Abstract
Purpose
The purpose of this study is to describe: 1) the receipt of diabetes self-management education (DSME) in a large, diverse cohort of US youth with type 1 diabetes (T1DM); 2) the segregation of self-reported DSME variables into domains; and 3) the demographic and clinical characteristics of youth who receive DSME.
Methods
Data are from the US population-based cohort, SEARCH for Diabetes in Youth. A cross-sectional analysis was employed using data from 1273 youth < 20 years of age at time of diagnosis of T1DM. Clusters of 19 self-reported DSME variables were derived using factor analysis and their associations with demographic and clinical characteristics were evaluated using polytomous logistic regression.
Results
Nearly all participants reported receiving DSME content consistent with ‘survival skills’ (e.g., target blood glucose and what to do for low or high blood glucose), yet gaps in continuing education were identified [e.g., fewer than half of participants reported receiving specific medical nutrition therapy (MNT) recommendations]. Five DSME clusters were explored: Receipt of Specific MNT Recommendations, Receipt of Diabetes Information Resources, Receipt of Clinic Visit Information, Receipt of Specific Diabetes Information, and Met with Educator or Nutritionist. Factor scores were significantly associated with demographic and clinical characteristics, including race/ethnicity, socioeconomic status, and diabetes self-management practices.
Conclusions
Health care providers should work together to address reported gaps in DSME in order to improve patient care.
The Diabetes Control and Complications Trial provided unequivocal scientific evidence that intensive glycemic control achieved by matching food intake, physical activity, and insulin to the self-monitoring of blood glucose (SMBG) improves micro- and macrovascular outcomes among individuals with type 1 diabetes (T1DM).1 Achieving this level of self-management requires frequent, rigorous diabetes education and support.2-4 Patients must be provided with knowledge and skills, empowering them to successfully take control of their diabetes. The American Diabetes Association (ADA) and the International Society for Pediatric and Adolescent Diabetes recommend ongoing, tailored diabetes self-management education (DSME) provided by a multidisciplinary healthcare team.5,6
Most studies evaluating adherence to ADA guidelines among individuals with diabetes in the US have focused on the ABC of diabetes7,8: hemoglobin A1c (A1C), blood pressure, and cholesterol.9 To date, no epidemiological study has systematically evaluated the content and processes of diabetes education received as part of routine care among youth with T1DM in the US. Furthermore, the characteristics of youth who report receiving recommendations or information relating to diabetes from their health care providers are unknown. The identification of demographic and clinical variables associated with receipt of DSME is important for classifying populations based on need and adapting service delivery to more precisely meet the needs of youth with T1DM. With the rising cost of healthcare in the US and persistent disparities in healthcare utilization,10 it is essential that gaps in care are realized in order to maximize medical resource consumption and improve patient outcomes.
SEARCH for Diabetes in Youth is an ongoing, population-based study of diabetes in youth across five centers in the US: South Carolina, Ohio, Colorado, California, and Washington. This large, diverse sample provides a unique opportunity to explore the content and processes of diabetes education received as part of routine pediatric and adolescent care. The objectives of this study were to describe: 1) the receipt of DSME in a large, diverse cohort of US youth with T1DM; 2) the segregation of self-reported DSME variables into domains; and 3) the demographic and clinical characteristics of youth who receive DSME.
Methods
Sample
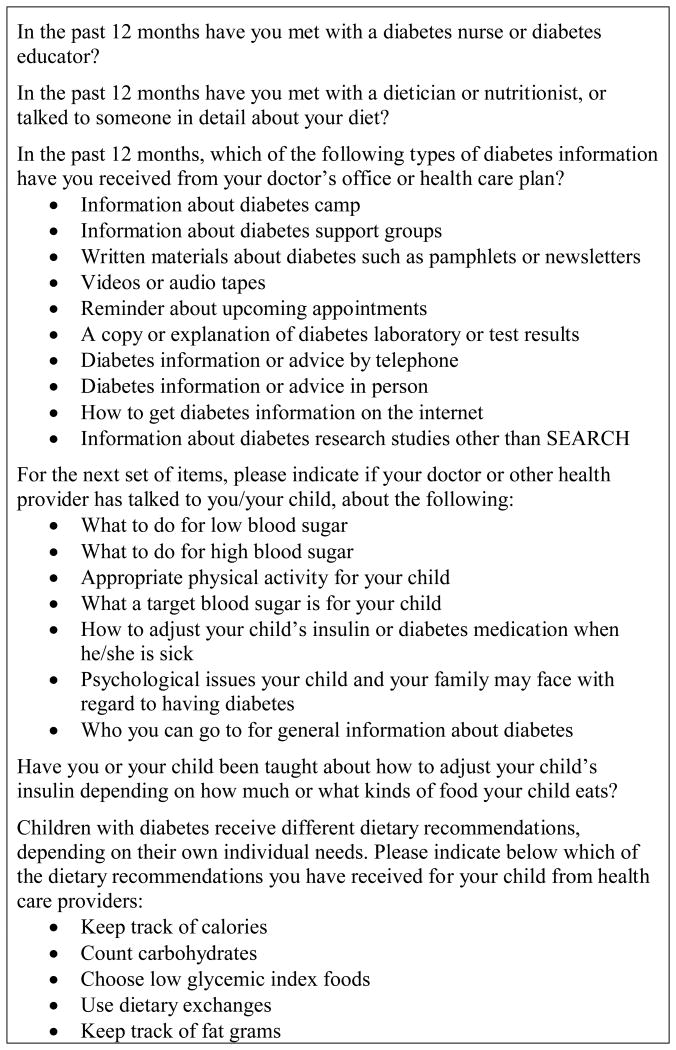
Data are from SEARCH for Diabetes in Youth. Study details are published elsewhere.11 Briefly, incident cases of physician-diagnosed diabetes in youth < 20 years of age were identified beginning in 2002 with estimated case ascertainment > 90%.12,13 Participants were asked to complete an initial survey and after completion were invited for an initial study visit. Participants in the 2002-2005 incident cohorts who participated in this visit were also invited to follow-up visits at approximately 12, 24, and 60 months. Questionnaires querying DSME content and process variables (Figure 1) were added to the study protocol part-way into the implementation of the 24-month follow-up visits and were completed by the participant if ≥ 18 years of age or by the parent/guardian, commonly with assistance from the youth, if < 18 years of age. The present analysis used cross-sectional data collected from participants with T1DM during the most recent of these visits (e.g., 24 or 60 months) for which both A1C and complete questionnaires relevant to DSME were obtained (n = 1275).
Figure 1.
Twenty-five questions relating to diabetes self-management education content and process queried in follow-up visits of SEARCH for Diabetes in Youth participants.
Measures
Staff were trained and certified in standardized procedures prior to initiating data collection and re-certified annually. Study protocols were approved by Institutional Review Boards at all participating sites.
