Abstract
Introduction
Practice guidelines recommend the use of ICDs in patients with heart failure (HF) and a left ventricular ejection fraction (LVEF) of ≤ 35% in the absence of contraindications.
Methods and Results
We performed an analysis of ICD use among patients admitted with HF with LVEF of ≤ 35% and discharged alive from 251 hospitals participating in the American Heart Association’s Get With The Guidelines-HF Program between January 2005 and September 2011. Among 35,772 guideline-eligible patients, 17,639 received an ICD prior to hospitalization (10,886), during hospitalization (4,876), or were discharged with plans to undergo ICD placement after hospitalization (1,877). After adjustment, increasing age was associated with lower ICD use (odds ratio [OR] 0.89, 95% confidence interval [CI] 0.87–0.91 per 5-year increase in age, p<0.0001). Compared with patients age < 55 years, older age groups ≥ 65 years were less likely to receive an ICD (p<0.003). Compared with men in the same age group, women were significantly less likely to receive an ICD; this difference was more marked with increasing age (p-value for interaction=0.006). There was a temporal increase in ICD use (adjusted OR 1.23, 95% CI 1.15–1.31 of ICD use per year) that was similar in each age group (p-value for interaction =0.665).
Conclusions
Eligible older HF patients age ≥ 65 years were significantly less likely to receive an ICD. With increasing age, women were less likely to receive an ICD than men. ICD use significantly increased over time in all age groups; however, age-related differences in ICD use persisted.
Keywords: defibrillator, implantable, heart failure, healthcare disparities, age, sex
Introduction
Sudden cardiac death is a major public health concern with an annual incidence of more than 300,000 deaths in the United States.1 Based on demonstrated efficacy in several randomized clinical trials,2–5 implantable cardioverter-defibrillator (ICD) use is a class I indication in practice guidelines for many patients with a reduced left ventricular ejection fraction.6–8 Prior studies have suggested that many potentially eligible patients do not receive an ICD.9–11 In hospitals participating in the American Heart Association’s (AHA) Get With The Guidelines- Heart Failure (GWTG-HF) program between January 2005 and June 2007, less than 40% of eligible patients received an ICD. Compared with white men, rates of ICD use were lower in black patients and women.9
Whereas race- and sex-based differences in ICD use have been described, little is known about the influence of age on ICD use among eligible patients.12, 13 In light of the increasing number of US individuals who are ≥ 65 years old, estimated to be 35 million in 2000 and 72 million in 2030,14 and the corresponding rise in the number of individuals eligible for ICD implantation, ICD use in older patients merits scrutiny. The goals of this analysis were (1) to determine whether ICD use among eligible HF patients differs among age groups, (2) to ascertain whether sex influences any age-related differences, and (3) to examine temporal trends of ICD use among age groups.
Methods
Data Source
The GWTG program is a national, voluntary, observational, hospital-based, and ongoing quality improvement initiative that began in the year 2000 under the auspices of the AHA. The GWTG program has been described previously.9, 10 With a point-of-care, interactive, internet-based Patient Management Tool to submit information on patients’ in-hospital care and outcomes, healthcare providers at participating hospitals are encouraged to apply the most current guidelines to patients admitted with HF, coronary artery disease, and stroke. Begun in January/March 2005 and continued to the present, the HF module originating from the Organized Program to Initiate Life-Saving Treatment in Hospitalized Patients with Heart Failure serves as the primary dataset for this analysis. Using case-ascertainment methods, trained personnel at participating institutions abstract data on consecutive eligible HF patients and submit them to the GWTG registry.
Prior to participating in this initiative, all participating institutions are required to comply with local regulatory and privacy guidelines and to obtain their institutional review board’s approval. Since these data are used primarily at the local level for quality improvement, waiver of informed consent was granted under the common rule. Outcomes Sciences (Cambridge, MA) serves as the data collection and coordination center for the GWTG program. The Duke Clinical Research Institute (Durham, NC) serves as the data analysis center and has an agreement to analyze the aggregate, de-identified data for research purposes.
Using standardized definitions, data include race/ethnicity, demographic and clinical characteristics, medical history and prior treatments, and in-hospital outcomes. Data collected in reference to ICDs include whether an ICD was implanted during the index hospitalization or was planned upon hospital discharge and any explanation documented by a physician regarding why an ICD was not implanted during the index hospitalization as well as contraindications to ICD use. Contraindications to ICD placement include an acute myocardial infarction in the 40 days prior to admission, new-onset HF, revascularization within 3 months, or life-expectancy with an acceptable functional status of less than 1 year. Data quality is monitored with computerized edit checks to ensure accuracy and completeness, and no significant changes have been detected over time. Further, patient identification and data collection processes did not change appreciably during the study period.
Study Population
We queried the GWTG-HF database to identify the records of patients with chronic heart failure and an LVEF ≤ 35% hospitalized between January 1, 2005, and October 31, 2011, and discharged alive. Records were excluded if discharge information was missing or in-hospital death occurred (n=9,348), HF was newly-diagnosed (n=12,636), or patients were discharged to a facility other than home (n=29,839). Records were also excluded if LVEF was missing (n=9,702) or was >35% (n=42,820) or a contraindication to ICD placement was documented (n=6,507). A total of 35,772 HF hospitalizations from 251 sites comprised our final study sample.
Outcome measures
The principal outcome measure was ICD use with or without cardiac resynchronization therapy among eligible patients without documented contraindications. The term “use” includes ICD placement prior to admission, ICD placement during the index hospitalization, and a documented plan to place an ICD upon discharge. We also examined whether sex has an impact on ICD use in relation to age and the temporal change in ICD use.
