Abstract
Objective
Examine the hazard of incident and progressive radiographic OA (rOA) and chronic joint symptoms at the hip and knee by limb length inequality (LLI) in a large, community-based sample.
Methods
A longitudinal cohort completed baseline (1991–1997) clinical evaluation and identical follow-up assessment (1999–2003) (median follow-up time = 5.9 years, range=3.0–13.1 years). LLI was defined at baseline as a measured difference between limbs of ≥ 2 cm. The study groups with LLI data comprised 1,583 participants with paired (baseline and follow-up) knee radiographs and 1,453 participants with paired hip radiographs. Multivariable Cox regression models were used to examine the hazard of incident and progressive knee and hip rOA and chronic joint symptoms, while adjusting for demographic and clinical factors.
Results
The hazard of developing incident knee or hip rOA was 20–30% higher and of developing progressive knee or hip rOA was 35–83% higher among participants with LLI, but results were only statistically significant for progressive knee rOA (adjusted hazard ratio = 1.83, 95% confidence interval = 1.10–3.05). The hazards of progressive chronic knee symptoms and incident and progressive chronic hip symptoms were 13–59% higher among participants with LLI, but were not statistically significant.
Conclusion
LLI was associated with progressive knee rOA and was non-significantly associated with incident knee or hip rOA and progressive hip rOA, progressive chronic knee symptoms, and incident and progressive chronic hip symptoms. Longer studies may strengthen these associations and help determine whether LLI is a risk factor or marker of these outcomes.
Introduction
Osteoarthritis (OA) is a leading cause of disability among older adults, with lower extremity OA limiting mobility, basic daily activities, and quality of life1–3. Chronic joint symptoms, including joint pain, aching, and stiffness, also may contribute to impaired daily function and quality of life. The prevalence of OA and chronic joint symptoms is high in the United States adult population. In the United States, approximately 33% of persons over the age of 63 years have knee OA and at least 3% ages 55–74 have hip OA4. After adjusting for age, an estimated 29.2% of the 2006 civilian noninstitutionalized adult population reported chronic joint symptoms during the prior 30 days5.
Radiographic OA (rOA) and chronic joint symptoms of the lower extremity may be caused by or exacerbated by injuries, chronic joint disorders, and mechanical and anatomical factors, such as obesity, joint malalignment, and joint instability6–9. Limb length inequality (LLI), a condition in which paired lower extremities are of unequal length, has been suggested as another mechanical factor that may contribute to the development or progression of lower extremity rOA and chronic joint symptoms. In the Johnston County Osteoarthritis Project, a community-based sample of African American and Caucasian men and women, LLI was associated with prevalent rOA and chronic joint symptoms of the knee and hip in cross-sectional analyses10, 11, but it is unknown whether LLI precedes rOA or chronic joint symptoms of the lower extremity, potentially contributing to a greater incidence or accelerated progression of these outcomes. This may occur because individuals with LLI might functionally minimize the inequality by increasing knee flexion or hip adduction of the longer limb12, thus altering movement patterns that may amplify forces across lower extremity joints and contribute to the degradation of cartilage that characterizes rOA13.
One method of determining whether LLI may be a predictor of lower extremity rOA or chronic joint symptoms is to examine the incidence of these outcomes among individuals with and without LLI. The same method could determine whether LLI may be a predictor of progression among those with these conditions at baseline. The purpose of this analysis was to compare the hazard of incident and progressive rOA of the knee or hip between individuals with LLI and those without LLI in a large community-based sample. Additionally, the hazard of incident and progressive chronic joint symptoms (i.e., pain, aching and stiffness of the joint on most days) of the knee and hip between individuals with LLI and those without LLI was examined, adjusting for the presence of rOA.
Methods
Study Participants
The Johnston County Osteoarthritis Project is an ongoing, community-based study of the occurrence of knee and hip OA in African American and Caucasian residents in a rural county in North Carolina. Details of this study have been reported previously14. Briefly, this study involves civilian, non-institutionalized adults aged 45 years and older who resided in six townships in Johnston County. Participants were recruited by probability sampling, with over-sampling of African Americans. A total of 3,187 individuals were recruited at baseline (T0) between May 1991 and December 1997 and completed a clinical evaluation14. 1,329 participants were not eligible due to lack of data at follow-up (T1) for the following reasons: emigration from study area (N=161), refusal (N=435), inability to participate due to physical or mental conditions (N=234), death (N=411), and inability to be contacted or found (N=88). Assessments of 1868 participants at T1 were completed from 1999–2003 (median time from T0 to T1 = 5.6 years, range=3.0–13.1 years). Paired T0 and T1 knee and hip radiograph assessments were available for 1,726 participants. LLI data were collected for 3,067 participants at T0 and were available for 1,558 participants with paired knee radiographs and 1,413 participants with paired hip radiographs.
