Abstract
♦ Objective: We evaluated the role of a quality improvement initiative in improving clinical outcomes in peritoneal dialysis (PD).
♦ Methods: In a retrospective analysis of 6 years of data from a hospital registry, the period between 1 July 2005 and 30 June 2008 (control group) provided baseline data from before implementation of systemic outcomes monitoring, and the period between 1 July 2008 and 30 June 2011 [continuous quality improvement (CQI) group] represented the time when a CQI program was in place. Peritonitis incidence, patient and technique survival, cardiovascular status, causes of death, and drop-out were compared between the groups.
♦ Results: In the 370 patients of the CQI group and the 249 patients of the control group, the predominant underlying kidney diseases were chronic glomerulonephritis and diabetic nephropathy. After implementation of the CQI initiative, the peritonitis rate declined to 1 episode in 77.25 patient-months from 1 episode in 22.86 patient-months. Ultrasound parameters of cardiac structure were generally unchanged in the CQI group, but significant increases in cardiothoracic ratio and interventricular septal thickness were observed in the control group (both p < 0.05). Patient survival at 1, 2, and 3 years was significantly higher in the CQI group (97.3%, 96.3%, and 96.3% respectively) than in the control group (92.6%, 82.4%, and 67.3% respectively, p < 0.001). Implementation of the CQI initiative also appeared to significantly improve technique survival rates: 95.6%, 92.6%, and 92.6% in the CQI group compared with 89.6%, 79.2%, and 76.8% in the control group (p < 0.001) after 1, 2, and 3 years respectively.
♦ Conclusion: Integration of a CQI process into a PD program can significantly improve the quality of therapy and its outcomes.
Keywords: Continuous quality improvement, outcomes
Clinical studies have shown that mortality and technique survival rates in peritoneal dialysis (PD) are closely associated with the implementation of quality monitoring initiatives (1,2) and with the size and experience of the PD center (3). Adopting quality standards for PD is a key factor in improving outcomes in both developed and developing parts of the world. To enhance the quality of care, the International Society for Peritoneal Dialysis has developed a number of guidelines for managing PD. However, there is a lack of guidance on how to implement such models.
In recent years, the number of PD centers and the number of PD patients have both increased rapidly in China's Jiangsu Province as a consequence of the recommendations of the Chinese Medical Administrative Command, a provincial bureau responsible for medical insurance. That entity has reimbursed PD and hemodialysis (HD) equally since 2010. We established a PD program with a dedicated PD team in 2008, and since then, we have implemented guidelines and new procedures. The number of PD patients grew to 510 in 2011 from 50 in 2005 likely because of those two factors. In parallel, a number of key performance indicators such as the peritonitis incidence reached or exceeded internationally accepted levels. Here, we describe the effects on mortality and morbidity in PD of introducing a continuous quality improvement (CQI) program.
Methods
Patients
Between July 2005 and June 2011, we inserted catheters for 624 PD patients (Figure 1). In the present study, we divided our 6 years of experience (2005 - 2011) into two time periods to compare the effects of a CQI program on PD quality. The CQI group comprised PD patients who started PD between 1 July 2008 and 30 June 2011; the control group comprised patients initiating PD between 1 July 2005 and 30 June 2008—that is, before implementation of the CQI program. Patients who suffered acute kidney injury, who underwent HD or transplantation before PD, or who were not stabilized on PD within 3 months after initiation were excluded. Thus, 619 patients (18-75 years of age at start of PD) were included in the present study.