Statistical analysis
Using the chi-square test for categorical variables and Wilcoxon rank-sum test for continuous variables, we compared the baseline characteristics of patients who have an ICD with those who have no ICD. Summary statistics are reported as percentages for categorical variables and medians with 25th and 75th percentiles for continuous variables.
The primary age groups of interest were < 55, 55–64, 65–74, 75–84, and ≥ 85 years. We used the age group “<55 years” as the reference group for comparisons. Although patients aged ≥ 65 years were considered “older,” a group of patients aged 55–64 was included to better understand trends by age. We examined contraindications to ICD use overall and by age group. To construct a risk model for ICD use by age group, we used multivariable logistic regression with generalized estimating equations to account for hospital clustering of patients. Selection of covariates was based on clinical experience and prior GWTG analyses. Variables included in the model are detailed in Supplementary Table 1. Patients with missing data for age or hospital variables were excluded, while imputation was performed for the remaining covariates using the most frequent age-specific value for categorical variables and the age-specific median for continuous variables.
To determine whether the association of sex with ICD use varies by age, we assessed the significance of the multiplicative interaction of sex by age groups adjusting for the same variables enumerated above. In a sensitivity analysis, ICD use was analyzed according to age group stratified by sex. We determined the percentage of patients with an ICD over time for the overall population and by age groups. Temporal ICD use was further delineated according to whether it was present on admission, placed during the index hospitalization, or prescribed on discharge for the overall population and by age group. Formal testing for the presence of a trend across years was performed using the row means score. We further explored the change in ICD use over time overall and by age groups using both a main effects model as well as models with multiplicative age group by time interaction terms. In sensitivity analyses, we developed models stratified by age groups.
A P value <0.05 was considered statistically significant, and all tests were 2-sided. Analyses were performed using SAS software version 9.2 (SAS Institute, Cary, NC). The institutional review board of the Duke University Health System approved this study. The authors had full access to the data, take responsibility for its integrity, and have read and agree to the manuscript as written.
Results
Of 35,772 guideline-eligible patients, 17,639 received an ICD prior to hospitalization (10,886), during hospitalization (4,876), or were discharged with plans to undergo ICD placement after hospitalization (1,877).
Table 1 shows the baseline characteristics of the study population. The median age was 68 (interquartile range (IQR) 57–78) years and 35.4% were female. The majority of patients were white, had hypertension, and had coronary artery disease. In comparison to patients who received an ICD, patients who did not receive an ICD were older (70 (interquartile range (IQR) 57–80) years v. 67 (IQR 58–76) years) and more often female and non-white. They had a lower prevalence of atrial fibrillation, atrial flutter, COPD, hyperlipidemia, cerebrovascular disease, heart failure, and renal insufficiency. Further, the hospitals to which patients without an ICD were admitted were more likely to be small (with fewer beds), located in the West and South, and non-academic.
Table 1.
Baseline Patient Characteristics
| Characteristic | Total (n= 35,772) | ICD (n=17,639) | No ICD (n=18,133) | P Value |
|---|---|---|---|---|
| Age, y | 68 (57–78) | 67 (58–76) | 70 (57–80) | <0.001 |
| Men, % | 64.6 | 70.1 | 59.2 | <0.001 |
| Race, % | <0.001 | |||
| White | 60.4 | 63.0 | 57.9 | |
| Black | 24.9 | 24.5 | 25.2 | |
| Other | 14.7 | 12.5 | 16.9 | |
| Insurance, % | <0.001 | |||
| Medicare | 46.6 | 48.4 | 44.9 | |
| Medicaid | 10.4 | 10.1 | 10.8 | |
| Other | 28.5 | 28.2 | 28.8 | |
| None | 14.5 | 13.3 | 15.5 | |
| Systolic blood pressure, mm Hg | 131 (113–150) | 126 (110–144) | 136 (118–156) | <0.001 |
| Heart rate, bpm | 83 (71–98) | 80 (70–92) | 88 (75–103) | <0.001 |
| Body mass index, kg/m2† | 27.8 (23.9–3.0) | 28.1 (24.3–33.0) | 27.5 (23.5–32.9) | <0.001 |
| Medical History, % | ||||
| Anemia | 12.9 | 13.9 | 11.9 | <0.001 |
| Atrial flutter | 2.3 | 2.7 | 1.9 | <0.001 |
| Atrial fibrillation | 27.9 | 31.2 | 24.6 | <0.001 |
| Cerebrovascular disease | 11.4 | 15.2 | 7.5 | <0.001 |
| Chronic obstructive pulmonary disease | 26.9 | 28.0 | 25.8 | <0.001 |
| Coronary artery disease | 53.5 | 58.2 | 48.6 | <0.001 |
| Depression | 2.9 | 2.2 | 3.6 | <0.001 |
| Diabetes | 41.4 | 41.6 | 41.1 | 0.363 |
| Dialysis | 12.5 | 11.8 | 13.2 | <0.001 |
| Hyperlipidemia | 46.2 | 52.6 | 39.6 | <0.001 |
| Hypertension | 71.9 | 70.3 | 73.5 | <0.001 |
| Prior coronary artery bypass grafting | 7.4 | 7.7 | 7.1 | 0.017 |
| Prior myocardial infarction | 24.9 | 30.5 | 19.2 | <0.001 |
| Prior percutaneous intervention | 18.9 | 20.1 | 17.7 | <0.001 |
| Peripheral vascular disease | 11.0 | 11.6 | 10.4 | <0.001 |
| Renal insufficiency | 66.0 | 74.9 | 57 | <0.001 |
| Smoking | 22.3 | 21.3 | 23.3 | <0.001 |
| Valvular heart disease | 11.7 | 12.8 | 10.5 | <0.001 |
| Left ventricular ejection fraction, % | 25 (20–30) | 23 (18–30) | 25 (20–30) | <0.001 |
| Hospital characteristics | ||||
| No. beds in hospital, median (IQR) | 400 (305–587) | 420 (325–590) | 349 (243–575) | <0.001 |
| Geographic region, % | <0.001 | |||
| West | 14.2 | 11.6 | 16.9 | |
| South | 34.0 | 31.3 | 36.7 | |
| Midwest | 20.6 | 22.4 | 18.8 | |
| Northeast | 30.7 | 34.1 | 27.3 | |
| Location, % | <0.001 | |||
| Rural | 4.2 | 2.5 | 5.9 | |
| Urban | 95.8 | 97.5 | 94.1 | |
| Academic site | 59.6 | 65.3 | 54 | <0.001 |
Values are presented as % or median (interquartile range).
