Abstract
Fixed drug eruption (FDE) is an unusual adverse effect of any drug, especially antibiotics like clarithromycin. Herein we report a case of clarithromycin induced FDE in a 30-year-old man who presented with recurrent erythematous and pruritic cutaneous lesions on the lower lip, right hand and left thigh. The lesions were initially misdiagnosed as lichen planus and treated with topical steroids. Each recurrence was at the same site and the lesions faded within 2 weeks leaving behind violacceous pigmentation. All the cutaneous lesions were reproduced following an oral provocation test thus confirming the diagnosis of clarithromycin induced FDE, which is a rare occurrence. When it does occur, it is often misdiagnosed, so physicians should be aware of this condition in order to prevent future recurrences as it causes a lot of cosmetic and physical discomfort to the patient.
Keywords: Clarithromycin, fixed drug eruption, oral provocation test
INTRODUCTION
Clarithromycin, a macrolide antibiotic, is a frequently prescribed drug in clinical practice. Though side-effects such as diarrhea, dizziness, headache, nausea and rashes are well known with clarithromycin, fixed drug eruption (FDE) is thought to be unusual. We have come across only four such case reports in the literature and hence we present an unusual case of clarithromycin induced FDE we encountered at our center.
CASE REPORT
This was a case report of a 30-year-old man who presented to the out-patient department of medicine with the complaints of itching and redness over the lower lip, right hand, left thigh and genitals. He had no other systemic complaints. Local examination revealed a red erythematous macule on the dorsal aspect of the right index finger and a similar lesion on the anterior aspect of the left thigh and the right corner of the lower lip [Figures 1 and 2]. Though he complained of itching over the genitals, no lesion was noted. General examination revealed normal vital signs, other systems being unremarkable. Patient had no notable past medical history. However, he had a clinical history of being prescribed oral clarithromycin for upper respiratory tract infection at a medical center 1 week back. Our patient denied consumption of any other drugs or of having a reaction to any drug in the past. At this point patient sought the opinion of a dermatologist and a diagnosis of lichen planus was made. He was treated with topical steroids and eventually the macules faded after 2 weeks leaving a violacceous pigmentation behind. At 4 months later, he again developed erythematous macules over the same sites mentioned above. This time patient had clinical history of consuming two tablets from the Helicobacter pylori Kit (H. pylori eradication therapy) as prescribed to him by a private practitioner. Within 2 h of consumption of the first-dose, he developed itching and redness over the same sites involved during the first episode. This time the patient suspected that the symptoms could have been caused by the drugs and visited us for a consult. Review of the contents of the H. pylori Kit revealed the presence of clarithromycin along with lansoprazole and amoxycillin. Further doses of the drugs were withheld and eventually the lesions faded away with hyperpigmentation within the next 2 weeks. An oral challenge test with the three drugs was conducted 4 weeks later, each drug of the three drugs being tested separately 2 weeks apart. Patient tolerated amoxycillin and lansoprazole without any adverse effects. However following challenge with oral clarithromycin, the patient developed similar skin changes 2 h after intake, hence supporting the diagnosis of FDE secondary to clarithromycin. Patient refused skin biopsy for further confirmation. We counseled him regarding the nature of the drug reaction and recommended avoidance of clarithromycin in future.
Figure 1.

Fixed drug eruption in the form of erythematous plaques on the dorsal aspect of the right index finger and the base of the right middle finger
Figure 2.
