Abstract
Objective:
The primary objective of this study is to examine the medication adherence levels (as a function of pharmaceutical care) and its contributing factors in schizophrenic patients receiving antipsychotic drugs.
Methods:
This was a cross-sectional study administering a structured questionnaire to 231 patients. Adherence was measured through patient self-reporting. Association between independent variables and adherence to antipsychotics were measured through odds ratios (OR) in the univariate analysis while the best predictors of adherence were determined through the multiple logistic regressions.
Findings:
Adherence level was found to be 65.8% (95% confidence interval [CI]: 59.3-71.9%). The following factors were identified to be associated with adherence in the univariate analysis: age (OR 1.088), sex (OR 1.231), employment (OR 0.366), marital status (singles, OR 0.022), drug adherence counseling (OR 11.641), twice a day frequency (OR 8.434), alcohol non-intake (OR 1.469), educational level (primary OR 1.9312, secondary OR 11.022, tertiary OR 4.771), occupation (public servant 6.273). In the multivariate analysis, age, three times a day frequency of drug intake, singles and educational levels such as primary, secondary or tertiary school, strongly affected adherence (P < 0.05).
Conclusion:
Although patients adherence level was high (65.8%), there is a need to emphasize that pharmacists spend more time in counseling and educating patients, especially younger ones on drug adherence before any antipsychotic medications are dispensed. Furthermore, patients should be taught the use of adherence devices such as reminders so that adherence to antipsychotic medications can be optimized.
Keywords: Antipsychotic drugs, drug adherence, pharmaceutical care, schizophrenia
INTRODUCTION
The World Health Organization reports that approximately 450 million persons world-wide suffer from mental, neurological disorders or from psychological problems.[1] In Africa, neuropsychiatric disorders result in about 17.6% of all years of life lived with disability. An estimated 26.2% of Americans aged 18 years and older representing almost 25% of all adults suffer from a diagnosable mental disorder in a given year.[2] Reports from South Western Nigeria showed that 12.1% of those sampled had at least one lifetime mental disorder and that 5.6% had experienced at least one mental disorder in the previous 12 months.[3] As a result of this burden of mental illness, health professionals, including pharmacists should be involved in their management. The need for pharmaceutical care in mental disease being more relevant now than previously realized or even acknowledged. Reasons for this include the increasing number of available antipsychotic medications with various mechanisms of action, potentials for drug-drug and drug-food interactions; and increasing incidences of drug usage in the society tending towards community rather than institutional patient management.
Pharmaceutical care is provision of drug therapy in a responsible way with the aim of achieving definite outcomes geared towards improving a patient's quality-of-life.[4] Pharmaceutical care activities ensure that patients use drugs in a safe and rational way.[5,6] This includes Pharmaceutical care activities such as determination of drug needs for a given patient and the provision, not only of the drug needs but also of the services necessary (before, during and after treatment) to ensure safe and effective therapy.[7]
Medication adherence is a very important factor in drug use by schizophrenic patients. Many factors can affect drug adherence in these patients. The factors may include disease related factors, treatment related factors (such as actual or perceived unpleasant side-effects, regimen complexity and treatment duration) and patient related factors (sensory or cognitive impairment, economic problems and educational deficiencies). Pharmacists have roles in resolving these adherence related problems. In particular, pharmacists can be involved in educational activities such as provision of drug adherence counseling and also providing safe effective and affordable drugs.
The institutionalization of pharmaceutical care will ensure that patients adhere to their antipsychotic medication regimens. This is very important in the management of psychiatric patients and psychiatric drug used in general given the associated problems earlier mentioned. This study examines medication adherence (as a sub function of pharmaceutical care) and explores factors associated with it in schizophrenic patients receiving antipsychotic drugs.
METHODS
This was a cross-sectional study carried out at the pharmacy unit of the Psychiatric Department, Jos University Teaching Hospital, North Central region of Nigeria. Patients were schizophrenic patients, who have been on antipsychotic drugs on an out-patient basis for at least 1 year.
All out-patients that fulfilled the inclusion criteria (231) were recruited.
Written informed consents were obtained from stable patients or their representatives/relations that are bringing them to the hospital. The ethics committee of the Jos University Teaching Hospital reviewed and approved the study protocol through letter number JUTH/DCS/ADM/127/4841.
