Abstract
Objective:
Incomplete medication histories obtained on hospital admission are responsible for more than 25% of prescribing errors. This study aimed to evaluate whether pharmacy technicians can assist hospital physicians’ in obtaining medication histories by performing medication reconciliation and prescribing reviews. A secondary aim was to evaluate whether the interventions made by pharmacy technicians could reduce the time spent by the nurses on administration of medications to the patients.
Methods:
This observational study was conducted over a 7 week period in the geriatric ward at Odense University Hospital, Denmark. Two pharmacy technicians conducted medication reconciliation and prescribing reviews at the time of patients’ admission to the ward. The reviews were conducted according to standard operating procedures developed by a clinical pharmacist and approved by the Head of the Geriatric Department.
Findings:
In total, 629 discrepancies were detected during the conducted medication reconciliations, in average 3 for each patient. About 45% of the prescribing discrepancies were accepted and corrected by the physicians. “Medication omission” was the most frequently detected discrepancy (46% of total). During the prescribing reviews, a total of 860 prescription errors were detected, approximately one per medication review. Almost all of the detected prescription errors were later accepted and/or corrected by the physicians. “Dosage and time interval errors” were the most frequently detected error (48% of total). The time used by nurses for administration of medicines was reduced in the study period.
Conclusion:
This study suggests that pharmacy technicians can contribute to a substantial reduction in medication discrepancies in acutely admitted patients by performing medication reconciliation and focused medication reviews. Further randomized, controlled studies including a larger number of patients are required to elucidate whether these observations are of significance and of importance for securing patient safety.
Keywords: Geriatric ward, medication administration time, medication reconciliation, medication review, pharmacy technicians
INTRODUCTION
Prescribing errors occur commonly for adult patients, and will probably affect 50% of all hospital admissions.[1] Incomplete medication histories obtained at hospital admission are responsible for more than 25% of prescribing errors occurring in hospitals.[2] Some of the best-known contributing factors of prescribing errors are inadequate knowledge of the prescribed medication or the patients’ medical history; whereas some other error-provoking conditions could be the lack of training or experience, fatigue, stress, high workload for the prescriber and inadequate communication between health care professionals.[3] Beside the use of sophisticated computer techniques, the participation of pharmacists in the medication prescribing process has produced a tremendous reduction in the number of prescribing errors.[4] Many of the studies have shown that pharmacists can enhance the accuracy of available information on patients’ medication use if the pharmacist carries out medication reconciliation when the patients are admitted to the hospital.[5,6,7,8,9]
Only a few studies have reported results from pharmacy technicians obtaining medication histories and conducting medicine reviews. Studies comparing pharmacists and pharmacy technicians in obtaining precise and accurate medication histories showed that pharmacy technicians had the same accuracy and completeness when compared with pharmacists,[10,11,12] therefore it might be beneficial to include pharmacy technicians in some clinical pharmacy activities. At the same time, pharmacy technicians could replace pharmacist so they can use their pharmaceutical competencies in conducting more challenging tasks, i.e. medication reviews of complicated poly-pharmacy taking patients, cancer patients, etc., A multicenter intervention study conducted at 12 Dutch hospitals showed that pharmacy-based medication reconciliation in which also pharmacy technicians participated resulted in a substantial reduction in the number of medical discrepancies in acutely admitted elderly adults.[13] A study evaluating the impact of pharmacy technicians doing reconciliation services on medication discrepancies on admissions in a mental health department showed that trained pharmacy technicians were able to reduce the frequency of medication discrepancies significantly.[14] To the best of our knowledge, no studies have yet explored the value of using pharmacy technicians in both conducting medication reconciliation and prescribing reviews in geriatric wards.
The ratio between pharmacists and pharmacy technicians (pharmaconomists) working in Danish hospital pharmacies is around 1:4. Danish pharmacy technicians undergo a 3-year formal education, which takes place partly at a pharmacy-school for technicians and in a private pharmacy. During the education period, the pharmacy technicians are trained in medical and pharmaceutical disciplines such as anatomy, pathology, pharmacology, ethics, and patient communication.
In this study, we define medication reconciliation as a process in which the patients’ medication history and changes in drug prescribing information at the time of admission to the acute ward and at the time of transferring to other hospital departments are notified using multiply medication information resources.