Limb Length Measurement
With the participant supine, a tape measure was used to determine right and left lower extremity lengths (in centimeters) between two defined bony landmarks: the anterior superior iliac spine (ASIS) and the medial malleolus. An intertester reliability of r = 0.98 and an intratester reliability from r = 0.89 to 0.95 has been reported with this measurement technique15. To account for potential measurement error in this clinical measurement, LLI was defined conservatively as a 2.0 cm or greater difference in length between limbs. Additionally, a cutpoint of 1.0 cm was explored to compare with the estimates obtained by the 2.0 cm conservative definition.
Radiographic Assessment
All participants completed bilateral standing anteroposterior radiography of the knee. Women over 50 years of age and all men completed supine anteroposterior pelvic radiography. Radiographs were rated by a single musculoskeletal radiologist (JBR) using the Kellgren-Lawrence (K-L) radiographic atlas for overall knee and hip radiographic grades16. As previously described, interrater reliability (comparison of radiograph readings between JBR and another radiologist) and intrarater reliability (comparison of radiograph readings completed by JBR at two separate times) for the radiologist were high (weighted kappa for interrater reliability 0.9; kappa for intrarater reliability 0.9)14. Radiographs without the features of OA were defined as K-L grade of 0 (normal findings). A minute radiographic osteophyte of doubtful pathologic significance was assigned a K-L grade of 1 (questionable). Radiographs showing an osteophyte without joint space narrowing were assigned a K-L grade of 2 (mild). A moderate decrease of the joint space was assigned a K-L grade of 3 (moderate). K-L grade 4 (severe) was defined as severe joint space narrowing with subchondral bone sclerosis17. The incidence of rOA was defined as a K-L grade ≥2 at T1 among participants with K-L grade <2 at T0. Progression of rOA was defined two ways: 1) an increase of at least 1 K-L grade from T0 to T1 among individuals with at least K-L grade of 1 at T0, and 2) an increase of at least 1 K-L grade from T0 to T1 among individuals with at least K-L grade of 2 at T0.
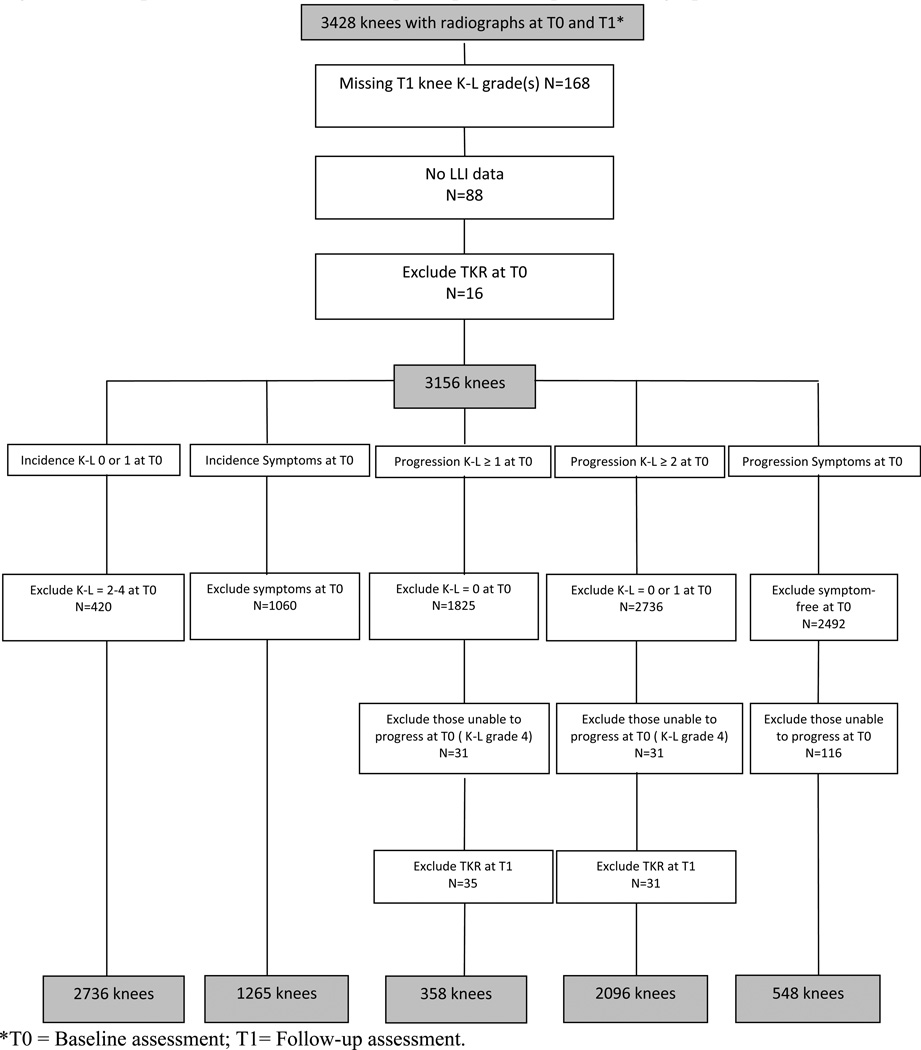
Figures 1 and 2 detail the selection of knee or hip joints for analyses. Of the 3,428 knees with radiographs, knees that did not have K-L grades available at both T0 and T1 (n=168) or had undergone a total knee replacement (TKR) prior to T0 (n=16) were excluded. Of the 3,440 hips with radiographs, hips that did not have K-L grades available at both T0 and T1 (n=495) or had undergone a total hip replacement (THR) prior to T0 (n=16) were excluded.