Figure 1 —
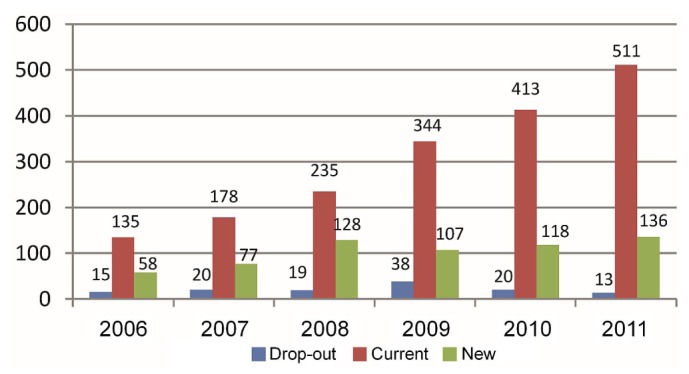
Number of incident, prevalent, and drop-out patients at 30 June, by year.
PD Management in the Pre-CQI Period
Before July 2008, we did not have a dedicated PD team, and thus PD patients were usually managed by whichever nephrologist they met at the outpatient clinic. Follow-up was irregular, and patient records or data were incomplete. No comprehensive training program led by a PD nurse was available.
PD Management During the CQI Program
In this period, the PD program was managed by a dedicated team. Three PD physicians were responsible for catheter insertion, follow-up, data analysis, and CQI, and four nurses were responsible for patient education (one nurse), follow-up and data collection (two nurses), and CQI (one nurse). All members of the team worked together in the clinic and at the ward. All data—such as those concerning dialysis adequacy, nutrition status, glomerular filtration rate, cardiac function, and so on—were collected and recorded in a PD database at our hospital.
The CQI program had 3 phases:
The first phase included identification of the outcome parameters on which to focus, implementation of targets for those parameters, a comparison of center data with those targets, identification of the likely causes of any differences, and development of an intervention strategy.
The second phase of the program verified the feasibility of the proposed procedural changes. After the modifications had been implemented, data were collected and compared with the new targets.
In the final phase, the robustness of the outcomes was ensured by continuation of the monitoring.
The PD team held monthly meetings to discuss and review each phase in the CQI process. This approach helped to identify and resolve procedural issues, and to maintain engagement in and motivation for the CQI program.
Two Examples of Key Performance Indicator Targets
Between 2005 and 2007, the most common causes of death and PD drop-out were cardio- and cerebrovascular diseases and peritonitis. Cardio- or cerebrovascular disease accounted for 60.9% of all deaths and 47.4% of all drop-outs. During the same period, the rate of peritonitis fluctuated at around 1 episode in 22 patient-months, and the percentage of patients with adequate blood pressure was low (47.4%). Because persistent high blood pressure is the most important risk factor for heart failure and cerebrovascular disease (4), we implemented a plan to achieve adequate blood pressure control (≤140/90 mmHg) in 60% or more of the patients. In addition to prescribing hypertensive agents to treat hypertension, we provided 5 g spoons to all patients to encourage normal salt intake (5 g daily). Furosemide was also given in some patients.
At the start of this new initiative, we planned to achieve a peritonitis rate of 1 episode in 30 patient-months. The plan included an assessment, by telephone call or home visit, of risk factors for each patient—for example, failure to wear a mask, washing hands incorrectly, and so on. In most cases, the home environment was bad, the handwashing procedure was wrong, and some patients did not use a mask or wear clean clothes when performing bag exchanges. Our improvement strategy therefore focused on mandatory use of clean “PD clothes” for the exchanges. Our strategy was implemented using an education program and provision of free PD clothes every 3 months. Compliance with the changes was monitored by monthly telephone calls to each patient.
Quality Evaluation
Mortality was defined as death related to the treatment being received. Death within 3 months of transfer to HD was regarded as a PD-related death. Technique failure was defined as the need to transfer to HD permanently because of peritonitis, ultrafiltration failure, subcutaneous tunnel infection, or underdialysis.
Statistical Methods
Statistical analyses were performed using the Statistica software application (version 6.0: StatSoft, Tulsa, OK, USA). Quantitative data are presented as means with standard error, or as medians. Between-group differences were analyzed using chi-square tests. Kaplan-Meier analysis was used to calculate patient and technique survival rates according to the time of death or of last follow-up. Values of p < 0.05 were considered statistically significant.
