Abstract
Despite the rapid growth of electronic health data, most data systems do not connect individual patient records to data sets from outside the health care delivery system. These isolated data systems cannot support efforts to recognize or address how the physical and environmental context of each patient influences health choices and health outcomes. In this article we describe how a geographic health information system in Durham, North Carolina, links health system and social and environmental data via shared geography to provide a multidimensional understanding of individual and community health status and vulnerabilities. Geographic health information systems can be useful in supporting the Institute for Healthcare Improvement’s Triple Aim Initiative to improve the experience of care, improve the health of populations, and reduce per capita costs of health care. A geographic health information system can also provide a comprehensive information base for community health assessment and intervention for accountable care that includes the entire population of a geographic area.
Donald Berwick and colleagues’ influential 2008 Health Affairs article, “The Triple Aim: Care, Health, and Cost,” describes a conceptual framework developed by the Institute for Healthcare Improvement for improving the US health care system.1 In the Triple Aim, the institute has identified three aims that must be simultaneously pursued: improve the experience of care, improve the health of populations, and reduce per capita costs of health care. In this article we introduce and describe information technology designed to support health systems and communities in achieving the Triple Aim. We demonstrate how this technology can be used to assess the health of a community and to deploy resources to integrate community and health care delivery system resources to improve population health. We describe three contemporary applications: a public health intervention strategy to prevent childhood lead exposure; a health services application to better manage patient flow to emergency departments (EDs); and a clinical population health application designed to care for people with diabetes at the individual, neighborhood, and county levels.
The Triple Aim has been used by a number of health systems as a conceptual framework for designing health system improvement programs.2–4 The abundant electronic health data that are accumulating are highly relevant to managing population health and developing new insights.5 Until recently, however, these data have been dispersed across many locations, with little integration.6,7 As integrated health systems are becoming more widespread, these data are being organized and stored within enterprise data warehouses, where they link clinical, laboratory, patient history, and prescription data.8
To make sense of the health records data, a number of challenging hurdles must be overcome (for example, interoperability, incompatibility, and unstructured data).9,10 Even if these obstacles are overcome, the underlying data systems often lack analytical tools that connect individual patient records to disparate data sets from outside the health care delivery information system.11 As a result, they fail to address how individual patients’ social and environmental contexts may influence health outcomes, or how evidence of these connections could be used in the broader context of population health and illness.
Health information systems typically contain information about patients and their clinical status (including medications, diagnoses, labs, and clinical documentation). Geographic health information systems (GHIS) integrate patient databases with census data and other information on where patients live, where they receive their care, the availability of community resources, and other characteristics of their communities.12
The key to such geographic or spatial analysis is that most data sets contain a variable that can be tied to a specific location, such as a state, county, ZIP code area, census block, or single address. Geographic analysis enables users to explore and overlay data by location. Additionally, adding geography to a large-scale health information system allows for an alternative method of linking data both from within and outside the system, providing a richer basis for analyzing and understanding patients’ choices and outcomes. Geographic health information systems also support the generation of clear and accessible maps and data reports that can be used to inform health management, community outreach, and policy design.
Constructing A Geographic Health Information System
DATA SYSTEMS
The geographic health information system described in this article is specific to Durham County, North Carolina. The system was constructed collaboratively among researchers and health system information systems personnel at Duke University and the University of Michigan, local and state public health agencies, and community stakeholders. It took three years of negotiations and relationship building to establish the trust needed for stakeholders to share the data required to build the system.
The system is maintained and operated by Duke Health Technology Solutions, the clinical informatics infrastructure of the Duke University Health System. It includes data from multiple local and national information sources. Individual patient data come from the Duke University Health System, a multihospital, multiclinic system with two hospitals in Durham County that cares for most of the county’s population. Birth and death records were obtained from the State of North Carolina’s Office of Vital Records. Also included are US census demographic data; county tax-parcel data; crime and housing quality data; environmental exposure and quality data; and health care, social, and community resources data.