Figure 1. Description of knees from N=1726 participants with paired radiographs.
*T0 = Baseline assessment; T1= Follow-up assessment.
Figure 2. Description of hips for analysis from N=1726 participants with paired radiographs.
*T0 = Baseline assessment; T1= Follow-up assessment.
Chronic Knee and Hip Symptoms
Participants completed an interviewer-administered questionnaire in which they answered “Yes” or “No,” separately for left and right knees and left and right hips, to the question: “On most days do you have pain, aching or stiffness in your [left/right] [knee/hip]?” The presence of groin pain was recorded for right and left sides. Participants were considered to have chronic knee symptoms if they answered affirmatively to the knee symptoms question and to have chronic hip symptoms if they answered affirmatively to the hip symptoms question or reported groin pain. Participants who provided affirmative answers to the chronic joint symptoms question were asked to grade the severity: “Is the pain, aching or stiffness in your [left/right] [knee/hip] mild, moderate, or severe?”
The incidence of chronic joint symptoms was defined as an affirmative response to the symptoms questions at T1 among participants who reported no symptoms at T0. Progression of symptoms was defined as an increase of at least 1 level of severity from T0 to T1 among individuals who reported mild or moderate symptoms at T0.
Demographic and Clinical Characteristics
The following participant characteristics were included as covariates in our analyses because they have been associated with knee and / or hip rOA: gender; self-reported race (African American or Caucasian); age (continuous variable in years); history of knee joint problems among those with knee outcomes (i.e., knee injury [“Have you ever injured your right/left knee?”], knee fracture [“Has a doctor ever told you that you had broken or fractured your right/left knee?”], and knee surgery [“Have you ever had surgery on your right/ left knee?”]); history of hip joint problems among those with hip outcomes (i.e., congenital hip problem [“Has a doctor ever told you that you had a problem with your right/left hip from birth or childhood?”], hip injury [“Have you ever injured your right/left hip?”], hip fracture [“Has a doctor ever told you that you had broken or fractured your right/left hip?”], and hip surgery [“Have you ever had surgery on your right/left hip?”]); and body mass index at baseline (BMI: continuous variable calculated as weight in kilograms/height in meters squared). Height without shoes was measured in centimeters and weight was measured in kilograms using a balance beam scale.
