Abstract
Background
There have been mixed findings on the temporal relation between anxiety disorders and alcohol use disorders (AUDs), suggesting that the pathway to AUDs may differ among individuals. The aim of the current study was to test whether parental support moderated the association between anxiety disorders and the development of AUDs. We also tested whether our effects differed as a function of age of AUD onset.
Methods
817 individuals were assessed for lifetime diagnoses of psychopathology during 4-waves between adolescence (mean age = 16) and adulthood (mean age = 30).
Results
Proportional hazards model analyses indicated that baseline anxiety disorders interacted with baseline perceived maternal support to prospectively predict onset of AUDs. At high levels of maternal support, anxiety disorders were associated with a reduced risk for AUD onset (HR=0.74, 95% CI = 0.55–1.00). However, this effect was more robust for AUDs that developed prior to age 20. At low levels of maternal support, anxiety disorders were associated with an increased risk for AUD onset (HR=1.65, 95% CI = 1.21–2.26). This effect was present for AUDs that developed across adolescence and adulthood. Paternal support was not associated with AUDs and did not interact with anxiety disorders.
Conclusions
Prevention and intervention efforts targeted at maternal support in adolescents with anxiety disorders may be valuable, as this may represent a factor that has a significant impact on the developmental course of AUDs.
Keywords: anxiety disorders, alcohol use disorders, maternal support
1. INTRODUCTION
Lifetime diagnoses of alcohol abuse and dependence are common (Hasin et al., 2007) and associated with serious adverse consequences (Rehm et al., 2009; Mokdad et al., 2004; Wilcox et al., 2004). Numerous risk factors for alcohol use disorders (AUDs) have been identified (Sher et al., 2005; Tucker et al., 2008; Patterson et al., 2000). However, the identification of at-risk populations continues to be a major public health issue and there is a critical need to examine interactions among risk factors to improve prevention and intervention approaches.
There are multiple developmental pathways to AUD onset. One of the most robust trajectories is via externalizing personality traits and disorders (see Zucker, 2006, 2008 for reviews). Broadly, evidence indicates that externalizing disorders, such as attention-deficit-hyperactivity disorder (ADHD) and conduct disorder (CD; Charach et al., 2011; Nock et al., 2006), as well as externalizing traits, such as impulsivity and sensation seeking (Verdejo-García et al., 2008), are associated with AUD onset. It has been theorized that externalizing traits/symptoms emerge early in development and are associated with an inability or unwillingness to inhibit behaviors despite negative consequences (Iacono et al., 2008). These traits, coupled with a high-risk environment, are thought to ultimately propel individuals along the externalizing pathway to AUD onset (Zucker et al., 2006).
Notably, research indicates that not all individuals develop AUDs via the externalizing pathway and that there may be a separate internalizing pathway (see Hussong et al., 2011). Studies have shown that internalizing personality traits and disorders, including anxiety, depression and neuroticism, also lead to the onset of AUDs (Dixit and Crum, 2000; Kushner et al., 2012; Littlefield et al., 2010). Although the mechanisms underlying the internalizing pathway are not fully understood, evidence suggests that individuals with high levels of negative affect engage in alcohol use to alleviate their aversive affective states (Bolton et al., 2009). The use of alcohol as a means of avoidance-based coping becomes negatively reinforced over time, increasing the likelihood and maintenance of AUDs (Crum et al., 2013; Baker et al., 2004).
To date, the literature on the role of anxiety disorders in the development of AUDs has been mixed, calling into question the etiological validity of the internalizing pathway. Several studies have demonstrated that anxiety disorders increase the risk for AUD onset (Behrendt et al., 2011; Buckner et al., 2008), whereas others have reported weak effects (Crum and Pratt, 2001). Some studies have also found the opposite relation – anxiety disorders and symptoms are associated with a reduced risk for AUDs (Eggleston et al., 2004; Kaplow et al., 2001). Considering these disparate findings, it is likely that key factors influence the direction and strength of the anxiety to AUD pathway. More specifically, it is possible that anxiety disorders can act as either risk or protective factors, as a function of different traits or features (i.e., moderators). It is necessary to consider that individuals with anxiety disorders are often behaviorally inhibited (Clauss and Blackford, 2012) and consequently may fail to affiliate with peers (Booth-LaForce et al., 2012). Since drinking often occurs in social settings (particularly in young adulthood), it is possible that some individuals with anxiety disorders are avoidant of social situations and novel stimuli (i.e., alcohol) which decreases their likelihood of developing AUDs (see Kagan, 2007).
One important developmental variable which may influence the association between anxiety disorders and AUDs is parental support. Parental support has been defined in several ways but typically encompasses parental displays of companionship, intimacy, affection, and instrumental aid. Research indicates that adolescents with low levels of parental support have reduced self-esteem and poor social skills which make them vulnerable to peer pressure, deviant behavior, and alcohol use (Parker and Benson, 2004). High levels of parental support have the opposite effect and have been shown to buffer adolescents from risk factors and enhance the impact of protective factors (Stadler et al., 2010; Wills and Cleary, 1996). Given that the influence of parental factors may be greater among those with high levels of negative affect (Wills et al., 2001), it is possible that the relationship between anxiety disorders and AUDs differs as a function of parental support. In other words, at low levels of parental support, individuals with anxiety disorders may be at risk for AUDs due to reduced self-esteem and vulnerability to affiliate with deviant peers. In contrast, at high levels of parental support, individuals with anxiety disorders may spend more time with parents (and less with peers) and thus, be protected from alcohol use initiation and AUD onset.
Another important factor which may contribute to previous mixed findings is the role of developmental period (Hussong et al., 2013). Research indicates that risk processes can differ as a function of age and environment (Dick et al., 2006; Hussong et al., 2011; Kendler et al., 2008). For example, Sung and colleagues (2004) found that anxiety disorders increased the risk of developing SUDs in girls at age 16, but prior to this, anxiety disorders were unrelated to SUDs. Elkins et al. (2006) also found effects of timing of disorder onset such that the personality trait ‘low constraint’ was more robustly associated with the development of AUDs prior to age 17 relative to ages 17 to 20. This suggests that the effects of anxiety disorders and parental support may differ as a function of age/developmental period.
The aim of the current study is to test: 1) whether maternal and/or paternal support moderates the association between anxiety disorders and the development of AUDs and 2) whether the unique and interactive effects of anxiety disorders and parental support differ as a function of age of AUD onset. Data come from the Oregon Adolescent Depression Project (OADP; Lewinsohn et al., 1993) – an extensive 4-wave longitudinal study on adolescent and adult psychopathology. Anxiety disorders included in the study are social phobia, specific phobia, panic disorder, obsessive compulsive disorder, and separation anxiety disorder. Based on the reviewed literature, we hypothesized that at low maternal support, but not high maternal support, anxiety disorders would increase the risk of AUD onset.
