Abstract
Background
Hypertension is increasingly common in sub-Saharan Africa, and rates of hypertension control are low. Use of traditional herbal medicines (THM) is common among adults in sub-Saharan Africa and may affect hypertension therapy.
Methods
We searched Ovid MEDLINE, Ovid EMBASE, and Web of Knowledge in June 2013 to find studies about THM use among hypertensive patients living in sub-Saharan Africa. Two independent reviewers evaluated titles and abstracts. Qualifying references were reviewed in full text. Data were extracted using a standardized questionnaire.
Results
Four hundred eighty-one references were retrieved, and 4 articles from 2 countries met criteria for inclusion. The prevalence of THM use was 25-65% (average 38.6%). THM was the most common type of complementary and alternative medicines used by patients (86.7%-96.6%). Among THM users, 47.5% concomitantly used both allopathic medicine and THM. Increased age (p<0.001), male sex (RR 2.58), belief in a supernatural cause of hypertension (RR 2.11), and family history of hypertension (OR 1.78) were positively associated with THM use while belief that hypertension is preventable was negatively associated with THM use (OR 0.57).
Conclusion
More than a third of adults with hypertension in sub-Saharan Africa use THM. Half of these patients use THM concurrently with allopathic medicine. Healthcare workers in sub-Saharan Africa must discuss THM use with their hypertensive patients. More research is urgently needed to define the impact of THM use on hypertension control and outcomes in sub-Saharan Africa.
Keywords: sub-Saharan Africa, hypertension, blood pressure, traditional herbal medicine, complementary and alternative medicine, traditional healers
Introduction
Although hypertension (HTN) was formerly rare in Africa [1–3], HTN prevalence is now rapidly increasing [4]. In one serial survey of Tanzanian adults 47-57 years old, the overall prevalence of hypertension increased from 25% to 40% between 1987 and 1998 alone [5–7]. According to the World Health Organization, the age-standardized prevalence of HTN in adults >25 years in Africa is now the highest in the world [8].
HTN-related complications are increasingly common in sub-Saharan Africa (SSA) [9,10]. The incidence of stroke in adults aged 30-69 in Tanzania is one of the highest rates in the world (120/100,000 person years) and is 6-10 fold higher than the US, UK and Canada [11]. At our own hospital in Western Tanzania, HTN-related diseases accounted for 15% of all medical admissions, deaths, and hospital days – second only to HIV – and half of these deaths occurred in adults < 65 years old [12]. The early onset of HTN-related complications has been attributed to low rates of diagnosis, treatment and control [13,14]. In one study, the authors summarized this problem as the rule of 1/6ths: among adults with HTN in Africa, only 2/6 are aware of their diagnosis, of these only 1/6 are on treatment, and of these only 1/6 are controlled [15].
Traditional herbal medicine (THM), may have significant impact on HTN treatment and control in sub-Saharan Africa [16]. THM use is high among adults in SSA with a prevalence ranging from 38.5%-90% [17–20]. THM is commonly used around the world for both cardiovascular disease in general [21] and HTN specifically [22–24]. In our experience in Tanzania, adults admitted with complications of HTN frequently report prior THM use.
Therefore, we conducted a systematic review of the literature to collect and describe the currently available data regarding THM use among adults with HTN in SSA. In particular, we aimed to describe the prevalence of THM use, the timing and effects of THM use, reasons reported for THM use and factors associated with THM use.
Methods
Literature Search
In June 2013 we searched Ovid MEDLINE (1946 to present) including in-process and non-indexed citations, Ovid EMBASE (1974 to present), and Web of Knowledge, for studies which investigated the use of THM among hypertensive patients living in SSA. A detailed search using words, phrases, and controlled vocabulary was created by an information specialist with input from a clinical pharmacologist and two board certified internal medicine physicians. The search strategies were peer reviewed by a second information specialist to ensure high methodological quality. Key words and search terms for each database are provided in Appendix A. The search was not limited to a specific language, date, or publication status. Additional references were found through reviewing the reference lists and related articles of included studies.
Two independent reviewers sorted references based on title and abstract according to predetermined inclusion and exclusion criteria. Differences were resolved through discussion with a third reviewer. References marked for inclusion were obtained, read in full, and marked for inclusion or exclusion.
References were included if they enrolled participants aged 18 years old and above currently living in SSA who were suffering from arterial HTN and described the prevalence of THM use among hypertensive patients. References were excluded if they included pediatric data but did not report data separately for adults, if they included patients outside of SSA and did not report data separately for those living in SSA, or if they included less than 10 patients. References were also excluded if they were pharmacological studies, interventional trials, meta-analyses, reviews, editorial material, or guidelines. See Figure 1 for an explanation of how many references were retrieved and reasons for exclusion.
