of postoperative uterine specimen and microscopic finding of malignant melanoma (hematoxylin & eosin, ×400).
After adjuvant treatment, PET-CT was taken again showing the disappearance of previously existing hypermetabolic lesions in uterine cervix and internal iliac area. The patient has been followed up for 24 months and she has not shown any symptoms or signs of recurrence.
Discussion
Malignant melanoma can occur in a variety of mucosal sites. However, female genital area is an extremely unusual site. Among women, 3% to 7% of all cases develop within genital tract and the most favorite sites are vulva and vagina. Primary malignant melanoma of the uterine cervix is an extremely rare neoplasm of which only 80 cases have been reported. Indeed, cervix is the worst site for tumors to grow due to its limited blood supply and fibrous stromas with an incidence five times lower than primary vaginal or vulva mucosal melanomas (3-6).
In addition to its rarity, the lack of melanocytes in the vaginal and cervical mucus membranes makes diagnosing malignant melanoma of cervix more difficult. Cervical malignant melanomas can also mimic various types of neoplasm such as malignant lymphoma, carcinoma, and sarcoma and tend to metastasize early (6,7).
The incident of malignant melanoma of cervix becomes higher as the age of the patient increases though it is not known whether prognosis of the patient depends on the age. The extremely low survival rates of the cervical cancer even compared to the vagina or vulva cancers may reflect the fact that the higher proportion of cervical tumors are initially diagnosed at an advanced stage and consequently, and the increasing potential for post-treatment complications prevents aggressive therapy (8). As a consequence, poor prognosis is considered for the neoplasm itself and there is very little consensus on the therapeutic approach of primary malignant melanoma.
Radical hysterectomy with pelvic LNs dissection has been accepted as the treatment recommendation for malignant melanoma of the uterine cervix, followed by external beam and/or intracavitary radiation therapy and chemotherapy (1,2). However, the study on this recommendation has not been evidenced and still very few cases have been reported.
In this study, we report our new combination of treatment regimen. Unlike in the previous ones, the patient was initially treated with neo-adjuvant chemotherapy followed by radical hysterectomy. Adjuvant chemo-radiation was also taken and 24-month follow-up has shown no evidence of recurrence.
Primary malignant melanoma of the uterine cervix is hard to diagnose because it usually presents with no symptom but nonspecific vaginal bleeding as in our case. To correctly diagnose such subtle disease as quickly as possible, careful examinations and detailed clinical investigations should be done even when patients present with such subtle symptoms. Except for a few reported cases, most patients of malignant melanoma present with unusual vaginal bleeding and post coital bleeding (9). Further investigations and more studies are mandatory for a better understanding of this rare entity and consequently better prognosis.
Acknowledgements
Disclosure: The authors declare no conflict of interest.
References
- 1.Tomicic J, Wanebo HJ. Mucosal melanomas. Surg Clin North Am 2003;83:237-52 [DOI] [PubMed] [Google Scholar]
- 2.Pusceddu S, Bajetta E, Carcangiu ML, et al. A literature overview of primary cervical malignant melanoma: an exceedingly rare cancer. Crit Rev Oncol Hematol 2012;81:185-95 [DOI] [PubMed] [Google Scholar]
- 3.Gupta S, Sodhani P, Jain S.Primary malignant melanoma of uterine cervix: a rare entity diagnosed on fine needle aspiration cytology--report of a case. Cytopathology 2003;14:153-6 [DOI] [PubMed] [Google Scholar]
- 4.Chang AE, Karnell LH, Menck HR. The National Cancer Data Base report on cutaneous and noncutaneous melanoma: a summary of 84,836 cases from the past decade. The American College of Surgeons Commission on Cancer and the American Cancer Society. Cancer 1998;83:1664-78 [DOI] [PubMed] [Google Scholar]
- 5.McLaughlin CC, Wu XC, Jemal A, et al. Incidence of noncutaneous melanomas in the U.S. Cancer 2005;103:1000-7. [DOI] [PubMed]
- 6.Duggal R, Srinivasan R.Primary amelanotic melanoma of the cervix: case report with review of literature. J Gynecol Oncol 2010;21:199-202 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mordel N, Mor-Yosef S, Ben-Baruch N, et al. Malignant melanoma of the uterine cervix: case report and review of the literature. Gynecol Oncol 1989;32:375-80 [DOI] [PubMed] [Google Scholar]
- 8.Calderón-Salazar L, Cantú de Leon D, Perez Montiel D, et al. Primary malignant melanoma of the uterine cervix treated with ultraradical surgery: a case report. ISRN Obstet Gynecol 2011;2011:683020. [DOI] [PMC free article] [PubMed]
- 9.Baruah J, Roy KK, Kumar S, et al. A rare case of primary malignant melanoma of cervix. Arch Gynecol Obstet 2009;280:453-6 [DOI] [PubMed] [Google Scholar]