Results
Patients
There were no significant differences between the patient groups with respect to age or sex (Table 1). Chronic glomerulonephritis was the primary underlying kidney disease in both groups. The percentage of patients with diabetic nephropathy was slightly higher in the control group than in the CQI group. Glomerulonephritis and diabetic nephropathy were both diagnosed clinically and not by renal biopsy.
TABLE 1.
Patients Characteristics at Baseline

Peritonitis Rate
In the first year after implementation of the CQI program, the peritonitis incidence had improved to 1 episode in 30.1 patient-months from 1 episode in 22.2 patient-months in the control group (p > 0.05, Figure 2). The incidences in years 2 and 3 were 1 episode in 71.1 and 77.3 patient-months in the CQI group and 1 episode in 22.6 and 22.9 patient-months in the control group (p < 0.01 for the CQI group in both years).
Figure 2 —
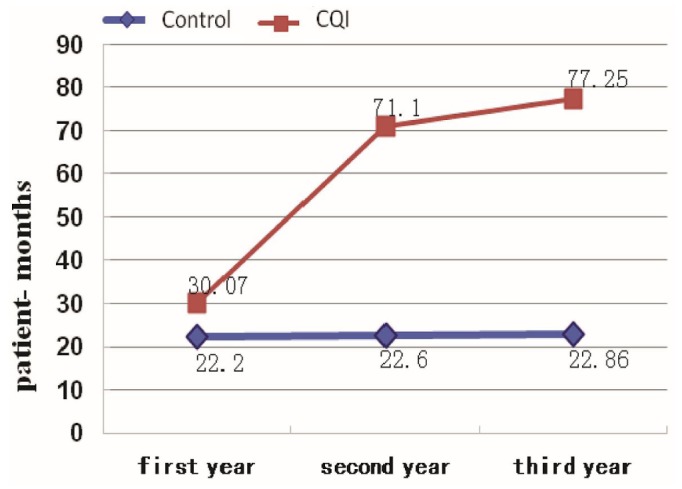
Peritonitis rates, first three years, by study group.
Cardiac Morphology
In the CQI group, no statistically significant change in cardiac morphology occurred during the 3-year monitoring period. However, in the control group, the cardiothoracic ratio (0.55 ± 0.08), interventricular septal thickness (11.07 ± 1.66 mm), and left ventricular wall thickness (10.79 ± 1.47 mm) were all significantly increased compared with values observed at the start of dialysis (0.51 ± 0.05, 10.25 ± 1.38 mm, and 9.38 ± 1.06 mm respectively; all p < 0.05).
Patient and Technique Survival Rates
Figures 3 and 4 show patient and technique survival rates. Patient survival in the CQI group at 1, 2, and 3 years was 97.3%, 96.3%, and 96.3% respectively, significantly higher (p < 0.001) than in the control group (92.6%, 82.4%, and 67.3%). Technique survival at 1, 2, and 3 years was also significantly higher in the CQI group than in the control group: 95.6% versus 89.6%, 92.6% versus 79.2%, and 92.6% versus 76.8% respectively (p < 0.001).