The GHIS is continually refreshed with updated data and with the addition of new data layers as they are built or become available. Access to the systems’ capabilities and data is provided to specific participating users. For example, Duke University Health System physicians who would normally have access to patients’ medical records through an institutional electronic health record system can access all of the medical record data in the GHIS—as well as the social and environmental data, which, unlike patients’ medical record data, are not privacy protected. Public health professionals can access aggregated data in the system for their purposes without breaching patient confidentiality.
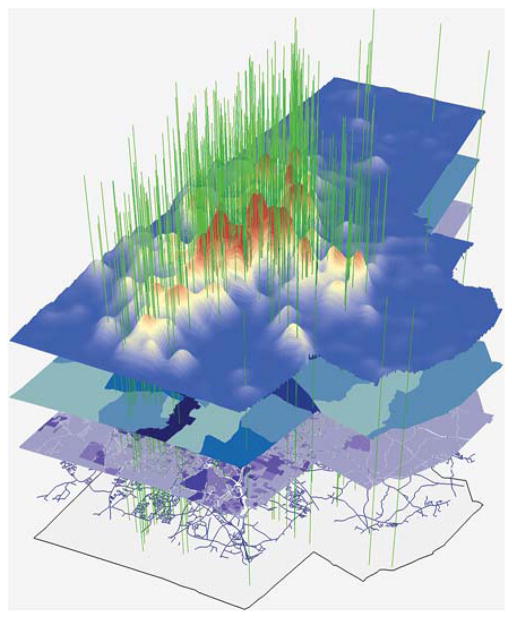
Exhibit 1 depicts the terrain of diabetes for Durham County and illustrates the relationships we are building across the major data domains, with clinical, billing, cost, environmental, demographic, community resources, birth record, and death record data all linked via shared geography. The top layer’s simulated peaks, colored red, depict the county’s highest concentrations of diabetes patients. The next layer down, in shades of blue, represents census block groups shaded to reflect the percentage of households headed by a single female parent—an indicator of socioeconomic status. Below that, another layer, this one in shades of purple, depicts individual tax-parcel boundaries shaded according to the assessed value of the parcel—another indicator of economic status. The bottom layer maps the county boundary and streets. The vertical green spines represent the latitude and longitude coordinates of where diabetes patients live and locations of key social or commercial institutions, such as churches or pharmacies, that can be used to link all of these disparate data sets together based on shared geography.
Exhibit 1.
Example Of Geographic Health Information Systems (GHIS) For Mapping The Terrain Of Diabetes In Durham County, North Carolina
SOURCE Duke Health Technology Solutions Decision Support Repository (DSR), using information on boundaries and streets layers from the US Census Bureau Geography Division, census 2010; and tax-parcel data from the Durham County Tax Assessor. NOTE The elements of this GHIS map are explained thoroughly in the text.
PATIENT DATA
The patient data include all patients using the Duke University Health System. Duke’s enterprise data warehouse, also known as the Decision Support Repository (DSR), has been in existence for more than a decade. Originally built for financial analysis and health system planning purposes, the DSR holds sixteen years of patient, diagnosis, and procedure data gathered from billing systems. Clinical data have been added, and the DSR now includes laboratory results, computerized physician order entries, medication order and fulfillment data, patient allergy data, data from perioperative systems, data on vital signs, patient home address and other encounter data, and a variety of safety information including adverse drug event surveillance information.
It is recognized that billing codes are suboptimal for identifying clinical phenotypes or diagnoses. The DSR is progressively being populated by standardized clinical data vetted by a health system governance group. This group consists of health system leaders, researchers with analytical skills, and academic leaders. All members participate in planning and resource allocation and in resolving issues concerning access to data.13 Researchers have used these data in numerous studies with Institutional Review Board approval, quality improvement initiatives, extension programs, and regulatory reports.
