Abstract
Extrahepatic manifestations are frequently encountered among patients with chronic hepatitis C virus (HCV) infection. Many of these manifestations are autoimmune disorders, with added mortality and morbidity due to involvement of multiple organ systems. Symptoms of HCV infection and rheumatic diseases may be similar and include arthralgia, myalgia, arthritis, and vasculitis. Also, serologic abnormalities may be found in both cases. Some treatment modalities for HCV infection, including interferon therapy, may aggravate the symptoms of rheumatic diseases, thus confounding clinical presentation. It is imperative to distinguish whether symptoms such as arthralgia, myalgia, and arthritis occur in patients with HCV infection due to primary chronic HCV infection or to a newly developed rheumatologic disease process.
Keywords: Hepatitis C virus, rheumatologic implication, autoimmune disease
Hepatitis C virus (HCV) was first identified and cloned in 1989.1 The overall course of HCV infection is typically chronic, systemic, and asymptomatic.2 It is stated that approximately 3 to 4 million persons are newly infected with HCV each year. The World Health Organization estimates that 3% of the world’s population has chronic HCV infection.3 According to the US Centers for Disease Control and Prevention, approximately 2.7 million persons have chronic HCV infection. It has been reported that, every year, an estimated 30,000 new cases of infection occur in the United States, and the number of deaths annually due to HCV infection and HCV infection-related complications is nearly 10,000.4
The diagnosis of HCV infection is difficult because the course of the disease is asymptomatic. It is usually diagnosed incidentally by serologic screening or in relation to diagnosis of end-stage liver dis-ease.5 HCV infection primarily affects the liver; however, extrahepatic manifestations are not rare. Because there are so many extrahepatic manifestations, diagnosis can be challenging. Rheumatologic extrahepatic manifestations are observed in 2% to 38% of HCV-infected patients. This variability is attributed to the geographic region and design of the studies from which these statistics come.6-8 Rheumatologic extrahepatic symptoms include arthralgia (23%), paresthesia (17%), myalgia (15%), pruritus (15%), and sicca syndrome (11%).9 Knowing the extrahepatic manifestations of HCV infection is important in diagnosis and treatment of the disease.10
HCV has been known as a hepatotropic and also lymphotropic virus. This lymphotropism plays an important role in the pathogenesis of virus-related autoimmune diseases. Lymphotropism and chronic stimulation of the immune system by several viral proteins may be responsible for non-organ—specific autoantibody production, such as rheumatoid factor (RF) and cryoglobulins.11,12 Anti-cyclic citrullinated peptide (CCP) positivity is considered specific for a differential diagnosis of arthritis in patients infected with HCV and is more significant for rheumatoid arthritis (RA) than the other causes.13 Increased interleukin (IL)-6 levels are observed in rheumatoid and HCV-related arthritis, but the cause of this increase is not related to HCV viremia or elevated transaminase levels. Thus, increased IL-6 levels are considered to play the main role in both rheumatoid- and HCV-related arthritis.14
Cryoglobulinemia is the main HCV-related autoimmune entity, and the relationship between cryoglobuli-nemia and HCV infection is well identified. It has been observed that approximately 80% of patients with cryo-globulinemia are infected with HCV. Other rheumatic diseases, such as RA, systemic lupus erythematosus (SLE), Sjogren syndrome (SS), polyarteritis nodosa (PAN), sar-coidosis, antiphospholipid syndrome, and osteosclerosis, are observed in patients with HCV infection. The true causal relationship between these diseases and HCV has not been well established.15 RA, SLE, SS, and PAN comprise approximately 95% of the HCV infection—related autoimmune diseases.16
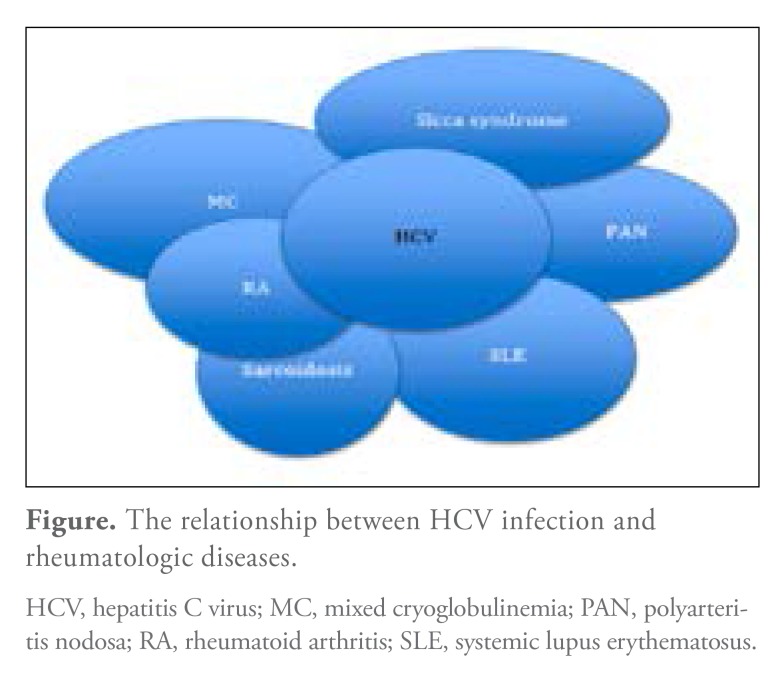
This review emphasizes the importance of identifying rheumatologic manifestations that may be identified during diagnosis, treatment, and follow-up of HCV-infected patients. Also presented are some data on whether rheu-matologic diseases that occur during the follow-up of HCV-infected patients are actually associated with HCV or primary rheumatic disorders (Figure).
Figure.
The relationship between HCV infection and rheumatologic diseases.
HCV, hepatitis C virus; MC, mixed cryoglobulinemia; PAN, polyarteri-tis nodosa; RA, rheumatoid arthritis; SLE, systemic lupus erythematosus.