Questionnaires administered at the follow-up visits queried 25 DSME content and process variables (Figure 1). Demographic covariates, based on self-report, included: age, gender, race/ethnicity defined according to the 2000 US Census categories,14 parent migration status, parent educational attainment, family structure, estimated total annual household income, and health insurance coverage. Self-reported clinical covariates included: diabetes duration, frequency of SMBG, proportion of diabetes care done by participant, and insulin regimen.
Body mass index (BMI) was calculated as measured weight (kg) divided by height (m) squared, and obesity was defined as a BMI ≥ 95th age- and sex-specific percentile for participants ≤ 20 years of age and BMI ≥ 30 kg/m2 for participants > 20 years of age. A1C was measured in whole blood using automated high-performance liquid chromatography (Tosoh Bioscience, Montgomeryville, Pennsylvania). Glycemic control was specified as “good” according to the ADA age-specific target values: < 6 years, A1C < 8.5%; 6-12 years, A1C < 8.0%; 13-18 years, A1C < 7.5%; ≥ 19 years, A1C < 7.0%.15 Participants of all ages with an A1C ≥ 9.5% were classified as having “poor” glycemic control15 and participants with an A1C between the “good” and “poor” limits were classified as having “intermediate” glycemic control.
Analysis
Participant characteristics were analyzed using standard univariate statistical procedures. Due to the large number of DSME content and process variables collected in SEARCH and the fact that many of these variables are correlated, a variable reduction technique was employed to derive a smaller number of independent latent variables—clusters of DSME content and process variables called “factors”—that could account for the majority of variance in the observed variables. Factors with eigenvalues > 1, indicating that the factor is accounting for a greater amount of variance than any single variable, and that explained > 5% of total variance were further evaluated using a scree plot.16 Given these criteria, five factors were retained in the final analysis. Orthogonally rotated factor loadings [e.g., the correlations (range -1.0 to 1.0) between the factors and the independent variables] greater than ± 0.40 were interpreted. Factors were named according to the variables with high factor loadings and names are italicized throughout the text. Scores for each factor were computed for participants as the linear composite of all optimally-weighted observed input variables.
The association of demographic and clinical characteristics—the independent variables, including both categorical and interval specifications—with DSME factor scores—the dependent variables, specified as quartiles with quartile 1 as the referent—was evaluated using polytomous logistic regression (a.k.a., multiple logistic regression). The measures of association were therefore odds ratios with corresponding 95% confidence intervals. All analyses were conducted using SAS 9.2 (SAS Institute, Cary, North Carolina). Values are presented as mean ± SD or %. Statistical significance was considered for P < 0.05.
Results
Participants with A1C > 17.0% (n = 2) were excluded because the circumstances surrounding this extreme level of poor control are likely different from those surrounding “typical” poor control (final results consistent with inclusion; data not shown). The final sample size was 1273.
Participants were 14.6 ± 4.5 years of age (range: 3.5 to 26.1), had a T1DM duration of 63.1 ± 17.0 months (range: 23 to 103), and among participants ≥ 10 years of age, 41.6% reported being responsible for all of their own diabetes care. Approximately half of participants were on insulin pumps and 72.8% reported a frequency of SMBG ≥ 4 times per day, yet only 27.1% were classified as having good glycemic control (Table 1).
Table 1.
Demographic and clinical characteristics of youth with type 1 diabetes from the 2002-2005 SEARCH for Diabetes in Youth incident cohorts (n = 1273).
| Demographic Characteristics | % (n) | |
|---|---|---|
| Age at Follow-up Visit | ||
| < 10 years | 18.1 (230) | |
| ≥ 10 years | 81.9 (1043) | |
| Male | 51.9 (660) | |
| Race/Ethnicity | ||
| Non-Hispanic white | 77.2 (983) | |
| Hispanic | 10.1 (129) | |
| Asian/Pacific Islander | 1.8 (23) | |
| Non-Hispanic black | 10.1 (128) | |
| Native American | 0.4 (5) | |
| Other | 0.4 (5) | |
| ≥ 1 Foreign-born Parent1 | 13.1 (143) | |
| Parent Educational Attainment | ||
| ≤ High School | 16.1 (202) | |
| Some college or a degree beyond high school | 83.9 (1056) | |
| Family Structure | ||
| Two-parent household | 73.1 (922) | |
| Single-parent household | 24.4 (308) | |
| Other household | 2.5 (32) | |
| Estimated Total Annual Household Income | ||
| < $24 999 | 11.2 (142) | |
| $25 000-$49 999 | 16.1 (204) | |
| $50 000-$74 999 | 17.4 (220) | |
| ≥ $75,000 | 44.0 (556) | |
| Don't know/Refuse to answer | 11.2 (142) | |
| Health Insurance Coverage at Follow-up Visit | ||
| None | 2.6 (33) | |
| Medicaid/Medicare | 17.3 (219) | |
| Other | 1.7 (22) | |
| Private | 78.4 (995) | |
|
| ||
| Clinical Characteristics | ||
| Frequency of SMBG | ||
| < 1 time per day | 2.7 (34) | |
| 1-2 times per day | 9.5 (120) | |
| 3 times per day | 15.0 (190) | |
| ≥ 4 times per day | 72.8 (920) | |
| Proportion of Diabetes Care Done by Participant | ||
| < 25% | 11.1 (141) | |
| 25-75% | 27.1 (345) | |
| >75% | 61.8 (785) | |
| Insulin Regimen | ||
| Pump | 49.3 (612) | |
| Long + short/rapid ≥ 3 per day | 33.9 (421) | |
| Other | 16.8 (209) | |
| Glycemic Control2 | ||
| Good | 27.1 (345) | |
| Intermediate | 45.8 (583) | |
| Poor | 27.1 (345) | |
| Obese3 | 11.8 (148) | |
Missing for n = 178.
Good: < 6 years, A1C < 8.5%; 6-12 years, A1C < 8.0%; 13-18 years, A1C < 7.5%; ≥ 19 years, A1C < 7.0%. Poor: all ages, A1C ≥ 9.5%. Intermediate: A1C between good and poor.
BMI ≥ 95th age- and sex-specific percentile for participants ≤ 20 years of age and BMI ≥ 30 kg/m2 for participants > 20 years of age.
The proportion of participants reporting DSME content and process variables are presented in Table 2. Although nearly all participants reported knowing their target blood glucose, 15.4% of parents/guardians reported not knowing the preferred A1C for their child. Of those who did report a value, the mean ± SD was 6.9 ± 1.2% (range: 0.2 to 15). Due to their inability to discriminate between participants, DSME variables for which the proportion responding “yes” was > 90% were excluded from the factor analysis. Six of the 25 DSME content and processes variables met this criterion. The remaining 19 variables were included in the factor analysis.
Table 2.