Among 6,507 patients with a documented reason that an ICD was not placed, 76.1% had a medical reason and 23.1% had a non-medical reason (Table 2). The minority of patients had a medical contraindication (11.5%), which included a myocardial infarction in the preceding 40 days, revascularization within 3 months, new-onset heart failure, or an expected survival of <1 year. Non-medical factors taken into consideration included economic (1.1%), social (1.5%), religious (0.1%), and anticipated non-compliance (9.5%). In comparison to patients < 55 years of age, a medical contraindication was more frequently cited and non-compliance was less commonly cited among older patients (p<0.0001).
Table 2.
Reasons ICD not placed or prescribed in eligible patients*
| Reasons | Overall (n=6,507) | < 55 (n=7153) | 55–64 (n=1,608) | 65–74 (n=1,327) | 75–84 (n=1,408) | ≥ 85 (n=836) | P value+ |
|---|---|---|---|---|---|---|---|
| Medical reason | 76.1 | 77.9 | 75.1 | 74.6 | 77.1 | 75.2 | 0.1851 |
| Medical contraindication* | 11.5 | 10.1 | 9.9 | 10.7 | 12.6 | 16 | <0.0001 |
| Other medical reason | 65.8 | 69.3 | 66.1 | 65.1 | 65.4 | 60.5 | <0.0001 |
| Nonmedical reason | 23.1 | 31.2 | 22.4 | 16.9 | 20.9 | 22.4 | <0.0001 |
| Economic | 1.1 | 1.9 | 1.3 | 0.6 | 0.6 | 0.7 | 0.1489 |
| Social | 1.5 | 2.1 | 1.8 | 0.8 | 0.9 | 1.7 | 0.333 |
| Religious | 0.1 | 0 | 0 | 0 | 0.2 | 0 | 0.015 |
| Non-compliance | 9.5 | 21.6 | 10.5 | 5.7 | 2.8 | 2.3 | <0.0001 |
| Other non-medical | 12.5 | 8.2 | 10.7 | 11 | 16.7 | 18.7 | <0.0001 |
| Reason unknown | 19.4 | 16.4 | 20.9 | 22.5 | 18 | 20 | 0.0003 |
Values are presented as %. Some patients reported more than one reason.
Includes myocardial infarction in preceding 40 days, revascularization within 3 months, new-onset heart failure, and expected survival < 1 year.
Reference group is age <55 years.
Table 3 shows ICD use among eligible HF patients according to age group in multivariable logistic regression models. In comparison to patients < 55 years of age, patients between 55 and 64 years were equally likely to receive an ICD. By contrast, patients in age groups 65–74, 75–85, and > 85 were less likely to receive an ICD. Further, a multiplicative interaction of age group by sex was detected (Table 4). Compared with men in the same age group, women were significantly less likely to receive an ICD, and this difference was more marked with increasing age (p-value for interaction = 0.0059). A sensitivity analysis of ICD use according to age group stratified by sex yielded similar results.
Table 3.
ICD use by age group
| Age, y | ICD, n | CRT-D, n | Overall ICD use (%) | Unadjusted | P value | Adjusted | P value |
|---|---|---|---|---|---|---|---|
| Overall* | 14,474 | 3,165 | 17,639/35,772 (49.3) | 0.97 (0.95, 0.98) | <0.0001 | 0.89 (0.87, 0.91) | <0.0001 |
| < 55 | 2,932 | 451 | 3,383/7,153 (47.3) | 1.00 (reference) | |||
| 55–64 | 3,309 | 694 | 4,003/7,360 (54.4) | 1.24 (1.16, 1.32) | <0.0001 | 0.96 (0.89, 1.04) | 0.3446 |
| 65–74 | 3,918 | 910 | 4,828/8,671 (55.7) | 1.32 (1.22, 1.43) | <0.0001 | 0.85 (0.76, 0.95) | 0.0029 |
| 75–84 | 3,489 | 905 | 4,394/8,890 (49.4) | 1.09 (1.00, 1.18) | 0.0492 | 0.63 (0.56, 0.72) | <0.0001 |
| ≥ 85 | 826 | 205 | 1,031/3,698 (27.9) | 0.50 (0.43, 0.58) | <0.0001 | 0.28 (0.24, 0.34) | <0.0001 |
Values are presented as odds ratios (95% confidence intervals) unless otherwise specified. Generalized estimating equations models are unadjusted or adjusted for patient characteristics and hospital factors. The reference group is age <55 years in both the overall analysis and those by age group.