Hepatitis C Virus and Rheumatoid Arthritis
Arthralgia is a frequent symptom in HCV infection.17 The clinical presentation of joint involvement varies and includes monoarticular, oligoarticular, or polyarticular involvement.18 It is important to distinguish between HCV-related arthropathy and RA. Most of the drugs given to patients with RA are hepatotoxic. If HCV-related arthropathy and RA are successfully distinguished from each other, liver toxicity caused by the RA drugs may be avoided.19 A prospective study has shown that 20% of patients infected with HCV suffer from arthralgia during a 1-year follow-up period.20
How HCV infection triggers arthritis remains unclear. Three supported mechanisms may exist: direct invasion of the synovial tissue by the virus, autoimmune response to the virus in the synovium, and immune complex or cryoglobulin deposition.21,22 The virus may directly invade the synovium, or the cryoglobulin-induced immune complex in the syno-vial fluid may trigger local inflammation in the synovium.23 Extrahepatic manifestations of HCV infection occur because HCV can replicate efficiently in extrahepatic tissues,24,25 although, in one study, samples from synovial fluid failed to distinguish HCV-related arthritis from RA.26
HCV-related arthritis can present with signs and symptoms as well as joint involvement similar to RA. Thus, clinically, it may be almost impossible to distinguish HCV-related arthritis from RA.27 RF positivity is approximately 70% to 80% in patients with RA, but in HCV-related arthritis, this positivity is between 54% and 82%.28 RF is relatively nonspecific and may be present in several diseases.29,30 On the other hand, CCP antibodies are more specific for RA (96%-98%) and present in approximately 75% to 80% of patients with RA.31,32 However, recent studies have shown that anti-CCP antibodies are present in 4.5% to 7% of patients in whom HCV-related arthritis is diagnosed.28,33,34
Many studies show that anti-CCP antibodies are a better diagnostic laboratory marker than RF for the diagnosis of RA in patients with HCV.35 Anti-CCP antibodies are very specific for RA (96%-98%), and they are found in 60% to 75% of patients with RA.36,37 In addition, anti-CCP antibodies are more predictive of more aggressive and erosive RA.38,39 However, despite the high specificity of anti-CCP—positive antibodies for RA, few doctors argue for the use of these antibodies to differentiate HCV-related arthritis from RA.40 In one study, anti-CCP antibody was positive in 83% of patients with established RA and in 4.5% with HCV-related arthropathy.41
HCV-related arthritis can present with symmetric polyarthritis involving small joints similar to RA. However, it is less likely to lead to bone erosion or subcutaneous nodules.42 The assessment of synovial fluid or a synovial biopsy may not be useful for differentiation of the diseases.43 History of blood transfusion, intravenous drug abuse, or hepatitis should lead to investigation of HCV infection in any patient presenting with polyarthritis, as it may be almost impossible to clinically distinguish HCV infection from RA.27,42
The treatment of HCV-related arthritis is challenging. Interferon (IFN)-α treatment in patients with HCV-related arthritis may aggravate existing pain.44-46 General principles of management include treating the underlying HCV infection as well as using low-dose corticosteroids, nonsteroidal anti-inflammatory drugs, and hydroxychloroquine. Novel non-IFN—based antiviral therapies may eventually play a role in the future.
Hepatitis C Virus and Systemic Lupus Erythematosus
SLE is a common connective tissue disease, and its prevalence is estimated to be 15 to 200 per 100,000.47,48 Articular, mucocutaneous, renal, hematologic, central nervous system, liver, and lung involvement are well documented in this disease. The pathophysiology of SLE is multifactorial and includes environmental triggers, such as viral infec-tions,49 with HCV considered to be among the suspected viruses.50 HCV infection and SLE may share common clinical and serologic features. The extrahepatic manifestations of HCV may mimic SLE, with associated symptoms such as arthralgia, myalgia, sicca syndrome, and antinuclear antibody (ANA) positivity.51,52 One study has shown that the prevalence of HCV infection in patients with SLE was greater than that of the general population.53 In another study, the prevalence of HCV among patients evaluated for SLE was found to be 10%.54 In a study from Egypt, the frequency of HCV infection among patients in a rheuma-tologic clinic was found to be 18.5%. Only 7% had clinical symptoms of HCV infection.55
Known serologic abnormalities may occur in HCV infection. ANA positivity has been reported to be between 10% and 30%,56,57 and HCV infection is associated with cryoglobulinemia.58 All except one study have shown that HCV antibody positivity is observed more frequently in patients with SLE than in patients with HCV infec-tion.59,60 Hence, low-titer ANA, double-stranded DNA (dsDNA) positivity, fewer cutaneous features, liver damage, and cryoglobulinemia should alert physicians to carry out HCV screening in patients with SLE. It also has been emphasized that HCV screening should be conducted before confirming the diagnosis of SLE.61-63
There is evidence that IFN use in the treatment ofHCV infection can trigger autoimmune disorders, including SLE.64 The frequency of autoimmune diseases in patients receiving IFN is between 4.3% and 18.5%.64 Twenty-six IFN-induced SLE cases were reported between 1990 and 2010.65,66 The period between the beginning of IFN treatment and the occurrence of SLE symptoms varied from 2 months to 7 years.65,66 The symptoms in IFN-induced SLE regressed approximately 1 week after the discontinuation of IFN treatment.67 Hence, patients receiving IFN treatment should be monitored for the development of autoimmune diseases, including SLE.68
In summary, extrahepatic manifestations of HCV infection may mimic features that resemble SLE. Further testing of anti-Smith antibody, anti-dsDNA, and anti-nucleosome antibodies may help clinicians establish the diagnosis of SLE. Although the association between HCV and SLE is still uncertain, it has been suggested that HCV may play a role in triggering SLE.