Figure 3 —
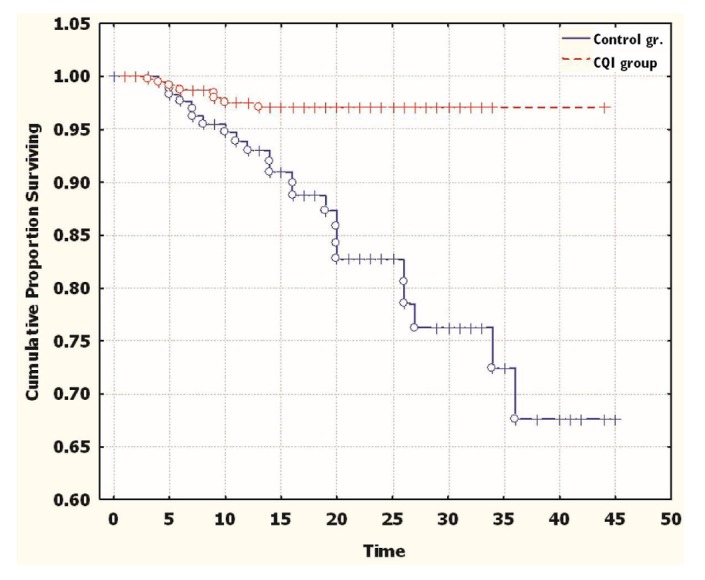
Patient survival by the Kaplan-Meier method (p = 0.00146). CQI = continuous quality improvement.
Figure 4 —
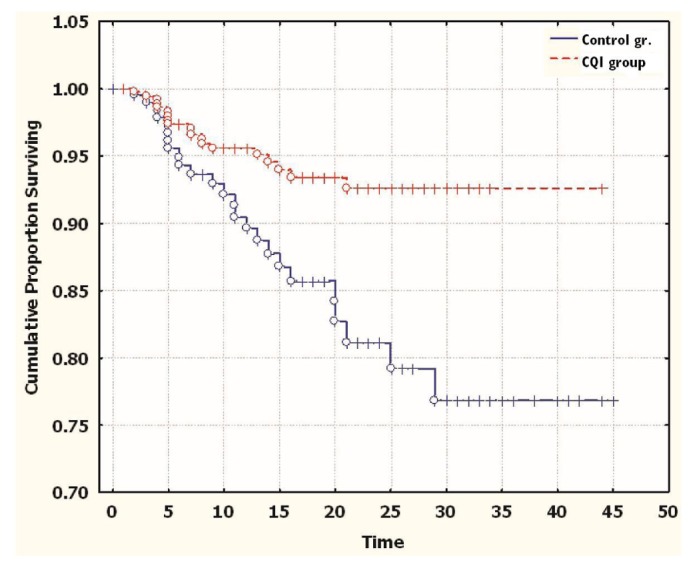
Technique survival by the Kaplan-Meier method (p = 0.0014). CQI = continuous quality improvement.
Table 2 summarizes the causes of death and drop-out. The number of patients with fatal cardio- or cerebrovascular complications was significantly lower in the CQI group than in the control group (p < 0.001). Cardio- or cerebrovascular complications accounted for 50% of deaths in the CQI group and for 60.9% of deaths in the control group.
TABLE 2.
Causes of Death and Technique Failure in the Patient Groups
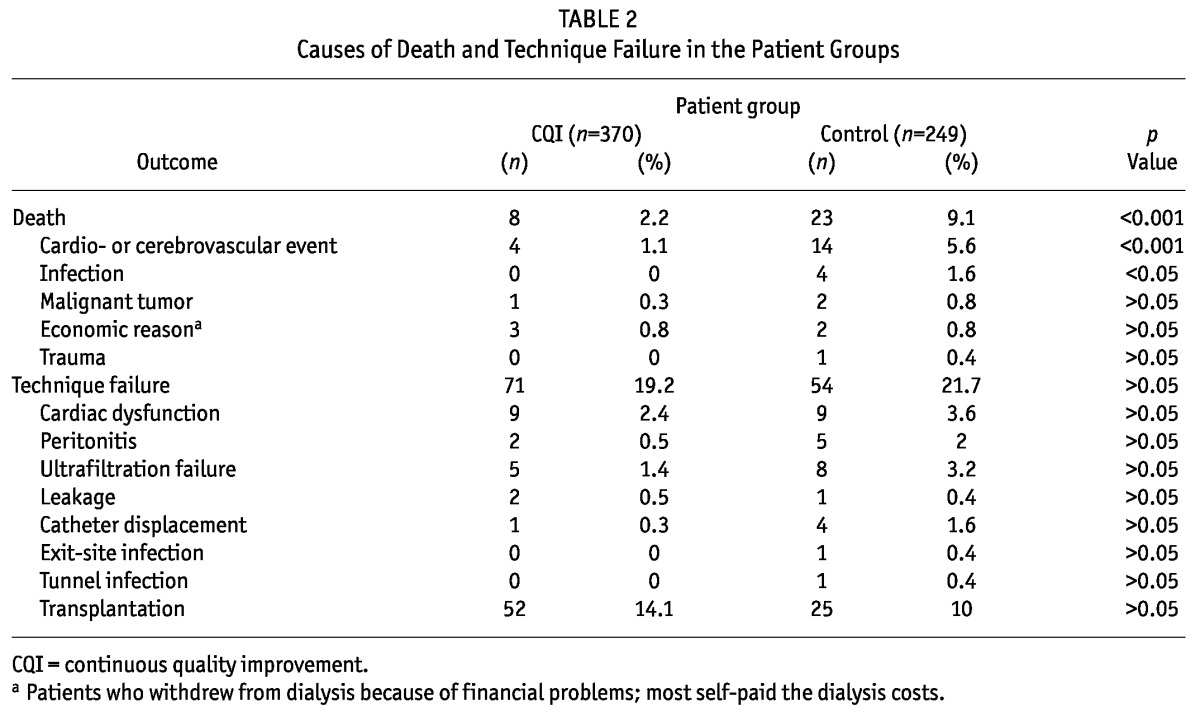
Further analysis showed that cardio- and cerebrovascular complications accounted for 47.4% of technique failures in the CQI group and for 31% in the control group (Table 2) Peritonitis accounted for 10.5% of technique failures in the CQI group and for 17.2% in the control group. Those differences were not statistically significant.
Discussion
Although PD has been used in China for more than 30 years, the rate of uptake for the technique lags far behind that of HD. The difference is related not only to financial factors and medical policy, but also to a lack of advancement in PD management.