We also defined focused prescribing reviews as a technical review which secures that prescribing of each medicinal product to patients is based on national accepted guidelines and evidence based practice. The core of the prescribing reviews is the patients’ drug prescriptions, in which the pharmacy technicians check whether the name of the medicinal product is listed in the hospital drug formulary and whether the strength of the drug and the administered doses are consistent with the recommendations.
The primary aim of this study was to evaluate whether pharmacy technicians can assist hospital physicians’ in obtaining medication histories by performing medication reconciliation and prescribing reviews. A secondary aim was to evaluate whether the interventions made by pharmacy technicians could reduce the time spent by the nurses on administration of medications to the patients.
METHODS
The study was performed over a 7 week period from October to December 2012 at the Department of Geriatric Medicine, Odense University Hospital, Denmark. The department contains of 35 hospital beds with an average patient admission time of 7-8 days, and the average age of the admitted patients were 84 years. During the study period, two pharmacy technicians were present at the geriatric ward every day from 8 a.m. to 3 p.m., Monday to Friday. In order to secure consistency and minimize bias, it was decided that two pharmacy technicians who were trained together by the clinical pharmacist should conduct the medication reconciliation and prescribing reviews at the ward.
A cooperation agreement, describing the pharmacy technicians’ tasks on the ward as well as multiply focus areas (standard operation procedures) describing in details which drug interventions the pharmacy technicians were permitted to do during the study period were written by a clinical pharmacist and a clinical pharmacologist. The procedures were later approved by the Head of the Geriatric Department. The defined tasks for the pharmacy technicians were to conduct medication reconciliation on the time of patients’ hospital admission and to perform focused medication reviews on all admitted patients, each day. The pharmacy technicians were trained by clinical pharmacists in performing medication reconciliation and the focused medication reviews according to the cooperation agreement. The clinical pharmacist also trained the pharmacy technicians on how to make notes in the electronic patient records. During the study period, the pharmacy technicians were able to consult the clinical pharmacist in cases of doubt. Before the study period, the ward staffs were informed about the study through information leaflets and an oral presentation made by a senior physician.
Medication reconciliation
All patients admitted to the geriatric ward from Monday to Friday during the study period were included in the study. On admittance, physicians entered the patients’ actual medication history in the electronic medical record (EMR) as part of the daily routine. Afterwards, pharmacy technicians performed medication reconciliation review. In the process, as many information sources as possible were included in order to obtain a precise and actual medication list. Pharmacy technicians could conduct interviews with the patient, patient relatives, general practitioner, and/or home care nurses in order to collect information about the use of over-the-counter medicine, complementary medicine, etc., Information sources such as the personal electronic medication profile (PEM), and home care notes were used to obtain an overview over the patient's medicine history. PEM is an online electronic system that has complete information on all Danish citizens’ prescriptions and purchases of medicine. Information about the patients’ use of over-the-counter-medicine and complementary medicine cannot be found in the PEM. Access is only for authorized persons, i.e. physicians and nurses. The PEM is updated every day with information about the citizens’ medicine use purchased in Danish pharmacies. Any discrepancies between the medication histories entered in the EMR by the physician and the medication history obtained by the pharmacy technicians were noted in the EMR. Latter, the physicians decided whether or not corrections in the patients’ prescriptions were necessary.
Each day, the pharmacy technicians registered the time spent on medication reconciliation and the number of medication reconciliations conducted. They also registered all inconsistencies in medicine histories. After patients’ discharge from the geriatric ward, the pharmacy technicians looked through all patient records to register how many of the inconsistencies that were later corrected by the physicians.