Hepatitis C Virus and Mixed Cryoglobulinemia
Mixed cryoglobulinemic vasculitis (MCV) is known to be the most frequently encountered extrahepatic disease that HCV infection can trigger.69,70 MCV is immune complex—mediated vasculitis that affects small vessels due to the presence of cryoglobulins.71,72 Cryoglobulins are immunoglobulins (Igs) that are insoluble below 37°C and soluble after warming.73 Cryoprecipitation was first described among patients with multiple myeloma in 1933 by 2 hematologists, Wintrobe and Buell from Johns Hopkins University. The term “cryoglobulin” was first used by Lerner and Watson in 1947.74 The clinical triad of MCV, including purpura, arthralgia, and weakness, was initially described by Meltzer and colleagues in 1966.75
According to the Brouet classification, cryoglobulins may be grouped into 3 types. Type 1 cryoglobulinemia includes isolated monoclonal Ig (IgM) and may account for 10% to 15% of cryoglobulinemia. It is usually associated with lymphoproliferative disorders. The IgG and IgA subtypes exist but are rare.76 Type 2 cryoglobulinemia presents with IgM and polyclonal IgG and is mostly encountered in viral infections and inflammatory disor-ders.77,78 HCV can potentially induce type 2 cryoglobuli-nemia in 50% to 60% of cases. Type 3 cryoglobulinemia may present without monoclonal proliferation. Immune complexes are typically formed by polyclonal IgM. Some doctors believe that type 3 cryoglobulinemia may be a transition form between type 1 and type 2.79
The underlying mechanism of HCV-induced MCV may be related to B-cell proliferation, which in turn stimulates CD 5+ cells that are responsible for producing IgM RF. Studies have also shown that HCV may exert an inhibitory response to B-cell apoptosis via activity of B-lymphocyte activating factor.69,70
In some studies, it was observed that anti-HCV and HCV RNA tests were positive in 40% to 90% of patients with mixed cryoglobulinemia (MC).58,80,81 However, studies also showed that the frequency of MC in patients with chronic HCV infection was 10% to 15%.78 MCV clinically presents as cutaneous purpura, arthralgia, and weakness. Involvement of many other organ systems is also reported.82 Palpable purpura, supramalleolar ulcers, or Raynaud phenomenon in the lower limbs of patients with chronic HCV infection should make physicians think about the presence of MC. Besides symmetrical arthralgia in the hands and knees, involvement with the kidneys, liver, and nervous system can also contribute to the diagnosis. Approximately 70% of patients with HCV infection—related MCV have liver involvement and histopathologic finding of active hepatitis.83,84 Complement activation is possibly responsible for endothelial damage in HCV infection—related MCV.85
The main aim of treatment is to eradicate the HCV infection. Serum HCV RNA induces complement activation and, therefore, increases the complement levels. Hence, treatment of HCV infection is important to decrease the circulating complements. The decrease in cryoglobulins and B-cell proliferation in the circulation is also important.
IFN-α and ribavirin remain the cornerstones of therapy for MC type 2.86 Rituximab (Rituxan, Genentech/ Biogen Idec) therapy with or without corticosteroids and plasma exchange may be beneficial therapeutic modalities in the treatment of MC, as it causes B-cell depletion.87 The current standard treatment with triple therapy, including protease inhibitors plus pegylated IFN plus ribavirin, and potential non-IFN—based HCV treatment regimens have yet to be defined.
Hepatitis C Virus and Sjogren Syndrome
Several studies suggest a close correlation between SS and HCV infection. However, the role of HCV infection in the pathogenesis of SS is still unclear.88,89 It is unknown whether HCV infection mimics SS or if HCV has a direct role in the etiopathogenesis of SS. Various outcomes were observed in studies related to the prevalence of HCV infection in patients with SS. These outcomes varied according to study and regional differences. The coprevalence of HCV and SS was reported to be 49% in one study90 and 80% in another.91 In a European study, anti-HCV antibody in patients with primary SS varied between 2% and 26%.92
According to the American and European Consensus Study Group, HCV must be ruled out to diagnose primary SS. It is important to differentiate primary SS from HCV infection—related SS (HCV-SS).93 Male dominance, older age, and anti-Ro/La negativity more commonly suggest HCV-SS.94 The variability of liver function tests and the risk of malignancy development are higher in patients with primary SS than in patients with HCV-SS. Immuno-logically, ANA positivity in patients with HCV-SS is about 70%.95 Anti-Ro/La negativity may support the diagnosis of HCV-SS. However, in one study, some subgroups of patients with HCV-SS and Ro/La positivity were observed.94 Almost half of patients with HCV-SS test positive for cryoglobu-lins. Cryoglobulinemia may predict future extraglandular manifestations. After the diagnosis of cryoglobulinemia, an increase in the risk of development of hypocomplement-emia, liver involvement, and neoplasia is observed.95,96 In addition to cryoglobulinemia, hypocomplementemia and RF are important markers for the diagnosis of HCV-SS.
Hepatitis C Virus and Polyarteritis Nodosa
PAN is a systemic and necrotizing vasculitis of medium and small-sized arteries. This condition, which was previously shown to be associated with hepatitis B virus infection, may also be associated with HCV infection.97,98 The risk of development of HCV-related PAN may be 5% to 12% in chronic HCV infection.99 In a study of 161 patients with chronic HCV infection and HCV-related vasculitis, 31 (19.3%) patients were given a diagnosis of PAN. Compared with HCV-associated MCV, HCV-related PAN was associated with more severe symptoms. However, it was also observed that HCV-related PAN was associated with a higher rate of clinical remission.100
Hypocomplementemia is an important marker for the diagnosis of HCV-related PAN. Moreover, cutaneous manifestations (especially purpura) are observed more frequently, and C-reactive protein and the erythrocyte sedimentation rate are higher in HCV-related PAN.101 The finding of motor mononeuropathy on clinical examination, which is present in almost 90% of patients, may be more useful.102 Symptoms such as cerebral vasculitis, severe hypertension, and ischemic abdominal pain also may be observed in patients with HCV-related PAN.
Antiviral therapies and corticosteroids are the cornerstone treatments for HCV-related PAN. Some specialists also suggest plasma exchange, cyclophosphamide, and rituximab in resistant cases.103
Hepatitis C Virus and Sarcoidosis
Sarcoidosis is a systemic inflammatory disease characterized by the formation of noncaseating epithelioid cell granulomas in the organs. The etiology of the disease is still not well understood.104
The relationship between chronic HCV infection and sarcoidosis was first described in 1993.104 This relationship can be IFN-related or completely unrelated to IFN treatment. IFN-related sarcoidosis is rare but well defined in the literature. Studies have shown that the incidence of sarcoidosis may vary between 0.09% and 0.2% in HCV-infected patients undergoing IFN treatment. The incidence rate seems low, but it is higher than the rate seen in the general population.105,106
Symptoms of sarcoidosis develop in almost two-thirds of patients during the first 6 months of IFN treatment.105 However, data also demonstrate that the disease may occur toward the end of treatment. IFN-related sarcoidosis presents mostly with lung and cutaneous findings. Thus, HCV-infected patients treated with IFN therapy should be carefully evaluated for development of sarcoidosis.106 Although rare, non-IFN—related sarcoidosis has been reported in chronic HCV infection. IFN-related sarcoidosis clinically progresses in a benign fashion. Patients with mild symptoms may continue with IFN treatment. However, IFN treatment should be stopped in patients whose symptoms do not regress. In such cases, corticosteroids and hydroxychloroquine can be considered as possible treatment options.105-107
Conclusion
Extrahepatic manifestations are frequently encountered among patients with chronic HCV infection. Several of these manifestations can mimic autoimmune disorders. Moreover, primary autoimmune disorders can coexist with HCV infection. They cause mortality and morbidity by affecting multiple organ systems. Arthralgia, myalgia, sicca symptoms, and vasculitis are some clinically common syndromes. Serologic abnormalities such as ANA and RF positivity are common in both HCV infection and primary autoimmune disorders. Some treatment modalities for HCV infection, such as IFN, can induce or aggravate the symptoms of rheumatologic diseases. In patients with HCV infection, it is critical to distinguish whether these syndromes occur secondary to chronic HCV infection or a primary rheumatologic disease, as this differentiation is critical in tailoring appropriate therapeutic management.