As an example of how the DSR can be leveraged, we constructed a data set of all patient records in the DSR from January 1, 2007, to December 31, 2009, from ZIP codes that lie in whole or in part in Durham County. This database includes demographic, medical, administrative, and laboratory data on the patients. From these data, we identified some 216,000 unique individuals residing in Durham County, corresponding to roughly 80 percent of the total county population. The average patient visited Duke University Health System facilities or providers a dozen times during the three-year period, which indicates that most of these patients were frequent users of the health system. Having such a high percentage of the county population captured in a single database enables a true community health assessment, in which most individuals are accounted for, instead of a representative sample. The DSR also supports those making decisions about deploying resources to improve population health, unbiased by adverse selection.14
SPATIALLY REFERENCING THE DSR
We used the geographic information systems software ArcGIS to place all patients on the map of Durham County by matching residential addresses with addresses from the county tax assessor’s office (a process called “parcel geocoding”). This contrasts with the typical public health approach where data are most commonly geocoded to the county, ZIP code, or census tract areal scale. Our approach allows us to link the patient data to a variety of other databases (see below). We successfully mapped the residential addresses of roughly 95 percent of Durham County patients, which is considered a very high proportion in most spatial analyses of health data.
PATIENT CONTEXT DATA
In addition to the DSR patient data, our spatial data architecture includes demographic data tables from the 1990, 2000, and 2010 US censuses; and birth and death records for Durham County, linked to patient records where possible. Also included are electronic city directories for businesses, institutions, and community resources; county tax assessor data for information on age of housing, zoning codes, land use codes, date remodeled (if any), building class or type, owner address, physical address, owner (versus renter) occupancy, heating/cooling system, and assessed tax value; and public transportation routes. Data on environmental exposures (for example, air pollution data) and community characteristics—such as recreational facilities, green spaces, sidewalks, day care centers, physicians’ offices, schools, libraries, athletic programs, religious institutions, traffic patterns, crime, abandoned housing, housing code enforcement actions, and manufacturing facilities—are also part of the system. These additional data layers were developed over the course of several years as project needs evolved. We are rapidly developing the equivalent layers in three additional counties in the southern United States with the help of a Center for Medicare and Medicaid Innovation grant.
Applying GHIS To Support The Triple Aim
The geographic health information system can be leveraged to support projects focused on achieving the Triple Aim. Here we present three examples from Durham County. Each application uses different subsets of the data embedded in the larger GHIS.
CHILDHOOD LEAD EXPOSURE
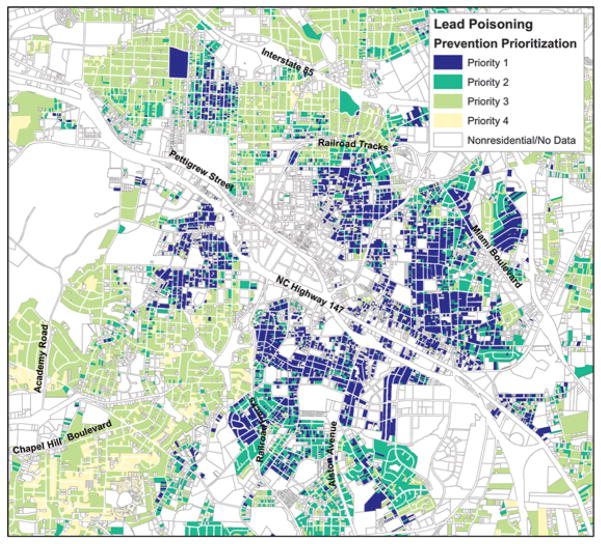
As an example of a GHIS public health application, Exhibit 2 presents a sample map from a Durham County project focused on reducing childhood lead exposure. This project created a map that models household-level childhood lead exposure risk levels using a combination of county tax assessor data, blood lead screening data from clinic visits, and census data. This project required only non-DSR data to accomplish its goals. The map uses spatial analysis to categorize lead risk levels at the individual tax-parcel level. The model was validated by conducting in-home environmental sampling.15
Exhibit 2.
Childhood Lead Exposure Risk Model For Durham, North Carolina
SOURCE Modeled lead exposure risk based on lead screening data provided by North Carolina Division of Public Health, Children’s Environmental Health Branch; and demographic data from the 2000 US census. NOTE The elements of this geographic health information system (GHIS) map are explained thoroughly in the text.
Exhibit 2 depicts the priority categories for residences in Durham. Dark blue represents priority 1 (highest risk) parcels, predicted to be most likely to contain lead paint hazards. Priority 2 and 3 parcels are colored medium and light green, respectively, and are less likely to contain lead paint hazards. Priority 4 (lowest risk) parcels are light yellow and least likely to contain lead paint hazards.