Focused prescribing reviews
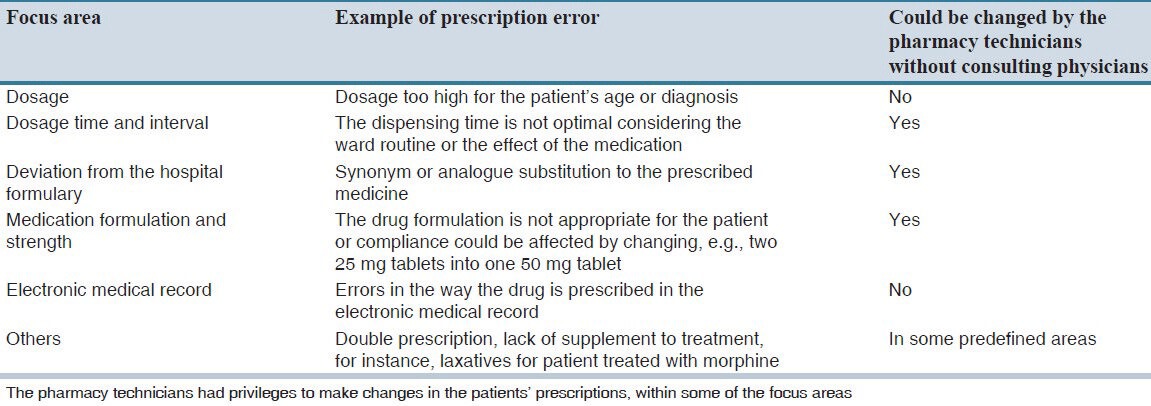
All patients admitted to the geriatric ward had their prescriptions reviewed by the pharmacy technicians on each day. The focused prescribing review were performed in order to identify prescription errors within different focus areas, as described in the cooperation agreement, and summarized in Table 1. If the pharmacy technicians detected any prescribing errors in the patients’ prescriptions and it could be corrected without consulting a physician, the pharmacy technicians were - according to the cooperation agreement - authorized to do the changes in the electronic patient record. Prescription errors that may not be corrected by the pharmacy technicians were written in a suggestion note, and then physicians afterwards decided if the suggested corrections were necessary to implement. After patients’ discharge from the geriatric ward, the pharmacy technicians looked through the patient EMR to register the number of the prescription errors that were corrected by the physicians.
Table 1.
Focus areas used for conducting prescribing reviews, including examples
Nurses’ medication administration time
Before the study, the pharmacy technicians measured the time used by nurses in dispensing medicines between 12 a.m. and 2 p.m., during a 10 day period. The same measures were conducted during the last 10 days of the study period. The end point of drug administration time by nurses was the time used for the dispensing of each medication to the individual patient. We measured only the time used in the administration process, from the time which nurses looked in EMR for each patient prescription to time in which all drugs were dispensed in a small bottle for the same patient. If the nurses were disturbed by issues not related to the drug administration to the included patients, we did stop the time. After the nurses had administered all the prescribed medications to the patients, the number of drug dispenses in the small bottle were counted. P < 0.05 was chosen as the level of statistical significance. All significance tests were two-sided. We present means and 95% confidence intervals in the result section.
RESULTS
Medication reconciliation
In total, 212 medication reconciliations and 936 focused prescribing reviews were conducted by the pharmacy technicians during the study period. The main results of the medication reconciliations and the focused prescribing reviews are displayed in Table 2.
Table 2.
Overview of the results from medication reconciliation and focused prescribing reviews conducted by the pharmacy technicians over a 7 weeks period
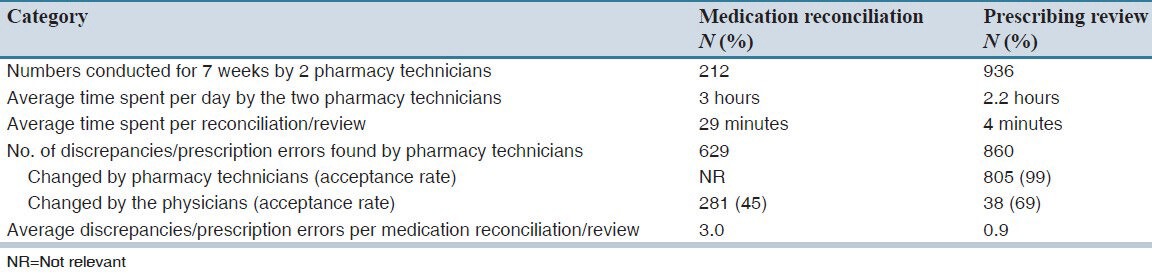
On average, pharmacy technicians spent 29 minutes on one medication reconciliation. In total, 629 discrepancies were detected during the medication reconciliations, with an average of 3 for each patient. The physicians later accepted and corrected 45% of the discrepancies.