Footnotes
The authors have no relevant conflicts of interest to disclose.
References
- 1.Choo QL, Kuo G, Weiner AJ, Overby LR, Bradley DW, Houghton M. Isolation of a cDNA clone derived from a blood-borne non-A, non-B viral hepatitis genome. Science. 1989;244(4902):359–362. doi: 10.1126/science.2523562. [DOI] [PubMed] [Google Scholar]
- 2.Ryan KJ, Ray CG, editors. Sherris Medical Microbiology. 4th ed. New York, NY: McGraw-Hill; 2004. pp. 551–552. [Google Scholar]
- 3.Houghton M. The long and winding road leading to the identification of the hepatitis C virus. J Hepatol. 2009;51(5):939–948. doi: 10.1016/j.jhep.2009.08.004. [DOI] [PubMed] [Google Scholar]
- 4. [March 27, 2014]. www.who.int/csr/disease/hepatitis/whocdscsrlyo2003/en/index1.html Global alert and response (GAR). Hepatitis C World Health Organization.
- 5. [March 27, 2014]. www.cdc.gov/hepatitis/HCV/HCVfaq.htm#section1 Hepatitis C FAQs for health professionals. Centers for Disease Control and Prevention.
- 6.Cacoub P, Renou C, Rosenthal E, et al. Extrahepatic manifestations associated with hepatitis C virus infection. A prospective multicenter study of 321 patients. The GERMIVIC Groupe d’Etude et de Recherche en Medecine Interne et Maladies Infectieuses sur le Virus de l’ Hepatite C. Medicine (Baltimore). 2000;79(1):47–56. doi: 10.1097/00005792-200001000-00005. [DOI] [PubMed] [Google Scholar]
- 7.Mohammed RH, ElMakhzangy HI, Gamal A, et al. Prevalence of rheumato-logic manifestations of chronic hepatitis C virus infection among Egyptians. Clin Rheumatol. 2010;29(12):1373–1380. doi: 10.1007/s10067-010-1463-x. [DOI] [PubMed] [Google Scholar]
- 8.Palazzi C, Olivieri I, Cacciatore P, Pennese E, D’Amico E. Difficulties in the differential diagnosis between primitive rheumatic diseases and hepatitis C virus-related disorders. Clin Exp Rheumatol. 2005;23(1):2–6. [PubMed] [Google Scholar]
- 9.Cacoub P, Poynard T, Ghillani P, et al. Extrahepatic manifestations of chronic hepatitis C MULTIVIRC group. Multidepartment virus C. Arthritis Rheum. 1999;42(10):2204–2212. doi: 10.1002/1529-0131(199910)42:10<2204::AID-ANR24>3.0.CO;2-D. [DOI] [PubMed] [Google Scholar]
- 10.Ali A, Zein NN. Hepatitis C infection: a systemic disease with extrahepatic manifestations. Cleve Clin J Med. 2005;72(11):1005–1008. doi: 10.3949/ccjm.72.11.1005. 1010-1014, 1016 passim. [DOI] [PubMed] [Google Scholar]
- 11.Zignego AL, Macchia D, Monti M, et al. Infection of peripheral mononuclear blood cells by hepatitis C virus. J Hepatol. 1992;15(3):382–386. doi: 10.1016/0168-8278(92)90073-x. [DOI] [PubMed] [Google Scholar]
- 12.Conca P, Tarantino G. Hepatitis C virus lymphotropism and peculiar immunological phenotype: effects on natural history and antiviral therapy. World J Gastroenterol. 2009;15(19):2305–2308. doi: 10.3748/wjg.15.2305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Riccio A, Postiglione L, La Dogana P, Spanò A, Marzocchella C, Tarantino G. Anti-cyclic citrullinated peptide antibodies in patients affected by HCV-related arthritis. J Biol Regul Homeost Agents. 2008;22(1):57–61. [PubMed] [Google Scholar]
- 14.Riccio A, Postiglione L, Sabatini P, et al. Similar serum levels of IL-6 and its soluble receptors in patients with HCV-related arthritis and rheumatoid arthritis: a pilot study. Int J Immunopathol Pharmacol. 2012;25(1):281–285. doi: 10.1177/039463201202500132. [DOI] [PubMed] [Google Scholar]
- 15.Fabrizi F, Lunghi G, Messa P, Martin P. Therapy of hepatitis C virus-associated glomerulonephritis: current approaches. J Nephrol. 2008;21(6):813–825. [PubMed] [Google Scholar]
- 16.Ramos-Casals M, Jara LJ, Medina F, et al. HISPAMEC Study Group. Systemic autoimmune diseases co-existing with chronic hepatitis C virus infection (the HIS-PAMEC Registry): patterns of clinical and immunological expression in 180 cases. J Intern Med.. 2005;257(6):549–557. doi: 10.1111/j.1365-2796.2005.01490.x. [DOI] [PubMed] [Google Scholar]
- 17.Rivera J, García-Monforte A, Pineda A, Millán Núñez-Cortés J. Arthritis in patients with chronic hepatitis C virus infection. J Rheumatol. 1999;26(2):420–424. [PubMed] [Google Scholar]
- 18.Buskila D, Shnaider A, Neumann L, et al. Musculoskeletal manifestations and autoantibody profile in 90 hepatitis C virus infected Israeli patients. Semin Arthritis Rheum. 1998;28(2):107–113. doi: 10.1016/s0049-0172(98)80043-7. [DOI] [PubMed] [Google Scholar]
- 19.Giannitti C, Bellisai F, Ferri C, Galeazzi M. Treatment strategies for a patient with rheumatoid arthritis and hepatitis C. Expert Opin Pharmacother. 2009;10(4):579–587. doi: 10.1517/14656560902731951. [DOI] [PubMed] [Google Scholar]
- 20.Poantă L, Albu A. Chronic hepatitis C with extrahepatic manifestations. Rom J Intern Med.. 2007;45(1):85–88. [PubMed] [Google Scholar]
- 21.Zuckerman E, Keren D, Rozenbaum M, et al. Hepatitis C virus-related arthritis: characteristics and response to therapy with interferon alpha. Clin Exp Rheumatol. 2000;18(5):579–584. [PubMed] [Google Scholar]