Affirmative responses to queries about diabetes self-management education (DSME) assessed in youth with type 1 diabetes from the 2002-2005 SEARCH for Diabetes in Youth incident cohorts (n = 1273).
| Component of DSME | % yes (n) |
|---|---|
| Met in past 12 months with: | |
| Diabetes educator or nurse | 76.0 (968) |
| Dietician or nutritionist | 53.3 (679) |
|
| |
| Types of information received from doctor's office or health care plan in past 12 months: | |
| Diabetes camp | 53.0 (675) |
| Diabetes support groups | 39.0 (497) |
| Written materials about diabetes | 63.2 (805) |
| Videos or audio tapes | 5.7 (72) |
| Appointment reminder | 90.0 (1146) |
| Copy/explanation of laboratory results | 72.4 (921) |
| Diabetes information by telephone | 47.1 (599) |
| Diabetes information in person | 89.4 (1138) |
| How to get diabetes information on Internet | 40.2 (512) |
| Diabetes research studies other than SEARCH | 29.9 (381) |
|
| |
| Doctor or other health provider has talked with parent/guardian or participant about: | |
| What to do for high blood glucose | 96.9 (1233)1 |
| What to do for low blood glucose | 96.4 (1227)1 |
| What target blood glucose is | 97.3 (1236)1 |
| How to adjust insulin when sick | 92.2 (1174)1 |
| How to adjust insulin based on amount/type of food | 93.1 (1176)1 |
| Who to go to for information about diabetes | 76.7 (976) |
| Appropriate physical activity | 87.8 (1118) |
| Psychological issues in regard to having diabetes | 58.4 (743) |
|
| |
| Nutrition recommendations ever received: | |
| Calorie tracking | 21.7 (276) |
| Carbohydrate counting | 97.5 (1239)1 |
| Dietary exchanges | 31.2 (397) |
| Track fat grams | 25.1 (319) |
| Low glycemic foods | 33.9 (431) |
Queries with proportion of participants responding “yes” > 90% were excluded from the factor analysis.
Factor retention criteria resulted in the retention of five factors (Table 3). Receiving recommendations relating to dietary exchanges, fat gram tracking, calorie tracking, and low glycemic index foods loaded heavily on the first factor, which was named Receipt of Specific Medical Nutrition Therapy (MNT) Recommendations. Receiving information about diabetes support groups, diabetes camps, how to find information relating to diabetes on the Internet, and written information about diabetes loaded heavily on the second factor: Receipt of Diabetes Information Resources. Receiving information in-person or via telephone, a copy/explanation of laboratory results, and an appointment reminder loaded heavily on the third factor: Receipt of Clinic Visit Information. Receiving information about appropriate physical activity and psychological issues in regard to diabetes, and who to go to for general diabetes information loaded heavily on the fourth factor: Receipt of Specific Diabetes Information. Finally, meeting with a dietician or nutritionist and meeting with a diabetes educator or nurse in the past 12 months loaded heavily on the fifth factor: Met with Educator or Nutritionist.
Table 3.
Summary of variables with rotated factor loadings > 0.40 for the five retained factors.
| Factor | Variable | Factor Loading |
|---|---|---|
| (1) Receipt of Specific MNT Recommendations | Fat gram tracking recommendation | 0.74 |
| Calorie tracking recommendation | 0.74 | |
| Dietary exchanges recommendation | 0.73 | |
| Low glycemic index recommendation | 0.66 | |
|
| ||
| (2) Receipt of Diabetes Information Resources | Received info about diabetes support groups | 0.72 |
| Received info about diabetes camps | 0.61 | |
| Received written info about diabetes | 0.57 | |
| Received info on how to find diabetes info on Internet | 0.53 | |
|
| ||
| (3) Receipt of Clinic Visit Information | Received info in-person | 0.71 |
| Received a copy/explanation of laboratory results | 0.65 | |
| Received appointment reminder | 0.65 | |
| Received info via telephone | 0.43 | |
|
| ||
| (4) Receipt of Specific Diabetes Information | Received info about who to go to for info about diabetes | 0.75 |
| Received info about psychological issues with regards to diabetes | 0.73 | |
| Received info about appropriate physical activity | 0.70 | |
|
| ||
| (5) Met with Educator or Nutritionist | Met with dietician or nutritionist in past 12 months | 0.82 |
| Met with diabetes educator or nurse in past 12 months | 0.78 | |