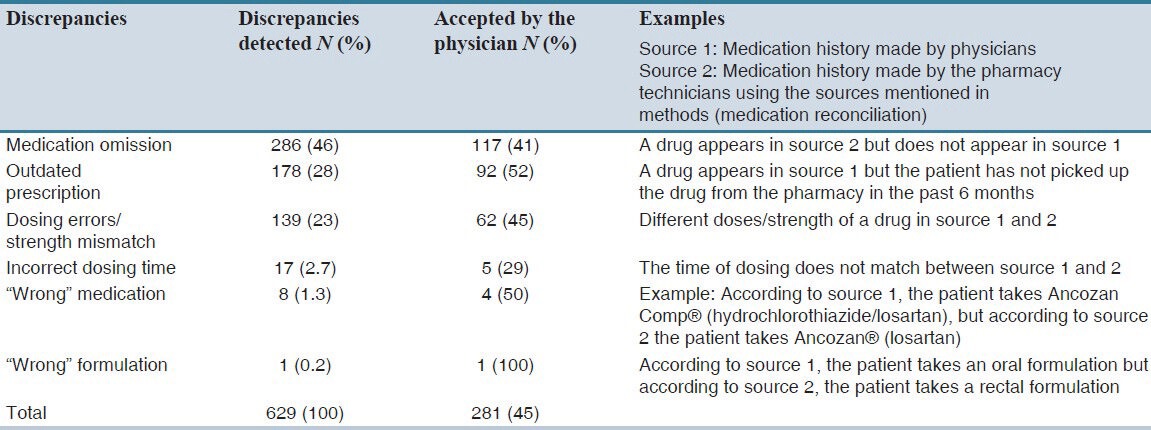
Table 3 shows an overview over the 629 discrepancies detected by the pharmacy technicians by doing medication reconciliation, and the number of corrections accepted by the physicians. The largest number of detected discrepancies was “medication omission” (46% of total). The most commonly accepted and corrected discrepancies were “dosage errors”, which were accepted by physicians in 53% of the cases.
Table 3.
Discrepancies detected during medication reconciliations made by pharmacy technicians and the number of corrections accepted by physicians
Focused prescribing reviews
On average, pharmacy technicians spent four minutes on doing a focused prescribing review During the reviews, a total of 860 prescription errors were detected, approximately one per review. The pharmacy technicians were allowed to change 805 (94% of total) prescription errors without consulting a physician according to the cooperation agreement. Almost all (96% of total errors) of the prescription errors detected were accepted or corrected by the physicians. The physicians later accepted approximately 60% of the suggestions made by the pharmacy technicians. Table 4 shows the characteristics of 860 prescription errors detected by the pharmacy technicians. “Dosage and time interval errors” were the most frequent detected (48% of total) and “EMR errors” were the least frequent (1% of total) ones. The physicians accepted almost all prescription errors including the errors corrected by the pharmacy technicians.
Table 4.
Overview of prescription errors detected in the focused prescribing reviews divided into focus areas and the number of prescription errors accepted/corrected by physicians
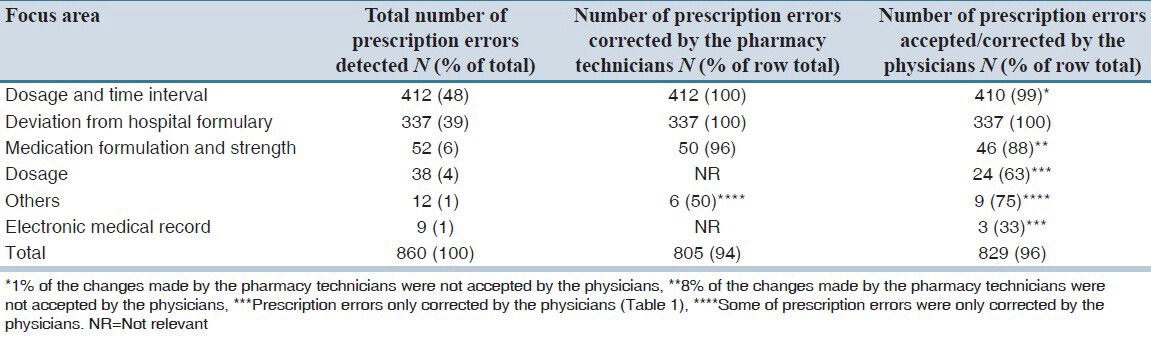
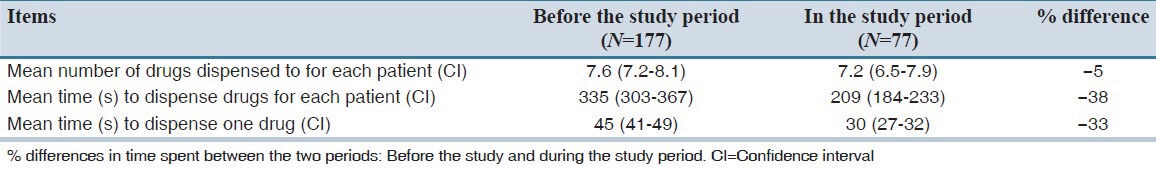
Table 5 shows the time used by nurses in dispensing medicines to patients before and during the study period. Reduction in medication dispensing time varied from 33% to 38%.