Data was collected with the aid of a structured, pretested, interviewer-administered questionnaire consisting of 27 questions. Nine questions were on socio-demographic data, four were on patients’ knowledge of schizophrenia, three on patients’ knowledge of antipsychotics, nine on medication adherence and two on drug side-effects. The records of prescriptions in the patient folders were used to obtain information on drug regimen when the patient could not provide such information.
The following are the criteria for inclusion of patients in the study:
All schizophrenic out-patients attending the psychiatric clinic who have been on antipsychotic medications for at least 1 year.
Patients who were 16 years of age or older.
All patients having a Diagnostic and Statistical Manual for Mental disorders, 4th Edition (DSM IV) psychiatric diagnosis made by a consultant psychiatrist at the Jos University Teaching Hospital.
Patients that consented to participate in the study.
The following categories of patients were excluded from the study:
All schizophrenic out-patients who were attending the clinic, but had not started antipsychotics.
Patients not stable enough to complete the questionnaire or interview.
All patients who neither consented nor received drug adherence counseling by the pharmacist.
Data were analyzed using EPI-Info version 3.4.3, a public domain statistical software for epidemiology developed by Centers for Disease Control and Prevention, CDC, Atlanta, Georgia, USA. The magnitude of the association among the different variables in relation to medication adherence was measured through odds ratios and their 95% confidence intervals (CI). Determinants of good adherence were identified via a stepwise multivariable logistic regression. P < 0.05 was considered to be significant in all analysis.
RESULTS
A total of 231 respondents aged 16-80 years participated in the study. About 213 (92.2%) patients confirmed to having received drug adherence counseling from the pharmacist during the pick-up of their medications while 18 (7.8%) claimed they were not counseled at all. Seventy nine (34.2%) reported missing their doses. Demographic and clinical characteristics of the study population and the reasons for missing doses are presented in Table 1. Out of the 231 patients, 152 (65.8%) had adherence > 95% (95% CI: 59.3-71.9) while 79 (34.2%) had adherence < 95% (95% CI: 28.1-40.7).
Table 1.
Demographic and clinical characteristics of the study population (N=231)
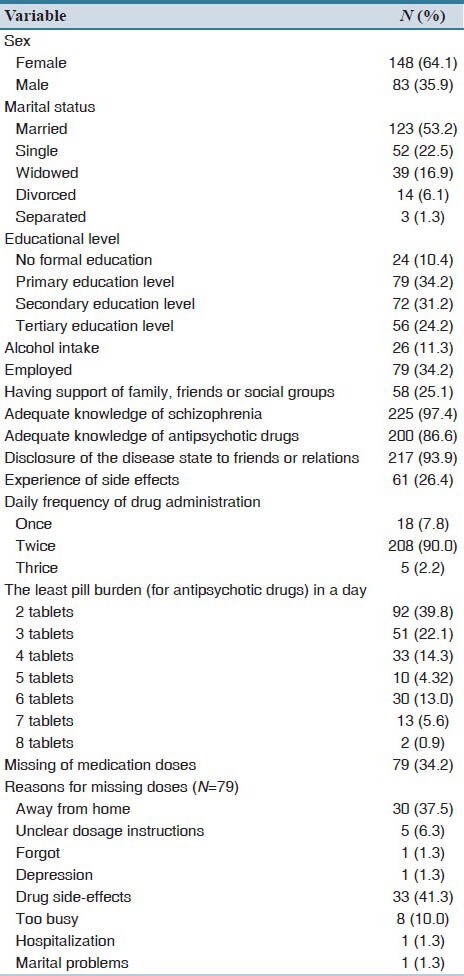
Sixty one (26.4%) respondents experienced side-effects with the commonest being extrapyramidal and anticholinergic side-effects.