Per 5-year increase in age.
Table 4.
ICD use by age group and sex, women versus men
| Age, y | ICD use among women (%) | ICD use among men (%) | Unadjusted | P value | Adjusted | P value |
|---|---|---|---|---|---|---|
| Overall* | 4,921/11,836 (41.6) | 12,366/23,104 (53.5) | 0.66 (0.61, 0.70) | <0.0001 | 0.74 (0.69, 0.79) | <0.0001 |
| < 55 | 960/2,123 (45.2) | 2,368/4,882 (48.5) | 0.82 (0.73, 0.93) | <0.0001 | 0.82 (0.73, 0.93) | 0.0059 |
| 55–64 | 1,112/2,234 (49.8) | 2,807/4,964 (56.6) | 0.79 (0.71, 0.88) | 0.85 (0.76, 0.95) | ||
| 65–74 | 1,319/2,734 (48.2) | 3,409/5,732 (59.5) | 0.70 (0.61, 0.81) | 0.78 (0.66, 0.92) | ||
| 75–84 | 1,236/3,138 (39.4) | 3,071/5,547 (55.4) | 0.58 (0.52, 0.66) | 0.66 (0.58, 0.74) | ||
| ≥ 85 | 294/1,607 (18.3) | 711/1,979 (35.9) | 0.41 (0.33, 0.52) | 0.51 (0.40, 0.64) |
Values are presented as odds ratios (95% confidence intervals). Generalized estimating equations models are unadjusted or adjusted for patient characteristics and hospital factors.
Per 5-year increase in age.
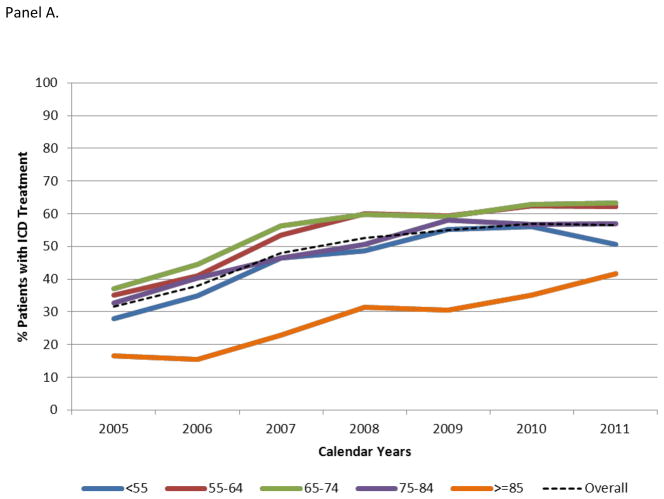
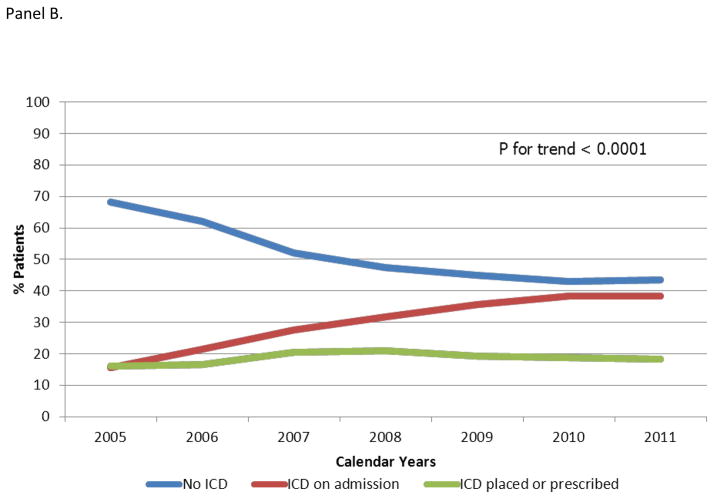
Figure 1, Panel A shows temporal changes in ICD use overall and each age group. Overall ICD use increased from 31.7% in 2005 to 56.6% in 2011. During the same time period, ICD use increased from 27.8% in 2005 to 50.5% in 2011 among patients age <55 years and from 16.6% to 41.7% among patients age > 85 years. Total ICD use increased over time (adjusted OR 1.23, 95% CI 1.15–1.31 of ICD use per year), and all age groups experienced a similar increase in ICD use (p-value for interaction = 0.67). Nonetheless, age differences persisted. Figure 1, Panel B shows the increase in ICD use in all age groups was driven mainly by a rise in the proportion of ICDs present on admission rather than new or planned ICDs (P for trend < 0.0001).
Figure 1. Temporal Trends in ICD Use.
All age groups experienced a similar increase in ICD use (p-value for interaction = 0.67). The increase in ICD use was driven mainly by a rise in the proportion of ICDs present on admission rather than the proportion placed during the index hospitalization or prescribed upon discharge.
Discussion
There are four principal findings from this study. First, after accounting for patient demographics, comorbid conditions, laboratory values, diagnostic studies, and hospital characteristics, guideline-eligible older HF patients were significantly less likely to receive an ICD. Second, the impact of age on ICD use varied by sex, with a larger impact in women. Third, there was a significant, clinically relevant temporal increase in ICD use among eligible patients in all age groups mainly driven by a rise in the proportion of ICDs present on admission. Finally, even in 2011, age-related differences in ICD use persisted.