Figure 1.
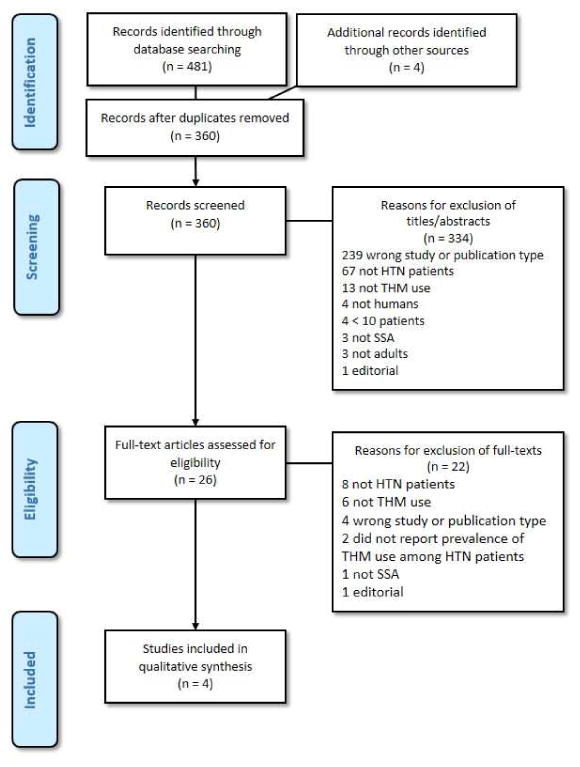
Flow diagram showing the description and selection process of studies included in the systematic review.
Data Extraction
A predefined data questionnaire template was used to extract data from the included studies by two reviewers independently. Any disagreements between the first two reviewers were resolved through independent review of a senior member of the research team. The following data points were extracted from each reference and included in the evidence table: sample size, average age ± SD, age range, gender distribution, prevalence of HTN, prevalence of complementary and alternative CAM) use, prevalence of THM use, source of THM prescription, types of THM used, factors associated with and reasons stated for THM use, timing of HTM use, and effects of THM use. Risk of selection bias was scored on a three point scale with 1 representing a randomly-selected, representative sample of the population, 2 representing a non-random sample of the community, and 3 representing a hospital-based sample. Risk of measurement bias was also scored on a 3 point scale with 1 representing biologically confirmed THM use, 2 representing self-reported THM use, and 3 representing THM use reported by someone other than the patient.
Results
Study Selection
For details of the study selection process, see Figure 1 for a PRISMA diagram. A systematic search of the literature revealed a total of 481 references: 58 from Ovid MEDLINE, 172 from Ovid Embase, and 251 from Web of Knowledge. An additional 4 references were found through hand searching reference lists. After removal of duplicates, 360 references remained. The titles and abstracts were reviewed, and 334 references were excluded. The remaining 26 were reviewed in full text and an additional 22 were excluded. Data extraction was completed on the remaining 4 references.
Characteristics of Selected Studies
For details of study characteristics, see Table 1. Of the 4 studies included, 1 was conducted in South Africa [16], and 3 were conducted in Nigeria [25–27]. The 3 studies from Nigeria all took place in an urban setting. Two were conducted in an urban hospital clinic [25,26], and 1 was conducted in an urban general population [27]. The 1 study from South Africa was conducted in a rural hospital clinic [16]. The sample size ranged from 100 to 480 participants. All 4 articles dealt exclusively with hypertensive patients [16,25–27]. The 3 references that included gender distribution reported a majority of respondents were female (60-67%)[16,25,27]. The average age of study participants was 55.1-60.7 years.
Table 1.
Characteristics of included studies of THM use among adults with HTN in SSA.
| Study | Country | Setting | Sample Frame | Sample Size | Average Age ± SD (years) | Female Gender (%) | Risk of Selection Bias (1-3) |
|---|---|---|---|---|---|---|---|
| Amira 2007 | Nigeria | Urban | Hospital | 225 | 55.1 ± 12.4 | 135/256 (60%) | 3 |
| Olisa 2009 | Nigeria | Urban | Hospital | 480 | 60.33 ± 16.33 | NR | 3 |
| Osamor 2010 | Nigeria | Urban | Population | 440 | 60 ± 12 | 287/440 (65.23%) | 1 |
| Peltzer 2004 | South Africa | Rural | Hospital | 100 | 60.7 ± 9.8 | 67/100 (67%) | 3 |
Key: SD: Standard deviation. IQR: Interquartile range. NR: Not reported. HTN: hypertension.