2. METHODS
2.1 Participants and Procedures
Detailed descriptions of recruitment procedures, participation rates, and sample characteristics have previously been reported (Lewinsohn et al., 1993, 2003; Olino et al., 2008; Rohde et al., 2007). Briefly, participants were randomly selected from nine high schools in western Oregon. A total of 1,709 adolescents (mean age 16.6 years [SD = 1.2]) completed the initial (T1) assessment between 1987 and 1989. Approximately one year later, 1,507 of the adolescents completed the second assessment (T2). Once participants were 24 years old, a third wave (T3) of data collection took place. By design, only a subset of 941 individuals, over-sampled for psychopathology and non-white race, completed the T3 evaluation. Thus, those without a history of psychopathology by T2 were under-sampled. To account for this sampling approach, in each model adolescents were weighted based on their probability of being invited to participate in T3. At age 30, 816 of the participants completed a T4 assessment. Though differences between participants and non-participants at each wave were minor (Lewinsohn et al., 1993; Olino et al., 2008), individuals with a lifetime diagnosis of AUDs evidenced significantly higher attrition rates (17%) at the T4 assessment relative to individuals with no history of AUDs (12%). Higher attrition rates were also found for men versus women (16% vs. 11%) and for those with and without a history of cannabis use disorders (18% vs. 12%).
Participants were excluded from the current study if they did not participate in the T3 (n=566). An individual was classified as having an anxiety disorder (N = 80) if they had a lifetime diagnosis by T1 of social phobia (n = 12), specific phobia (n = 23), panic disorder (n = 4), obsessive compulsive disorder (n = 3), or separation anxiety disorder (n = 38). Of note, 11 individuals had more than one anxiety disorder diagnosis at T1. Analyses indicated that there were no differences between individuals with anxiety disorders at T1 that did and did not complete the T3 assessment on any major demographic or diagnostic variables. We excluded adolescents with a T1 lifetime diagnosis of alcohol abuse or dependence (n = 61) so that we could test the temporal relation between anxiety disorders and first onset of an AUD. Lastly, a subset of participants were excluded due to missing parental support (n = 16) or covariate data (n = 47). Our final sample included 817 individuals. Demographic and clinical information from the T1 assessment is provided in Table 1.
Table 1.
Participant Demographics, Clinical Characteristics, and Study Variables
| Those without Anxiety Disorders at T1 (n = 737) |
Those with Anxiety Disorders at T1 (n = 80) |
|
|---|---|---|
| Demographic Variables at T1 | ||
| Age (years; SD) | 16.6 (1.2)a | 16.7 (1.1)a |
| Gender (% female) | 56.3%a | 70.0%b |
| Race (% Caucasian) | 89.9%a | 92.1%a |
| Average Parent Education | ||
| Less than High School Degree | 7.5%a | 10.0%a |
| High School Degree or Equivalent | 62.4%a | 66.3%a |
| Greater than High School Degree | 30.1%a | 23.7%a |
| Alcohol Use Disorders T2-T4 | ||
| Alcohol Abuse | 15.7%a | 11.3%a |
| Alcohol Dependence | 18.5%a | 23.8%a |
| Study Variables at T1 | ||
| Maternal Support | 0.2 (4.3)a | −0.3 (3.8)a |
| Paternal Support | −0.1 (4.2)a | 0.1 (4.4)a |
| No. of People in the Household | 3.1 (1.4)a | 3.0 (1.6)a |
| Mother is Biological Mother | 90.1%a | 91.3%a |
| Father is Biological Father | 67.2%a | 57.5%a |
| Birth Order | 1.9 (1.1)a | 2.0 (1.3)a |
| Major Depressive Disorder Through T1 | 22.5%a | 41.3%b |
| Externalizing Disorder Through T1 | 10.3%a | 16.3%a |
| Coping Skills | 47.5 (7.5)a | 45.9 (7.9)a |
Note. Means or percentages with different subscripts across rows were significantly different in pairwise comparisons (p < .05, chi-square test for categorical variables and Tukey’s honestly significant difference test for continuous variables).
2.2 Diagnostic Assessments
Current and lifetime diagnoses were assessed directly at T1 and T2 and by telephone at T3 and T4. Phone interviews and direct interviews yielded high inter-method reliability for diagnoses and symptoms (Rohde et al., 1997). Participants were interviewed at T1 with a modified version of the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS; Chambers et al., 1985; Orvaschel et al., 1982), which included additional items used to derive DSM-III-R diagnoses (APA, 1987). At T2 and T3, participants were interviewed using the K-SADS and the Longitudinal Interval Follow-up Evaluation (LIFE; Keller et al., 1987) to assess psychopathology since the last interview. At T4, participants were administered the LIFE interview and the Structured Clinical Interview for Axis-I DSM-IV Disorders Non-Patient Edition (SCID-NP; First et al., 1996). Therefore, diagnoses were made according to DSM-III-R criteria (APA, 1987) for T1 and T2 and DSM-IV criteria (APA, 1994) for T3 and T4.
All interviewers were carefully trained and supervised, and completed a 70-hour course in diagnostic interviewing. The inter-rater reliability of lifetime diagnoses for any anxiety disorder (kappa = .94) and AUDs (kappa = .97) were excellent. Individuals were considered to have an anxiety disorder if they had a lifetime (i.e., current or past) diagnosis of an aforementioned anxiety disorder by the T1 assessment. At the T1 evaluation, 29 individuals had a current diagnosis of an anxiety disorder and 51 had a past diagnosis of an anxiety disorder. AUDs were coded as diagnoses of alcohol abuse or alcohol dependence starting after T1 through T4 (yes/no).
2.3 Maternal and Paternal Support
At the T1 evaluation, adolescents completed a battery of self-report measures. The Appraisal of Parents subscale of the Conflict Behavior Questionnaire (CBQ; 11 items; Prinz et al., 1979) and the Parental Attitude Research Instrument (PARI; 6 items; Schaefer, 1965) were combined to create the parental support measures. The CBQ assesses adolescent-parent communication, conflict, and relationship quality, while the PARI assesses emotional support and affection. Paraphrased examples of questionnaire items include: “I enjoy talking with my mother/father; My mother/father and I don’t get along; My mother/father believes in showing me love; My mother/father makes me feel better when I am worried.” For all items, participants based their ratings on the past four weeks. Maternal and paternal support variables were derived by standardizing each item and computing the mean of the standardized item scores. A prorated scale score was computed by multiplying the mean of the standardized item scores by the number of items in the scale (maternal support range: −3.3 to 13.5; paternal support range: −4.3 to 10.8). Analyses indicated acceptable reliability for maternal (α = .76) and paternal support (α = .77).