Table 5.
Time spent by the nurses for medication administration before and during the study period
DISCUSSION
Medication reconciliation
The medication reconciliation conducted by the pharmacy technicians rendered on average the finding of 3 discrepancies between the medication history obtained by the physician and the medication history taken by the pharmacy technician. Only 45% of the discrepancies found by the pharmacy technicians were accepted and corrected by the physicians. The low acceptance rate could be explained by many factors, e.g. the way the information were presented to physicians in the electronic patient chart, the physicians found the discrepancies unimportant or incorrect, or the physicians had no time to correct the discrepancies due to busy work schedules. If the pharmacy technicians should continue the job on the ward, it would be important to investigate eventual barriers and make an effort to achieve a good cooperation between the professions, thereby raising the acceptance rate. We also demonstrated that almost 30% of all patients had one or more medication discrepancies, which also were reported in other international studies.[10,11,12,13,14]
Focused medication reviews
The focused medication reviews conducted by the pharmacy technicians were not very time consuming, only four minutes on average per review. This indicates that the predetermined focus areas described in the cooperative agreement were easy for the pharmacy technicians to use in practice. The fact that all patients at the ward had their prescriptions reviewed every day by the pharmacy technicians meant, that the pharmacy technicians only had to review the patients’ new prescriptions each day, which have shortened the time used. This may also explain the finding of only 0.9 prescription errors per review. The prescription errors detected by the pharmacy technicians were well accepted by the physicians (96% of total). According to the cooperation agreement, the pharmacy technicians were allowed to correct the majority of detected errors by themselves (94% of total).
Nurses’ dispensing time
The study indicates that time spent by nurses’ on administering medicines to the patients can be reduced by the focused medication reviews conducted by the pharmacy technicians. The medication dispensing time was approximately 33% shorter in the study period. We don’t know whether this reduction in the time of nurses’ medication administration is permanent. However, from an economic perspective, this possible time reduction is interesting and this topic should be investigated further in larger studies involving pharmacist, pharmacy technicians and nurses in obtaining medication histories.
Strength and limitations of this study
This is the first study in which pharmacy technicians have conducted both medication reconciliation and prescribing reviews for geriatric patients admitted to a hospital ward. Due to the relatively long intervention period (7 weeks), and the large number of detected discrepancies and the high number of physician - accepted interventions, this study can be considered to be robust. However, the study was conducted in a single geriatric ward and the interventions only involved two pharmacy technicians, which may limits the generalizability of the findings to other geriatric wards, patient groups and pharmacy technicians.
This study suggests that pharmacy technicians can contribute to a substantial reduction in medication discrepancies in acutely admitted patients by performing medication reconciliation and focused medication reviews. Further randomized, controlled studies including a larger number of patients are required to elucidate whether these observations are of significance and of importance for securing patient safety.