Prevalence of CAM/THM Use
For details about the prevalence of CAM and THM use, see Table 2. The rate of CAM use (inclusive of THM) was reported by 3 studies and ranged from 29.1-75% [16,25,27], and the average was 47.7%. The rural study from South Africa reported a much higher rate of CAM use (75%) [16] than the 2 studies from Nigeria (29.1-39.1%) [25,27]. THM use in the 4 studies ranged from 25% to 65% with an average of 38.6%. The rural study from South Africa reported higher rate of THM use (65%) [16] than the 3 studies from Nigeria (25%-37.77%) [25–27]. In the three studies that reported both CAM use and THM use, THM use represented the overwhelming majority of CAM use (86.7%-96.6%) [16,25,27].
Table 2.
The prevalence of CAM and THM use among adults with HTN in SSA.
| Study | Patients Using CAM | Patients Using THM | THM use as a % of CAM use |
|---|---|---|---|
| Amira 2007 | 88/225 (39.1%) | 85/225 (37.77%) | 85/88 (96.6%) |
| Olisa 2009 | NR | 120/480 (25%) | NR |
| Osamor 2010 | 128/440 (29.1%) | 118/440 (26.8%)* | 118/128 (92.2%)* |
| Peltzer 2004 | 75/100 (75%) | 65/100 (65%)† | 65/75 (86.7%) |
Key: CAM: Complementary and alternative medicine. THM: Traditional herbal medicine. HTN: Hypertension. NR: Not reported.
Percentage is the sum of THM mentioned as being commonly used by all CAM users
Sum of home remedies (39%) and traditional healing herbs (26%). Categories were not mutually exclusive, so actual % may be lower.
Timing and Effects of THM Use
Results regarding the timing and effects of THM use are summarized in Table 3. Two studies specifically reported that patients with HTN used THM and allopathic medicines concurrently [25,26], although only one quantified the number of THM users who were also using allopathic medicines (47.5%) [26]. Only one study [25] compared the blood pressures between the patients who reported using allopathic medications alone and those who reported using both allopathic and THM and reported no difference. The other three studies did not report any outcomes in those who were taking THM [16,26,27]. One study reported reasons for stopping THM among a small fraction of the study population (<5%) that had formerly used THM [26]. They found that 1.5% of their total study population stopped using THM due to inefficacy and 3% stopped using THM due to improvement of their disease.
Table 3. The timing and general effects of THM use.
| Study | Timing of THM use | General effects of THM |
|---|---|---|
| Amira 2007 | Concurrent use of THM and allopathic (not quantified) | No change in BP control between THM+allopathic and allopathic alone. |
| Olisa 2009 | Concurrent use of THM and allopathic 57/120 (47.50%) | Only reported in the 4.5% of patients who stopped using THM. |
Key: THM: Traditional herbal medicine. BP: Blood pressure. NR: Not reported.
Reasons for THM use
For reasons provided and factors associated with THM use, see Table 4. One study [26] reported why patients used THM. These included 1) perceived failure of allopathic medicines (31.73%), 2) relatively high cost of allopathic medicines (23.08%), 3) social cultural practices and/or herbal knowledge (20.19%), 4) poor accessibility to medical facilities (19.23%), 5) safety concerns about allopathic medicines (9.62%), 6) uncaring attitudes of hospital staff (6.73%). Other reasons reported for THM use included prior phobia to hospitals, curiosity about using THM and pressure from herbal sellers.
Table 4. Associated factors and reasons for THM use.
| Study | Associated with THM Use among HTN Patients | Reasons for THM Use |
|---|---|---|
| Olisa 2009 | Higher THM Use: Increased age (p < 0.001) |
|
| Lower THM Use: NR | ||
| Osamor 2010 |
Higher THM Use:
|
NR |
| Lower THM Use: Belief that HTN is preventable: OR 0.57, CI 0.36-0.89, p = 0.014. |
Key: CAM: Complementary and alternative medicine. HTN: Hypertension. THM: Traditional herbal medicine. OR: Odds ratio. CI: Confidence interval. NR: Not reported.
Factors Associated with THM Use
Factors which were statistically associated with THM use were reported by 2 studies [26,27]. One found that increased age was associated with THM use (p<0.001) [26]. The other found that three factors with were positively associated with increased THM use: 1) male sex, RR 2.58 (CI 1.66-3.99, p<0.0001), 2) belief in a supernatural cause of HTN, OR 2.11 (CI 1.18-3.78, p=0.012), and 3) a family history of HTN, OR 1.78 (CI 1.02-3.10, p=0.042) [27]. Belief that HTN is preventable was associated with decreased THM use, OR 0.57 (CI 0.36-0.89, p=0.014) [27].