In 2005, ICD use was a class I indication in the ACC/AHA heart failure guidelines for many patients with heart failure and reduced LVEF irrespective of age.6 In 2006 and 2008, guidelines emphasized that older age alone is not a contraindication to ICD use. Rather, implanting physicians should take into account the burden of comorbidities in addition to procedural risk and patient preferences.7, 8 Counter to this recommendation, guideline-eligible ICD non-recipients in our unadjusted analysis had a lower burden of comorbidities. After adjustment for patient comorbidities among other factors, older HF patients in our study sample were significantly less likely to receive an ICD in comparison to their younger counterparts. Lower ICD use among older patients may in part reflect skepticism regarding device efficacy and effectiveness.
Skepticism regarding device efficacy in older patients is not unfounded, as older patients were underrepresented in the major clinical trials. Patients in the Multicenter Automatic Defibrillator Implantation Trial II had a median age of 64 years,3 and patients in the Sudden Cardiac Death in Heart Failure Trial had a median age of 60 years.5 A total of 204 patients in the former trial and 236 patients in latter trial were ≥ 75 years of age.15 The results of these trials may not be generalizable to older individuals, who may have more advanced heart disease and more comorbid illnesses. These factors may explain why some stakeholders have expressed doubt about the benefit of an ICD in older patients.16 However, emerging observational data suggest clinical effectiveness is sustained in older patients.15, 16 In a prior analysis of the GWTG-HF database linked with Medicare claims, ICD recipients had an inverse probability-weighted adjust hazard ratio (HR) of mortality of 0.71 (95% CI 0.56–0.91) compared with non-recipients three years post-implantation. This effect was observed regardless of age (HR 0.65, 95% CI 0.47–0.89 among patients 65 to 74 years (n=188 ICD recipients); HR 0.80, 95% CI 0.62–1.03 among patients 75 to 84 years (n=188 ICD recipients); p=0.31 for interaction between ICD effectiveness and age).17 These results suggest the mortality benefit of ICDs may be maintained in patients up to 84 years of age.
Older patients may be disinclined to undergo surgical procedures such as ICD placement in view of their elevated risk of complications.18 In an analysis of primary prevention ICD recipients in the National Cardiovascular Data’s ICD registry, older patients had a higher risk of periprocedural complications and in-hospital mortality compared to patients aged <65 years: OR 1.14, 95% CI 1.03–1.25 among patients 65 to 74 years; OR 1.22, 95% CI 1.10–1.36 among patients 75 to 84 years; and OR 1.15, 95% CI 1.01–1.32 among patients ≥ 85 years.19 This modestly higher risk may be unacceptable to some patients.
Cost-effectiveness analyses of ICDs that used data from clinical trials have been inconclusive.20 Analyses based on observational data suggest that cost-effectiveness is preserved in older patients.21, 22 However, the lack of definitive data on ICD effectiveness and cost-effectiveness likely does not entirely account for lower ICD use among older patients. Older patients may place a higher premium on therapies that improve quality of life,23, 24 functional capacity, independence, and reduced hospitalizations rather than longevity and thus be more likely to decline ICD placement. Frailty, an increasingly recognized and highly prevalent geriatric syndrome related to but distinct from comorbidities and disabilities, may influence patient decisions and preferences.25 Components of frailty, including unintentional weight loss, exhaustion, weakness, slow gait, and low physical activity,26 may lead patients to defer ICD placement. Non-cardiac conditions including progressive cognitive decline and reduced vision and hearing, and social concerns such as placing undue burden on family members, may also play a role.27 Indeed, patients may view life-prolonging ICDs as burdensome in the setting of chronic debilitation and comorbid illnesses, and as such patients may prefer an arrhythmic death to alternative modes of death.28 Alternatively, patients who prioritize longevity may have limited access to care or economic means.
Physician- and healthcare system-related factors may also influence ICD use among older patients. Heterogeneity in physician training and familiarity with guideline recommendations regarding the role of age in ICD use may pose as barriers to guideline implementation. The wide array of practice settings and corresponding range of support for ICD decision-making, implantation, and follow-up may similarly limit consistent guideline application.
Our study is among the first to show the interplay between age- and sex- differences in ICD use.13 Age-related ICD use was lower in women compared with men. This finding is striking but perhaps not surprising, as not only older patients but also women were underrepresented in the major trials examining ICD efficacy. Previous studies suggest women may not derive as much benefit as men.2–5 The largest meta-analysis on this subject was hampered by a small sample size (n=934),29 a critical limitation in light of the reduced risk of sudden death in women compared to men. By contrast, in the aforementioned GWTG analysis on ICD effectiveness, ICD recipients had a reduced mortality rate regardless of sex (HR 0.58, 95% CI 0.41 to 0.83 among women (n=99 with ICD); HR 0.80, 95% CI 0.63–1.01 among men (n=277 with ICD); p-value for interaction between ICD effectiveness 3 years post-implantation and sex =0.15) 17. Further studies on the efficacy of ICDs in women as well as older patients may be required.
The rise in proportion of ICDs present on admission in comparison to those placed during the index hospitalization or prescribed upon discharge likely reflects the maturation and dissemination of ICD technology, increasing acceptance as a standard of care among patient subgroups by the medical community, and greater patient familiarity with ICDs. The longer lifespan it affords many patients may also contribute to its greater footprint on HF admission over time. The persistence of age-related differences in ICD use in 2011 underscores the importance of future studies to define ICD efficacy and potential reasons for low ICD use among older patients.