Statistical Analysis
The unit of analysis was the joint (not the person). Chi-square and t-tests were used to compare gender, race, baseline age, baseline BMI, baseline height, history of knee or hip joint problems, rOA at T0 and T1, and chronic symptoms at T0 and T1 between groups with and without LLI. Because of the wide range of follow-up times for participants (mean = 5.9 years; standard deviation ± 1.4 years; range= 3.0 – 13.2 years) and interval censoring (i.e., when the precise time of the occurrence of the outcome is unknown), separate multivariable Cox regression models (with the midpoint of each individual’s follow-up period as the approximated endpoint among those with the outcome of interest) with generalized estimating equations to account for correlated data (paired joints within same person) were used to estimate hazard ratios of knee or hip rOA outcomes and knee or hip symptoms outcomes by LLI status (LLI versus no LLI) and in comparisons of the shorter and longer limbs versus limbs without LLI. Estimates from the Cox models were compared with those from parametric Weibull time-to-event models to determine whether the endpoint assumption used with the Cox model was reasonable. The Weibull model accommodates variable follow-up times and allows for estimation of the time-to-event when interval censoring is present18. We chose to report the Cox model estimates because the Cox model is more widely used and understood than the Weibull model. Covariates included in adjusted models were identified by their association with both the exposure of LLI and outcome of rOA or joint symptoms, either based on statistical significance in bivariate associations or on prior Johnston County OA studies of each covariate in the LLI and OA/symptoms association. Using a forward selection strategy, any statistically significant interaction terms of LLI with the other covariates were considered for inclusion. A sensitivity analysis was conducted exploring a LLI definition using a cutpoint of 1 cm. Statistical computations were performed using SAS Version 9.1 software (SAS Institute, Cary, NC) and Stata/IC 10.1 software (Stata Corporation, College Station, TX). Statistical significance was evaluated at the p < 0.05 level.
Results
Characteristics of the sample are detailed in Table 1. The total study group comprised 1,583 participants with paired knee radiographs and LLI data (64.3% female, 27.0% African American) and 1,453 participants with paired hip radiographs and LLI data (61.4% female, 26.8% African American). Ninety participants (5.7%) had an LLI ≥ 2 cm among those with paired knee radiographs, and 78 (5.4%) had an LLI ≥ 2 cm among those with hip radiographs. A history of joint problems was more common for the knee (18.1% among those with paired knee radiographs) than for the hip (7.0% among those with paired hip radiographs). The proportion of participants reporting a history of knee problems at baseline was statistically higher among those with LLI than without LLI (26.1% versus 17.7%, p=0.04). Proportionally more participants reported a history of hip problems at baseline among those with LLI than without LLI (10.3% versus 6.8%, p=0.24), although this difference was not statistically significant. Presence of rOA was less at T0 than T1 for both the knee (18.6% and 33.0%) and the hip (31.4% and 38.5%) among those with paired radiographs. Presence of chronic knee symptoms was slightly higher at T0 than T1 (42.1% and 38.6%) among those with paired knee radiographs; presence of chronic hip symptoms was less at T0 than T1 (34.5% and 50.6%) among those with paired hip radiographs.
Table 1.
Characteristics of Sample, by LLI and Joint Site.
| Participants with Paired Knee Radiographs | Participants with Paired Hip Radiographs | |||||||
|---|---|---|---|---|---|---|---|---|
| Total Sample (N=1583) |
LLI* (N=90) | No-LLI* (N=1493) |
P-value | Total Sample (N=1453) |
LLI* (N=79) |
No-LLI* (N=1374) |
P-value | |
| Female (%) | 64.3 | 64.4 | 64.2 | 0.97 | 61.4 | 60.8 | 61.4 | 0.91 |
| Black (%) | 27.0 | 34.4 | 26.5 | 0.10 | 26.8 | 34.2 | 26.4 | 0.13 |
| History of Joint Problem†(%) | 18.1 | 26.1 | 17.7 | 0.04 | 7.0 | 10.3 | 6.8 | 0.24 |
| rOA‡ at T0§ (%) | 18.6 | 42.2 | 17.2 | <0.01 | 31.4 | 31.7 | 31.4 | 0.96 |
| rOA‡ at T1** (%) | 33.0 | 53.4 | 31.8 | <0.01 | 38.5 | 43.6 | 38.2 | 0.34 |
| Joint Symptoms‡ at T0§ (%) | 42.1 | 54.6 | 41.4 | 0.02 | 38.4 | 40.5 | 38.3 | 0.50 |
| Joint Symptoms‡ at T1** (%) | 38.6 | 43.3 | 38.3 | 0.37 | 50.6 | 67.1 | 49.7 | <0.01 |
| Baseline Age (mean (SD)) | 60.9 (±10.0) | 62.1 (±10.2) | 60.8 (±10.3) | 0.24 | 61.9 (±9.6) | 64.0 (±9.4) | 61.8 (±9.6) | 0.05 |
| Baseline BMI (mean kg/m2 (SD)) | 29.1 (±5.6) | 31.1 (±7.9) | 29.0 (±5.7) | 0.01 | 29.1 (±5.6) | 30.6 (±7.4) | 29.0 (±5.5) | 0.06 |
| Baseline Height (cm (SD)) | 166.4 (±9.3) | 166.0 (±9.7) | 166.4 (±9.3) | 0.75 | 166.6(±9.5) | 166.5 (±9.9) | 166.6(±9.5) | 0.89 |
LLI = limb length inequality
History of joint problem: Among participants with paired knee radiographs = history of injury, fracture, or surgery of the knee; among participants with paired hip radiographs = history of injury, fracture, surgery, or congenital problem of the hip.