Based on data provided by Baxter Healthcare, there were, at the end of March 2012, fewer than 30 PD centers in China managing more than 200 patients. Reports from 13 of the Chinese centers showed that 1-year patient and technique survival were about 82% and 88.7% respectively in 2007 (5). Data from our center during 2005 - 2007 (the control group) showed similar patient and technique survival rates, which were markedly lower than the rates achieved in Europe, Japan, Korea, and Hong Kong (1,6-8). It has been reported that patient and technique survival rates are higher in larger centers than in smaller centers and that the PD drop-out rate is negatively correlated with the size of the PD program (3,5).
A key impediment to the improvement of PD quality in our unit before 2008 was the lack of individually designed PD prescriptions, which affected patient compliance. Other problems included incoherence of care and training between the ward and the clinic, and lack of a PD quality evaluation system. Moreover, after the patient was discharged from hospital, health care was provided by a different physician, which further hampered the identification of problems and made implementation of an appropriate management plan more difficult.
To address those issues, we established a dedicated PD center in 2008. We used the CQI concept to improve the quality of PD provided to patients. The specific procedures we used were assembling a core team, assigning responsibilities to the team members, and monitoring their progress. To that end, we identified workflow issues, defined criteria for evaluation, and made every team member independently responsible for specific issues. We also established an evaluation system based on workload data and monthly group discussion of quality issues.