Limitations
Participation in the GWTG program is voluntary, and it likely attracts hospitals interested in quality improvement. Hence, the findings of our study may not be generalizable to other clinical practices. Further, the GWTG program only captures patients hospitalized for HF, and ICD placement in this setting is debatable. Class IV HF symptoms were not identified as a contraindication to ICD placement unless specifically documented as such in the medical record. We excluded patients with new-onset HF and included only those with chronic HF who qualified for an ICD prior to hospitalization. GWTG data are acquired by chart review and thus dependent on completeness and accuracy of both initial documentation and subsequent abstraction.30 Information in medical records may have suggested that patients were eligible for ICD treatment. However, decisions to place ICDs often require multiple, in-depth discussions that resulted in appropriate decision to withhold them. These discussions or documentation of current HF symptoms or contraindications or intolerances may not have been fully documented in patients’ medical records. Potential risk factors for sudden cardiac death outside of traditional indications for ICD placement such as a widened QRS complex or non-sustained ventricular tachycardia were not available for analysis. In the absence of QRS duration, eligibility for cardiac reynchronization therapy with ICD could not be determined. Patients discharged to a facility other than home were excluded were excluded from analysis since many are at high risk of 1-year mortality.31 This convention is in keeping with prior GWTG-HF analyses.10, 17 However, some may have been eligible for an ICD. Patient-related factors, such as access to care and a measure of frailty; physician-related factors, such as heterogeneity in training and familiarity with guidelines; and healthcare system related- factors, such as the broad array of practice settings with corresponding degrees of support for ICD use, were not fully captured. The units of analysis were individual hospitalizations rather than patients, and thus patients who were hospitalized frequently were proportionally represented in our findings. However, each hospitalization was a unique opportunity to either provide an ICD or not. Further, whether confined to individual hospitalizations or patients, prior GWTG analyses have yielded similar results.10 Age and sex distributions in our study likely do not mirror the overall United States population and therefore our study sample may not be generalizable. Whether patients with a planned ICD on discharge actually received one after the index hospitalization was not verified. Finally, residual measured and unmeasured confounders may exist and affect some or all of our results.
Conclusions
In the GWTG-HF program, older HF patients eligible for an ICD in the absence of documented contraindications were significantly less likely to receive an ICD. With increasing age, women were less likely to receive an ICD than men. Although there was an appreciable increase in ICD use over time across all age groups driven mainly by a rise in ICDs placed prior to admission, age-related differences persisted. Further study is required to define the efficacy of ICDs in older patients and identify the full complement of reasons for the age-related differences in guideline-directed use of ICDs.
Supplementary Material
Acknowledgments
Sources of Funding: Funding for the GWTG-HF program is provided by the American Heart Association. The GWTG-HF program is supported in part by MedTronic, Ortho-McNeil, and the American Heart Association Pharmaceuticals Roundtable. GWTG-HF was funded in the past by GlaxoSmithKline. This analysis was funded by the GWTG Young Investigator Database Research Seed Grant. The sponsors of GWTG-HF had no role in the design or conduct of the study or the management, analysis, or interpretation of the data. P.L.H. was funded by NIH T-32 training grant HL069749-09.
Footnotes
Author Contributions
Concept/design: Hess PL, Hernandez AF, Al-Khatib SM
Data analysis/interpretation: Hess PL, Grau-Sepulveda MV, Hernandez AF, Peterson ED, Bhatt DL, Schwamm LH, Yancy CW, Fonarow GC, Al-Khatib SM
Drafting of article: Hess PL, Al-Khatib SM
Critical revision of article: Hess PL, Grau-Sepulveda MV, Hernandez AF, Peterson ED, Bhatt DL, Schwamm LH, Yancy CW, Fonarow GC, Al-Khatib SM
Approval of article: Hess PL, Grau-Sepulveda MV, Hernandez AF, Peterson ED, Bhatt DL, Schwamm LH, Yancy CW, Fonarow GC, Al-Khatib SM
Statistics: Grau-Sepulveda MV
References
- 1.Myerburg RJ, Kessler KM, Castellanos A. Sudden cardiac death: Epidemiology, transient risk, and intervention assessment. Ann Intern Med. 1993;119:1187–1197. doi: 10.7326/0003-4819-119-12-199312150-00006. [DOI] [PubMed] [Google Scholar]
- 2.Buxton AE, Lee KL, Fisher JD, Josephson ME, Prystowsky EN, Hafley G. A randomized study of the prevention of sudden death in patients with coronary artery disease. Multicenter UnSustained Tachycardia Trial investigators. N Engl J Med. 1999;341:1882–1890. doi: 10.1056/NEJM199912163412503. [DOI] [PubMed] [Google Scholar]