Types and Sources of THM
For details of the types and sources of THM used, see Table 5. The three studies from Nigeria each asked study participants about the names of plants they used [25–27]. The list included “native herbs,” ginger, garlic, bitter leaf (vernonia amygdalina), aloe vera, azadirachta indica, allium sativa, tamarindus indica, hyenia thebacia, ocimum basil, carica papaya, adamsonia digitata, gacinia kola, zingiber officinalis, hymenocardia acida, melia azederach, mannix cymbopogon, piliostigma reticulatum, adeola herbal mixture, keys herbal mixture, herbal viagra, cassia alata, jatropha curcas, ximenis americana, moringa oleifera, kalms, and true man's capsule. Only one study reported on the specific preparations used [26]. Patients reported using preformulated THM from herb sellers, extracts that needed to be dissolved (in water, lime juice, or corn pap), steam inhalation, single herbs, and mixtures of herbs. Sources of THM were mentioned by 3 studies [16,26,27] and included open markets, friends, traditional healing homes, pharmacies, buses, spiritual pharmacies, traditional healers and faith healers.
Table 5. Plants, preparations used and the sources of THM.
| Study | Plants | Preparations | Sources |
|---|---|---|---|
| Amira 2007 | Native herbs, ginger, garlic, bitter leaf (vernonia amygdalina), aloe vera | NR | NR |
| Olisa 2009 | Azadirachta indica, allium sativa, aloe vera, tamarindus indica, hyenia thebacia, ocimum basil, carica papaya, adamsonia digitata, gacinia kola, zingiber officinalis, hymenocardia acida, melia azederach, mannix, cymbopogon, piliostigma reticulatum, adeola herbal mixture, Keys herbal mixture, herbal viagra, cassia alata, jatropha curcas, ximenis americana, moringa oleifera, kalms, true man's capsule, and garlic |
|
Open markets, friends, traditional healing homes, pharmacies and buses |
| Osamor 2010 | Herbs, garlic | NR | Traditional healers and spiritual pharmacies |
| Peltzer 2004 | NR | NR | Traditional healers and faith healers |
Key: THM: Traditional herbal medicine. HTN: Hypertension. NR: Not reported.
Discussion
THM use is very common among adults with HTN in SSA. Among hypertensive adults enrolled in the 4 studies included in this systematic review, more than one third reported using THM at the time of the study [16,25–27]. Rates of THM use varied considerably by country with 65% of adults in rural South Africa reporting THM use compared to 30% of adults from urban Nigeria. In these populations, THM use was the dominant form of CAM, accounting for 86.7-96.6% of all CAM use. The rates of THM use among adults with HTN in SSA were higher than those reported in 2 recent studies from the UK [24] and India [23] that found a prevalence of 28.8% and 14.4% respectively. Several studies explore the types of THM used to treat hypertensive patients [28–30], but very few quantify the amount of THM use. The high prevalence of THM use among adults with HTN in all 4 of these studies highlights the importance of considering the possible effects of THM use on HTN treatment and control in SSA.
Lack of knowledge, traditional beliefs and health systems deficiencies are 3 important factors associated with THM use among adults with HTN in these studies. Perceived failure of allopathic medications was the most common reason reported for THM use according to 1 study [26], and belief that HTN is both unpreventable and has a supernatural cause were factors associated with hypertension in another study [27]. In order to improve knowledge about potential effects of THM, community education campaigns are needed [7,31]. In addition, healthcare workers should utilize every interaction with hypertensive adults to ask about THM use and to consider the effects of THM on HTN control. Finally, health systems strengthening is needed to reduce the relatively high cost of allopathic medications, increase access to medical facilities and counteract the perception of uncaring attitudes of hospital staff.
Concurrent use of THM and allopathic medications seems to be common among adults with hypertension in SSA. In 1 study, half of HTN patients who were taking THM were also taking allopathic medications [26]. The high prevalence of concurrent THM and allopathic medicine use has been documented in other chronic diseases such as HIV in SSA [32,33]. The potential for therapeutic interactions between allopathic medication and THM is high with concomitant use. THM are known to have an effect on both the cardiovascular system and on blood pressure control [34–37]. Interactions may include altered drug metabolism, exaggerated hypotensive effect, or decreased HTN control. Since adults in SSA rarely volunteer information about THM use to their physicians [38], careful and non-judgmental history taking is essential.
Despite the high prevalence of THM use among African adults with HTN, the authors were surprised to discover that little data exists regarding THM use among adults with HTN in SSA. Although recording THM use is part of the WHO STEPS instrument for NCD risk factor screening [39], it is not systematically reported in studies of HTN in SSA. Even among the 4 studies that were included in this review, data regarding the prevalence, timing and reasons for THM use were not reported in a standardized manner. Physiologic outcomes (e.g. blood pressure measurements) were only reported in one study, and only 2 countries in SSA were represented by these 4 studies. Clearly there is an urgent need for more research regarding THM use among adults with HTN in SSA. Future studies should document the specific types of THM ingested by patients, physiologic effects of specific THM and any interactions with allopathic cardiovascular medications. Prospective cohort studies documenting the timing and impact of THM use on the natural history of HTN would be particularly valuable.