rOA= radiographic OA; among participants with paired knee radiographs refers to knee joint, among participants with paired hip radiographs refers to hip joint
T0: Baseline assessment
T1: Follow-up assessment
Baseline age, BMI, gender, race, and history of joint symptoms were included in all adjusted models, and rOA also was controlled for in models predicting chronic symptoms outcomes. Height was explored as a covariate, but it yielded little (<6%) to no change in the estimate when compared to models with other key covariates. Thus, height was not considered an important confounder in analyses and was not included in final adjusted models.
The hazard of developing incident knee or hip rOA was 20–30% higher among participants with LLI compared to those without LLI, but these results were not statistically significant before or after adjustment (Table 2). Participants with a LLI were 83% more likely to have progressive knee rOA and 34% more likely to have progressive hip rOA, but these results were only statistically significant for progressive knee rOA (adjusted hazard ratio[HR] = 1.83, 95% confidence interval [CI] = 1.10–3.05; Table 2). The hazard of progressive chronic knee symptoms and incident was higher among participants with LLI than those without LLI in unadjusted and adjusted models, but this association was not statistically significant (Table 2). A reverse relationship was noted with incident chronic knee symptoms in unadjusted models; participants with a LLI were less likely to develop incident symptoms than those without LLI, but this association was attenuated in adjusted models and was not statistically significant. No statistically significant interaction terms were observed between LLI and baseline age, baseline BMI, history of joint problems, gender, and race in the knee or hip models. Weibull models produced similar point estimates and 95% CIs to Cox models for incident outcome models, but estimates were closer to the null in Weibull models than in Cox models (data not shown). Attempts to explore whether LLI predicted the development of unilateral or bilateral incident knee or hip rOA were underpowered and uninformative.
Table 2.
Unadjusted and Adjusted Hazard Ratios (HR) of Radiographic OA (rOA) and Chronic Symptoms Outcomes, by Joint Site.
| LLI* Present? |
# of Joints at Risk |
# of Joints with Outcome |
Unadjusted HR (95% CI†) |
Adjusted‡ HR (95% CI†) |
|
|---|---|---|---|---|---|
| Incident Knee rOA | Yes | 122 | 20 | 1.20 (0.72–2.00) | 1.08 (0.66–1.76) |
| No | 2612 | 398 | |||
| Progressive Knee rOA 1§ | Yes | 85 | 37 | 1.70 (1.15–2.51) | 1.22 (0.82–1.80) |
| No | 1197 | 405 | |||
| Progressive Knee rOA 2** | Yes | 47 | 24 | 2.84 (1.72–4.69) | 1.83 (1.10–3.05) |
| No | 328 | 148 | |||
| Incident Knee Symptoms | Yes | 98 | 18 | 0.68 (0.42–1.09) | 0.83 (0.47–1.47) †† |
| No | 1998 | 463 | |||
| Progressive Knee Symptoms | Yes | 50 | 18 | 1.19 (0.66–2.15) | 1.13 (0.53–2.39) †† |
| No | 510 | 195 | |||
| Incident Hip rOA | Yes | 119 | 12 | 1.27 (0.72–2.23) | 1.17 (0.66–2.07) |
| No | 1898 | 187 | |||
| Progressive Hip rOA 1§ | Yes | 130 | 16 | 1.63 (0.96–2.76) | 1.32 (0.78–2.22) |
| No | 2305 | 189 | |||
| Progressive Hip rOA 2** | Yes | 33 | 4 | 2.11 (0.60–7.37) | 1.34 (0.37–4.83) |
| No | 629 | 36 | |||
| Incident Hip Symptoms | Yes | 142 | 69 | 1.20 (0.90–1.60) | 1.21 (0.82–1.77) †† |
| No | 2572 | 968 | |||
| Progressive Hip Symptoms | Yes | 22 | 7 | 1.15 (0.46–2.85) | 0.95 (0.23–3.94) †† |
| No | 295 | 117 | |||
LLI = limb length inequality
CI= confidence interval
Adjusted for baseline age, baseline BMI, gender, race, and joint problems (i.e., injury, surgery, or fracture).