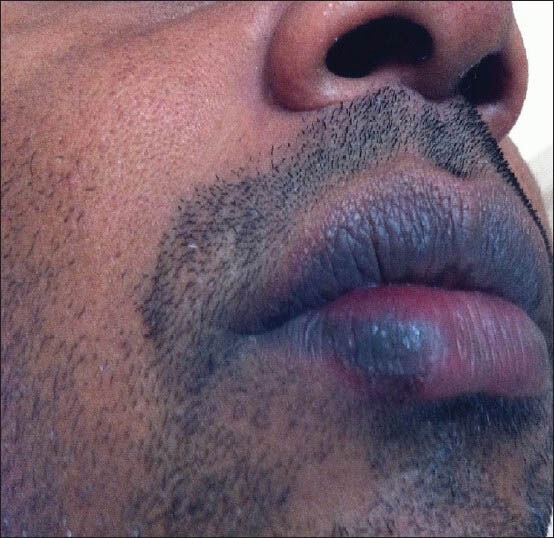
Fixed drug eruption on the right corner of the lower lip
DISCUSSION
Fixed drug reaction is a very rare adverse effect of any drug, especially antibiotics like clarithromycin and very few cases have been reported in the literature.[1,2,3] A FDE is characterized by the presence of a single or multiple, pruritic, well circumscribed erythematous plaques or macules. These lesions have a tendency to recur at same sites and heal with residual hyperpigmentation.[4] The healed lesions remain dormant until re-exposure of the causative drug. Most of the studies on FDE due to drugs demonstrated a higher occurrence in men compared with women.[5] The most commonly affected sites are trunk and limbs followed by lips and genitals.[6]
FDE is considered a form of delayed hypersensitivity, mediated by CD8+ T-cells. The reaction occurs when patients become sensitized to a particular drug and intermittent drug administration is more likely to cause sensitization than continuous use. Oral challenge test is a useful method for diagnosing the reaction.[7] Dermal biopsy is also of help in the diagnosis of FDE. Dermal biopsy of a lesion will demonstrate spongiosis, hydropic degradation of the basal layer and a lymphocytic infiltrate with dermal macrophages.[8]
FDE from clarithromycin, a commonly used drug, is a very rare occurrence. When it does occur, it is often misdiagnosed. Physicians should be aware of this condition in order to prevent future recurrences as it causes a lot of cosmetic and physical discomfort to the patient.
AUTHORS’ CONTRIBUTION
Dr. Naveen L and Dr. Santoshi Malkarnekar were responsible for the concept, design, literature search and review as well the manuscript preparation. Both the authors were responsible for the medical attention given to the patient.
ACKNOWLEDGMENTS
We express our gratitude to R. L. Jallappa Hospitals, Sri Devaraj Urs Medical College and University and Department of Medicine for their support.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Hamamoto Y, Ohmura A, Kinoshita E, Muto M. Fixed drug eruption due to clarithromycin. Clin Exp Dermatol. 2001;26:48–9. doi: 10.1046/j.1365-2230.2001.00760.x. [DOI] [PubMed] [Google Scholar]
- 2.Rosina P, Chieregato C, Schena D. Fixed drug eruption from clarithromycin. Contact Dermatitis. 1998;38:105. doi: 10.1111/j.1600-0536.1998.tb05661.x. [DOI] [PubMed] [Google Scholar]
- 3.Alonso JC, Melgosa AC, Gonzalo MJ, García CM. Fixed drug eruption on the tongue due to clarithromycin. Contact Dermatitis. 2005;53:121–2. doi: 10.1111/j.0105-1873.2005.0650h.x. [DOI] [PubMed] [Google Scholar]
- 4.Lee HJ, Kim HS, Park YM, Kim HO, Lee JY. Fixed drug eruption due to allopurinol: Positive oral provocation. Ann Dermatol. 2011;23:402–3. doi: 10.5021/ad.2011.23.S3.S402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mahboob A, Haroon TS. Drugs causing fixed eruptions: A study of 450 cases. Int J Dermatol. 1998;37:833–8. doi: 10.1046/j.1365-4362.1998.00451.x. [DOI] [PubMed] [Google Scholar]
- 6.Sharma VK, Dhar S, Gill AN. Drug related involvement of specific sites in fixed eruptions: A statistical evaluation. J Dermatol. 1996;23:530–4. doi: 10.1111/j.1346-8138.1996.tb02646.x. [DOI] [PubMed] [Google Scholar]
- 7.Lammintausta K, Kortekangas-Savolainen O. Oral challenge in patients with suspected cutaneous adverse drug reactions: Findings in 784 patients during a 25-year-period. Acta Derm Venereol. 2005;85:491–6. doi: 10.1080/00015550510042859. [DOI] [PubMed] [Google Scholar]
- 8.Morgan JM, Carmichael AJ. Fixed drug eruption with fluconazole. BMJ. 1994;308:454. doi: 10.1136/bmj.308.6926.454a. [DOI] [PMC free article] [PubMed] [Google Scholar]