Conclusions
In conclusion, according to this systematic review of the current literature, >1/3 of adults with HTN in SSA use THM. Half of these patients use THMs concurrently with allopathic medicine. Major drivers of THM use are lack of knowledge regarding HTN, traditional cultural beliefs and weakness in the current health systems for HTN primary care in SSA. Health care workers in SSA should screen for THM use among adults with HTN. In addition, both community education and opportunistic patient education are needed to improve knowledge about interactions between THM and allopathic medications. Primary healthcare systems for HTN diagnosis and treatment need to be less expensive, more available and respectful. Finally, more research is urgently needed to define the impact of THM use on HTN control and outcomes so that their beneficial effects can be leveraged and their negative effects avoided.
Acknowledgments
This project was supported in part by grants from the United States National Institute of Health/National Institute of Allergy and Infectious Diseases (AI098627), the National Institutes of Health Fogarty International Center (R25TW009337) and a United States Agency for International Development (USAID) leadership training program.
Luke R. Smart has received a grant from the National Institutes of Health Fogarty International Center (Grant #: R25TW009337).
Amara Frumkin has received paid travel accommodations from Yale Global Health Field Research Initiative.
Daniel W. Fitzgerald has received a grant from the United States National Institutes of Health, National Institute of Allergy and Infectious Diseases (Grant Number: K24 AI098627) and payments from the United States Agency for International Development (USAID) leadership training program.
Appendix A: Database Search Strategy
Medline (OVID SP)
#1 exp africa south of the sahara/
#2 (africa* adj (central or east or eastern or west or western or south or southern) ).mp
#3 (subsahara* or sub-sahara* or “sub sahara*”).mp
#4 (cameroon* or central africa* republic or chad or chadian or congo* or democratic republic of the congo* or equatorial guinea* or gabon*).mp
#5 (burundi* or djibouti* or eritrea* or ethiopia* or kenya* or rwanda* or somalia* or sudan* or tanzania* or uganda*).mp
#6 (angola* or botswana* or lesotho* or malawi* or mozambique* or namibia* or south africa* or swaziland* or zambia* or zimbabwe*).mp
#7 (benin* or “burkina faso*” or “cape verde*” or “cote d'ivoire*” or “ivory coast” or gambia* or ghana* or guinea* or guinea-bissau* or “guinea bissau*” or liberia* or mali or malian or mauritania* or niger* or nigeria* or senegal* or “sierra leone*” or togo*).mp
#8 or/1-7
#9 exp hypertension/ or exp antihypertensive agents
#10 (hypertensi* or antihypertensi*).mp
#11 ((high or increased or elevated) adj blood pressure).mp
#12 or/9-11
#13 medicine, african traditional/ or medicine, traditional/
#14 (african traditional medicine or traditional healing or traditional healer* or african medicine or ethnomedicine* or native medicine or ethnopharmaceutical* or ethnobotanical* or natural remed*).mp
#15 or/13-14
#16 8 and 12 and 15
Embase (OVID SP)
#1 exp Africa south of the sahara/
#2 (africa* adj (central or east or eastern or west or western or south or southern) ).mp
#3 (subsahara* or sub-sahara* or “sub sahara*”).mp
#4 (cameroon* or central africa* republic or chad or chadian or congo* or democratic republic of the congo* or equatorial guinea* or gabon*).mp
#5 (burundi* or djibouti* or eritrea* or ethiopia* or kenya* or rwanda* or somalia* or sudan* or tanzania* or uganda*).mp
#6 (angola* or botswana* or lesotho* or malawi* or mozambique* or namibia* or south africa* or swaziland* or zambia* or zimbabwe*).mp
#7 (benin* or “burkina faso*” or “cape verde*” or “cote d'ivoire*” or “ivory coast” or gambia* or ghana* or guinea* or guinea-bissau* or “guinea bissau*” or liberia* or mali or malian or mauritania* or niger* or nigeria* or senegal* or “sierra leone*” or togo*).mp
#8 or/1-7
#9 exp hypertension/ or exp antihypertensive agent
#10 (hypertensi* or antihypertensi*).mp
#11 ((high or increased or elevated) adj blood pressure).mp
#12 or/9-11
#13 african medicine/ or herbal medicine/
#14 traditional healer/ or traditional medicine/
#15 (african traditional medicine or african medicine or native medicine or native remed*).mp