An increase of at least 1 K-L grade from T0 assessment to T1 assessment among individuals with at least K-L grade of 1 at T0.
An increase of at least 1 K-L grade from T0 assessment to T1 assessment among individuals with at least K-L grade of 2 at T0.
Adjusted for baseline age, baseline BMI, gender, race, joint problems in same joint, and OA (presence of K-L grade of at least 2) in same joint.
In sensitivity analyses exploring a LLI cutpoint of 1 cm, the pattern of the hazard ratios (data not shown) were typically closer to the null compared to those displayed in Table 2 for a LLI cutpoint of 2 cm. An inverse relationship was noted for incident knee rOA and progressive hip rOA 2 outcomes with the LLI cutpoint of 1 cm. The hazards of incident knee and hip symptoms were higher among participants with a baseline LLI ≥ 1 cm than compared to those with a LLI < 1 cm (incident knee symptoms adjusted HR = 1.21, 95% CI = 0.95–1.53); incident hip symptoms HR = 1.14, 95% CI =0.92–1.41).
Table 3 displays the hazard of each knee and hip outcome for the shorter limb versus those without LLI and for the longer limb versus those without LLI. The hazard of developing incident knee or hip rOA was 35–51% higher in the shorter limb compared to limbs without LLI, but these results were not statistically significant before or after adjustment (Table 3). Incident knee or hip rOA was less likely in the longer limb than in limbs without LLI (Table 3). Participants with a shorter limb were twice as likely to have progressive knee rOA (adjusted HR=2.04, 95% CI 1.12–3.70; Table 3). Participants with a longer limb were 75% more likely to have progressive knee rOA, but these results were not statistically significant (Table 3). Interpretation of the results for the knee and hip outcomes is limited due to low numbers of events.
Table 3.
Adjusted Hazard Ratios (HR) of Radiographic OA (rOA) and Chronic Symptoms Outcomes --Shorter Limb and Longer Limb versus No LLI.
| No LLI* | Shorter Limb | Longer Limb | |
|---|---|---|---|
| Incident Knee rOA | |||
| Knees with outcome/knees at risk | 398/2612 | 13/63 | 7/59 |
| Adjusted HR (95%CI†) | 1.00 (reference) | 1.35 (0.77–2.35) | 0.79 (0.37–1.67) |
| Progressive Knee rOA 1§ | |||
| Knees with outcome/knees at risk | 405/1197 | 20/42 | 17/43 |
| Adjusted OR (95%CI) | 1.00 (reference) | 1.40 (0.89–2.20) | 1.12 (0.69–1.82) |
| Progressive Knee rOA 2** | |||
| Knees with outcome/knees at risk | 148/596 | 12/23 | 11/24 |
| Adjusted OR (95%CI) | 1.00 (reference) | 2.04 (1.12–3.70) | 1.75 (0.94–3.23) |
| Incident Knee Symptoms | |||
| Knees with outcome/knees at risk | 463/1998 | 10/51 | 8/47 |
| Adjusted OR (95%CI) | 1.00 (reference) | 0.87 (0.45–1.68) | 0.78 (0.37–1.65) |
| Progressive Knee Symptoms | |||
| Knees with outcome/knees at risk | 195/510 | 11/26 | 7/24 |
| Adjusted OR (95%CI) | 1.00 (reference) | 2.50 (0.86–7.27) | 1.90 (0.57–6.35) |
| Incident Hip rOA | |||
| Hips with outcome/hips at risk | 187/1898 | 9/62 | 3/57 |
| Adjusted HR (95%CI†) | 1.00 (reference) | 1.51 (0.74–3.11) | 0.61 (0.19–1.91) |
| Progressive Hip rOA 1§ | |||
| Hips with outcome/hips at risk | 189/2305 | 8/69 | 8/61 |
| Adjusted OR (95%CI) | 1.00 (reference) | 1.35 (0.68–2.68) | 1.30 (0.60–2.83) |
| Progressive Hip rOA 2** | |||
| Hips with outcome/hips at risk | 36/629 | 4/19 | 0/14 |
| Adjusted OR (95%CI) | 1.00 (reference) | 3.75 (1.26–11.13) | -- |
| Incident Hip Symptoms | |||
| Hips with outcome/hips at risk | 968/2572 | 35/71 | 34/71 |
| Adjusted OR (95%CI) | 1.00 (reference) | 1.22 (0.77–1.93) | 1.19 (0.73–1.93) |
| Progressive Hip Symptoms | |||
| Hips with outcome/hips at risk | 149/363 | 3/9 | 6/13 |
| Adjusted OR (95%CI) | 1.00 (reference) | 0.97 (0.13–7.46) | 0.94 (0.23–3.93) |
LLI = limb length inequality
CI= confidence interval
Adjusted for baseline age, baseline BMI, gender, race, and joint problems (i.e., injury, surgery, or fracture).