- 22.Olivieri I, Palazzi C, Padula A. Hepatitis C virus and arthritis. Rheum Dis Clin North Am. 2003;29(1):111–122. doi: 10.1016/s0889-857x(02)00097-2. [DOI] [PubMed] [Google Scholar]
- 23.Buskila D. Hepatitis C-associated rheumatic disorders. Rheum Dis Clin North Am. 2009;35(1):111–123. doi: 10.1016/j.rdc.2009.03.005. [DOI] [PubMed] [Google Scholar]
- 24.Ezzat WM, Raslan HM, Aly AA, Emara NA, El Menyawi MM, Edrees A. Anti-cyclic citrullinated peptide antibodies as a discriminating marker between rheumatoid arthritis and chronic hepatitis C-related polyarthropathy. Rheumatol Int. 2011;31(1):65–69. doi: 10.1007/s00296-009-1225-8. [DOI] [PubMed] [Google Scholar]
- 25.Clifford BD, Donahue D, Smith L, et al. High prevalence of serological markers of autoimmunity in patients with chronic hepatitis C. Hepatology. 1995;21(3):613–619. [PubMed] [Google Scholar]
- 26.Ogdie A, Schumacher HR, Jr, Dai L, Chen LX, Einhorn E, Pessler F. Synovial biopsy findings in arthritis associated with hepatitis C virus infection. J Rheumatol. 2010;37(6):1361–1363. doi: 10.3899/jrheum.091309. [DOI] [PubMed] [Google Scholar]
- 27.Rosner I, Rozenbaum M, Toubi E, Kessel A, Naschitz JE, Zuckerman E. The case for hepatitis C arthritis. Semin Arthritis Rheum. 2004;33(6):375–387. doi: 10.1016/j.semarthrit.2003.12.006. [DOI] [PubMed] [Google Scholar]
- 28.Sène D, Ghillani-Dalbin P, Limal N, et al. Anti-cyclic citrullinated peptide antibodies in hepatitis C virus associated rheumatological manifestations and Sjo-gren’s syndrome. Ann Rheum Dis. 2006;65(3):394–397. doi: 10.1136/ard.2005.038042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Amri M, Sfar I, Ounallah HS, et al. Anti-CCP antibodies, rheumatoid factors and anti-keratin antibodies: clinical value in established rheumatoid arthritis. Tunis Med.. 2011;89(3):231–235. [PubMed] [Google Scholar]
- 30.Harris ED. Clinical features of rheumatoid arthritis. In: Harris ED, Budd RC, Firestein GS, et al., editors. Kelly’s Textbook of Rheumatology. 7th ed. vol II. Philadelphia, PA: Elsevier Saunders; 2005. pp. 1043–1100. [Google Scholar]
- 31.Pinheiro GC, Scheinberg MA, Aparecida da Silva M, Maciel S. Anti-cyclic citrullinated peptide antibodies in advanced rheumatoid arthritis. Ann Intern Med. 2003;139(3):234–235. doi: 10.7326/0003-4819-139-3-200308050-00021. [DOI] [PubMed] [Google Scholar]
- 32.van Venrooij WJ, Hazes JM, Visser H. Anticitrullinated protein/peptide antibody and its role in the diagnosis and prognosis of early rheumatoid arthritis. Neth J Med. 2002;60(10):383–388. [PubMed] [Google Scholar]
- 33.Palazzi C, Buskila D, D’Angelo S, D’Amico E, Olivieri I. Autoantibodies in patients with chronic hepatitis C virus infection: pitfalls for the diagnosis of rheumatic diseases. Autoimmun Rev. 2012;11(9):659–663. doi: 10.1016/j.autrev.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 34.Wener MH, Hutchinson K, Morishima C, Gretch DR. Absence of antibodies to cyclic citrullinated peptide in sera of patients with hepatitis C virus infection and cryoglobulinemia. Arthritis Rheum. 2004;50(7):2305–2308. doi: 10.1002/art.20355. [DOI] [PubMed] [Google Scholar]
- 35.Nishimura K, Sugiyama D, Kogata Y, et al. Meta-analysis: diagnostic accuracy of anti-cyclic citrullinated peptide antibody and rheumatoid factor for rheumatoid arthritis. Ann Intern Med. 2007;146(11):797–808. doi: 10.7326/0003-4819-146-11-200706050-00008. [DOI] [PubMed] [Google Scholar]
- 36.Schellekens GA, de Jong BAW, van den Hoogen FHJ, van de Putte LBA, van Venrooij WJ. Citrulline is an essential constituent of antigenic determinants recognized by rheumatoid arthritis-specific autoantibodies. J Clin Invest. 1998;101(1):273–281. doi: 10.1172/JCI1316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schellekens GA, Visser H, de Jong BA, et al. The diagnostic properties of rheumatoid arthritis antibodies recognizing a cyclic citrullinated peptide. Arthritis Rheum. 2000;43(1):155–163. doi: 10.1002/1529-0131(200001)43:1<155::AID-ANR20>3.0.CO;2-3. [DOI] [PubMed] [Google Scholar]
- 38.Kroot EJ, de Jong BA, van Leeuwen MA, et al. The prognostic value of anti-cyclic citrullinated peptide antibody in patients with recent-onset rheumatoid arthritis. Arthritis Rheum. 2000;43(8):1831–1835. doi: 10.1002/1529-0131(200008)43:8<1831::AID-ANR19>3.0.CO;2-6. [DOI] [PubMed] [Google Scholar]
- 39.Visser H, le Cessie S, Vos K, Breedveld FC, Hazes JM. How to diagnose rheumatoid arthritis early: a prediction model for persistent (erosive) arthritis. Arthritis Rheum. 2002;46(2):357–365. doi: 10.1002/art.10117. [DOI] [PubMed] [Google Scholar]
- 40.Ferri C, Zignego AL. Relation between infection and autoimmunity in mixed cryoglobulinemia. Curr Opin Rheumatol. 2000;12(1):53–60. doi: 10.1097/00002281-200001000-00009. [DOI] [PubMed] [Google Scholar]
- 41.Antonelli A, Ferri C, Galeazzi M, et al. HCV infection: pathogenesis, clinical manifestations and therapy. Clin Exp Rheumatol. 2008;26(1 suppl 48):S39–S47. [PubMed] [Google Scholar]