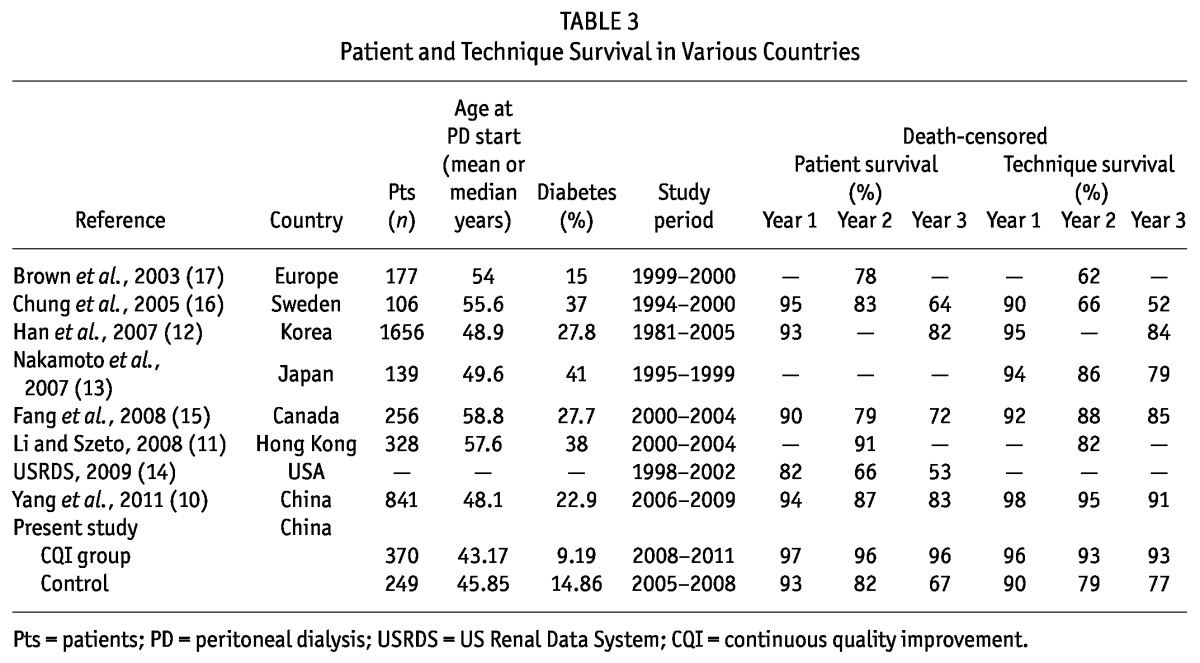
Our results indicate that drop-out from PD during the period 2005 - 2008 was most commonly a result of cardio- or cerebrovascular complications and peritonitis. Those two factors were also the leading causes of death. Further analysis of the data showed that drop-out was closely correlated with inadequate control of blood pressure and lack of guidance on dietary sodium intake. Those issues were addressed with training and retraining programs that also included standardization of sodium intake, prescription of loop diuretics and antihypertensive agents, and provision of clean “PD clothes” to all patients. Those measures resulted in noticeable improvements in blood pressure control, cardiac pathology, and procedural key performance indicators. The most important outcome of our CQI program was that the rate of drop-out from PD was reduced to 16%, suggesting that optimized management can play a key role in improving the quality of PD. In parallel, the patient and technique survival rates increased markedly in response to CQI initiatives aimed at reducing cardio- and cerebrovascular complications and peritonitis. As Table 3 shows, our current patient and technique survival rates are comparable to those reported by advanced PD centers in other countries (9-16).
TABLE 3.
Patient and Technique Survival in Various Countries
Summary
Implementing CQI at a PD center can optimize management procedures and significantly improve dialysis outcomes.
Disclosures
The authors have no financial conflicts of interest to disclose.
Acknowledgments
The authors express their appreciation to Dr. Anders Tranæus for valuable comments on this manuscript.