Participants in the highest quartile (relative to lowest quartile) for Receipt of Specific MNT Recommendations were more likely to report being of a minority race/ethnicity, having ≥ 1 foreign-born parent, living in a single-parent household, and having an estimated total annual household income < $50 000 (Table 4). They were also older, less likely to report doing 25-75% of their own diabetes care (relative to > 75%), more likely to be on an insulin regimen other than a pump, more likely to have poor glycemic control, and more likely to be obese.
Table 4.
Demographic and clinical correlates of factor scores derived from diabetes self-management education input variables among youth with type 1 diabetes from the 2002-2005 SEARCH for Diabetes in Youth incident cohorts (n = 1273).1
| Receipt of Specific MNT Recommendations | Receipt of Diabetes Information Resources | Receipt of Clinic Visit Information | Receipt of Specific Diabetes Information | Met with Educator or Nutritionist | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|
|||||||||||
| Factor Score Quartile | 2 | 3 | 4 | 2 | 3 | 4 | 2 | 3 | 4 | 2 | 3 | 4 | 2 | 3 | 4 |
| Minority race/ethnicity | 1.26 | 2.33* | 4.59* | 0.89 | 1.03 | 0.73 | 0.93 | 0.80 | 0.55* | 0.72 | 1.29 | 0.63* | 0.72 | 1.12 | 1.33 |
| 0.80, 1.98 | 1.53, 3.55 | 3.07, 6.88 | 0.62, 1.29 | 0.72, 1.48 | 0.50, 1.07 | 0.65, 1.33 | 0.56, 1.15 | 0.38, 0.81 | 0.49, 1.04 | 0.91, 1.83 | 0.43, 0.93 | 0.48, 1.06 | 0.77, 1.61 | 0.93, 1.91 | |
| ≥ 1 Foreign-born parent | 2.24* | 2.69* | 4.52* | 0.80 | 1.01 | 1.17 | 1.16 | 0.88 | 0.82 | 0.57* | 1.36 | 0.55* | 0.57* | 0.96 | 1.01 |
| 1.19, 4.22 | 1.43, 5.03 | 2.49, 8.19 | 0.48, 1.34 | 0.62, 1.65 | 0.72, 1.90 | 0.72, 1.88 | 0.54, 1.46 | 0.50, 1.35 | 0.34, 0.96 | 0.87, 2.14 | 0.32, 0.94 | 0.33, 0.97 | 0.60, 1.55 | 0.63, 1.62 | |
| Male | 1.05 | 1.21 | 1.16 | 0.83 | 1.05 | 0.92 | 0.93 | 1.01 | 1.05 | 0.92 | 1.15 | 1.11 | 1.00 | 1.25 | 1.18 |
| 0.77, 1.43 | 0.89, 1.65 | 0.85, 1.59 | 0.61, 1.13 | 0.77, 1.43 | 0.68, 1.26 | 0.68, 1.27 | 0.74, 1.38 | 0.77, 1.43 | 0.68, 1.26 | 0.84, 1.57 | 0.81, 1.51 | 0.73, 1.37 | 0.91, 1.70 | 0.86, 1.61 | |
| Age ≥ 10 years | 1.07 | 1.66* | 1.80* | 0.93 | 0.92 | 0.73 | 0.74 | 1.11 | 0.55* | 1.14 | 1.09 | 1.29 | 0.58* | 0.59* | 0.46* |
| 0.73, 1.56 | 1.10, 2.49 | 1.19, 2.73 | 0.61, 1.41 | 0.61, 1.38 | 0.49, 1.09 | 0.49, 1.13 | 0.71, 1.72 | 0.37, 0.83 | 0.76, 1.69 | 0.73, 1.61 | 0.86, 1.94 | 0.37, 0.90 | 0.38, 0.92 | 0.30, 0.70 | |
| Parent some college or a degree beyond high school | 1.09 | 0.94 | 0.78 | 0.96 | 1.04 | 1.49 | 1.43 | 1.70* | 1.70* | 0.99 | 0.95 | 1.05 | 1.54 | 1.23 | 1.08 |
| 0.70, 1.69 | 0.61, 1.44 | 0.51, 1.19 | 0.64, 1.45 | 0.69, 1.58 | 0.96, 2.33 | 0.95, 2.14 | 1.11, 2.59 | 1.11, 2.59 | 0.65, 1.51 | 0.63, 1.46 | 0.68, 1.62 | 1.00, 2.39 | 0.81, 1.87 | 0.72, 1.62 | |
| Family Structure | |||||||||||||||
| Two-parent household | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Single-parent household | 1.12 | 1.64* | 1.54* | 0.98 | 0.62* | 0.69* | 0.68* | 1.03 | 0.65* | 0.84 | 1.28 | 1.25 | 0.82 | 0.75 | 1.00 |
| 0.76, 1.65 | 1.13, 2.37 | 1.06, 2.24 | 0.69, 1.39 | 0.43, 0.91 | 0.48, 1.00 | 0.47, 0.99 | 0.73, 1.46 | 0.45, 0.94 | 0.57, 1.23 | 0.89, 1.83 | 0.87, 1.80 | 0.57, 1.18 | 0.52, 1.09 | 0.71, 1.43 | |
| Other household | 0.60 | 0.56 | 1.22 | 1.01 | 0.78 | 0.60 | 0.61 | 0.66 | 1.10 | 1.58 | 0.65 | 0.79 | 0.61 | 0.76 | 0.46 |
| 0.22, 1.68 | 0.19, 1.66 | 0.51, 2.93 | 0.39, 2.58 | 0.30, 2.07 | 0.21, 1.70 | 0.21, 1.74 | 0.23, 1.90 | 0.45, 2.71 | 0.64, 3.88 | 0.21, 2.03 | 0.27, 2.30 | 0.23, 1.60 | 0.31, 1.87 | 0.16, 1.34 | |
| Estimated Total Annual Household Income | |||||||||||||||
| < $24 999 | 1.51 | 1.64 | 2.55* | 0.67 | 0.70 | 0.66 | 0.71 | 0.66 | 0.39* | 0.65 | 0.79 | 0.59* | 0.52* | 1.17 | 1.83* |
| 0.86, 2.68 | 0.95, 2.86 | 1.50, 4.33 | 0.40, 1.12 | 0.43, 1.17 | 0.39, 1.12 | 0.42, 1.17 | 0.40, 1.11 | 0.23, 0.68 | 0.38, 1.09 | 0.48, 1.31 | 0.35, 0.98 | 0.28, 0.96 | 0.69, 1.98 | 1.11, 3.02 | |
| $25 000-$49 999 | 1.73* | 1.24 | 1.66* | 0.79 | 0.86 | 1.12 | 0.54* | 0.44* | 0.43* | 1.17 | 1.06 | 0.83 | 1.16 | 1.35 | 1.16 |
| 1.10, 2.72 | 0.78, 1.99 | 1.05, 2.63 | 0.49, 1.27 | 0.54, 1.37 | 0.71, 1.76 | 0.34, 0.84 | 0.28, 0.70 | 0.28, 0.70 | 0.75, 1.84 | 0.66, 1.67 | 0.52, 1.33 | 0.74, 1.84 | 0.86, 2.14 | 0.71, 1.88 | |
| $50 000-$74 999 | 1.21 | 0.96 | 1.07 | 0.76 | 0.59* | 0.98 | 0.83 | 0.79 | 0.52* | 1.01 | 1.05 | 0.84 | 1.01 | 1.09 | 1.47 |
| 0.79, 1.85 | 0.62, 1.48 | 0.69, 1.66 | 0.49, 1.18 | 0.37, 0.94 | 0.64, 1.51 | 0.53, 1.30 | 0.51, 1.23 | 0.33, 0.82 | 0.65, 1.57 | 0.67, 1.63 | 0.54, 1.30 | 0.64, 1.58 | 0.69, 1.72 | 0.94, 2.30 | |