An increase of at least 1 K-L grade from T0 assessment to T1 assessment among individuals with at least K-L grade of 1 at T0.
An increase of at least 1 K-L grade from T0 assessment to T1 assessment among individuals with at least K-L grade of 2 at T0.
Adjusted for baseline age, baseline BMI, gender, race, joint problems in same joint, and OA (presence of K-L grade of at least 2) in same joint.
Discussion
The hazard of incident and progressive knee or hip rOA and chronic joint symptoms was higher among participants with LLI than those without LLI for almost all outcomes examined, but results were only statistically significant for the outcome of progressive knee rOA (an increase of at least 1 K-L grade from T0 to T1 assessment among individuals with at least K-L grade of 2 at T0). Previous cross-sectional reports examining data from the Johnston County OA Project demonstrated associations between LLI and OA and LLI and chronic joint symptoms, which were statistically significant at the knee but not at the hip10, 11. Our ability to identify positive though non-significant associations for many of these slowly developing outcomes in just the average 4–7 year follow-up suggests that longer follow-up may produce stronger findings.
Among participants with at least a K-L grade of 2 in one knee at baseline, the hazard of progressive knee rOA was significantly higher among those with a LLI ≥ 2 cm versus < 2 cm when controlling for key covariates, but this result has at least two interpretations. One interpretation is that LLI causes faster progression of knee rOA. However, changes in the knee joint (e.g., joint contractures, development of frontal plane malalignment) from knee rOA may contribute to a LLI, and as a result LLI could be a marker, rather than a predictor, of more rapid progression of knee rOA due to other causes. In this dataset, the physical factors contributing to each participants’ LLI is not known, nor is it known whether the individuals with LLI who exhibited more rapid progression of knee rOA had a LLI prior to the onset of their radiographic disease.
The estimates for incident knee rOA, incident hip rOA, and progressive knee symptoms were higher for the shorter limb versus limbs without LLI than the longer limb versus limbs without LLI. Few knees and hips had these outcomes, and thus, adequate power was not available to clearly determine whether OA outcomes are more common in the longer or shorter limb. Harvey et al.19 reported that shorter limbs were at high risk (adjusted odds ratio 1.3, 95% CI 1.0–1.7) for progressive knee rOA, but they did not find an elevated risk for incident knee rOA in either the shorter or longer limb over a 30 month period. Their results suggested a pattern of knee rOA outcomes occurring more often in the shorter limb than the longer limb.
LLI may be more strongly associated with rOA of the knee and hip in cross-sectional analyses than in longitudinal analyses, as seen in this study population, because lower extremity rOA may predict LLI. Possibly, degeneration of the knee or hip joint from OA would be accompanied by the progressive development of joint contractures and alterations in symmetry between limbs that ultimately would make one limb appear shorter than the other. Alternatively, there may be a cyclical pattern for the development and progression of LLI and rOA in which each condition contributes to the advancement of the other, making them strongly associated but neither is a strong predictor of the other.
There are several limitations of the study. First, the follow-up time of 5.9 years on average may not have been adequate time for the outcomes of interest to develop or progress. However, this follow-up time is longer than the only other published longitudinal study on the association between LLI and knee OA, which had a 30 month follow-up period19. Second, the study results may be biased due to loss to follow-up. Third, our method for measuring LLI is another limitation. Tape measurement is highly accurate between testers when compared to supine radiography, but is less reliable compared to standing radiographs12, 20. Sources of error with tape measurement include difficulty with accurately placing the tape measure on identical bilateral bony landmarks, lower extremity girth differences affecting LLI measurements, masking of LLIs observed in weight bearing by measuring in the supine position, and exclusion of the contributions of the foot and ankle to limb length. LLI was defined categorically as discrepancies ≥ 2 cm to account for these potential sources of error. Use of an LLI of ≥ 1.5 cm with the tape measurement technique has moderate intertester reliability (post-standardization prevalence-adjusted bias-adjusted kappa = 0.72)21. Thus, we believe our definition of LLI is conservative and clinically relevant since subjects with supine tape measurement differences between limbs ≥ 2 cm would likely demonstrate a LLI in standing. In a sensitivity analysis, the accuracy of the LLI measurements to correctly categorize participants based on a LLI ≥ 1 cm was questionable, and a difference in limbs of at least 1 cm was unlikely to be clinically meaningful. For these reasons, the original choice of defining a LLI as ≥ 2 cm remained the definition used in analyses.
