Abstract
Objective:
The objective of this study is to analyze the health-care cost by calculating the direct and indirect costs of diabetes with co-morbidities in south India.
Methods:
A prospective observational study was conducted at Rohini super specialty hospital (India). Patient data as well as cost details were collected from the patients for a period of 6 months. The study was approved by the hospital committee prior to the study. The diabetic patients of age >18 years, either gender were included in the study. The collected data was analyzed for the average cost incurred in treating the diabetic patients and was calculated based on the total amount spent by the patients to that of total number of patients.
Findings:
A total of 150 patients were enrolled during the study period. The average costs per diabetic patient with and without co-morbidities were found to be United States dollar (USD) 314.15 and USD 29.91, respectively. The average cost for those with diabetic complications was USD 125.01 for macrovascular complications, USD 90.43 for microvascular complications and USD 142.01 for other infections. Out of USD 314.15, the average total direct medical cost was USD 290.04, the average direct non-medical cost was USD 3.75 and the average total indirect cost was USD 20.34.
Conclusion:
Our study results revealed that more economic burden was found in male patients (USD 332.06), age group of 51-60 years (USD 353.55) and the patients bearing macrovascular complications (USD 142.01). This information can be a model for future studies of economic evaluations and outcomes research.
Keywords: Cost analysis, diabetes, economics, health-care
INTRODUCTION
Pharmacoeconomic evaluations have grown to be an essential tool in therapeutic decision making especially in chronic diseases like diabetes, where there are limited resources. Pharmacoeconomic research is the process of identifying, measuring and comparing the cost, risks and benefit of programs, services or therapies and determining, which alternatives produce the best health outcomes for resource invested.[1,2] The economic burden of diabetes mellitus (DM) on patients, institutions and society in the form of direct and indirect costs is enormous world-wide. The prevalence of DM is rising in alarming scale in India, which poses a major threat to clinical management, economic growth and social well-being of the patients.[3,4] In 2011, 366 million adults with diabetes were recognized and by 2030 this will definitely rise to 552 million adults. This number will be continuing to increase globally due to the high growth of population size, age, urbanization and high prevalence of obesity and sedentary life-style.[5] In 2011, a total of 4.6 million deaths were reported with diabetes. The total health care expenditures were Unites States (US) 465 billion dollars in the same year of which 11% were adults within the age group of 20-79 years.[6] Although the South-East Asia region comprises only seven countries, it is one of the most heavily populated regions in the world. The adult population of India alone accounts for 86% of the region's total population of 856 million in 2011. Current estimates indicate that 8.3% of the South-East Asian adult population or 71.4 million people had diabetes in 2011 of which 61.3 million are from India. The number of people with diabetes in India, Bangladesh and Sri Lanka make up to 99% of the total region. The estimated regional diabetes prevalence increases to 10.2% in 2030 as a consequence of increasing life expectancy in India (the proportion of the population over 50 years is expected to increase from 16% to 23% from 2011 to 2030).[7] The main objective of this study is to analyze the healthcare cost by calculating the direct and indirect costs of diabetes with co-morbidities in south India.
METHODS
A prospective observational study was conducted at super-specialty hospital, Andhra Pradesh, India. Patient's data as well as cost details were collected from the records for a period of 6 months (February-July 2012). The study was approved by the hospital committee prior to the study initiation. The diabetic patients of age greater than 18 years, either gender who stayed in hospital for a minimum of 2 days were included in the study. Out-patients, pregnant women and those who avail reimbursement were excluded.
A total of 150 patients were identified during ward rounds and through regular case record reviews during study period. The enrolled patients were followed from the day of admission until the day of discharge and the relevant study data including age, sex, height, weight, education, occupation, body mass index (BMI), smoking habit and medical and social history were collected. Total direct costs include direct medical and non-medical costs. The direct medical cost includes the medication costs, cost of laboratory investigations, cost of consultation and cost of hospitalization and the direct non-medical costs include the transportation cost to hospital and cost of food during the hospitalization. The indirect costs (i.e., productivity loss) were determined based on modified labor force, employment and earnings data based on job category for patients who were employed during the evaluation period.[8] The costs of drugs, syringes, administration, extra nursing and medical care and any other invasive or non-invasive procedures along with laboratory tests were collected. All the relevant and necessary data was collected from patient's case notes, treatment charts, laboratory reports, interviewing patients or patient care takers, interviewing health-care professionals, or other relevant sources. Data pertaining to the cost of extra medications and administration devices was collected from the patient (interviewing), patient case sheets, nurses and pharmacy records.