#16 (tradition$ adj3 (healing or healer* or healed) ).mp
#17 (ethnomedicine* or ethnopharmaceutical* or ethnobotanical*).mp
#18 or/13-17
#19 8 and 12 and 18
Web OF KNOWLEDGE (Thomson Reuters)
#1 Topic=(cameroon* OR chad OR chadian OR congo* OR “central africa* republic” OR “democratic republic of the congo*” OR equatorial guinea* OR gabon*) OR Topic=(burundi OR djibouti* OR eritrea* OR ethiopia* OR kenya* OR rwanda* OR somalia* OR sudan* OR tanzania* OR uganda*) Timespan=All years Search language=English
#2 Topic=(angola* OR botswana* OR lesotho* OR malawi* OR mozambique* OR namibia* OR “south africa*” OR swaziland*) OR Topic=(zambia* OR zimbabwe* OR benin* OR “burkina faso*” OR “cape verde*” OR “cote d'ivoire*” OR “ivory coast”) OR Topic=(gambia* OR ghana* OR guinea* OR guinea-bissau* OR “guinea bissau*” OR liberia* OR mali OR malian) Timespan=All years Search language=English
#3 Topic=(mauritania* OR niger* OR nigeria* OR senegal* or “sierra leone*”) Timespan=All years Search language=English
#4 Topic=((africa OR african) NEAR/2 subsahara*) Timespan=All years Search language=English
#5 Topic=((africa OR african) NEAR/2 sub-sahara*) Timespan=All years Search language=English
#6 Topic=((africa OR african) NEAR/2 “sub sahara*”) Timespan=All years Search language=English
#7 Topic=((africa OR african) NEAR/2 (central OR east OR eastern OR west OR western OR south or southern)) Timespan=All years Search language=English
#8 #7 OR #6 OR #5 OR #4 OR #3 OR #2 OR #1 Timespan=All years Search language=English
#9 Topic=(hypertensi* OR antihypertensi*) Timespan=All years Search language=English
#10 Topic=((“blood pressure”) NEAR/2 (high OR increased OR elevated)) Timespan=All years Search language=English
#11 #10 OR #9 Timespan=All years Search language=English
#12 Topic=(ethnobotanical* OR ethnopharmaceutical* OR ethnomedicine) Timespan=All years Search language=English
#13 Topic=(africa* NEAR/2 medicine) Timespan=All years Search language= English
#14 Topic=(native NEAR/2 (medicine OR remed*)) Timespan=All years Search language=English
#15 Topic=(folk NEAR/2 medicine) Timespan=All years Search language=English
#16 Topic=(traditional NEAR/2 (heal* OR medicine OR remed*)) Timespan=All years Search language=English
#17 Topic=(natural NEAR/2 remed*) Timespan=All years Search language=English
#18 #17 OR #16 OR #15 OR #14 OR #13 OR #12 Timespan=All years Search language=English
#19 #18 AND #11 AND #8 Timespan=All years Search language=English
Footnotes
Compliance with Ethics Guidelines: Conflict of Interest: Anthony C. Liwa, Helen-Ann B. Epstein, and Robert N. Peck declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent: This article does not contain any studies with human or animal subjects performed by any of the authors.
References
- 1.Zein ZA, Assefa M. Blood-pressure levels and hypertension in rural Ethiopian communities. Ethiop Med J. 1986;24:169–78. [PubMed] [Google Scholar]
- 2.Department of Cardiology Cairo University Faculty of Medicine and Qalyub Training and Demonstration Centre. Qalyub heart survey. Bull Egypt Soc Cardiol. 1958;1:99–105. [Google Scholar]
- 3.Donnison C. Blood Pressure in the African Native: Its bearing upon the aetiology of hyperpiesia and arterio-sclerosis. Lancet. 1929;213:6–7. [Google Scholar]
- 4•.Twagirumukiza M, De Bacquer D, Kips JG, de Backer G, Stichele R Vander, Van Bortel LM. Current and projected prevalence of arterial hypertension in sub-Saharan Africa by sex, age and habitat: an estimate from population studies. J Hypertens. 2011;29:1243–52. doi: 10.1097/HJH.0b013e328346995d. This study is a systematic review of hypertension prevalence in sub-Saharan Africa It compares urban versus rural rates and provides both curent and projected estimates of the total number of people with hypertension in sub-Saharan Africa. [DOI] [PubMed] [Google Scholar]
- 5.Njelekela M, Negishi H, Nara Y, Tomohiro M, Kuga S, Noguchi T, et al. Cardiovascular risk factors in Tanzania: a revisit. Acta Trop. 2001;79:231–9. doi: 10.1016/s0001-706x(01)00134-6. [DOI] [PubMed] [Google Scholar]
- 6.Njelekela M, Sato T, Nara Y, Miki T, Kuga S, Noguchi T, et al. Nutritional variation and cardiovascular risk factors in Tanzania--rural-urban difference. S Afr Med J. 2003;93:295–9. [PubMed] [Google Scholar]