2.4 Covariates
Several well-established risk factors for AUDs, as well as other demographics, were included as covariates in the analyses - gender, average parental education (proxy for socioeconomic status), number of individuals living in the household at T1, whether or not each parent was the adolescents’ biological mother/father (separate parent variables coded yes/no), adolescent birth order, adolescent lifetime diagnoses of MDD through T1 (yes/no), adolescent lifetime diagnosis of an externalizing disorder (ADHD, CD, ODD, or illicit substance abuse or dependence) through T1 (yes/no), and adolescent self-reported coping skills. Coping skills were included in the model to account for unexplained variance in our dependent variable and increase power, as prior research indicates that maladaptive coping techniques are associated with AUD onset (Berking et al., 2011; Hasking et al., 2011). The coping skills variable was derived by computing the prorated mean of items from the Self-Control Scale (Rosenbaum, 1980), modified Antidepressive Activity Questionnaire (Rippere, 1977; Parker and Brown, 1979), and Ways of Coping Questionnaire (Folkman and Lazarus, 1980). This composite variable had adequate reliability in the current sample (α =.78). All covariates were assessed at T1 via adolescent self-report questionnaires or diagnostic interview.
2.5 Data Analysis Plan
To test our hypotheses, we used a series of Cox proportional hazards (PH) models. These models are similar to other regression techniques for dichotomous dependent variables (e.g., logistic regression) in that they allow for an examination of whether one or more variables predicts the likelihood of a specified outcome (Cox, 1972). PH models are superior to many of these other techniques, however, in that they allow for the timing of the event to be taken into account, not just whether or not the event occurred. In the current study, the time-to-event dependent variable was time (in years) since study enrollment (T1= 0 years) to the first onset of an AUD, or time of last assessment (i.e., total years enrolled in the study since the T1) for individuals that did not develop an AUD (i.e., censored observations). Separate PH models were used to examine the moderating effect of maternal and paternal support. Hazard ratios (HR) were used as estimates of effect size as they are considered indices of differences in hazards as a function of predictor variables.
A subset of adolescents did not have paternal support data (n = 70) and were therefore excluded from the paternal models. The proportional hazards assumption was tested by including a Time by Predictor interaction term in each Cox model (Singer and Willett, 1991). In all models, the interaction term was not significant (p’s > .79) and thus, the proportional hazard assumption was met and the interaction term was removed. Analyses were conducted using SUDAAN 8.0.3 (Shah et al., 1997).
Variables were entered into the models in three steps: all 8 covariates were simultaneously entered in Step1, the main effects of T1 lifetime diagnosis of an anxiety disorder and maternal or paternal support were entered in Step 2, and the interaction term was entered in Step 3. The covariates were identical for both maternal and paternal support models; however, whether or not the adolescents’ mother was the biological mother (yes/no) was included in the maternal support model, and whether or not the adolescents’ father was the biological father was included in the paternal support model.
To test the effects of developmental period, we first coded individuals that developed an AUD as either early onset (i.e., prior to age 20 years) or late onset (i.e., after age 20 years). Twenty years was chosen as the cut-off as it was the average age of AUD onset within the current sample, and was consistent with prior studies on median AUD age of onset (Kessler et al., 2005). Next, two separate PH models (identical to those described above) were run including either: 1) individuals that had developed an AUD prior to age 20 years and individuals that had never developed an AUD (total N = 681) and 2) individuals that had developed an AUD after age 20 years and individuals that had never developed an AUD (total N = 682). Therefore, the first model excluded individuals that developed an AUD after age 20 whereas the second model excluded individuals that developed an AUD prior to age 20.
3. RESULTS
3.1 Participant Diagnoses and Characteristics
At T1, 80 (9.8%) participants had a lifetime diagnosis of an anxiety disorder with a mean age of onset of 7.4 years (SD = 3.4). After T1, 280 (34.3%) participants developed an AUD. Of the 80 participants that had an anxiety disorder at T1, 28 (35%) developed an AUD during T2-T4. Average age of onset for an AUD was 20.8 years of age (SD = 3.2). Compared with adolescents without a lifetime history of anxiety disorders, participants with a lifetime diagnosis of an anxiety disorder at T1 reported greater levels of state anxiety (t(786) = 2.70, p < 0.05), worry (t(783) = 3.25, p < 0.05), and social anxiety (t(815) = 2.82, p < 0.05) at the T1 evaluation, and greater levels of worry (t(803) = 2.91, p < 0.05) and social anxiety (t(803) = 1.91, p = 0.05) at T2 (see Andrews et al., 1993 for detailed descriptions of self-report measures). This highlights that regardless of whether their anxiety diagnosis was current or past, adolescents with a lifetime diagnosis of anxiety disorders were more anxious than adolescents without an anxiety disorder diagnosis at T1 and T2. Individuals with anxiety disorders at T1 did not differ from individuals without anxiety disorders at T1 on maternal or paternal support (both p’s > 0.42). There were no significant differences between ratings of maternal and paternal support at T1 (p = 0.32).
3.2 Anxiety Disorders by Maternal Support Interaction on AUD onset
Results are presented in Table 2. There were no significant main effects of anxiety disorders at T1 or maternal support. However, there was a significant anxiety disorders by maternal support interaction. To follow-up the interaction, maternal support was centered 1 SD above and below the mean to probe the simple slopes (Aiken and West, 1991; Holmbeck, 2002). Two post-hoc PH models were run incorporating all the aforementioned covariates, anxiety disorders at T1, the moderator, and the interaction term. At low maternal support, individuals with anxiety disorders were 65% more likely to develop an AUD than individuals without anxiety disorders (HR = 1.65, 95% CI = 1.21 – 2.26, p < 0.01). At high maternal support, individuals with anxiety disorders were 35% less likely to develop an AUD than individuals without anxiety disorders (HR = 0.74, 95% CI = 0.55 – 1.00, p = 0.05).
Table 2.
Proportional hazards results examining unique and interactive effects of anxiety disorders at T1 and maternal support on time to develop an AUD.
| Variable | HR | 95% CI | p-value |
|---|---|---|---|
| Step 1 | |||
| Gender | 1.11 | 0.95 – 1.29 | 0.17 |
| Average Parent Education | 1.01 | 0.95 – 1.08 | 0.73 |
| No. of People in Household* | 0.94 | 0.89 – 0.99 | 0.03 |
| Mother’s Status | 0.97 | 0.76 – 1.24 | 0.81 |
| Birth Order | 1.01 | 0.95 – 1.08 | 0.66 |
| T1 MDD* | 1.23 | 1.04 – 1.45 | 0.02 |
| TI Externalizing Disorder+ | 1.26 | 0.98 – 1.62 | 0.07 |
| Coping Skills* | 0.99 | 0.98 – 0.99 | 0.04 |
| Step 2 | |||
| T1 Anxiety Disorders | 1.07 | 0.87 – 1.33 | 0.51 |
| Maternal Support | 1.00 | 0.98 – 1.02 | 0.91 |
| Step 3 | |||
| T1 Anxiety × Maternal Support** | 0.91 | 0.86 – 0.96 | < 0.00 |
Note.
p < 0.01;
p < 0.05;
p < 0.10;
MDD = major depressive disorder; Externalizing Disorder = attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, or illicit substance abuse or dependence; Mother’s Status = whether or not the mother was the adolescent’s biological mother.