| ≥ $75 000 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Don't know/Refuse to answer | 2.61* | 2.84* | 3.31* | 0.66 | 0.49* | 0.41* | 0.51* | 0.57* | 0.32* | 1.03 | 1.13 | 0.73 | 0.44* | 0.51* | 0.68 |
| 1.42, 4.79 | 1.57, 5.14 | 1.82, 6.00 | 0.41, 1.07 | 0.30, 0.82 | 0.24, 0.72 | 0.30, 0.85 | 0.34, 0.93 | 0.19, 0.55 | 0.61, 1.73 | 0.68, 1.90 | 0.43, 1.25 | 0.26, 0.74 | 0.31, 0.85 | 0.41, 1.11 | |
| Proportion Diabetes Care by Participant | |||||||||||||||
| < 25% | 0.68 | 0.56* | 0.60* | 1.11 | 1.11 | 1.39 | 0.87 | 0.73 | 1.05 | 0.84 | 0.70 | 0.85 | 2.14* | 1.85* | 2.88* |
| 0.42, 1.11 | 0.34, 0.94 | 0.37, 0.97 | 0.67, 1.84 | 0.66, 1.87 | 0.84, 2.31 | 0.53, 1.45 | 0.44, 1.20 | 0.65, 1.72 | 0.51, 1.37 | 0.42, 1.17 | 0.52, 1.39 | 1.21, 3.78 | 1.04, 3.28 | 1.66, 4.99 | |
| 25-75% | 0.85 | 0.88 | 0.50* | 0.90 | 1.42 | 1.71* | 1.42 | 0.86 | 1.40 | 1.02 | 1.08 | 0.95 | 1.56* | 1.23 | 1.60* |
| 0.60, 1.20 | 0.62, 1.25 | 0.35, 0.73 | 0.61, 1.31 | 0.99, 2.04 | 1.19, 2.44 | 0.99, 2.03 | 0.59, 1.26 | 0.98, 2.00 | 0.71, 1.45 | 0.76, 1.54 | 0.66, 1.36 | 1.08, 2.23 | 0.85, 1.78 | 1.11, 2.30 | |
| > 75% | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Insulin Regimen | |||||||||||||||
| Pump | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Long + short/rapid ≥ 3 per day | 1.65* | 1.41 | 2.69* | 0.72 | 0.50* | 0.48* | 0.66* | 0.76 | 0.50* | 0.86 | 0.74 | 0.70* | 0.92 | 1.14 | 1.32 |
| 1.16, 2.35 | 0.99, 2.03 | 1.87, 3.88 | 0.51, 1.02 | 0.35, 0.72 | 0.33, 0.68 | 0.46, 0.95 | 0.53, 1.08 | 0.34, 0.71 | 0.61, 1.20 | 0.52, 1.05 | 0.50, 1.00 | 0.64, 1.31 | 0.80, 1.63 | 0.92, 1.88 | |
| Other | 1.22 | 2.13* | 4.04* | 0.58* | 0.51* | 0.52* | 0.46* | 0.42* | 0.36* | 0.88 | 1.82* | 1.23 | 0.76 | 0.93 | 1.14 |
| 0.73, 2.03 | 1.34, 3.40 | 2.54, 6.44 | 0.37, 0.90 | 0.33, 0.80 | 0.34, 0.80 | 0.30, 0.70 | 0.27, 0.65 | 0.23, 0.56 | 0.54, 1.44 | 1.17, 2.84 | 0.78, 1.96 | 0.49, 1.19 | 0.60, 1.45 | 0.74, 1.76 | |
| Not on insulin | 1.02 | 0.53 | 3.94* | 0.70 | 0.70 | 0.69 | 0.20* | 0.08* | 0.21* | 0.93 | 1.15 | 1.18 | 0.33* | 0.36 | 0.55 |
| 0.34, 3.09 | 0.13, 2.06 | 1.56, 9.96 | 0.25, 1.98 | 0.25, 1.91 | 0.25, 1.88 | 0.07, 0.55 | 0.02, 0.36 | 0.08, 0.55 | 0.32, 2.70 | 0.41, 3.26 | 0.43, 3.25 | 0.11, 0.92 | 0.13, 1.02 | 0.22, 1.40 | |
| Frequency of SMBG | |||||||||||||||
| < 1 time per day | 4.03* | 3.35 | 3.83* | 0.64 | 0.36 | 0.46 | 0.40* | 0.13* | 0.13* | 0.56 | 0.34* | 0.41 | 0.25* | 0.25* | 0.24* |
| 1.12, 14.45 | 0.90, 12.54 | 1.04, 14.10 | 0.27, 1.53 | 0.13, 1.02 | 0.18, 1.18 | 0.18, 0.89 | 0.04, 0.46 | 0.04, 0.44 | 0.24, 1.31 | 0.12, 0.95 | 0.16, 1.09 | 0.09, 0.68 | 0.09, 0.67 | 0.09, 0.66 | |
| 1-2 times per day | 1.67 | 1.36 | 1.55 | 0.85 | 0.77 | 0.59 | 0.53* | 0.78 | 0.41* | 0.60 | 0.71 | 0.85 | 0.78 | 0.64 | 0.61 |
| 0.96, 2.88 | 0.76, 2.44 | 0.88, 2.74 | 0.51, 1.42 | 0.46, 1.31 | 0.34, 1.02 | 0.31, 0.91 | 0.48, 1.28 | 0.23, 0.73 | 0.35, 1.04 | 0.42, 1.21 | 0.51, 1.42 | 0.47, 1.29 | 0.38, 1.09 | 0.36, 1.04 | |
| 3 times per day | 0.57* | 1.44 | 1.48 | 0.71 | 0.90 | 0.57* | 0.64* | 0.65 | 0.69 | 0.65 | 1.10 | 1.08 | 1.29 | 1.32 | 1.27 |
| 0.34, 0.95 | 0.94, 2.20 | 0.96, 2.26 | 0.46, 1.10 | 0.59, 1.36 | 0.36, 0.89 | 0.41, 0.99 | 0.42, 1.01 | 0.45, 1.06 | 0.40, 1.04 | 0.72, 1.70 | 0.70, 1.67 | 0.81, 2.05 | 0.83, 2.08 | 0.80, 2.02 | |
| ≥ 4 times per day | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Glycemic Control2 | |||||||||||||||
| Poor | 1.56 | 1.61* | 2.65* | 1.05 | 0.81 | 0.65 | 0.43* | 0.45* | 0.34* | 0.94 | 1.16 | 1.19 | 0.86 | 1.54 | 1.18 |
| 0.97, 2.52 | 1.02, 2.54 | 1.62, 4.31 | 0.68, 1.63 | 0.52, 1.27 | 0.40, 1.06 | 0.28, 0.67 | 0.29, 0.71 | 0.22, 0.54 | 0.61, 1.45 | 0.73, 1.86 | 0.75, 1.88 | 0.55, 1.34 | 0.98, 2.42 | 0.75, 1.84 | |
| Intermediate | 1.06 | 0.79 | 1.18 | 1.08 | 0.95 | 0.84 | 0.71 | 0.80 | 0.71 | 0.95 | 1.25 | 1.19 | 0.95 | 1.08 | 1.19 |
| 0.72, 1.56 | 0.54, 1.16 | 0.77, 1.79 | 0.73, 1.59 | 0.64, 1.42 | 0.55, 1.29 | 0.47, 1.06 | 0.53, 1.20 | 0.47, 1.07 | 0.65, 1.40 | 0.82, 1.90 | 0.80, 1.79 | 0.65, 1.40 | 0.73, 1.62 | 0.80, 1.78 | |
| Good | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 | 1.00 |
| Obese3 | 0.75 | 1.41 | 2.02* | 1.29 | 1.41 | 1.20 | 0.96 | 0.96 | 0.93 | 1.20 | 1.32 | 0.78 | 1.19 | 1.48 | 1.37 |
| 0.42, 1.32 | 0.85, 2.33 | 1.25, 3.25 | 0.79, 2.13 | 0.86, 2.31 | 0.72, 2.00 | 0.59, 1.55 | 0.59, 1.56 | 0.58, 1.52 | 0.74, 1.94 | 0.82, 2.12 | 0.46, 1.32 | 0.71, 1.99 | 0.90, 2.43 | 0.83, 2.26 | |
Values represent odds ratios and 95% confidence intervals for polytomous logistic regression models predicting factor scores categorized as quartiles (referent: quartile 1).