- 42.Kemmer NM, Sherman KE. Hepatitis C-related arthropathy: diagnostic and treatment considerations. J Musculoskelet Med. 2010;27(9):351–354. [PMC free article] [PubMed] [Google Scholar]
- 43.Iagnocco A, Coari G, Mammarella A, et al. Joint sonography in asymptomatic patients with HCV correlated hepatitis. Clin Exp Rheumatol. 2004;22(1):43–48. [PubMed] [Google Scholar]
- 44.Yurci A, Guven K, Torun E, et al. Pyoderma gangrenosum and exacerbation of psoriasis resulting from pegylated interferon alpha and ribavirin treatment of chronic hepatitis C. Eur J Gastroenterol Hepatol. 2007;19(9):811–815. doi: 10.1097/MEG.0b013e32816e070b. [DOI] [PubMed] [Google Scholar]
- 45.Ketikoglou I, Karatapanis S, Elefsiniotis I, Kafiri G, Moulakakis A. Extensive psoriasis induced by pegylated interferon alpha-2b treatment for chronic hepatitis B. Eur J Dermatol. 2005;15(2):107–109. [PubMed] [Google Scholar]
- 46.Kartal ED, Colak H, Ozgunes I, Usluer G. Exacerbation of psoriasis due to peginterferon alpha-2b plus ribavirin treatment of chronic active hepatitis C. Chemotherapy. 2005;51(2-3):167–169. doi: 10.1159/000085626. [DOI] [PubMed] [Google Scholar]
- 47.Johnson AE, Gordon C, Hobbs FD, Bacon PA. Undiagnosed systemic lupus erythematosus in the community. Lancet. 1996;347(8998):367–369. doi: 10.1016/s0140-6736(96)90539-5. [DOI] [PubMed] [Google Scholar]
- 48.Gourley IS, Patterson CC, Bell AL. The prevalence of systemic lupus erythematosus in Northern Ireland. Lupus. 1997;6(4):399–403. doi: 10.1177/096120339700600410. [DOI] [PubMed] [Google Scholar]
- 49.Ramos-Casals M, Font J, Garcla-Carrasco M, et al. Hepatitis C virus infection mimicking systemic lupus erythematosus: study of hepatitis C virus infection in a series of 134 Spanish patients with systemic lupus erythematosus. Arthritis Rheum. 2000;43(12):2801–2806. doi: 10.1002/1529-0131(200012)43:12<2801::AID-ANR21>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 50.Marchesoni A, Battafarano N, Podico M, Tosi S. Hepatitis C virus antibodies and systemic lupus erythematosus [letter] Clin Exp Rheumatol. 1995;13(2):267. [PubMed] [Google Scholar]
- 51.Fessler BJ, Boumpas DT. Severe major organ involvement in systemic lupus erythematosus. Diagnosis and management. Rheum Dis Clin North Am. 1995;21(1):81–98. [PubMed] [Google Scholar]
- 52.Mohan P, Rajasekaran M, Ramanathan P, Venkataraman J. Prevalence of hepatitis C virus antibodies in systemic lupus erythematosus. Eur J Gastroenterol Hepatol. 2009;21(12):1437–1438. doi: 10.1097/MEG.0b013e328324ed47. [DOI] [PubMed] [Google Scholar]
- 53.Ahmed MM, Berney SM, Wolf RE, et al. Prevalence of active hepatitis C virus infection in patients with systemic lupus erythematosus. Am J Med Sci. 2006;331(5):252–256. doi: 10.1097/00000441-200605000-00003. [DOI] [PubMed] [Google Scholar]
- 54.Mercado U, Avendaño-Reyes M, Araiza-Casillas R, Díaz-Molina R. Prevalance of antibodies against hepatitis C and B viruses in patients with systemic lupus erythematosus [in Spanish] Rev Gastroenterol Mex. 2005;70(4):399–401. [PubMed] [Google Scholar]
- 55.El Garf A, El Zorkany B, Gheith R, Sheba H, Abdel Moneim G, El Garf K. Prevalence and clinical presentations of hepatitis C virus among patients admitted to the rheumatology ward. Rheumatol Int. 2012;32(9):2691–2695. doi: 10.1007/s00296-011-2014-8. [DOI] [PubMed] [Google Scholar]
- 56.McMurray RW, Elbourne K. Hepatitis C virus infection and autoimmunity. Semin Arthritis Rheum. 1997;26(4):689–701. doi: 10.1016/s0049-0172(97)80005-4. [DOI] [PubMed] [Google Scholar]
- 57.Pawlotsky JM, Roudot-Thoraval F, Simmonds P, et al. Extrahepatic immunologic manifestations in chronic hepatitis C and hepatitis C virus serotypes. Ann Intern Med. 1995;122(3):169–173. doi: 10.7326/0003-4819-122-3-199502010-00002. [DOI] [PubMed] [Google Scholar]
- 58.Sansonno D, Carbone A, De Re V, Dammacco F. Hepatitis C virus infection, cryoglobulinaemia, and beyond. Rheumatology (Oxford). 2007;46(4):572–578. doi: 10.1093/rheumatology/kel425. [DOI] [PubMed] [Google Scholar]
- 59.Dammacco F, Sansonno D. Therapy for hepatitis C virus-related cryoglobulinemia vasculitis. N Engl J Med. 2013;369(11):1035–1045. doi: 10.1056/NEJMra1208642. [DOI] [PubMed] [Google Scholar]
- 60.Karakoç Y, Dilek K, Gullulu M, et al. Prevalence of hepatitis C virus antibody in patients with systemic lupus erythematosus. Ann Rheum Dis. 1997;56(9):570–571. doi: 10.1136/ard.56.9.570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Lormeau C, Falgarone G, Roulot D, Boissier MC. Rheumatologic manifestations of chronic hepatitis C infection. Joint Bone Spine. 2006;73(6):633–638. doi: 10.1016/j.jbspin.2006.05.005. [DOI] [PubMed] [Google Scholar]
- 62.Manns MP, Rambusch EG. Autoimmunity and extrahepatic manifestations in hepatitis C virus infection. J Hepatol. 1999;31(suppl 1):39–42. doi: 10.1016/s0168-8278(99)80372-9. [DOI] [PubMed] [Google Scholar]
- 63.Willson RA. Extrahepatic manifestations of chronic viral hepatitis. Am J Gastroenterol. 1997;92(1):3–17. [PubMed] [Google Scholar]