3.3 Anxiety Disorders by Paternal Support Interaction on AUD onset
Results indicated that there were no significant main effects for anxiety disorders at T1 or paternal support. There was also no significant anxiety disorders at T1 by paternal support interaction (see Table 3).
Table 3.
Proportional hazards results examining unique and interactive effects of anxiety disorders at T1 and paternal support on time to develop an AUD.
| Variable | HR | 95% CI | p-value |
|---|---|---|---|
| Step 1 | |||
| Gender | 1.09 | 0.94 – 1.28 | 0.25 |
| Average Parent Education | 1.00 | 0.93 – 1.07 | 0.99 |
| No. of People in Household+ | 0.95 | 0.91 – 1.00 | 0.08 |
| Father’s Status | 0.97 | 0.82 – 1.14 | 0.72 |
| Birth Order | 1.01 | 0.95 – 1.07 | 0.79 |
| T1 MDD* | 1.25 | 1.05 – 1.48 | 0.01 |
| TI Externalizing Disorder+ | 1.29 | 0.98 – 1.70 | 0.07 |
| Coping Skills+ | 0.99 | 0.98 – 1.00 | 0.09 |
| Step 2 | |||
| T1 Anxiety Disorders | 1.13 | 0.89 – 1.44 | 0.30 |
| Paternal Support | 0.99 | 0.98 – 1.02 | 0.78 |
| Step 3 | |||
| T1 Anxiety × Paternal Support | 0.96 | 0.92 – 1.02 | 0.18 |
Note.
p < 0.05;
p < 0.10;
MDD = major depressive disorder; Externalizing Disorder = attention deficit hyperactivity disorder, conduct disorder, oppositional defiant disorder, or illicit substance abuse or dependence; Father’s Status = whether or not the mother was the adolescent’s biological father.
3.4 Early and Late Onset AUDs
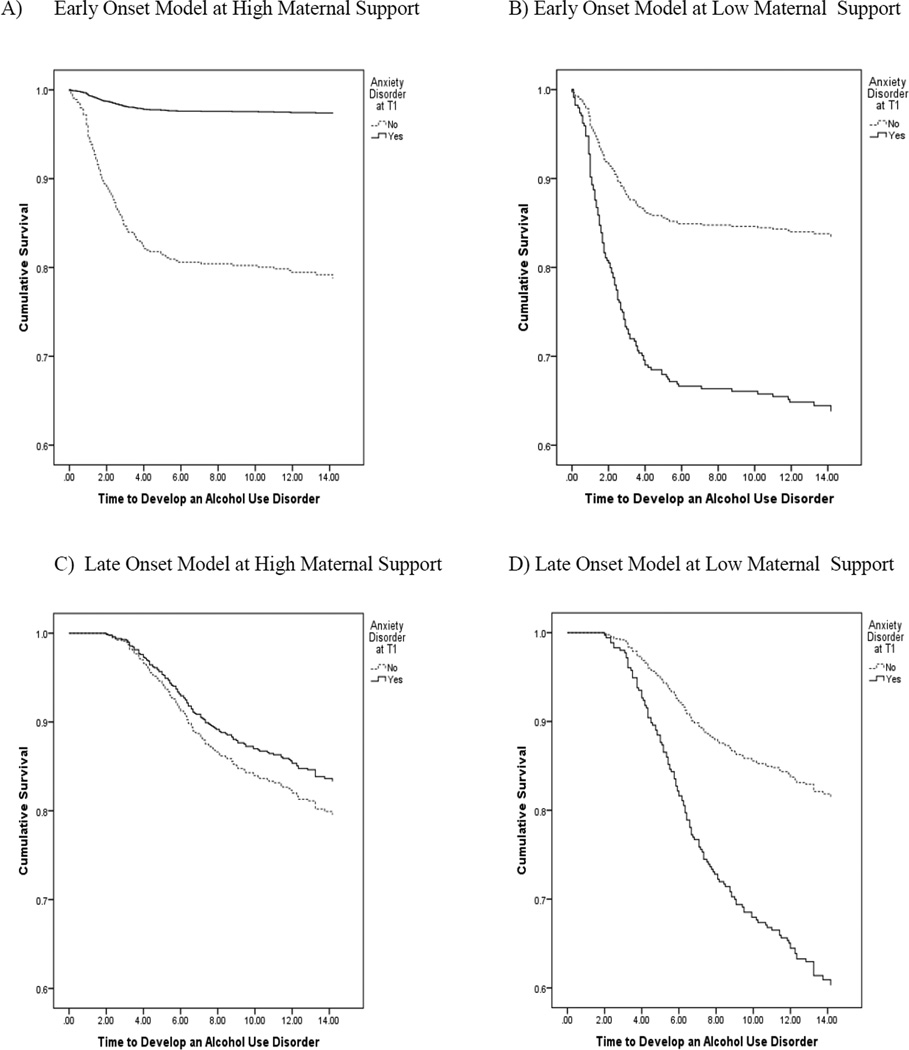
Results from the early onset model indicated that there was an anxiety disorders at T1 by maternal support interaction (HR = 0.92, 95% CI = 0.87 – 0.97, p < 0.01). At low maternal support, anxiety disorders were associated with a 50% greater risk of AUD onset (HR = 1.50, 95% CI = 1.06 – 2.13, p < 0.01). At high maternal support, anxiety disorders at T1 were associated with a 39% reduced risk of AUD onset (HR = 0.72, 95% CI = 0.52 – 0.98, p = 0.02). Results from the late onset model also indicated an anxiety disorders at T1 by maternal support interaction (HR = 0.92, 95% CI = 0.87 – 0.98, p = 0.01). At low maternal support, anxiety disorders at T1 were associated with a 73% greater risk of AUD onset (HR = 1.73, 95% CI = 1.19 – 2.52, p < 0.01). At high maternal support, anxiety disorders at T1 were not associated with AUD onset (HR = 0.90, 95% CI = 0.64 – 1.25, p = 0.52). These effects are displayed in Figure 1.
Figure 1.