This project was developed in the early 2000s through collaboration with health care providers, community groups, and local and state agencies. Usefulness to key stakeholders was a critical component in the development of the lead exposure risk model. The Durham County Health Department and community advocacy groups quickly adopted the model for their purposes. In 2003 the health department revised its lead exposure screening strategy to take advantage of the model. Previously the department had used the standard lead exposure screening tool from the Centers for Disease Control and Prevention.16
The health department credits the model with contributing to a 600 percent increase in its capture rate of elevated blood lead levels in children, without a cost increase. It also uses the model to monitor progress in eliminating childhood lead exposure and to reach out preventively to new mothers who reside in homes at high risk for lead exposure. In addition, it proactively holds screening clinics in neighborhoods with a significant concentration of housing at high risk for lead exposure.
Community groups have also conducted door-to-door campaigns focusing on the model’s priority 1 houses in a given geographic area. The county’s housing department has used the model to prioritize the expenditure of housing rehabilitation funds. Widespread public dissemination of resources based on the model has transformed lead screening from a public health strategy in which families were passive recipients to one in which families living in housing at high risk for lead exposure are partners, armed with information that prompts them to ask their health care providers to screen their children for lead—and to advocate for improving housing quality. These resources included summaries of state-of-the-art knowledge of the impacts of low-level lead exposure and clinical recommendations from the Centers for Disease Control and Prevention.17
The use of this model improved family interactions with the county health department and clinics, and it protected more children from lead exposure. Perhaps most important, it allowed families to advocate for their children using a model that was widely embraced across the county.
EMERGENCY DEPARTMENT USE
Visits to hospital EDs have been rising steadily in the United States. Between 1997 and 2007 ED visits rose to 125 million visits annually—a 23 percent increase.18 Many of these visits could have been prevented with treatment in lower-cost, and arguably more effective, non-ED settings.19,20 Mirroring national trends, visits to the two hospital-based EDs in Durham County increased 33.8 percent from 2000 to 2010. Understanding the key drivers and spatial patterns of ED usage can improve the experience of care by directing patients to more appropriate settings or getting them into care before an emergency arises, and it can reduce per capita costs of health care—two of the three Triple Aim components.
To that end, we employed the GHIS to examine the association between patient and census block group characteristics and ED usage. We generated predicted probabilities of at least one ED visit in the past year, by race and insurance status, and for nonsmoking males ages 30–39. The predicted probabilities were generated by fitting mixed-effects logistic regression models that included patient-level predictors (age, race, sex, and insurance and smoking status); block group characteristics (age, race, sex, and education composition of the block group; percentage with below-poverty incomes; and percentage owner occupancy); and random intercepts for each block group.21 Maps were created using a manual six-class classification to display the four populations on the same scale.
As the maps in the online Appendix indicate,22 the lowest rates of ED use were among white, privately insured patients (upper left panel), and the highest rates were among African Americans without private insurance (lower right panel) (see Appendix Exhibit 1). These results were confirmed by generalized estimating equation models, which indicated that African Americans have 1.55 (95% confidence interval: 1.46, 1.65) times higher odds of one or more ED visits per year compared to whites. The models also indicate that patients without private insurance have 3.61 (95% CI: 3.47, 3.75) higher odds of at least one visit annually compared to those with private insurance. In addition, all four maps in the online Appendix show clear clustering of ED use in neighborhoods in the central part of the county (see Appendix Exhibit 1). In these areas, whites with private insurance, who typically have the lowest chances of going to the ED, have higher ED use rates than whites with private insurance in other areas.
Our next step is to identify what brought patients to the ED and identify how many of these visits might have been avoided with better access to primary care. We are now working with Duke University Health System leaders—in the ED, primary care, and departments that provide specialty care for disease endpoints often associated with ED visits—to consider the implications of this work for redesigning the delivery of key health services in these geographic hot spots.