The data observed was analyzed for the average cost incurred in treating the diabetic patients and was calculated based on the total amount spent by the patients to that of total number of patients. Patient perspective was taken for the analysis of cost component and the details were collected by direct patient interview. Details of direct medical cost, direct non-medical cost and indirect cost were analyzed. Other costs such as intangible cost and opportunity cost were excluded. From the data obtained, overall cost per diabetic patient as well as total cost per period of 6 months was calculated. All the costs data of Indian Rupee (INR) was converted into United States dollar (USD) at the rate of 1 USD = 54.26 INR value in the year 2012.
RESULTS
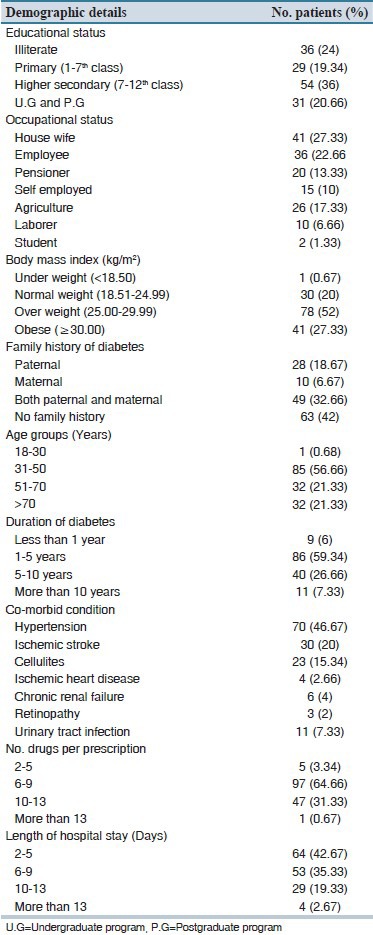
A total of 150 patients were enrolled during the study period. Out of 150 patients, 100 (66.67%) were males and 50 (33.33%) were females. The other demographic details such as age, educational status, occupational status, family history and duration of diabetes, BMI, co-morbidities, length of hospital stay and number of drugs per prescription were summarized in Table 1.
Table 1.
Demographic details of the studied patients (N=150)
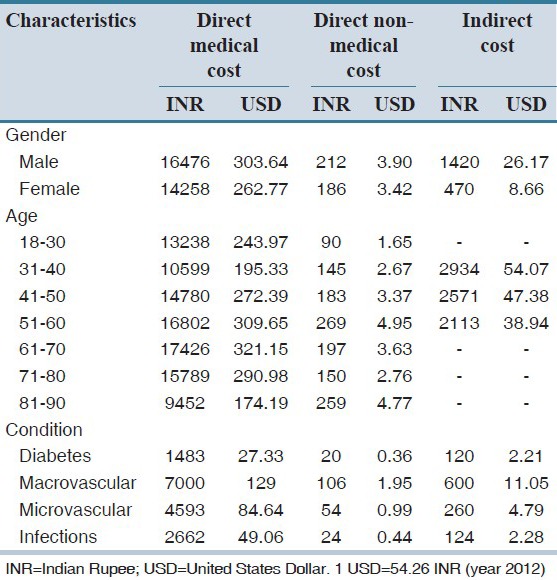
The average total cost per diabetic patient without complications was USD 29.91. Out of USD 29.91, the average total direct medical cost per patient was USD 27.33 (91.37%); direct non-medical cost was USD 0.36 (1.23%) and indirect cost was USD 2.21 (7.4%). The average total cost for the treatment of diabetes with co-morbidities per patient was found to be USD 314.15. Out of USD 314.15, the average total direct medical cost per patient was USD 290.04 (92.41%); direct non-medical cost was USD 3.75 (6.47%) and indirect cost was USD 20.34 (1.12%). The individual total direct medical cost components of diabetic patients (n = 150) were summarized in the Table 2. Out of 150 patients, the patients who have macrovascular complications were found to spend more health care cost compared with others. The male patients were found to have more healthcare cost compared to female patients. Furthermore, the age group of 61-70 years was found to have spent more health care cost than others. Individual costs were summarized in Table 3.
Table 2.
Direct medical cost components (per patient) in the studied diabetic patients (total cost: INR. 15738, USD. 255.32)
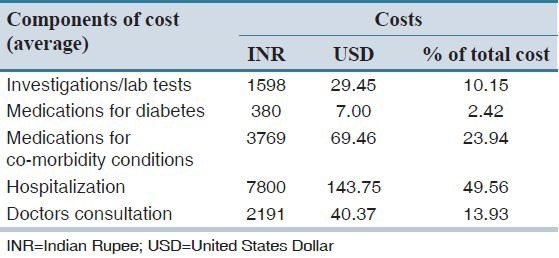
Table 3.