Survival hazards plot of the relation between anxiety disorders at T1 and time to develop an alcohol use disorder, at high and low maternal support, for early onset and late onset AUDs.
We also examined the moderating effect of paternal support for early and late onset AUDs. There was no significant interaction for the early onset (p = 0.13) or late onset AUD model (p = 0.19).
3.5 Additional Post-hoc Analyses
To examine the effects of our covariates, we conducted two PH models with just the main effects and the interaction term (i.e., no covariates). Results were consistent with the aforementioned findings – the anxiety disorders by maternal support interaction was significant (HR = 0.91, 95% CI = 0.87 – 0.96, p < 0.001) and the anxiety disorders by paternal support interaction was not significant (p = 0.17). We also conducted an additional analysis (with covariates) with both maternal and paternal support included in the model. Results indicated that the anxiety disorders at T1 by maternal support interaction remained significant (HR = 0.92, 95% CI = 0.86 – 0.97, p < 0.01), and the pattern of results was unchanged.
4. DISCUSSION
The aim of the current study was to examine whether parental support moderates the association between childhood/adolescent anxiety disorders and AUDs, and whether these effects differ as a function of age of AUD onset. Results indicated that across adolescence and early adulthood there was a significant anxiety disorders at T1 by maternal support interaction. Specifically, at low maternal support, anxiety disorders were associated with an increased risk for AUD onset. At high levels of maternal support, anxiety disorders were associated with a reduced risk for AUD onset at a trend level.
Interestingly, this pattern of results differed as a function of age of AUD onset. For individuals that developed an AUD prior to age 20, relative to later in life, anxiety disorders were more robustly associated with a reduced risk for AUD onset at high maternal support. The opposite was true at low maternal support. Anxiety disorders increased the risk of AUDs across both developmental periods. Therefore, anxiety disorders functioned as both a risk and protective factor at high versus low levels of support. These findings help to clarify previous mixed findings in the literature and indicate that perceptions of maternal support across early development have an important influence on the likelihood of developing AUDs.
At low levels of maternal support, our findings suggest that anxiety disorders are a risk factor for the development of AUDs across adolescence and early adulthood. This is consistent with the broader internalizing disorder-substance use literature which posits that individuals with anxiety are motivated to engage in alcohol use to reduce or avoid their negative affect (Baker et al., 2004; O’Neil et al., 2011). Specifically, acute alcohol consumption is thought to bring perceived relief from negative affective states (Abrams et al., 2001; Thomas et al., 2003), thereby negatively reinforcing this behavior and increasing the likelihood of continued use (Kassel et al., 2000; Robinson et al., 2011).
Although negative reinforcement processes could apply to all individuals with anxiety disorders, the results suggest that those with perceived low maternal support may be specifically vulnerable to AUD onset. It is possible that children and adolescents with low maternal support have less physical, emotional, and financial resources to cope with their distress, which makes them vulnerable to lifelong patterns of maladaptive coping. It is also possible that mothers that are perceived as providing low support engage in maladaptive parenting behaviors (and may even have anxiety disorders themselves) that impair the development of self-regulation capabilities in their offspring (Morris et al., 2007). This impairment may have persistent deleterious effects including increased vulnerability for alcohol use. Lastly, low maternal support may be associated with an overall aversive home environment which causes individuals to avoid home, spend more time with peers, and consequently, have more opportunities to initiate alcohol use (Duncan et al., 1994). High levels of anxiety coupled with early exposure to alcohol may ultimately propel individuals along the internalizing pathway to AUDs.
Our results indicate that at high maternal support, anxiety disorders decrease risk for developing AUDs. Notably, this protective effect is slightly weaker than the risk effect at low maternal support. Moreover, individuals with anxiety disorders were ‘protected’ from AUD onset at high maternal support to a greater extent prior to age 20. There are several potential mechanisms that may contribute to this finding. Most notably, children and adolescents with anxiety disorders often exhibit interpersonal deficits which could cause them to withdraw from peers and abstain from social activities (Chansky and Kendall, 1997; Clark et al., 1994). Since experimentation with alcohol frequently occurs in social settings in adolescence and early adulthood (Hussong, 2000) individuals with anxiety disorders may have fewer opportunities to experiment with alcohol and subsequently develop AUDs (Fite et al., 2006).
The findings suggest that the ‘protective power’ of anxiety may only apply to children and adolescents with perceived high maternal support. One possibility for this result is that those with a highly supportive mother may perceive their overall home environment as pleasant and be most reluctant to leave home and engage in social activities, including alcohol use. Alternatively, highly supportive mothers may also exhibit parenting behaviors that could be considered accommodating of the child’s anxiety symptoms which could implicitly or explicitly maintain anxiety symptoms and discourage adolescents to affiliate with peers. Importantly, past age 20, high maternal support no longer had a significant effect on AUDs. Given that after age 20, cohabitation with mothers is less frequent and alcohol is more easily accessible, perceived maternal support may no longer have an effect and these ‘protected’ (or overprotected) individuals may become vulnerable to AUD onset later in life.
Our findings indicated that perceived paternal support did not influence the association between anxiety disorders and AUDs. Research indicates that mothers often spend more time with their offspring than fathers during childhood through adolescence (Craig, 2006). Therefore, maternal support may be a more potent factor to individuals with anxiety disorders than paternal support. Second, evidence has suggested that mothers play more of a role in the emotional developmental of their offspring (Fivush et al., 2000; McDowell et al., 2002), and thus, may also play a larger role in onset of psychopathology. Third, of the individuals with anxiety disorders in the current study, approximately 58% were living with a step-father at T1. However, almost all individuals (91%) were living with their biological mother. It is therefore possible that the current pattern of results is specific to biological parents and not step-parents. Therefore, future studies are needed to clarify the role of biological fathers’ support.
Although these findings address important gaps in the literature, there are several limitations of note. First, the current sample of individuals with anxiety disorders at T1 was relatively small (9.8%) which likely reduced statistical power. Second, we did not include post-traumatic stress disorder (PTSD) or generalized anxiety disorder (GAD) in our baseline anxiety variable, as these disorders were not assessed at T1. It is important to note, however, that PTSD and GAD are both highly comorbid with other anxiety disorders (Kessler et al., 2005) and it is likely that some of these cases were accounted for. Third, our measure of parental support was broad and it is possible that different facets of support (e.g., affection, communication patterns) differentially moderate the association between anxiety disorders and AUD onset. Similarly, due to our small sample size, we were unable to adequately examine alcohol abuse and alcohol dependence as separate outcome variables. Of note, however, in the recent 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM5; APA, 2013), both disorders were consolidated into one condition. Fourth, we did not directly examine peer factors in the current study and it is possible that peer support and/or delinquent peer affiliation impacts the current findings. This is therefore an important area of future research. Lastly, there were a subset of individuals in the present study that did not have parental support data and individuals with AUDs had slightly higher attrition rates than individuals without AUDs. This may have affected the generalizability of the current sample and underscores the need for replication.