- 64.Andrade LJ, D’Oliveira A, Jr, Silva CA, et al. A meta-analysis of patients with chronic hepatitis C treated with interferon-alpha to determine the risk of autoimmune thyroiditis. Acta Gastroenterol Latinoam. 2011;41(2):104–110. [PubMed] [Google Scholar]
- 65.Wilson LE, Widman D, Dikman SH, Gorevic PD. Autoimmune disease complicating antiviral therapy for hepatitis C virus infection. Semin Arthritis Rheum. 2002;32(3):163–173. doi: 10.1053/sarh.2002.37277. [DOI] [PubMed] [Google Scholar]
- 66.Wandl UB, Nagel-Hiemke M, May D, et al. Lupus-like autoimmune disease induced by interferon therapy for myeloproliferative disorders. Clin Immunol Immunopathol. 1992;65(1):70–74. doi: 10.1016/0090-1229(92)90250-r. [DOI] [PubMed] [Google Scholar]
- 67.Niewold TB, Swedler WI. Systemic lupus erythematosus arising during interferon-alpha therapy for cryoglobulinemic vasculitis associated with hepatitis C. Clin Rheumatol. 2005;24(2):178–181. doi: 10.1007/s10067-004-1024-2. [DOI] [PubMed] [Google Scholar]
- 68.Rizvi R, Hojjati M. Interferonα induced lupus in a patient with chronic hepatitis C virus. J Clin Rheumatol. 2011;17(3):152–153. doi: 10.1097/RHU.0b013e31821557e7. [DOI] [PubMed] [Google Scholar]
- 69.Lauletta G, Russi S, Conteduca V, Sansonno L. Hepatitis C virus infection and mixed cryoglobulinemia. Clin Dev Immunol. 2012;2012:502156. doi: 10.1155/2012/502156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Agnello V, Chung RT, Kaplan LM. A role for hepatitis C virus infection in type II cryoglobulinemia. N Engl J Med. 1992;327(21):1490–1495. doi: 10.1056/NEJM199211193272104. [DOI] [PubMed] [Google Scholar]
- 71.Pozzato G, Mazzaro C, Crovatto M, et al. Low-grade malignant lymphoma, hepatitis C virus infection, and mixed cryoglobulinemia. Blood. 1994;84(9):3047–3053. [PubMed] [Google Scholar]
- 72.Misiani R, Bellavita P, Fenili D, et al. Hepatitis C virus infection in patients with essential mixed cryoglobulinemia. Ann Intern Med. 1992;117(7):573–577. doi: 10.7326/0003-4819-117-7-573. [DOI] [PubMed] [Google Scholar]
- 73.Vermeersch P, Gijbels K, Mariën G, et al. A critical appraisal of current practice in the detection, analysis, and reporting of cryoglobulins. Clin Chem. 2008;54(1):39–43. doi: 10.1373/clinchem.2007.090134. [DOI] [PubMed] [Google Scholar]
- 74.Wintrobe M, Buell M. Hyperproteinemia associated with multiple myeloma. With report of a case in which an extraordinary hyperproteinemia was associated with thrombosis of the retinal veins and symptoms suggesting Raynaud’s disease. Bull Johns Hopkins Hosp. 1933;52:156–165. [Google Scholar]
- 75.Meltzer M, Franklin EC, Elias K, McCluskey RT, Cooper N. Cryoglobuline-mia—a clinical and laboratory study. II. Cryoglobulins with rheumatoid factor activity. Am J Med. 1966;40(6):837–856. doi: 10.1016/0002-9343(66)90200-2. [DOI] [PubMed] [Google Scholar]
- 76.Brouet JC, Clauvel JP, Danon F, Klein M, Seligmann M. Biologic and clinical significance of cryoglobulins. A report of 86 cases. Am J Med. 1974;57(5):775–788. doi: 10.1016/0002-9343(74)90852-3. [DOI] [PubMed] [Google Scholar]
- 77.Levo Y, Gorevic PD, Kassab HJ, Zucker-Franklin D, Franklin EC. Association between hepatitis B virus and essential mixed cryoglobulinemia. N Engl J Med. 1977;296(26):1501–1504. doi: 10.1056/NEJM197706302962605. [DOI] [PubMed] [Google Scholar]
- 78.Ferri C, Greco F, Longombardo G, et al. Association between hepatitis C virus and mixed cryoglobulinemia [see comment] Clin Exp Rheumatol. 1991;9(6):621–624. [PubMed] [Google Scholar]
- 79.Tissot JD, Schifferli JA, Hochstrasser DF, et al. Two-dimensional polyacryl-amide gel electrophoresis analysis of cryoglobulins and identification of an IgM-associated peptide. J Immunol Methods. 1994;173(1):63–75. doi: 10.1016/0022-1759(94)90284-4. [DOI] [PubMed] [Google Scholar]
- 80.Dammacco F, Sansonno D, Piccoli C, Tucci FA, Racanelli V. The cryoglobu-lins: an overview. Eur J Clin Invest. 2001;31(7):628–638. doi: 10.1046/j.1365-2362.2001.00824.x. [DOI] [PubMed] [Google Scholar]
- 81.Sansonno D, Dammacco F. Hepatitis C virus, cryoglobulinaemia, and vasculi-tis: immune complex relations. Lancet Infect Dis. 2005;5(4):227–236. doi: 10.1016/S1473-3099(05)70053-0. [DOI] [PubMed] [Google Scholar]
- 82.De Vita S. Treatment of mixed cryoglobulinemia: a rheumatology perspective. Clin Exp Rheumatol. 2011;29(1 suppl 64):S99–S103. [PubMed] [Google Scholar]
- 83.Dammacco F, Sansonno D. Antibodies to hepatitis C virus in essential mixed cryoglobulinaemia. Clin Exp Immunol. 1992;87(3):352–356. doi: 10.1111/j.1365-2249.1992.tb03001.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Saadoun D, Asselah T, Resche-Rigon M, et al. Cryoglobulinemia is associated with steatosis and fibrosis in chronic hepatitis C. Hepatology. 2006;43(6):1337–1345. doi: 10.1002/hep.21190. [DOI] [PubMed] [Google Scholar]