These maps may be useful for the formation of partnerships among health care providers, families, and neighborhoods to create effective alternatives to the use of hospital-based EDs for primary care, and the underlying data provide a comprehensive picture of the community used in the Duke University Health System’s community needs assessment. A macrosystem redesign should provide better health outcomes by enabling earlier access to appropriate facilities in the neighborhood, thereby preempting clinical deterioration in a more efficient, lower-cost alternative setting and allowing EDs to focus on critically ill and injured patients.
MANAGING DIABETES AT THE INDIVIDUAL AND POPULATION LEVELS
According to 2011 figures, 18.8 million children and adults in the United States—roughly 6.0 percent of the total population—have diabetes.23 Estimates suggest that 7.0 million people are undiagnosed, making the true population burden more on the order of 8.3 percent.23 According to the North Carolina State Center for Health Statistics, roughly 7 percent of adults in Durham County stated in 2010 that they had been told by a doctor that they have diabetes.24 This contrasts with a 12.2 percent figure based on clinical indicators available within the DSR.
Using the standardized 2007–09 DSR data for Durham County described above, we identified 14,345 unique adult patients with an International Classification of Diseases, Ninth Revision (ICD-9), diagnosis code of diabetes mellitus within the patient data warehouse. We mapped these patients by, among other things, their residence and their level of hemoglobin A1c (HbA1c) monitoring and control. Exhibits in the online Appendix22 display the percentage of patients using the Duke University Health System with diabetes, the percentage of patients with diabetes for whom no HbA1c laboratory result was available, and the percentage of patients with diabetes whose HbA1c laboratory result was out of goal range (>7) (see Appendix Exhibit 2). Although some of these patients may have had their HbA1c checked at a non-Duke facility, these patients had an average of more than a dozen encounters with Duke providers per year.
The maps and analysis we produced are being used by a collaborative consisting of the Duke University Health System, University of Michigan, and Durham County Health Department to support the development and implementation of new individual and community-based diabetes intervention programs, funded by the Bristol-Myers Squibb Foundation. The approach is being replicated in Mingo County, West Virginia; Quitman County, Mississippi; and Cabarrus County, North Carolina, through a major Center for Medicare and Medicaid Innovation Health Care Innovations Challenges grant.
Community health workers are using the GHIS to create individualized diabetes management plans based on patients’ neighborhood contexts. GHIS applications in each of the four counties also support continuous individual, neighborhood, and community monitoring and evaluation of the impact of interventions. A modest improvement in the management of diabetes in the highest-risk patients would indicate that significant savings could be achieved while also improving outcomes.
The GHIS is especially potent in identifying pockets of individuals at very high risk for diabetes, where an intense investment of health care and social services could produce substantial improvement among those projected to have the most complications, as has been demonstrated in a similar effort in Camden, New Jersey. The Camden Coalition of Healthcare Providers has mapped a citywide health database and uses this information to target high-needs patients and develop neighborhood-based diabetes education programs.25 Thus, the combination of an intervention with community engagement, information system–based risk assessment, and use of the system to follow progress to enable continuous quality improvement offers promise for achieving the Triple Aim.
Discussion
There is growing recognition that fragmentation of care is a key factor in the poor health status of many Americans. Reducing or even eliminating fragmented care has been a central driver in the recent evolution of integrated health systems and accountable care organizations. As the Accountable Care Act’s implementation continues, organized delivery systems will assume accountability for population health manifested by community health assessments and accountability plans. Improving population health will require the use of comprehensive geographic systems to prevent delivery systems from employing adverse selection to make their metrics appear improved, leaving out neighborhoods or individuals at high risk.
The visualization capabilities made available through GHIS add an important tool for understanding and addressing critical issues in health care. In addition, since many health systems are in the midst of developing fully functional enterprise data warehouses, incorporating a GHIS into the development process is timely in terms of both data architecture and system costs.
CHALLENGES REMAINING
Challenges remain on many levels. For most of the United States, the primary challenge is the fragmented and unstructured data that populate electronic health records. The Duke University Health System’s data warehouse represents more than a decade of intensive efforts to develop a systemwide approach in which clinical, financial, and operational data are captured and curated to provide a structured data set that can be used for health care system operations, financial analysis, quality improvement, and clinical care.