Good: < 6 years, A1C < 8.5%; 6-12 years, A1C < 8.0%; 13-18 years, A1C < 7.5%; ≥ 19 years, A1C < 7.0%. Poor: all ages, A1C ≥ 9.5%. Intermediate: A1C between good and poor.
BMI ≥ 95th age- and sex-specific percentile for participants ≤ 20 years of age and BMI ≥ 30 kg/m2 for participants > 20 years of age.
P < 0.05.
Participants in the highest quartile (relative to lowest quartile) for Receipt of Diabetes Information Resources were less likely to report living in a single-parent household and being on an insulin regimen other than a pump, and more likely to report doing 25-75% of their own diabetes care (relative to > 75%) (Table 4).
Participants in the highest quartile (relative to lowest quartile) for Receipt of Clinic Visit Information were less likely to report being of a minority race/ethnicity, living in a single-parent household, and having an estimated total annual household income < $50 000, and more likely to report having a parent with some college or a degree beyond high school (Table 4). They were also younger, less likely to be on an insulin regimen other than a pump, less likely to report a SMBG frequency of < 3 times per day, and less likely to have poor glycemic control.
Participants in the highest quartile (relative to lowest quartile) for Receipt of Specific Diabetes Information were less likely to report being of a minority race/ethnicity or having ≥ 1 foreign-born parent (Table 4).
Finally, participants in the highest quartile (relative to lowest quartile) for Met with Educator or Nutritionist were younger and more likely to report doing 25-75% of their own diabetes care (relative to > 75%) (Table 4).
Discussion
In this diverse, population-based sample of youth with T1DM in the US, receipt of DSME content consistent with primary diabetes education [e.g., ‘survival skills’ and initial education occurring at and shortly after diagnosis6] is prevalent. Five clusters of DSME variables were identified: Receipt of Specific Medical Nutrition Therapy (MNT) Recommendations, Receipt of Diabetes Information Resources, Receipt of Clinic Visit Information, Receipt of Specific Diabetes Information, and Met with Educator or Nutritionist; and significant associations between these factors and demographic and clinical characteristics were observed.
As one might expect in a cohort with a mean diabetes duration of 5 years, a vast majority of participants reported receiving recommendations relating to diabetes ‘survival skills’6: blood glucose targets, basic nutrition advice (e.g., carbohydrate counting), an explanation of what to do for hyper- and hypoglycemia, and how to handle diabetes during illness. However, there were some aspects of primary diabetes education reported at low frequencies, including psychological issues in regard to diabetes and diabetes support services. Given the high prevalence of depressed mood and fears of hypoglycemia among youth with diabetes,17-20 these observed low frequencies represent an important gap in care.
Many aspects of secondary diabetes education [e.g., continuing diabetes education curriculum contributing to an in-depth understanding of self-management6] were reported at alarmingly low rates. For example, only half of participants reported meeting with a dietician or nutritionist in the past 12 months. Finally, only half of participants reported receiving information about diabetes camps, which may represent a missed opportunity for teaching diabetes self-management skills.21
Among participants ≥ 10 years of age, 42% reported doing all of their own diabetes care; among the entire sample, 62% reported doing more than 75% of their own diabetes care. Sustaining intensive diabetes self-management throughout childhood/adolescence relies on the involvement of parents/guardians.22,23 These observations, coupled with the high rate of youth not meeting glycemic goals, may suggest that responsibility for diabetes tasks is being assumed by youth too quickly without adequate reinforcement of DSME aimed at the child/adolescent with an emphasis on parent/guardian partnership. Youth often cannot apply knowledge consistently without adult partnership and supervision. Because SEARCH did not specifically query who the DSME was aimed towards, this analysis could not definitively answer whether the education was aimed at the child/adolescent. However, youth in this sample are doing the majority of their own diabetes care, and frequent repetition and family involvement are important for maintenance of skills in this age group.
To date, studies have focused on diabetes knowledge among youth with T1DM,24,25 but few have identified the routine sources of that knowledge or DSME processes.26 In this study, most participants reported receiving information about diabetes during a clinical visit, but fewer than half received counsel on how to find reliable diabetes information on the Internet. Additionally, the use of technologies for delivering diabetes information was not widely reported: only 6% of participants received videos or audiotapes while 47% received information via phone. The latter estimate could be biased because respondents may not have included or recalled brief telephone encounters, such as communications with nurse educators about blood glucose adjustments. The use of technology (e.g., mobile phones, text messaging, and social networking websites) as a tool for delivering education and improving motivation may be attractive to youth and has shown promise in interventions.27-31 The observations reported here may indicate an important gap in empowering patients to improve self-management practices. However, telephone case management, including text messaging, is not currently reimbursed and is time consuming for health care providers; these barriers may limit their use in routine care. Finally, the development of monitored social networking websites targeted at youth and publically available is a necessary step before health care professionals will be able to recommend these tools in the course of routine care.
Consistent differences in age and proportion of diabetes care done by the participant across factor quartiles were observed. Younger participants, reporting doing less of their own diabetes care, scored higher on Receipt of Clinic Visit Information and Met with Diabetes Educator or Nutritionist, while older participants, reporting being responsible for most of their own diabetes care, were more likely to score high on the Receipt of Specific MNT Recommendations. The increased odds of being on a pump among participants in the highest versus lowest quartile for Receipt of Diabetes Information Resources and Receipt of Clinic Visit Information may reflect the requirement for higher levels of education with the use of new management methods, such as insulin pumps.
Participants scoring high on Receipt of Specific MNT Recommendations had several distinct characteristics: they were more likely to be second-generation immigrants reporting a minority race/ethnicity and more likely to have lower socioeconomic status (e.g. live in a single-parent household and have a lower estimated total annual household income). These participants were also more likely to have poor glycemic control and be classified as obese. Together, these observations may indicate that health care providers are attempting to address known difficulties in adherence in these high-risk populations.
A limitation of this analysis is that because DSME variables were self-reported, participant perception and knowledge of professional credentials may have resulted in misreporting of meeting with various practitioners, including diabetes educators, nurses, nutritionists, and dieticians. Countering this, social desirability bias may have resulted in over-reporting of meetings: participants may think they should have these meetings and report attendance in the absence of an actual visit.
Conclusions
This is the first study to describe the receipt of DSME in a large, population-based sample of youth with T1DM in the US. The analysis focused on secondary diabetes education, e.g., continuing diabetes education following the initial ‘survival education’ provided at the time of diagnosis and soon thereafter, and was therefore able to identify gaps in self-reported continuation of diabetes-related education. Particularly, few participants reported receiving information relating to psychological issues in regard to diabetes, diabetes support services, and diabetes camps, which are important aspects of continuing education that may improve patient self-management and quality of life. Health care providers, including diabetes educators, should work to address these gaps in DSME content, perhaps through the use of new technologies. Future research should prospectively evaluate DSME received as part of routine care and clinical outcomes, to build upon the experimental evidence base supporting continuing diabetes education for youth with T1DM.