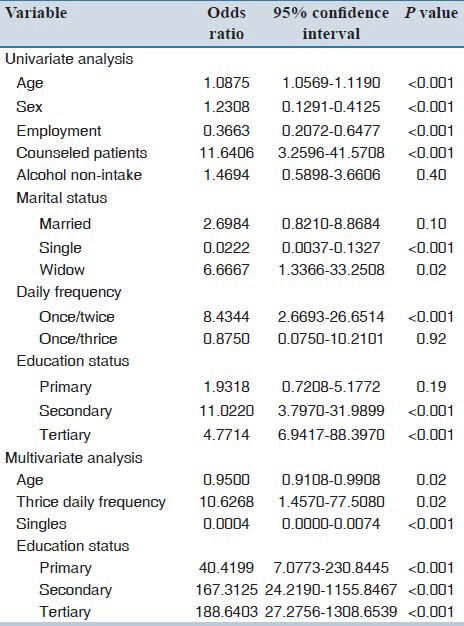
Variables associated with adherence
In the univariate analysis, age, frequency of drug intake, employment status, counseling status as well as educational status were all associated with good antipsychotic medication adherence [Table 2]. However, when all the variables were subjected to a multivariable logistic regression model, the best predictors of antipsychotic medication adherence were found to be age, three times daily frequency of administration and educational level [Table 2].
Table 2.
Variables associated with adherence
DISCUSSION
We found the overall proportion of out-patients with good adherence to antipsychotics therapy to be 65.8%, higher than that found in a similar study in South Western Nigeria in which the level of adherence was found to be 48%.[8] Drug adherence counseling at the time and point of drug pick up as well as the putting in place of Pharmaceutical Care strategies may have been responsible for this difference. Drug side-effects as shown in this study, has also been highlighted by other literature sources[9] as one of the most common reasons for missing doses. The other reasons we found were travelling away from home, being too busy and dosage instructions that are not clear as can be seen in Table 1. the implication of this is that these patients need medication adherence counseling intensification on the different side-effects and how to manage them. as has been suggested, this reduces the impact of perceived concerns[10] or increases the necessity of antipsychotic treatment.[11] Depression, marital problems, forgetfulness and hospitalization are also reasons that have been adduced for missing doses.[12] In this regard, adherence counseling employing a team approach (involving other health care givers such as physicians, pharmacists, nurses, psychologists and social support groups) may be effective. There is concurrence with this in literature given the assertion in some reports that adherence counseling is teamwork and that shared-decision making approach is needed in psychiatric drug adherence counseling.[13,14]
A number of variables (age, sex, employment, counseled patients, Educational level and marital status and alcohol intake, daily frequency of medication intake and pill burden) were identified as being associated with antipsychotic medication adherence in the univariate analysis. The study showed that medication adherence was higher in older patients. This is in consonance with other studies where age has been found to have a predictive value with respect to medication adherence. The main reason being that older patients may be more familiar with correct medication usage and increasing awareness of the fact that their disease condition is one that requires optimal adherence to medications.[15]
In the multivariate analysis, age, thrice daily frequency of drug administration, marital status (whether married or single) and literacy/level of education were the factors most strongly associated with adherence. This is not unexpected; older patients are more likely to be adherent in consonance with the reason given in the preceding paragraph. Marital status will play a part because those who are married would have a partner that will provide the much needed social support that might assist in medication adherence. Adewuya et al., found this to be so.[8] The literacy level is another factor that impacts medication adherence positively. Literature sources suggest that increasing education may increase knowledge of the disease condition as well as drugs and this can increase adherence. Thus, persons with higher levels of education should be expected to have higher adherence.[15]
In conclusion, medication adherence as a function of pharmaceutical care improves the effectiveness of antipsychotic drugs used in the management of psychosis. Factors that affect adherence to antipsychotic drugs include non-intake of alcohol and an older age as well as a reduction in the daily frequency of drug intake. We recommend that at the point of issuance of drugs to patients, pharmacists should intensify medication adherence counseling with special focus on patients being placed on antipsychotic drugs for the first time as younger patients even as patients should be encouraged to join social support groups.
The generalizability of the results of this study may be limited by the fact that only out-patients with chronic schizophrenia were studied, medication adherence was measured by a subjective assessment strategy and the fact that adherence to typical and atypical antipsychotics was not distinguished.
AUTHORS’ CONTRIBUTION
All authors contributed actively at all stages of the study and in preparation of the manuscript.
All authors participated in the concept design and preparation of the manuscript. JD, KDF, RAB and NSJ also participated in the literature search, data acquisition and analysis. DAD and HOD also participated in editing and reviewing the manuscript. All authors read and approved the final version submitted for publication.