Because of the unusual combination of the presence of a dominant health system in a single county and that system’s long history of collaboration with the public health department and federally qualified health center (the other major provider in the county), our system does not have to overcome the fragmentation characteristic of much of American health care. In our Health Care Innovations Challenges grant project, we are finding that issues related to fragmentation are not severe in rural counties, but they do constitute a major obstacle in urban areas, where competition among health care providers leads to difficulty in developing common data standards and to reluctance to share highly detailed data.
USING GHIS DATA
As data standards develop, additional hurdles will need to be overcome. For example, how can individual patients access and use the GHIS data? The concept of the use of an electronic health record by patients and families is just now evolving. In each of our examples, the spatial dimension enables strategic implementation of interventions at the level of the individual.
PATIENTS AND PROVIDERS
A map or risk algorithm score shared by a provider and a parent could motivate a family in a high-risk home to seek lead screening; a person with an acute illness could seek care at a convenient neighborhood urgent care facility; and a person with diabetes could track how his or her activity logs and food diaries correspond with blood sugar or blood pressure goals. While better navigation and information provide the substrate, more-sophisticated interactions with providers and systematic environmental improvement initiatives will be needed to produce a major change in health outcomes.
NEIGHBORHOODS
At the neighborhood level, meetings between health system leaders and communities could be enabled by sharing maps that “tell the story” of the health status and resources of the neighborhood compared with others in the county. The integration of graphic information in neighborhood meetings would allow community groups to visualize key issues and advocate for needed resources and services with government agencies and local businesses, while also working within the neighborhood to solve problems. A neighborhood with a high density of high-risk housing could advocate for housing code inspections and housing upgrades; a neighborhood with excessive use of hospital-based emergency care could work with the local hospital and health system to get a local urgent care facility; and a neighborhood with high rates of poorly controlled diabetes could call on the city or county government for appropriate access to safe places to exercise and improved grocery stores.
HEALTH PLANNERS
The combination of data and images of the data has also been instrumental in guiding the deployment of outpatient facilities in Durham County over the past several years, particularly the joint planning by the public health system, the federally qualified health center, and the Duke University Health System in placing clinics in strategic locations to optimize care access in disadvantaged neighborhoods with a high concentration of poor health outcomes.
At the county level, the ability to redesign systems using macrosystem data that are constantly updated is clear in all three cases. The equal application of resources for people and neighborhoods with very high and very low levels of appropriate self-care (low-risk housing, low use of emergency facilities, and well-controlled HbA1c) is wasteful, whereas focusing resources in areas of high risk is much more cost-effective.
ACHIEVING THE GOALS OF THE TRIPLE AIM
The spatially based organization and visualization provided by a GHIS can support progress toward all three elements of the Triple Aim. Partnerships between the health system and community would be enhanced by the ability to jointly view data displays on the key issues in the environment that may be affecting their health. Such data architectures could allow providers and patients to view, analyze, and interact with large and complex data sets through familiar map interfaces. For providers, the addition of spatially based applications could be used to understand patients more effectively within the context of their local environments. Providers, both individual and the health system as a whole, could use GHIS applications to identify gaps in care and to monitor specific health endpoints.
Patients could benefit from data and analysis that allowed them to advocate for healthful communities. If the spatial data architecture were married to the web-based patient interfaces being developed by many health systems, patients could better manage their health between visits by exchanging health data with their physicians and other health care staff (such as nurse educators, social workers, and nutritionists), who could in turn provide updated recommendations and information. This content might, for example, include maps depicting local walking trails, pharmacies, grocery stores, and the locations of health-related community events.
Redesign of the health care delivery system is facilitated by the GHIS. Given the comprehensive nature of the data, especially as we incorporate data from the federally qualified health center, population trends at the county level can be followed continuously without concern for adverse selection. GHIS can also be used to more effectively describe, longitudinally follow, and promote patients’ interaction with health services.
LIMITATIONS
Although the strengths of GHIS are significant, it is worth noting some important limitations. First, the use of most of these systems will be maximized only if all local health providers are willing and technologically prepared to participate in the hard work of developing an operational health information exchange. In the prototype described in this article, extensive meetings and negotiations have occurred between the health system and the local federally qualified health center, and data from the latter are only now becoming available. Second, some of the available advanced applications of a GHIS require knowledge of spatial statistics. However, we note that many helpful applications do not require any advanced knowledge of statistics.