Heath care cost (per patient) for gender and age wise distribution, diabetes and its complications among the studied patients
DISCUSSION
Our study results reveal that the cost of hospitalization, consultation and cost for other drugs were high and the cost of investigation and cost of medication for diabetes were less when compared to the study conducted by Kapur et al.[9] The overall average health care costs during the hospital stay were found to be higher in males than females and it was also found to be higher in the age group of 51-60 years followed by 61-70 years, which might be due to increased number of co-morbidities; similar results were found in the Henriksson et al., Al-Maskari et al., and Hogan et al. studies.[10,11,12] The overall average health care costs were found to be higher in the patients who have history of DM for more than 5 years when compared to those with a history of less than 5 years DM. Furthermore, the overall healthcare costs were found to be higher in the patients with more than three co-morbidities, which may be due to the more number of medications, laboratory investigations, consultations and hospitalization. In the present study, there was a positive relationship between increased costs of health care services with increased number of complications. In addition, the average healthcare costs were significantly increased with the increased length of the stay of the patients in the hospital. The hospital admission accounts for the largest part of diabetes cost; besides, the extra-need for inpatient hospital care for patients who have developed late complications will greatly affect cost, since hospital bed-day has a relatively high unit cost compared with other resources and overall medication costs.[13] Furthermore, most of the diabetics consuming oral hypoglycemic agents will receive insulin soon after hospital admission for complications and this further increase the costs. It has been documented that urban people spend more money on diabetes compared with rural counterpart, not only due to better awareness but also due to greater affordability. The present study focuses on the direct and indirect cost spent due to type 2 diabetes by patients in semi-urban setup. Patients needed consultation not only from physicians, but also from cardiologists and surgeons, which may cause the increased health care cost. The main limitations of this study include its duration (6 months) and performing in a single center. In future, multi-central studies should be conducted to compare cost of diabetes.
To the best of our knowledge, it is the first study in assessing the health care costs of diabetes in south Indian population, Andhra Pradesh. This information can be a model for future studies of economic evaluations and outcomes research.
AUTHORS’ CONTRIBUTION
All authors contributed in the idea of research, design of study, data analysis and manuscript preparation.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.McGhan WF. Introduction to pharmacoeconomics. In: Arnold RJ, editor. Pharmacoeconomics from Theory to Practice. New York: CRC Press; 2010. pp. 4–5. [Google Scholar]
- 2.Rascati KL. Future issues. In: Rascati KL, editor. Essentials of Pharmacoeconomics. Philadelphia: Lippincott, Williams and Wilkins; 2008. pp. 227–36. [Google Scholar]
- 3.Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, et al. High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia. 2001;44:1094–101. doi: 10.1007/s001250100627. [DOI] [PubMed] [Google Scholar]
- 4.Ramachandran A, Snehalatha C, Latha E, Vijay V, Viswanathan M. Rising prevalence of NIDDM in an urban population in India. Diabetologia. 1997;40:232–7. doi: 10.1007/s001250050668. [DOI] [PubMed] [Google Scholar]
- 5.Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract. 2010;87:293–301. doi: 10.1016/j.diabres.2010.01.026. [DOI] [PubMed] [Google Scholar]
- 6.International Diabetes Federation. The global burden, diabetes atlas. [Last cited on 2013 Aug 1]. Available from: http://www.idf.org//2011/diabetes-atlas/5e .
- 7.International Diabetes Federation. Diabetes atlas, South East Asia. [Last cited on 2013 Aug 10]. Available from: http://www.idf.org/diabetesatlas/5e/south-east-asia .
- 8.Montvale, NJ: Medical Economics Company, Inc; 2001. Medical Economics Data (Firm). The Red Book; pp. 1–856. [Google Scholar]
- 9.Kapur A. Economic analysis of diabetes care. Indian J Med Res. 2007;125:473–82. [PubMed] [Google Scholar]
- 10.Henriksson F, Agardh CD, Berne C, Bolinder J, Lönnqvist F, Stenström P, et al. Direct medical costs for patients with type 2 diabetes in Sweden. J Intern Med. 2000;248:387–96. doi: 10.1046/j.1365-2796.2000.00749.x. [DOI] [PubMed] [Google Scholar]
- 11.Al-Maskari F, El-Sadig M, Nagelkerke N. Assessment of the direct medical costs of diabetes mellitus and its complications in the United Arab Emirates. BMC Public Health. 2010;10:679. doi: 10.1186/1471-2458-10-679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hogan P, Dall T, Nikolov P American Diabetes Association. Economic costs of diabetes in the US in 2002. Diabetes Care. 2003;26:917–32. doi: 10.2337/diacare.26.3.917. [DOI] [PubMed] [Google Scholar]
- 13.Ballesta M, Carral F, Olveira G, Girón JA, Aguilar M. Economic cost associated with type II diabetes in Spanish patients. Eur J Health Econ. 2006;7:270–5. doi: 10.1007/s10198-006-0367-9. [DOI] [PubMed] [Google Scholar]