With these limitations in mind, there are several important implications of these findings. Most notably, perceived maternal support has a significant impact on the anxiety disorders-AUD pathway, but that the magnitude and direction of effects differs as a function of level of support and developmental period. Alcohol use intervention efforts may therefore benefit by assessing perceived maternal support in adolescents with anxiety disorders. More specifically, among adolescents with anxiety disorders and perceived low maternal support, family-based cognitive behavioral therapy (Creswell and Cartwright-Hatton, 2007) may consider systematically targeting expressions of maternal support to mitigate risk of AUDs. In contrast, adolescents with anxiety disorders that report high maternal support may not be at an immediate risk for AUDs and thus, a focus may be on assessing how other vulnerability and risk processes could contribute to their development of AUDs over time.
Acknowledgments
Role of Funding Source
Funding for this study was provided by NIAAA Grant F31 AA022273-01A1 awarded to Stephanie M. Gorka, NIMH Grant R01 MH098093-02 awarded to Stewart Shankman, and NIMH Grants R01 MH40501 and R01 MH50522 awarded to Peter Lewinsohn. The NIAAA and NIMH had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
Peter Lewinsohn was the principal investigator of the Oregon Adolescent Depression Project. John Seeley contributed to the design of the study and was involved in the collection and management of data. Thomas Olino, Derek Kosty, and Stewart Shankman provided assistance with statistical analyses and made important contributions to the editing of the manuscript. Stephanie Gorka provided the rationale for the paper, conducted the statistical analyses, and wrote the first draft of the manuscript. All authors contributed and have approved the final manuscript.
Conflict of Interest
All authors declare that they have no conflicts of interest.
REFERENCES
- Abrams K, Kushner M, Medina KL, Voight A. The pharmacologic and expectancy effects of alcohol on social anxiety in individuals with social phobia. Drug Alcohol Depend. 2001;64:219–231. doi: 10.1016/s0376-8716(01)00125-9. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple Regression: Testing and Interpreting Interactions. Thousand Oaks, CA: Sage; 1991. [Google Scholar]
- Albano AM, Chorpita BF, Barlow DH. Childhood anxiety disorders. In: E. J. Mash EJ, Barkley RA, editors. Child Psychopathology. New York: Guilford; 1996. pp. 196–241. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (3rd ed., rev.) Washington, DC: APA; 1987. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (4th ed.) Washington, DC: APA; 1994. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (5th ed.) Washington, DC: APA; 2013. [Google Scholar]
- Andrews JA, Lewinsohn PM, Hops H, Roberts RE. Psychometric properties of scales for the measurement of psychosocial variables associated with depression in adolescence. Psychol. Rep. 1993;73:1019–1046. doi: 10.2466/pr0.1993.73.3.1019. [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, Fiore MC. Addiction motivation reformulated: an affective processing model of negative reinforcement. Psychol. Rev. 2004;111:33–51. doi: 10.1037/0033-295X.111.1.33. [DOI] [PubMed] [Google Scholar]
- Berking M, Margraf M, Ebert D, Wupperman P, Hofmann SG, Junghanns K. Deficits in emotion-regulation skills predict alcohol use during and after cognitive–behavioral therapy for alcohol dependence. J. Consult. Clin. Psychol. 2011;79:307. doi: 10.1037/a0023421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bolton JM, Robinson J, Sareen. J. Self-medication of mood disorders with alcohol and drugs in the National Epidemiologic Survey on Alcohol and Related Conditions. J. Affect. Disord. 2009;115:367–375. doi: 10.1016/j.jad.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Booth-LaForce C, Oh W, Kennedy AE, Rubin KH, Rose-Krasnor L, Laursen B. Parent and peer links to trajectories of anxious withdrawal from grades 5 to 8. J. Clin. Child. Adolesc. Psychol. 2012;41:138–149. doi: 10.1080/15374416.2012.651995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chambers WJ, Puig-Antich J, Hirsch M, Paez P, Ambrosini PJ, Tabrizi MA, Davies M. The assessment of affective disorders in children and adolescents by semi-structured interview: Test-retest reliability of the Schedule for Affective Disorders and Schizophrenia for School-Age Children, Present Episode version. Arch. Gen. Psychiatry. 1985;42:696–702. doi: 10.1001/archpsyc.1985.01790300064008. [DOI] [PubMed] [Google Scholar]
- Chansky TE, Kendall PC. Social expectancies and self-perceptions in anxietydisordered children. J. Anxiety Disord. 1997;11:347–363. doi: 10.1016/s0887-6185(97)00015-7. [DOI] [PubMed] [Google Scholar]
- Charach A, Yeung E, Climans T, Lillie E. Childhood attention deficit/hyperactivity disorder and future substance use disorders: comparative meta-analyses. J. Am. Acad. Child Psy. 2011;50:9–21. doi: 10.1016/j.jaac.2010.09.019. [DOI] [PubMed] [Google Scholar]
- Clark DB, Smith MG, Neighbors BD, Skerlec LM, Randall J. Anxiety disorders in adolescence: characteristics, prevalence, and comorbidities. Clin. Psychol. Rev. 1994;14:113–137. [Google Scholar]
- Clauss JA, Blackford JU. Behavioral inhibition and risk for developing social anxiety disorder: a meta-analytic study. J. Am. Acad. Child Adolesc. Psychiatry. 2012;51:1066–1075. doi: 10.1016/j.jaac.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig L. Does father care mean fathers share? A comparison of how mothers and fathers in intact families spend time with children. Gend. Soc. 2006;20:259–281. [Google Scholar]
- Creswell C, Cartwright-Hatton S. Family treatment of child anxiety: outcomes, limitations and future directions. Clin. Child. Fam. Psych. 2007;10:232–252. doi: 10.1007/s10567-007-0019-3. [DOI] [PubMed] [Google Scholar]
- Crum RM, Mojtabai R, Lazareck S, Bolton JM, Robinson J, Sareen J, Green KM, Stuart EA, LaFlair L, Alvanzo AA, Storr CL. A prospective assessment of reports of drinking to self-medicate mood symptoms with the incidence and persistence of alcohol dependence. JAMA Psychiatry. 2013;70:718–726. doi: 10.1001/jamapsychiatry.2013.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crum RM, Pratt LA. Risk of heavy drinking and alcohol use disorders in social phobia: a prospective analysis. Am. J. Psychiatry. 2001;158:1693–1700. doi: 10.1176/appi.ajp.158.10.1693. [DOI] [PubMed] [Google Scholar]