Third, in presenting any maps or other visualizations from the GHIS in public settings, care must be taken to ensure that no protected information is presented. Providers and researchers are accustomed to thinking about protecting medical record data, but specialized training in confidentiality considerations in map graphics is necessary. Finally, achieving GHIS upgrades from a standard electronic health record will require enthusiasm and commitment from health system leaders.
Conclusion
The geographic health information system we describe demonstrates a scalable and replicable approach for integrating clinical and geospatial data for research, public health, health services, and clinical applications. It supports work to monitor population health, develop new care models, improve priority setting and decision making, and tailor public health interventions. By integrating multiple components into a comprehensive system, GHIS and associated analytical applications offer innovative strategies that can facilitate progress toward achieving the Triple Aim and, in so doing, can fundamentally change how health systems address the health needs of their communities.
Supplementary Material
Acknowledgments
This research was made possible by grants from the Centers for Medicare and Medicaid Services (1C1CMS331018-01-00); the Bristol-Myers Squibb Foundation; and the National Center for Research Resources (UL1RR024128), a component of the National Institutes of Health (NIH) and the NIH Roadmap for Medical Research. The article’s contents are solely the responsibility of the authors and do not necessarily represent the official view of any of the funding agencies.
Contributor Information
Marie Lynn Miranda, Email: mlmirand@umich.edu, Dean of and a professor in the School of Natural Resources and Environment and is a professor in the Department of Pediatrics, University of Michigan, in Ann Arbor.
Jeffrey Ferranti, Chief medical information officer and vice president for clinical informatics, and an assistant professor in newborn critical care, at Duke University Medical Center, in Durham, North Carolina.
Benjamin Strauss, Associate in research at the Nicholas School of the Environment, Duke University.
Brian Neelon, Statistician at the Nicholas School of the Environment, Duke University.
Robert M. Califf, Chancellor for clinical and translational research and a professor of medicine in the Division of Cardiology, Duke University Medical Center
NOTES
- 1.Berwick DM, Nolan TW, Whittington J. The Triple Aim: care, health, and cost. Health Aff (Millwood) 2008;27(3):759–69. doi: 10.1377/hlthaff.27.3.759. [DOI] [PubMed] [Google Scholar]
- 2.Klein S, McCarthy D. Genesys HealthWorks: pursuing the Triple Aim through a primary care–based delivery system, integrated self-management support, and community partnerships. New York (NY): Commonwealth Fund; 2010. Jul 1, p. 49. [Google Scholar]
- 3.Hester J., Jr Designing Vermont’s pay-for-population health system. Prev Chronic Dis. 2010;7(6):A122. [PMC free article] [PubMed] [Google Scholar]
- 4.Fisher ES, Berwick DM, Davis K. Achieving health care reform—how physicians can help. N Engl J Med. 2009;360(24):2495–7. doi: 10.1056/NEJMp0903923. [DOI] [PubMed] [Google Scholar]
- 5.Mayer-Schonberger V, Cukier K. Big data: a revolution that will transform how we live, work, and think. New York (NY): Eamon Dolan/Houghton Mifflin Harcourt; 2013. [Google Scholar]
- 6.Mathews SC, Pronovost PJ. The need for systems integration in health care. JAMA. 2011;305(9):934–5. doi: 10.1001/jama.2011.237. [DOI] [PubMed] [Google Scholar]
- 7.Institute of Medicine and National Academy of Engineering Roundtable on Value and Science-Driven Health Care. Engineering a learning healthcare system: a look at the future. Washington (DC): National Academies Press; 2011. [Google Scholar]
- 8.Garson K, Adams C. In: Seamons K, McBurnett N, Polk T, editors. Security and privacy system architecture for an e-hospital environment; Proceedings of the 7th Symposium on Identity and Trust on the Internet; Gaithersburg, MD. 2008 Mar 4–6; New York (NY): ACM; 2008. pp. 122–30. [Google Scholar]