Acknowledgments
The SEARCH for Diabetes in Youth Study is indebted to the many youth and their families, and their health care providers, whose participation made this study possible.
Funding: SEARCH for Diabetes in Youth is funded by the Centers for Disease Control and Prevention (PA numbers 00097, DP-05-069, and DP-10-001) and supported by the National Institute of Diabetes and Digestive and Kidney Diseases. Site Contract Numbers: Kaiser Permanente Southern California (U48/CCU919219, U01 DP000246, and U18DP002714), University of Colorado Denver (U48/CCU819241-3, U01 DP000247, and U18DP000247-06A1), Children's Hospital Medical Center (Cincinnati) (U48/CCU519239, U01 DP000248, and 1U18DP002709), University of North Carolina at Chapel Hill (U48/CCU419249, U01 DP000254, and U18DP002708-01), University of Washington School of Medicine (U58/CCU019235-4, U01 DP000244, and U18DP002710-01), Wake Forest University School of Medicine (U48/CCU919219, U01 DP000250, and 200-2010-35171). The authors wish to acknowledge the involvement of General Clinical Research Centers (GCRC) at the South Carolina Clinical & Translational Research (SCTR) Institute, at the Medical University of South Carolina (NIH/NCRR Grant number UL1RR029882); Children's Hospital and Regional Medical Center (Grant Number M01RR00037); Colorado Pediatric General Clinical Research Center (Grant Number M01RR00069) and the Barbara Davis Center at the University of Colorado at Denver (DERC NIH P30DK57516); and the Institutional Clinical and Translational Science Award (CTSA), NIH/NCRR at the University of Cincinnati (Grant Number UL1RR026314-01).
The contents of this paper are solely the responsibility of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention and the National Institute of Diabetes and Digestive and Kidney Diseases.
The writing group for this manuscript wishes to acknowledge the contributions of the following individuals to the SEARCH for Diabetes in Youth Study: California: Jean M. Lawrence, ScD, MPH, MSSA, Kristi Reynolds, PhD, MPH, Jin-Wen Hsu, PhD, Mary Helen Black, PhD, Kim Holmquist, BA, and Harpreet S. Takhar, MPH, for the Department of Research & Evaluation and Ann K. Kershnar, MD for the Department of Pediatrics, Kaiser Permanente Southern California; and David J. Pettitt, MD, for the Sansum Diabetes Research Institute. Colorado: Dana Dabelea, MD, PhD, Richard F. Hamman, MD, DrPH, Lisa Testaverde, MS, for the Department of Epidemiology, Colorado School of Public Health, University of Colorado Denver, Georgeanna J. Klingensmith, MD, Marian J. Rewers, MD, PhD, David Maahs, MD and Paul Wadwa, MD for the Barbara Davis Center for Childhood Diabetes, Stephen Daniels, MD, PhD, Kristen Nadeau, MD, Department of Pediatrics and Children's Hospital, Clifford A. Bloch, MD, for the Pediatric Endocrine Associates, Carmelita Sorrelman, MSPH, Alfreda Beartrack, MSPH for the Navajo Area Indian Health Prevention Program. Hawaii: Beatriz L. Rodriguez, MD, PhD, Wilfred Fujimoto, MD, J. David Curb, MD (deceased), Fiona Kennedy, RN, Greg Uramoto, MD, Sorrell Waxman, MD, , and Richard Chung, MD, for Kuakini Medical Center; Beth Waitzfelder, PhD, for the Center for Health Research, Kaiser Permanente Hawaii; and Teresa Hillier, MD for the Center for Health Research, Kaiser Permanente Northwest and Hawaii. Ohio: Lawrence M. Dolan, MD, Michael Seid, PhD, Elaine Urbina, MD, MS, Debra A. Standiford, MSN, CNP for the Cincinnati Children's Hospital Medical Center. Carolina: Elizabeth J. Mayer-Davis, PhD, Joan Thomas MS, RD for the University of North Carolina, Chapel Hill, Anwar Merchant, ScD, Angela D. Liese, PhD, MPH, , Robert R. Moran, PhD, Gladys Gaillard-McBride, RN, CFNP, Deborah Lawler, MT (ASCP), Malaka Jackson, MD for the University of South Carolina, Deborah Bowlby, MD, for the Medical University of South Carolina, James Amrhein, MD, for Greenville Hospital Systems, Pam Clark, MD for McLeod Pediatric Subspecialists, Mark Parker, MD for Pediatric Endocrinology & Diabetes Specialists, Charlotte, NC. Washington: Catherine Pihoker, MD, Maryam Afkarian, MD, Angela Badaru, MD, Lisa Gilliam, MD, PhD, Irl Hirsch, MD, Lenna L. Liu, MD, MPH, John Neff, MD, and Joyce Yi-Frazier, PhD for the University of Washington, Beth Loots, MPH, MSW, Rebecca O'Connor, RN, Sue Kearns, RN, Mary Klingsheim, RN, Emil Buscaino, BS, Katherine Cochrane, BS, Onel Martinez, MS, and Sharla Semana, BS, for Seattle Children's Hospital, and Carla Greenbaum, MD for Benaroya Research Institute. Centers for Disease Control and Prevention: Giuseppina Imperatore, MD, PhD, Desmond E. Williams, MD, PhD, Henry S. Kahn, MD, Bernice Moore, MBA, Gregg W. Edward, PhD, Sharon H. Saydah, PhD. National Institute of Diabetes and Digestive and Kidney Diseases, NIH: Barbara Linder, MD, PhD. Central Laboratory: Santica M. Marcovina, PhD, ScD, Vinod P. Gaur, PhD, and Jessica Harting for the University of Washington Northwest Lipid Research Laboratories. Coordinating Center: Ronny Bell, PhD, MS, Ralph D'Agostino, Jr., PhD, Bettina Beech, DrPH, Douglas Case, PhD, Jasmin Divers, PhD, Timothy Morgan, PhD, Michelle Naughton, PhD, Leora Henkin, MPH, MEd, Susan Moxley, BS, Gena Hargis, MPH, Donna Kronner, Maureen T. Goldstein, BA, Andrea Anderson, MS, Jeanette Andrews, MS, Abigail Lauer, MS, Jennifer Talton, MS for Wake Forest School of Medicine.