- 3.Moss AJ, Zareba W, Hall WJ, Klein H, Wilber DJ, Cannom DS, Daubert JP, Higgins SL, Brown MW, Andrews ML. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002;346:877–883. doi: 10.1056/NEJMoa013474. [DOI] [PubMed] [Google Scholar]
- 4.Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP, Calkins H, Hoch D, Goldberger J, Shalaby A, Sanders WE, Schaechter A, Levine JH. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl J Med. 2004;350:2151–2158. doi: 10.1056/NEJMoa033088. [DOI] [PubMed] [Google Scholar]
- 5.Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH. Amiodarone or implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237. doi: 10.1056/NEJMoa043399. [DOI] [PubMed] [Google Scholar]
- 6.Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, Jessup M, Konstam MA, Mancini DM, Michl K, Oates JA, Rahko PS, Silver MA, Stevenson LW, Yancy CW. ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to update the 2001 guidelines for the evaluation and management of heart failure) J Am College Cardiol. 2005;46:e1–82. doi: 10.1016/j.jacc.2005.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Zipes DP, Camm AJ, Borggrefe M, Buxton AE, Chaitman B, Fromer M, Gregoratos G, Klein G, Moss AJ, Myerburg RJ, Priori SG, Quinones MA, Roden DM, Silka MJ, Tracy C, Smith SC, Jr, Jacobs AK, Adams CD, Antman EM, Anderson JL, Hunt SA, Halperin JL, Nishimura R, Ornato JP, Page RL, Riegel B, Blanc JJ, Budaj A, Dean V, Deckers JW, Despres C, Dickstein K, Lekakis J, McGregor K, Metra M, Morais J, Osterspey A, Tamargo JL, Zamorano JL. ACC/AHA/ESC 2006 guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A report of the American College of Cardiology/American Heart Association task force and the European Society of Cardiology committee for practice guidelines (writing committee to develop guidelines for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death) J Am Coll Cardiol. 2006;48:e247–346. doi: 10.1016/j.jacc.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 8.Epstein AE, DiMarco JP, Ellenbogen KA, Estes NA, 3rd, Freedman RA, Gettes LS, Gillinov AM, Gregoratos G, Hammill SC, Hayes DL, Hlatky MA, Newby LK, Page RL, Schoenfeld MH, Silka MJ, Stevenson LW, Sweeney MO, Smith SC, Jr, Jacobs AK, Adams CD, Anderson JL, Buller CE, Creager MA, Ettinger SM, Faxon DP, Halperin JL, Hiratzka LF, Hunt SA, Krumholz HM, Kushner FG, Lytle BW, Nishimura RA, Ornato JP, Riegel B, Tarkington LG, Yancy CW. ACC/AHA/HRS 2008 guidelines for device-based therapy of cardiac rhythm abnormalities: A report of the American College of Cardiology/American Heart Association task force on practice guidelines (writing committee to revise the ACC/AHA/NASPE 2002 guideline update for implantation of cardiac pacemakers and antiarrhythmia devices): Developed in collaboration with the American Association for Thoracic Surgery and Society of Thoracic Surgeons. Circulation. 2008;117:e350–408. doi: 10.1161/CIRCUALTIONAHA.108.189742. [DOI] [PubMed] [Google Scholar]
- 9.Hernandez AF, Fonarow GC, Liang L, Al-Khatib SM, Curtis LH, LaBresh KA, Yancy C, Albert NM, Peterson ED. Sex and racial differences in the use of implantable cardioverter-defibrillators among patients hospitalized with heart failure. JAMA. 2007;298:1525–1532. doi: 10.1001/jama.298.13.1525. [DOI] [PubMed] [Google Scholar]
- 10.Al-Khatib SM, Hellkamp AS, Hernandez AF, Fonarow GC, Thomas KL, Al-Khalidi HR, Heidenreich PA, Hammill BG, Yancy C, Peterson ED. Trends in use of implantable cardioverter defibrillator therapy among patients hospitalized for heart failure: Have the previously observed sex and racial disparities changed over time? Circulation. 2012:1094–1101. doi: 10.1161/CIRCULATIONAHA.111.066605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fonarow GC, Yancy CW, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Mehra MR, O’Connor CM, Reynolds D, Walsh MN. Heart failure care in the outpatient cardiology practice setting: Findings from IMPROVE HF. Circ Heart Fail. 2008;1:98–106. doi: 10.1161/CIRCHEARTFAILURE.108.772228. [DOI] [PubMed] [Google Scholar]
- 12.Forman DE, Cannon CP, Hernandez AF, Liang L, Yancy C, Fonarow GC. Influence of age on the management of heart failure: Findings from Get With The Guidelines-Heart Failure (GWTG-HF) Am Heart J. 2009;157:1010–1017. doi: 10.1016/j.ahj.2009.03.010. [DOI] [PubMed] [Google Scholar]
- 13.Yancy CW, Fonarow GC, Albert NM, Curtis AB, Stough WG, Gheorghiade M, Heywood JT, McBride ML, Mehra MR, O’Connor CM, Reynolds D, Walsh MN. Influence of patient age and sex on delivery of guideline-recommended heart failure care in the outpatient cardiology practice setting: Findings from IMPROVE HF. Am Heart J. 2009;157:754–762. e752. doi: 10.1016/j.ahj.2008.12.016. [DOI] [PubMed] [Google Scholar]
- 14.Federal Interagency Forum on Aging-Related Statistics. Older americans 2010: Key indicators of well-being. Federal Interagency Forum on Aging-Related Statistics; 2010. pp. 1–156. [Google Scholar]