- 7.Addo J, Smeeth L, Leon DA. Hypertension in sub-saharan Africa: a systematic review. Hypertension. 2007;50:1012–8. doi: 10.1161/HYPERTENSIONAHA.107.093336. [DOI] [PubMed] [Google Scholar]
- 8.World Health Organization. Global Status Report on Noncommunicable Diseases 2010. Geneva, Switzerland: WHO Press; 2011. [Google Scholar]
- 9.Mash B, Fairall L, Adejayan O, Ikpefan O, Kumari J, Mathee S, et al. A morbidity survey of South African primary care. PLoS One. 2012;7:e32358. doi: 10.1371/journal.pone.0032358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kolo PM, Jibrin YB, Sanya EO, Alkali M, Peter Kio IB, Moronkola RK. Hypertension-related admissions and outcome in a tertiary hospital in northeast Nigeria. Int J Hypertens. 2012;2012:960546. doi: 10.1155/2012/960546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mensah GA. Epidemiology of stroke and high blood pressure in Africa. Heart. 2008;94:697–705. doi: 10.1136/hrt.2007.127753. [DOI] [PubMed] [Google Scholar]
- 12.Peck RN, Green E, Mtabaji J, Majinge C, Smart LR, Downs JA, et al. Hypertension-related diseases as a common cause of hospital mortality in Tanzania: a 3-year prospective study. J Hypertens. 2013;31:1806–11. doi: 10.1097/HJH.0b013e328362bad7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cappuccio FP, Micah FB, Emmett L, Kerry SM, Antwi S, Martin-Peprah R, et al. Prevalence, detection, management, and control of hypertension in Ashanti, West Africa. Hypertension. 2004;43:1017–22. doi: 10.1161/01.HYP.0000126176.03319.d8. [DOI] [PubMed] [Google Scholar]
- 14.Hendriks ME, Wit FWNM, Roos MTL, Brewster LM, Akande TM, de Beer IH, et al. Hypertension in sub-Saharan Africa: cross-sectional surveys in four rural and urban communities. PLoS One. 2012;7:e32638. doi: 10.1371/journal.pone.0032638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dewhurst MJ, Dewhurst F, Gray WK, Chaote P, Orega GP, Walker RW. The high prevalence of hypertension in rural-dwelling Tanzanian older adults and the disparity between detection, treatment and control: a rule of sixths? J Hum Hypertens. 2013;27:374–80. doi: 10.1038/jhh.2012.59. [DOI] [PubMed] [Google Scholar]
- 16.Peltzer K. Health beliefs and prescription medication compliance among diagnosed hypertension clinic attenders in a rural South African Hospital. Curationis. 2004;27:15–23. doi: 10.4102/curationis.v27i3.994. [DOI] [PubMed] [Google Scholar]
- 17.Eddouks M, Maghrani M, Lemhadri A, Ouahidi ML, Jouad H. Ethnopharmacological survey of medicinal plants used for the treatment of diabetes mellitus, hypertension and cardiac diseases in the south-east region of Morocco (Tafilalet) J Ethnopharmacol. 2002;82:97–103. doi: 10.1016/s0378-8741(02)00164-2. [DOI] [PubMed] [Google Scholar]
- 18.Singh V, Raidoo DM, Harries CS. The prevalence, patterns of usage and people's attitude towards complementary and alternative medicine (CAM) among the Indian community in Chatsworth, South Africa. BMC Complement. Altern Med. 2004;4:3. doi: 10.1186/1472-6882-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.World Health Organization. WHO Traditional Medicine Strategy 2002-2005. Geneva, Switzerland: WHO Press; 2002. [Google Scholar]
- 20.Oreagba IA, Oshikoya KA, Amachree M. Herbal medicine use among urban residents in Lagos, Nigeria. BMC Complement. Altern Med. 2011;11:117. doi: 10.1186/1472-6882-11-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21•.Grant SJ, Bin YS, Kiat H, Chang DHT. The use of complementary and alternative medicine by people with cardiovascular disease: a systematic review. BMC Public Health. 2012;12:299. doi: 10.1186/1471-2458-12-299. This article is a systematic review that describes the prevalence of both complementary and alternative medicine in general and herbal medicine specifically for the treatment of cardiovascular disease. It focuses on developed countries and also makes note of the lack of physician awareness of patients' use of these alternate therapies. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delgoda R, Ellington C, Barrett S, Gordon N, Clarke N, Younger N. The practice of polypharmacy involving herbal and prescription medicines in the treatment of diabetes mellitus, hypertension and gastrointestinal disorders in Jamaica. West Indian Med J. 2004;53:400–5. [PubMed] [Google Scholar]