References
- 1.Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med. 1993;329(14):977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 2.American Diabetes Association. Implications of the Diabetes Control and Complications Trial. Diabetes Care. 2003;26(Suppl 1):S25–27. doi: 10.2337/diacare.26.2007.s25. [DOI] [PubMed] [Google Scholar]
- 3.Clement S. Diabetes self-management education. Diabetes Care. 1995;18(8):1204–1214. doi: 10.2337/diacare.18.8.1204. [DOI] [PubMed] [Google Scholar]
- 4.Funnell MM, Brown TL, Childs BP, et al. National standards for diabetes self-management education. Diabetes Care. 2008;31(Suppl 1):S97–104. doi: 10.2337/dc10-S097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.American Diabetes Association. Position statement: Standards of medical care in diabetes. Diabetes Care. 2010;33(Suppl 1):S11–61. doi: 10.2337/dc10-S011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Swift PPGF. Diabetes education in children and adolescents. Pediatric diabetes. 2009;10:51–57. doi: 10.1111/j.1399-5448.2009.00570.x. [DOI] [PubMed] [Google Scholar]
- 7.Waitzfelder B. Adherence to guidelines for youth with diabetes mellitus. Pediatrics. 2011;128(3):531–538. doi: 10.1542/peds.2010-3641. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Resnick HE, Foster GL, Bardsley J, Ratner RE. Achievement of American Diabetes Association clinical practice recommendations among US adults with diabetes, 1999–2002. Diabetes Care. 2006;29(3):531–537. doi: 10.2337/diacare.29.03.06.dc05-1254. [DOI] [PubMed] [Google Scholar]
- 9.Watkins PPJ. ABC of diabetes: Cardiovascular disease, hypertension, and lipids. BMJ. 2003;326(7394):874–876. doi: 10.1136/bmj.326.7394.874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harris MMI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care. 2001;24(3):454–459. doi: 10.2337/diacare.24.3.454. [DOI] [PubMed] [Google Scholar]
- 11.SEARCH Study Group. SEARCH for diabetes in youth: A multicenter study of the prevalence, incidence and classification of diabetes mellitus in youth. Control Clin Trials. 2004;25(5):458–471. doi: 10.1016/j.cct.2004.08.002. [DOI] [PubMed] [Google Scholar]
- 12.SEARCH for Diabetes in Youth Study Group. Liese AD, D'Agostino RB, et al. The burden of diabetes mellitus among US youth: Prevalence estimates from the SEARCH for Diabetes in Youth Study. Pediatrics. 2006;118(4):1510–1518. doi: 10.1542/peds.2006-0690. [DOI] [PubMed] [Google Scholar]
- 13.SEARCH for Diabetes in Youth Study Group. Incidence of diabetes in youth in the US. JAMA. 2007;297(24):2716–2724. doi: 10.1001/jama.297.24.2716. [DOI] [PubMed] [Google Scholar]
- 14.US Department of Census, Bureau of the Census. United States Census 2000. OMB 0607-0856
- 15.Silverstein J, Klingensmith G, Copeland K, et al. Care of children and adolescents with type 1 diabetes: A statement of the American Diabetes Association. Diabetes Care. 2005;28(1):186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- 16.Kaiser HF. The application of electronic computers to factor analysis. Educ Psychol Meas. 1960;20:141–151. [Google Scholar]
- 17.Lawrence JM, Standiford DA, Loots B, et al. Prevalence and correlates of depressed mood among youth with diabetes: The SEARCH for Diabetes in Youth Study. Pediatrics. 2006;117(4):1348–1358. doi: 10.1542/peds.2005-1398. [DOI] [PubMed] [Google Scholar]
- 18.Kanner S, Hamrin V, Grey M. Depression in adolescents with diabetes. J Child Adolesc Psychiatr Nurs. 2003;16(1):15–24. doi: 10.1111/j.1744-6171.2003.tb00342.x. [DOI] [PubMed] [Google Scholar]
- 19.Type 1 diabetes: Rates of depression in mothers and children are high. Am J Nurs. 2008;108(10):22. doi: 10.1097/01.NAJ.0000337730.46236.d7. [DOI] [PubMed] [Google Scholar]
- 20.Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: Implications for diabetes management and patient education. Patient Educ Couns. 2007;68(1):10–15. doi: 10.1016/j.pec.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 21.American Diabetes Association. Diabetes management at camps for children with diabetes. Diabetes Care. 2012;35(Suppl 1):S72–75. doi: 10.2337/dc12-s072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smaldone AA. Educating your patient with diabetes. Totowa, NJ: Humana Press; 2009. Pediatric diabetes education: A family affair; pp. 251–271. [Google Scholar]
- 23.La Greca AM. It's “all in the family”: Responsibility for diabetes care. J Pediatr Endocrinol Metab. 1998;11(Suppl 2):379–385. [PubMed] [Google Scholar]
- 24.Olsen Roper S, Call A, Leishman J, et al. Type 1 diabetes: Children and adolescents' knowledge and questions. J Adv Nurs. 2009;65(8):1705–1714. doi: 10.1111/j.1365-2648.2009.05033.x. [DOI] [PubMed] [Google Scholar]
- 25.O'Neil KKJ. Quality of life and diabetes knowledge of young persons with type 1 diabetes: Influence of treatment modalities and demographics. J Am Diet Assoc. 2005;105(1):85–91. doi: 10.1016/j.jada.2004.10.010. [DOI] [PubMed] [Google Scholar]
- 26.Rankin D, Heller S, Lawton J. Understanding information and education gaps among people with type 1 diabetes: A qualitative investigation. Patient Educ Couns. 2011;83(1):87–91. doi: 10.1016/j.pec.2010.04.026. [DOI] [PubMed] [Google Scholar]
- 27.Howells L, Wilson AC, Skinner TC, Newton R, Morris AD, Greene SA. A randomized control trial of the effect of negotiated telephone support on glycaemic control in young people with type 1 diabetes. Diabet Med. 2002;19(8):643–648. doi: 10.1046/j.1464-5491.2002.00791.x. [DOI] [PubMed] [Google Scholar]
- 28.Howe CJ, Jawad AF, Tuttle AK, et al. Education and telephone case management for children with type 1 diabetes: A randomized controlled trial. J Pediatr Nurs. 2005;20(2):83–95. doi: 10.1016/j.pedn.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 29.Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med. 2006;23(12):1332–1338. doi: 10.1111/j.1464-5491.2006.01989.x. [DOI] [PubMed] [Google Scholar]
- 30.Pinsker JE, Nguyen C, Young S, Fredericks GJ, Chan D. A pilot project for improving paediatric diabetes outcomes using a website: The pediatric diabetes education portal. J Telemed Telecare. 2011;17(5):226–230. doi: 10.1258/jtt.2010.100812. [DOI] [PubMed] [Google Scholar]
- 31.Ellis DA, Naar-King S, Frey M, Templin T, Rowland M, Cakan N. Multisystemic treatment of poorly controlled type 1 diabetes: Effects on medical resource utilization. Journal of Pediatric Psychology. 2005;30(8):656–666. doi: 10.1093/jpepsy/jsi052. [DOI] [PubMed] [Google Scholar]