AUTHORS’ CONTRIBUTION
TC Buck designed the study, analyzed data and wrote the first version of the manuscript. L Aagaard conducted a comprehensive review of the first version of the manuscript and during the peer-review process. LS Gronkjaer and JU Rosholm commented on previous versions of this article and ML Duckert carried out data sampling. All authors read and approved the final version of the manuscript.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lewis PJ, Dornan T, Taylor D, Tully MP, Wass V, Ashcroft DM. Prevalence, incidence and nature of prescribing errors in hospital inpatients: A systematic review. Drug Saf. 2009;32:379–89. doi: 10.2165/00002018-200932050-00002. [DOI] [PubMed] [Google Scholar]
- 2.Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: A systematic review. CMAJ. 2005;173:510–5. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tully MP, Ashcroft DM, Dornan T, Lewis PJ, Taylor D, Wass V. The causes of and factors associated with prescribing errors in hospital inpatients: A systematic review. Drug Saf. 2009;32:819–36. doi: 10.2165/11316560-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 4.von Laue NC, Schwappach DL, Koeck CM. The epidemiology of preventable adverse drug events: A review of the literature. Wien Klin Wochenschr. 2003;115:407–15. doi: 10.1007/BF03040432. [DOI] [PubMed] [Google Scholar]
- 5.Gardella JE, Cardwell TB, Nnadi M. Improving medication safety with accurate preadmission medication lists and postdischarge education. Jt Comm J Qual Patient Saf. 2012;38:452–8. doi: 10.1016/s1553-7250(12)38060-4. [DOI] [PubMed] [Google Scholar]
- 6.Musgrave CR, Pilch NA, Taber DJ, Meadows HB, McGillicuddy JW, Chavin KD, et al. Improving transplant patient safety through pharmacist discharge medication reconciliation. Am J Transplant. 2013;13:796–801. doi: 10.1111/ajt.12070. [DOI] [PubMed] [Google Scholar]
- 7.Ghatnekar O, Bondesson A, Persson U, Eriksson T. Health economic evaluation of the lund integrated medicines management model in elderly patients admitted to hospital. BMJ Open. 2013;3:pii: e001563. doi: 10.1136/bmjopen-2012-001563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee YY, Kuo LN, Chiang YC, Hou JY, Wu TY, Hsu MH, et al. Pharmacist-conducted medication reconciliation at hospital admission using information technology in Taiwan. Int J Med Inform. 2013;82:522–7. doi: 10.1016/j.ijmedinf.2013.01.006. [DOI] [PubMed] [Google Scholar]
- 9.Galvin M, Jago-Byrne MC, Fitzsimons M, Grimes T. Clinical pharmacist's contribution to medication reconciliation on admission to hospital in Ireland. Int J Clin Pharm. 2013;35:14–21. doi: 10.1007/s11096-012-9696-1. [DOI] [PubMed] [Google Scholar]
- 10.van den Bemt PM, van den Broek S, van Nunen AK, Harbers JB, Lenderink AW. Medication reconciliation performed by pharmacy technicians at the time of preoperative screening. Ann Pharmacother. 2009;43:868–74. doi: 10.1345/aph.1L579. [DOI] [PubMed] [Google Scholar]
- 11.Johnston R, Saulnier L, Gould O. Best possible medication history in the emergency department: Comparing pharmacy technicians and pharmacists. Can J Hosp Pharm. 2010;63:359–65. doi: 10.4212/cjhp.v63i5.947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flynn EA, Barker KN, Pepper GA, Bates DW, Mikeal RL. Comparison of methods for detecting medication errors in 36 hospitals and skilled-nursing facilities. Am J Health Syst Pharm. 2002;59:436–46. doi: 10.1093/ajhp/59.5.436. [DOI] [PubMed] [Google Scholar]
- 13.van den Bemt PM, van der Schrieck-de Loos EM, van der Linden C, Theeuwes AM, Pol AG Dutch CBO WHO High 5s Study Group. Effect of medication reconciliation on unintentional medication discrepancies in acute hospital admissions of elderly adults: A multicenter study. J Am Geriatr Soc. 2013;61:1262–8. doi: 10.1111/jgs.12380. [DOI] [PubMed] [Google Scholar]
- 14.Brownlie K, Schneider C, Culliford R, Fox C, Boukouvalas A, Willan C, et al. Medication reconciliation by a pharmacy technician in a mental health assessment unit. Int J Clin Pharm. 2013 Nov;:15. doi: 10.1007/s11096-013-9875-8. DOI: 10.1007/s11096-013-9875-8. [DOI] [PubMed] [Google Scholar]