- 23.Shafiq N, Gupta M, Kumari S, Pandhi P. Prevalence and pattern of use of complementary and alternative medicine (CAM) in hypertensive patients of a tertiary care center in India. Int J Clin Pharmacol Ther. 2003;41:294–8. doi: 10.5414/cpp41294. [DOI] [PubMed] [Google Scholar]
- 24.Gohar F, Greenfield SM, Beevers DG, Lip GYH, Jolly K. Self-care and adherence to medication: a survey in the hypertension outpatient clinic. BMC Complement. Altern Med. 2008;8:4. doi: 10.1186/1472-6882-8-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Amira OC, Okubadejo NU. Frequency of complementary and alternative medicine utilization in hypertensive patients attending an urban tertiary care centre in Nigeria. BMC Complement Altern Med. 2007;7:30. doi: 10.1186/1472-6882-7-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Olisa NS, Oyelola FT. Evaluation of use of herbal medicines among ambulatory hypertensive patients attending a secondary health care facility in Nigeria. Int J Pharm Pract. 2009;17:101–5. [PubMed] [Google Scholar]
- 27.Osamor PE, Owumi BE. Complementary and alternative medicine in the management of hypertension in an urban Nigerian community. BMC Complement Altern Med. 2010;10:36. doi: 10.1186/1472-6882-10-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gbolade A. Ethnobotanical study of plants used in treating hypertension in Edo State of Nigeria. J Ethnopharmacol. 2012;144:1–10. doi: 10.1016/j.jep.2012.07.018. [DOI] [PubMed] [Google Scholar]
- 29.Karou SD, Tchacondo T, Djikpo Tchibozo MA, Abdoul-Rahaman S, Anani K, Koudouvo K, et al. Ethnobotanical study of medicinal plants used in the management of diabetes mellitus and hypertension in the Central Region of Togo. Pharm Biol. 2011;49:1286–97. doi: 10.3109/13880209.2011.621959. [DOI] [PubMed] [Google Scholar]
- 30.Moshi MJ, Otieno DF, Weisheit A. Ethnomedicine of the Kagera Region, north western Tanzania. Part 3: plants used in traditional medicine in Kikuku village, Muleba District. J Ethnobiol Ethnomed. 2012;8:14. doi: 10.1186/1746-4269-8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31•.Ibrahim MM, Damasceno A. Hypertension in developing countries. Lancet. 2012;380:611–9. doi: 10.1016/S0140-6736(12)60861-7. This is a review article which describest the rates of awareness, treatment, and control of hypertension in developing countries. It also describes several risk factors that are specific to developing countries. [DOI] [PubMed] [Google Scholar]
- 32.Langlois-Klassen D, Kipp W, Jhangri GS, Rubaale T. Use of traditional herbal medicine by AIDS patients in Kabarole District, western Uganda. Am J Trop Med Hyg. 2007;77:757–63. [PubMed] [Google Scholar]
- 33.Bepe N, Madanhi N, Mudzviti T, Gavi S, Maponga CC, Morse GD. The impact of herbal remedies on adverse effects and quality of life in HIV-infected individuals on antiretroviral therapy. J Infect Dev Ctries. 2011;5:48–53. doi: 10.3855/jidc.1415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chavez ML, Jordan MA, Chavez PI. Evidence-based drug--herbal interactions. Life Sci. 2006;78:2146–57. doi: 10.1016/j.lfs.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 35.Izzo AA, Di Carlo G, Borrelli F, Ernst E. Cardiovascular pharmacotherapy and herbal medicines: the risk of drug interaction. Int J Cardiol. 2005;98:1–14. doi: 10.1016/j.ijcard.2003.06.039. [DOI] [PubMed] [Google Scholar]
- 36•.Tabassum N, Ahmad F. Role of natural herbs in the treatment of hypertension. Pharmacogn Rev. 2011;5:30–40. doi: 10.4103/0973-7847.79097. This review article provies a thorough synopsis of herbs that are known to have hypotensive and antihypertensive properties. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vora CK, Mansoor GA. Herbs and alternative therapies: relevance to hypertension and cardiovascular diseases. Curr Hypertens Rep. 2005;7:275–80. doi: 10.1007/s11906-005-0025-0. [DOI] [PubMed] [Google Scholar]
- 38.Lubinga SJ, Kintu A, Atuhaire J, Asiimwe S. Concomitant herbal medicine and Antiretroviral Therapy (ART) use among HIV patients in Western Uganda: a cross-sectional analysis of magnitude and patterns of use, associated factors and impact on ART adherence. AIDS Care. 2012;24:1375–83. doi: 10.1080/09540121.2011.648600. [DOI] [PubMed] [Google Scholar]
- 39.World Health Organization. The STEPS Instrument and Support Materials [Internet] Available from http://www.who.int/chp/steps/instrument/en/index.html.