- 9.Botsis T, Hartvigsen G, Chen F, Weng C. Secondary use of EHR: data quality issues and informatics opportunities. AMIA Summits Transl Sci Proc. 2010:1–5. [PMC free article] [PubMed] [Google Scholar]
- 10.Brailer DJ. Interoperability: the key to the future health care system. Health Aff (Millwood) 2005;24:w5-19-21. doi: 10.1377/hlthaff.w5.19. [DOI] [PubMed] [Google Scholar]
- 11.Wang T, Plaisant C, Quinn A, Stanchak R, Murphy S, Shneiderman B. In: Burnett M, Costabile MF, Catarci T, de Ruyter B, Tan D, Czerwinski M, et al., editors. Aligning temporal data by sentinel events: discovering patterns in electronic health records; Proceedings of the 26th annual CHI Conference on Human Factors in Computing Systems; Florence, Italy. 2008 Apr 5–10; New York (NY): ACM; 2008. pp. 457–66. [Google Scholar]
- 12.Bullen N, Moon G, Jones K. Defining localities for health planning: a GIS approach. Soc Sci Med. 1996;42(8):15. doi: 10.1016/0277-9536(95)00180-8. [DOI] [PubMed] [Google Scholar]
- 13.Payne PR, Embi PJ, Sen CK. Translational informatics: enabling high-throughput research paradigms. Physiol Genomics. 2009;39(3):131–40. doi: 10.1152/physiolgenomics.00050.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koepsell TD, Wagner EH, Cheadle AC, Patrick DL, Martin DC, Diehr PH, et al. Selected methodological issues in evaluating community-based health promotion and disease prevention programs. Annu Rev Public Health. 1992;13:31–57. doi: 10.1146/annurev.pu.13.050192.000335. [DOI] [PubMed] [Google Scholar]
- 15.Miranda ML, Dolinoy DC, Overstreet MA. Mapping for prevention: GIS models for directing childhood lead poisoning prevention programs. Environ Health Perspect. 2002;110(9):947–53. doi: 10.1289/ehp.02110947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Centers for Disease Control and Prevention. Screening young children for lead poisoning: guidance for state and local public health officials. Atlanta (GA): CDC; 1997. [Google Scholar]
- 17.Centers for Disease Control and Prevention. Preventing lead poisoning in young children. Atlanta (GA): CDC; 2005. [Google Scholar]
- 18.Owens PL, Mutter R. Emergency department visits for adults in community hospitals, 2008. Rockville (MD): Agency for Healthcare Research and Quality; 2010. Jan 1, (HCUP Statistical Brief No. 100) [PubMed] [Google Scholar]
- 19.Weinick RM, Burns RM, Mehrotra A. Many emergency department visits could be managed at urgent care centers and retail clinics. Health Aff (Millwood) 2010;29(9):1630–6. doi: 10.1377/hlthaff.2009.0748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Jayaprakash N, O’Sullivan R, Bey T, Ahmed SS, Lotfipour S. Crowding and delivery of healthcare in emergency departments: the European perspective. West J Emerg Med. 2009;10(4):233–9. [PMC free article] [PubMed] [Google Scholar]
- 21.Neelon B, Ghosh P, Loebs P. A spatial Poisson hurdle model for exploring geographic variation in emergency department visits. J R Stat Soc Ser A Stat Soc. 2013;176(2):389–413. doi: 10.1111/j.1467-985X.2012.01039.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.To access the Appendix, click on the Appendix link in the box to the right of the article online.
- 23.Centers for Disease Control and Prevention. National Diabetes Fact Sheet: national estimates and general information on diabetes and prediabetes in the United States. Atlanta (GA): CDC; 2011. [Google Scholar]
- 24.Centers for Disease Control and Prevention. Behavioral Risk Factor Surveillance System survey questionnaire. Atlanta (GA): CDC; 2010. [Google Scholar]
- 25.Brenner J. Building an accountable care organization in Camden, NJ. Prescriptions for Excellence in Health Care [serial online] 2010 Summer;(9) [cited 2013 Aug 12]. Available from: http://jdc.jefferson.edu/cgi/viewcontent.cgi?article=1075&context=pehc.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.