- 15.Kong MH, Al-Khatib SM, Sanders GD, Hasselblad V, Peterson ED. Use of implantable cardioverter-defibrillators for primary prevention in older patients: A systematic literature review and meta-analysis. Cardiol J. 2011;18:503–514. doi: 10.5603/cj.2011.0005. [DOI] [PubMed] [Google Scholar]
- 16.Redberg RF. Disparities in use of implantable cardioverter-defibrillators: Moving beyond process measures to outcomes data. JAMA. 2007;298:1564–1566. doi: 10.1001/jama.298.13.1564. [DOI] [PubMed] [Google Scholar]
- 17.Hernandez AF, Fonarow GC, Hammill BG, Al-Khatib SM, Yancy CW, O’Connor CM, Schulman KA, Peterson ED, Curtis LH. Clinical effectiveness of implantable cardioverter-defibrillators among medicare beneficiaries with heart failure. Circ Heart Fail. 2010;3:7–13. doi: 10.1161/CIRCHEARTFAILURE.109.884395. [DOI] [PubMed] [Google Scholar]
- 18.Swindle JP, Rich MW, McCann P, Burroughs TE, Hauptman PJ. Implantable cardiac device procedures in older patients: Use and in-hospital outcomes. Arch Intern Med. 2010;170:631–637. doi: 10.1001/archinternmed.2010.30. [DOI] [PubMed] [Google Scholar]
- 19.Tsai V, Goldstein MK, Hsia HH, Wang Y, Curtis J, Heidenreich PA. Influence of age on perioperative complications among patients undergoing implantable cardioverter-defibrillators for primary prevention in the united states. Circ Cardiovasc Qual Outcomes. 2011;4:549–556. doi: 10.1161/CIRCOUTCOMES.110.959205. [DOI] [PubMed] [Google Scholar]
- 20.Sanders GD, Kong MH, Al-Khatib SM, Peterson ED. Cost-effectiveness of implantable cardioverter defibrillators in patients >or=65 years of age. Am Heart J. 2010;160:122–131. doi: 10.1016/j.ahj.2010.04.021. [DOI] [PubMed] [Google Scholar]
- 21.Chan PS, Nallamothu BK, Spertus JA, Masoudi FA, Bartone C, Kereiakes DJ, Chow T. Impact of age and medical comorbidity on the effectiveness of implantable cardioverter-defibrillators for primary prevention. Circ Cardiovasc Qual Outcomes. 2009;2:16–24. doi: 10.1161/CIRCOUTCOMES.108.807123. [DOI] [PubMed] [Google Scholar]
- 22.Groeneveld PW, Farmer SA, Suh JJ, Matta MA, Yang F. Outcomes and costs of implantable cardioverter-defibrillators for primary prevention of sudden cardiac death among the elderly. Heart Rhythm. 2008;5:646–653. doi: 10.1016/j.hrthm.2008.01.038. [DOI] [PubMed] [Google Scholar]
- 23.Huang DT, Sesselberg HW, McNitt S, Noyes K, Andrews ML, Hall WJ, Dick A, Daubert JP, Zareba W, Moss AJ. Improved survival associated with prophylactic implantable defibrillators in elderly patients with prior myocardial infarction and depressed ventricular function: A MADIT-II substudy. J Cardiovasc Electrophysiol. 2007;18:833–838. doi: 10.1111/j.1540-8167.2007.00857.x. [DOI] [PubMed] [Google Scholar]
- 24.Friedmann E, Thomas SA, Inguito P, Kao CW, Metcalf M, Kelley FJ, Gottlieb SS. Quality of life and psychological status of patients with implantable cardioverter defibrillators. J Interv Card Electrophysiol. 2006;17:65–72. doi: 10.1007/s10840-006-9053-1. [DOI] [PubMed] [Google Scholar]
- 25.Afilalo J, Karunananthan S, Eisenberg MJ, Alexander KP, Bergman H. Role of frailty in patients with cardiovascular disease. Am J Cardiol. 2009;103:1616–1621. doi: 10.1016/j.amjcard.2009.01.375. [DOI] [PubMed] [Google Scholar]
- 26.Fried LP, Tangen CM, Walston J, Newman AB, Hirsch C, Gottdiener J, Seeman T, Tracy R, Kop WJ, Burke G, McBurnie MA. Frailty in older adults: Evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 27.Forman DE, Rich MW, Alexander KP, Zieman S, Maurer MS, Najjar SS, Cleveland JC, Jr, Krumholz HM, Wenger NK. Cardiac care for older adults. Time for a new paradigm. J Am Coll Cardiol. 2011;57:1801–1810. doi: 10.1016/j.jacc.2011.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Goldstein NE, Lampert R, Bradley E, Lynn J, Krumholz HM. Management of implantable cardioverter defibrillators in end-of-life care. Ann Intern Med. 2004;141:835–838. doi: 10.7326/0003-4819-141-11-200412070-00006. [DOI] [PubMed] [Google Scholar]
- 29.Ghanbari H, Dalloul G, Hasan R, Daccarett M, Saba S, David S, Machado C. Effectiveness of implantable cardioverter-defibrillators for the primary prevention of sudden cardiac death in women with advanced heart failure: A meta-analysis of randomized controlled trials. Arch Intern Med. 2009;169:1500–1506. doi: 10.1001/archinternmed.2009.255. [DOI] [PubMed] [Google Scholar]
- 30.LaPointe NM, Al-Khatib SM, Piccini JP, Atwater BD, Honeycutt E, Thomas K, Shah BR, Zimmer LO, Sanders G, Peterson ED. Extent of and reasons for nonuse of implantable cardioverter defibrillator devices in clinical practice among eligible patients with left ventricular systolic dysfunction. Circ Cardiovasc Qual Outcomes. 2011;4:146–151. doi: 10.1161/CIRCOUTCOMES.110.958603. [DOI] [PubMed] [Google Scholar]
- 31.Allen LA, Hernandez AF, Peterson ED, Curtis LH, Dai D, Masoudi FA, Bhatt DL, Heidenreich PA, Fonarow GC. Discharge to a skilled nursing facility and subsequent clinical outcomes among older patients hospitalized for heart failure. Circ Heart Fail. 2011;4:293–300. doi: 10.1161/CIRCHEARTFAILURE.110.959171. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.