ACKNOWLEDGMENTS
The authors acknowledge the interest and support of the Head of Pharmacy Department as well as the staff of the Psychiatric pharmacy unit and consultants in the Department of Psychiatry at the Jos University Teaching Hospital.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Geneva, Switzerland: World Health Organization; 2008. [Last accessed on 2013 Apr 5]. World Health Organization. The Global Burden of Disease: 2004 Update. Available from: http://www.who.int/healthinfo/global_burden_disease/GDB_report_2004updat_fullpdf . [Google Scholar]
- 2.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, et al. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the epidemiologic catchment area (ECA) study. JAMA. 1990;264:2511–8. [PubMed] [Google Scholar]
- 3.Adewuya AO, Makanjuola RO. Lay beliefs regarding causes of mental illness in Nigeria: Pattern and correlates. Soc Psychiatry Psychiatr Epidemiol. 2008;43:336–41. doi: 10.1007/s00127-007-0305-x. [DOI] [PubMed] [Google Scholar]
- 4.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp Pharm. 1990;47:533–43. [PubMed] [Google Scholar]
- 5.Coons SJ, Johnson JA. Humanistic outcomes. In: Smith MC, Wertheiner AI, editors. Social and Behavioural Aspects of Pharmaceutical Care. New York: Pharmaceutical Products; 1996. pp. 403–45. [Google Scholar]
- 6.Kucukarslan S, Schommer JC. Patients’ expectations and their satisfaction with pharmacy services. J Am Pharm Assoc (Wash) 2002;42:489–95. doi: 10.1331/108658002763316923. [DOI] [PubMed] [Google Scholar]
- 7.Brodie DC, Parish PA, Poston JW. Societal needs for drugs and drug-related services. Am J Pharm Educ. 1980;44:276–8. [PubMed] [Google Scholar]
- 8.Adewuya AO, Owoeye OA, Erinfolami AR, Coker AO, Ogun OC, Okewole AO, et al. Prevalence and correlates of poor medication adherence amongst psychiatric outpatients in Southwestern Nigeria. Gen Hosp Psychiatry. 2009;31:167–74. doi: 10.1016/j.genhosppsych.2008.12.005. [DOI] [PubMed] [Google Scholar]
- 9.Rettenbacher MA, Hofer A, Eder U, Hummer M, Kemmler G, Weiss EM, et al. Compliance in schizophrenia: Psychopathology, side effects, and patients’ attitudes toward the illness and medication. J Clin Psychiatry. 2004;65:1211–8. doi: 10.4088/jcp.v65n0908. [DOI] [PubMed] [Google Scholar]
- 10.Taira M, Hashimoto T, Takamatsu T, Maeda K. Subjective response to neuroleptics: The effect of a questionnaire about neuroleptic side effects. Prog Neuropsychopharmacol Biol Psychiatry. 2006;30:1139–42. doi: 10.1016/j.pnpbp.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 11.Beck EM, Cavelti M, Wirtz M, Kossowsky J, Vauth R. How do socio-demographic and clinical factors interact with adherence attitude profiles in schizophrenia? A cluster-analytical approach. Psychiatry Res. 2011;187:55–61. doi: 10.1016/j.psychres.2010.10.012. [DOI] [PubMed] [Google Scholar]
- 12.Lacro JP, Dunn LB, Dolder CR, Leckband SG, Jeste DV. Prevalence of and risk factors for medication non-adherence in patients with schizophrenia: A comprehensive review of recent literature. J Clin Psychiatry. 2002;63:892–909. doi: 10.4088/jcp.v63n1007. [DOI] [PubMed] [Google Scholar]
- 13.Deegan PE, Drake RE. Shared decision making and medication management in the recovery process. Psychiatr Serv. 2006;57:1636–9. doi: 10.1176/ps.2006.57.11.1636. [DOI] [PubMed] [Google Scholar]
- 14.Hamann J, Kruse J, Schmitz FS, Kissling W, Pajonk FG. Patient participation in antipsychotic drug choice decisions. Psychiatry Res. 2010;178:63–7. doi: 10.1016/j.psychres.2008.08.008. [DOI] [PubMed] [Google Scholar]
- 15.Falang KD, Akubaka P, Jimam NS. Patient factors impacting antiretroviral drug adherence in a Nigerian tertiary hospital. J Pharmacol Pharmacother. 2012;3:138–42. doi: 10.4103/0976-500X.95511. [DOI] [PMC free article] [PubMed] [Google Scholar]