- 85.Sansonno D, Tucci FA, Ghebrehiwet B, et al. Role of the receptor for the globular domain of C1q protein in the pathogenesis of hepatitis C virus-related cryoglobulin vascular damage. J Immunol. 2009;183(9):6013–6020. doi: 10.4049/jimmunol.0902038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Ferri C, Sebastiani M, Antonelli A, Colaci M, Manfredi A, Giuggioli D. Current treatment of hepatitis C-associated rheumatic diseases. Arthritis Res Ther. 2012;14(3):215. doi: 10.1186/ar3865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zaja F, De Vita S, Mazzaro C, et al. Efficacy and safety of rituximab in type II mixed cryoglobulinemia. Blood. 2003;101(10):3827–3834. doi: 10.1182/blood-2002-09-2856. [DOI] [PubMed] [Google Scholar]
- 88.Ramos-Casals M, Brito-Zerón P, Font J. Lessons from diseases mimicking Sjögren’s syndrome. Clin Rev Allergy Immunol. 2007;32(3):275–283. doi: 10.1007/s12016-007-8006-5. [DOI] [PubMed] [Google Scholar]
- 89.Ramos-Casals M, Munoz S, Zeron PB. Hepatitis C virus and Sjögren’s syndrome: trigger or mimic? Rheum Dis Clin North Am. 2008;34(4):869–884, vii. doi: 10.1016/j.rdc.2008.08.007. [DOI] [PubMed] [Google Scholar]
- 90.Pawlotsky JM, Ben Yahia M, Andre C, et al. Immunological disorders in C virus chronic active hepatitis: a prospective case-control study. Hepatology. 1994;19(4):841–848. [PubMed] [Google Scholar]
- 91.Loustaud-Ratti V, Riche A, Liozon E, et al. Prevalence and characteristics of Sjögren’s syndrome or Sicca syndrome in chronic hepatitis C virus infection: a prospective study. J Rheumatol. 2001;28(10):2245–2251. [PubMed] [Google Scholar]
- 92.Madaliński K, Godzik P, Zimmermann-Górska I, et al. Anti-HCV and HCV RNA in patients with the primary Sjogren syndrome [in Polish] Przegl Epidemiol. 2009;63(2):299–304. [PubMed] [Google Scholar]
- 93.Baldini C, Talarico R, Tzioufas AG, Bombardieri S. Classification criteria for Sjogren’s syndrome: a critical review. J Autoimmun. 2012;39(1-2):9–14. doi: 10.1016/j.jaut.2011.12.006. [DOI] [PubMed] [Google Scholar]
- 94.Ramos-Casals M, Font J. Extrahepatic manifestations in patients with chronic hepatitis C virus infection. Curr Opin Rheumatol. 2005;17(4):447–455. doi: 10.1097/01.bor.0000166386.62851.49. [DOI] [PubMed] [Google Scholar]
- 95.Ramos-Casals M, Loustaud-Ratti V, De Vita S, et al. Sjogren syndrome associated with hepatitis C virus: a multicenter analysis of 137 cases. Medicine (Baltimore). 2005;84(2):81–89. doi: 10.1097/01.md.0000157397.30055.c9. [DOI] [PubMed] [Google Scholar]
- 96.Ramos-Casals M, Theander E, Tzioufas AG, et al. Digestive involvement in primary Sjogren syndrome. In: Font J, Ramos-Casals M, Rodes J, et al., editors. Digestive Involvement of Autoimmune Diseases. Amsterdam, The Netherlands: Elsevier; 2008. pp. 71–81. [Google Scholar]
- 97.Valente RM, Conn DL. Current therapies for systemic vasculitis. Semin Neurol. 1994;14(4):380–386. doi: 10.1055/s-2008-1041098. [DOI] [PubMed] [Google Scholar]
- 98.Talarico R, Baldini C, Della Rossa A, et al. Large- and small-vessel vasculitis: a critical digest of the 2010-2011 literature. Clin Exp Rheumatol. 2012;30(1 suppl 70):S130–S138. [PubMed] [Google Scholar]
- 99.Pagnoux C, Seror R, Henegar C, et al. French Vasculitis Study Group. Clinical features and outcomes in 348 patients with polyarteritis nodosa: a systematic retrospective study of patients diagnosed between 1963 and 2005 and entered into the French Vasculitis Study Group Database. Arthritis Rheum. 2010;62(2):616–626. doi: 10.1002/art.27240. [DOI] [PubMed] [Google Scholar]
- 100.Saadoun D, Terrier B, Semoun O, et al. Hepatitis C virus-associated polyar-teritis nodosa. Arthritis Care Res (Hoboken). 2011;63(3):427–435. doi: 10.1002/acr.20381. [DOI] [PubMed] [Google Scholar]
- 101.Soufir N, Descamps V, Crickx B, et al. Hepatitis C virus infection in cutaneous polyarteritis nodosa: a retrospective study of 16 cases. Arch Dermatol. 1999;135(8):1001–1002. doi: 10.1001/archderm.135.8.1001. [DOI] [PubMed] [Google Scholar]
- 102.Cacoub P, Maisonobe T, Thibault V, et al. Systemic vasculitis in patients with hepatitis C. J Rheumatol. 2001;28(1):109–118. [PubMed] [Google Scholar]
- 103.de Menthon M, Mahr A. Treating polyarteritis nodosa: current state of the art. Clin Exp Rheumatol. 2011;29(1 suppl 64):S110–S116. [PubMed] [Google Scholar]
- 104.Culver DA. Sarcoidosis. Immunol Allergy Clin North Am. 2012;32(4):487–511. doi: 10.1016/j.iac.2012.08.005. [DOI] [PubMed] [Google Scholar]
- 105.Ramos-Casals M, Mañá J, Nardi N, et al. HISPAMEC Study Group. Sar-coidosis in patients with chronic hepatitis C virus infection: analysis of 68 cases. Medicine (Baltimore). 2005;84(2):69–80. doi: 10.1097/01.md.0000157577.69729.e6. [DOI] [PubMed] [Google Scholar]
- 106.Jadali Z. Dermatologic manifestations of hepatitis C infection and the effect of interferon therapy: a literature review. Arch Iran Med. 2012;15(1):43–48. [PubMed] [Google Scholar]
- 107.Leclerc S, Myers RP, Moussalli J, Herson S, Poynard T, Benveniste O. Sar-coidosis and interferon therapy: report of five cases and review of the literature. Eur J Intern Med. 2003;14(4):237–243. doi: 10.1016/s0953-6205(03)00078-5. [DOI] [PubMed] [Google Scholar]