- Dick DM, Rose RJ, Kaprio J. The next challenge for psychiatric genetics: characterizing the risk associated with identified genes. Ann. Clin. Psychiatry. 2006;18:223–231. doi: 10.1080/10401230600948407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dixit AR, Crum RM. Prospective study of depression and the risk of heavy alcohol use in women. Am. J. Psychiatry. 2000;157:751–758. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC, Hops H. Effects of family cohesiveness and peer encouragement on the development of adolescent alcohol use: A cohort-sequential approach to the analysis of longitudinal data. J. Stud. Alcohol. 1994;55:588–599. doi: 10.15288/jsa.1994.55.588. [DOI] [PubMed] [Google Scholar]
- Elkins IJ, King SM, McGue M, Iacono WG. Personality traits and the development of nicotine, alcohol, and illicit drug disorders: Prospective links from adolescence to young adulthood. J. Abnorm. Psychol. 2006;115(1):26–39. doi: 10.1037/0021-843X.115.1.26. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Non-patient Edition (SCID-NP, Version 2.0) New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- Fite PJ, Colder CR, O'Connor RM. Childhood behavior problems and peer selection and socialization: risk for adolescent alcohol use. Addict. Behav. 2006;31:1454–1459. doi: 10.1016/j.addbeh.2005.09.015. [DOI] [PubMed] [Google Scholar]
- Fivush R, Brotman MA, Buckner JP, Goodman SH. Gender differences in parent–child emotion narratives. Sex Roles. 2000;42:233–253. [Google Scholar]
- Folkman S, Lazarus RS. An analysis of coping in a middle-aged community sample. J. Health Soc. Behav. 1980;21:219–239. [PubMed] [Google Scholar]
- Hasking P, Lyvers M, Carlopio C. The relationship between coping strategies, alcohol expectancies, drinking motives and drinking behaviour. Addict. Behav. 2011;36:479–487. doi: 10.1016/j.addbeh.2011.01.014. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States: results from the National Epidemiologic Survey on Alcohol and Related Problems. Arch. Gen. Psychiatry. 2007;64:830–842. doi: 10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Burns AR, Solis JM, Rothenberg WA. Future directions in the developmental science of addictions. J. Clin. Child Adoles. 2013 doi: 10.1080/15374416.2013.838772. (epub ahead-of-print). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong AM, Curran PJ, Chassin L. Pathways of risk for accelerated heavy alcohol use among adolescent children of alcoholic parents. J. Abnorm. Child Psychol. 1998;26:453–466. doi: 10.1023/a:1022699701996. [DOI] [PubMed] [Google Scholar]
- Hussong AM, Jones DJ, Stein GL, Baucom DH, Boeding S. An internalizing pathway to alcohol use and disorder. Psychol. Addict. Behav. 2011;25:390–404. doi: 10.1037/a0024519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iacono WG, Malone SM, McGue M. Behavioral disinhibition and the development of early-onset addiction: common and specific influences. Annu. Rev. Clin. Psychol. 2008;4:325–348. doi: 10.1146/annurev.clinpsy.4.022007.141157. [DOI] [PubMed] [Google Scholar]
- Kagan J. An Argument for Mind. New Haven: Yale University Press; 2007. [Google Scholar]
- Kaplow JB, Curran PJ, Angold A, Costello EJ. The prospective relation between dimensions of anxiety and the initiation of adolescent alcohol use. J. Clin. Child Psychol. 2001;30:316–326. doi: 10.1207/S15374424JCCP3003_4. [DOI] [PubMed] [Google Scholar]
- Kassel JD, Jackson SI, Unrod M. Generalized expectancies for negative mood regulation and problem drinking among college students. J. Stud. Alcohol Drugs. 2000;61:332–340. doi: 10.15288/jsa.2000.61.332. [DOI] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E, Endicott J, McDonald-Scott PA. The Longitudinal Interval Follow-up Evaluation: a comprehensive method for assessing outcome in prospective longitudinal studies. Arch. Gen. Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kendler KS, Schmitt E, Aggen SH, Prescott CA. Genetic and environmental influences on alcohol, caffeine, cannabis, and nicotine use from early adolescence to middle adulthood. Arch. Gen. Psychiatry. 2008;65:674–682. doi: 10.1001/archpsyc.65.6.674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch. Gen. Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- Kushner MG, Wall MM, Krueger RF, Sher KJ, Maurer E, Thuras P, Lee S. Alcohol dependence is related to overall internalizing psychopathology load rather than to particular internalizing disorders: evidence from a national sample. Alcohol. Clin. Exp. Res. 2012;36:325–331. doi: 10.1111/j.1530-0277.2011.01604.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Holm-Denoma JM, Small JW, Seeley JR, Joiner TE., Jr Separation anxiety disorder in childhood as a risk factor for future mental illness. J. Am. Acad. Child Adolesc. Psychiatry. 2008;47:548–555. doi: 10.1097/CHI.0b013e31816765e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewinsohn PM, Hops H, Roberts RE, Seeley JR, Andrews JA. Adolescent psychopathology: I. Prevalence and incidence of depression and other DSM-III-R disorders in high school students. J. Abnorm. Psychol. 1993;102:133–144. doi: 10.1037//0021-843x.102.1.133. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Alcohol consumption in high school adolescents: frequency of use and dimensional structure of associated problems. Addiction. 1996;91:375–390. doi: 10.1046/j.1360-0443.1996.9133757.x. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR, Klein DN, Gotlib I. Psychosocial functioning of young adults who have experienced and recovered from major depressive disorder during adolescence. J. Abnorm. Psychol. 2003;112:353–363. doi: 10.1037/0021-843x.112.3.353. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Zinbarg R, Seeley JR, Lewinsohn M, Sack WH. Lifetime comorbidity among anxiety disorders and between anxiety disorders and other mental disorders in adolescents. J. Anxiety Disord. 1997;11:377–394. doi: 10.1016/s0887-6185(97)00017-0. [DOI] [PubMed] [Google Scholar]
- Littlefield AK, Sher KJ, Wood PK. A personality-based description of maturing out of alcohol problems: extension with a five-factor model and robustness to modeling challenges. Addict. Behav. 2010;35:948–954. doi: 10.1016/j.addbeh.2010.06.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McDowell DJ, Kim M, O'neil R, Parke RD. Children's emotional regulation and social competence in middle childhood: the role of maternal and paternal interactive style. Marriage Fam. Rev. 2002;34:345–364. [Google Scholar]
- Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- Morris AS, Silk JS, Steinberg L, Myers SS, Robinson LR. The role of the family context in the development of emotion regulation. Soc. Dev. 2007;16:361–388. doi: 10.1111/j.1467-9507.2007.00389.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Kazdin AE, Hiripi E, Kessler RC. Prevalence, subtypes, and correlates of DSM-IV conduct disorder in the National Comorbidity Survey Replication. Psychol. Med. 2006;36:699–710. doi: 10.1017/S0033291706007082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olino TM, Klein DN, Lewinsohn PM, Rohde P, Seeley JR. Longitudinal associations between depressive and anxiety disorders: a comparison of two trait models. Psychol. Med. 2008;38:353–363. doi: 10.1017/S0033291707001341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Neil KA, Conner BT, Kendall PC. Internalizing disorders and substance use disorders in youth: comorbidity, risk, temporal order, and implications for intervention. Clin. Psychol. Rev. 2011;31:104–112. doi: 10.1016/j.cpr.2010.08.002. [DOI] [PubMed] [Google Scholar]
- Orvaschel H, Puig-Antich J, Chambers WJ, Tabrizi MA, Johnson R. Retrospective assessment of prepubertal major depression with the Kiddie-SADS-E. J. Am. Acad. Child Psychiatry. 1982;21:392–397. doi: 10.1016/s0002-7138(09)60944-4. [DOI] [PubMed] [Google Scholar]
- Parker JS, Benson MJ. Parent-adolescent relations and adolescent functioning: self-esteem, substance abuse, and delinquency. Adolescence. 2004;39:519–530. [PubMed] [Google Scholar]
- Parker G, Brown LB. Repertoires of response to potential precipitants of depression. Aust. NZ J. Psychiatry. 1979;13:327–333. doi: 10.3109/00048677909159155. [DOI] [PubMed] [Google Scholar]
- Patterson GR, Dishion TJ, Yoerger K. Adolescent growth in new forms of problem behavior: macro- and micro-peer dynamics. Prev. Sci. 2000;1:3–13. doi: 10.1023/a:1010019915400. [DOI] [PubMed] [Google Scholar]
- Prinz RJ, Foster S, Kent RN, O’Leary KD. Multivariate assessment of conflict in distressed and nondistressed mother-adolescent dyads. J. Appl. Behav. Anal. 1979;12:691–700. doi: 10.1901/jaba.1979.12-691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- Rippere V. Some cognitive dimensions of antidepressive behaviour. Behav. Res. Ther. 1977;15:57–63. doi: 10.1016/0005-7967(77)90088-2. [DOI] [PubMed] [Google Scholar]
- Robinson J, Sareen J, Cox BJ, Bolton JM. Role of self-medication in the development of comorbid anxiety and substance use disorders: a longitudinal investigation. Arch. Gen. Psychiatry. 2011;68:800–807. doi: 10.1001/archgenpsychiatry.2011.75. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR. Comparability of telephone and face-to-face interviews assessing Axis I and II disorders. Am. J. Psychiatry. 1997;154:1593–1598. doi: 10.1176/ajp.154.11.1593. [DOI] [PubMed] [Google Scholar]
- Rohde P, Lewinsohn PM, Seeley JR, Klein DN, Andrews JA, Small JW. Psychosocial functioning of adults who experienced substance use disorders as adolescents. Psychol. Addict. Behav. 2007;21:155–164. doi: 10.1037/0893-164X.21.2.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum MA. A schedule for assessing self-control behaviors: preliminary findings. Behav. Ther. 1980;11:109–121. [Google Scholar]
- Schaefer ES. Children’s report of parental behavior: an inventory. Child Dev. 1965;36:413–424. [PubMed] [Google Scholar]
- Shah BV, Barnwell BG, Biegler GS. SUDAAN User’s Manual, release 7.5. Research Triangle Park, NC: Research Triangle Institute; 1997. [Google Scholar]
- Sher KJ, Grekin ER, Williams NA. The development of alcohol use disorders. Annu. Rev. Clin. Psychol. 2005;1:493–523. doi: 10.1146/annurev.clinpsy.1.102803.144107. [DOI] [PubMed] [Google Scholar]
- Stadler C, Feifel J, Rohrmann S, Vermeiren R, Poustka F. Peer-victimization and mental health problems in adolescents: are parental and school support protective? Child Psychiat. Hum. D. 2010;41:371–386. doi: 10.1007/s10578-010-0174-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sung M, Erkanli A, Angold A, Costello EJ. Effects of age at first substance use and psychiatric comorbidity on the development of substance use disorders. Drug Alcohol Depend. 2004;75:287–299. doi: 10.1016/j.drugalcdep.2004.03.013. [DOI] [PubMed] [Google Scholar]
- Swendsen JD, Tennen H, Carney MA, Affleck G, Willard A, Hromi A. Mood and alcohol consumption: an experience sampling test of the self-medication hypothesis. J. Abnorm. Psychol. 2000;109:198–204. [PubMed] [Google Scholar]
- Thomas SE, Randall CL, Carrigan MH. Drinking to cope in socially anxious individuals: a controlled study. Alcohol. Clin. Exp. Res. 2003;27:1937–1943. doi: 10.1097/01.ALC.0000100942.30743.8C. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, Klein DJ. Growing up in a permissive household: what deters at-risk adolescents from heavy drinking? J. Stud. Alcohol Drugs. 2008;69:528–534. doi: 10.15288/jsad.2008.69.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neurosci. Biobehav. R. 2008;32:777–810. doi: 10.1016/j.neubiorev.2007.11.003. [DOI] [PubMed] [Google Scholar]
- Wilcox HC, Conner KR, Caine ED. Association of alcohol and drug use disorders and completed suicide: an empirical review of cohort studies. Drug Alcohol Depend. 2004;76:S11–S19. doi: 10.1016/j.drugalcdep.2004.08.003. [DOI] [PubMed] [Google Scholar]
- Wills TA, Cleary SD. How are social support effects mediated? A test with parental support and adolescent substance use. J. Pers. Soc. Psychol. 1996;71:937–952. doi: 10.1037//0022-3514.71.5.937. [DOI] [PubMed] [Google Scholar]
- Wills TA, Sandy JM, Yaeger A, Shinar O. Family risk factors and adolescent substance use: moderation effects for temperament dimensions. Dev. Psychol. 2001;37:283–297. [PubMed] [Google Scholar]
- Zucker RA. Alcohol use and the alcohol use disorders: a developmental-biopsychosocial systems formulation covering the life course. In: Cicchetti D, Cohen DJ, editors. Developmental Psychopathology: Vol. 3. Risk, Disorder and Adaptation. New York, NY: Wiley; 2006. [Google Scholar]
- Zucker RA. Anticipating problem alcohol use developmentally from childhood into middle adulthood: what have we learned? Addiction. 2008;103:100–108. doi: 10.1111/j.1360-0443.2008.02179.x. [DOI] [PMC free article] [PubMed] [Google Scholar]