REFERENCES
- 1. Li PK, Law MC, Chow KM, Leung CB, Kwan BC, Chung KY, et al. Good patient and technique survival in elderly patients on continuous ambulatory peritoneal dialysis. Perit Dial Int 2007; 27(Suppl 2):S196–201 [PubMed] [Google Scholar]
- 2. Ersoy FF. Improving technique survival in peritoneal dialysis: what is modifiable? Perit Dial Int 2009; 29(Suppl 2):S74–7 [PubMed] [Google Scholar]
- 3. Afolalu B, Troidle L, Osayimwen O, Bhargava J, Kitsen J, Finkelstein FO. Technique failure and center size in a large cohort of peritoneal dialysis patients in a defined geographic area. Perit Dial Int 2009; 29:292–6 [PubMed] [Google Scholar]
- 4. Sipahi I, Swaminathan A, Natesan V, Debanne SM, Simon DI, Fang JC. Effect of antihypertensive therapy on incident stroke in cohorts with prehypertensive blood pressure levels: a meta-analysis of randomized controlled trials. Stroke 2012; 43:432–40 [DOI] [PubMed] [Google Scholar]
- 5. Jiang Z, Yu X. Advancing the use and quality of peritoneal dialysis by developing a peritoneal dialysis satellite center program. Perit Dial Int 2011; 31:121–6 [DOI] [PubMed] [Google Scholar]
- 6. Mujais S, Story K. Peritoneal dialysis in the US: evaluation of outcomes in contemporary cohorts. Kidney Int Suppl 2006; (103):S21–6 [DOI] [PubMed] [Google Scholar]
- 7. Sipahioglu MH, Aybal A, Unal A, Tokgoz B, Oymak O, Utas C. Patient and technique survival and factors affecting mortality on peritoneal dialysis in Turkey: 12 years' experience in a single center. Perit Dial Int 2008; 28:238–45 [PubMed] [Google Scholar]
- 8. Han SH, Lee JE, Kim DK, Moon SJ, Kim HW, Chang JH, et al. Long-term clinical outcomes of peritoneal dialysis patients: single center experience from Korea. Perit Dial Int 2008; 28(Suppl 3):S21–6 [PubMed] [Google Scholar]
- 9. Yang X, Mao HP, Guo QY, Yu XQ. Successfully managing a rapidly growing peritoneal dialysis program in Southern China. Chin Med J (Engl) 2011; 124:2696–700 [PubMed] [Google Scholar]
- 10. Li PK, Szeto CC. Success of the peritoneal dialysis programme in Hong Kong. Nephrol Dial Transplant 2008; 23:1475–8 [DOI] [PubMed] [Google Scholar]
- 11. Han SH, Lee SC, Ahn SV, Lee JE, Choi HY, Kim BS, et al. Improving outcome of CAPD: twenty-five years' experience in a single Korean center. Perit Dial Int 2007; 27:432–40 [PubMed] [Google Scholar]
- 12. Nakamoto H, Kawaguchi Y, Suzuki H. Is technique survival on peritoneal dialysis better in Japan? Perit Dial Int 2006; 26:136–43 [PubMed] [Google Scholar]
- 13. United States, Department of Health and Human Services, National Institutes of Health, National Institute of Diabetes and Digestive and Kidney Diseases, US Renal Data System (USRDS). 2009 Annual Data Report. 2 vols Bethesda, MD: USRDS; 2009. [Google Scholar]
- 14. Fang W, Qian J, Lin A, Rowaie F, Ni Z, Yao Q, et al. Comparison of peritoneal dialysis practice patterns and outcomes between a Canadian and a Chinese centre. Nephrol Dial Transplant 2008; 23:4021–8 [DOI] [PubMed] [Google Scholar]
- 15. Chung SH, Heimbürger O, Lindholm B, Lee HB. Peritoneal dialysis patient survival: a comparison between a Swedish and a Korean centre. Nephrol Dial Transplant 2005; 20:1207–13 [DOI] [PubMed] [Google Scholar]
- 16. Brown EA, Davies SJ, Rutherford P, Meeus F, Borras M, Riegel W, et al. Survival of functionally anuric patients on automated peritoneal dialysis: the European APD Outcome Study. J Am Soc Nephrol 2003; 14:2948–57 [DOI] [PubMed] [Google Scholar]