Strengths of this study include that it is community-based, consists of African American and Caucasian men and women, includes rOA data and chronic symptoms data of the knee and hip in the same dataset, and uses an analytical approach that can accommodate the interval censoring of the study design. Additionally, the same study population was examined for the present study and the prior cross-sectional analyses of LLI and knee and hip rOA and symptoms10, 11.
To our knowledge, this is the first population-based study to examine hazard of incident and progressive knee and hip rOA and chronic knee or hip symptoms among individuals with and without LLI. Strengths of this study include that it is community-based, consists of African American and Caucasian men and women, includes rOA data and chronic symptoms data of the knee and hip, and uses an analytical approach that can accommodate the interval censoring of the study design.
In summary, in this community-based sample, the hazard of developing progressive knee rOA was significantly higher among those with LLI; other outcomes (incident knee or hip rOA and progressive hip rOA, progressive chronic knee symptoms, and incident and progressive chronic hip symptoms) were non-significantly higher among participants with LLI. However, LLI may be a marker of progression of knee rOA rather than a true predictor. Future studies should examine the incidence and progression of knee or hip rOA and chronic joint symptoms over a longer period to allow adequate time for the development of these conditions, establish duration of LLI, and identify physical factors contributing to each participants’ LLI. Additionally, the role of lower extremity rOA as a predictor of LLI should be explored.
Acknowledgements
This is a pre-copy-editing, author-produced PDF of an article accepted for publication in The Journal of Rheumatology following peer review. The definitive publisher-authenticated version [Golightly YM, Allen KD, Helmick CG, Schwartz TA, Renner JB, Jordan JM. Hazard of incident and progressive knee and hip radiographic osteoarthritis and chronic joint symptoms in individuals with and without limb length inequality. J Rheumatol. 2010 Oct;37(10):2133-40. doi: 10.3899/jrheum.091410. Epub 2010 Jul 15. PubMed PMID: 20634243.] is available online at: http://www.jrheum.org/content/37/10/2133.full.pdf+html.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Funding was made possible in part by the Centers for Disease Control and Prevention/Association of Schools of Public Health S043 and S3486.
Funding: Jordan/Renner: Centers for Disease Control and Prevention/Association of Schools of Public Health S043 and S3486, Multipurpose Arthritis and Musculoskeletal Diseases Center grant 5-P60-AR-30701 from the National Institute of Arthritis and Musculoskeletal and Skin Diseases; Golightly: Arthritis and Immunology T-32 Training grant AR-07416 from the National Institute of Health and American College of Rheumatology Research and Education Foundation/Abbott Health Professional Graduate Student Research Preceptorship 2008.
Footnotes
Competing Interests: The authors report no conflicts of interest in relation to this work.
Contributor Information
Yvonne M. Golightly, Department of Epidemiology, Gillings School of Global Public Health, University of North Carolina, Chapel Hill, NC and Thurston Arthritis Research Center, University of North Carolina, Chapel Hill, NC.
Kelli D. Allen, Health Services Research and Development Service, Durham Veterans Affairs Medical Center, Durham, NC and Department of Medicine, Division of General Internal Medicine, Duke University Medical Center, Durham, NC
Charles G. Helmick, Centers for Disease Control and Prevention, Atlanta, GA.
Todd A. Schwartz, Department of Biostatistics, School of Public Health, University of North Carolina, Chapel Hill, NC and Thurston Arthritis Research Center, University of North Carolina, Chapel Hill, NC.
Jordan B. Renner, Department of Radiology, University of North Carolina, Chapel Hill, NC, USA and Thurston Arthritis Research Center, University of North Carolina, Chapel Hill, NC.
Joanne M. Jordan, Thurston Arthritis Research Center, University of North Carolina, Chapel Hill, NC, Department of Medicine, University of North Carolina, Chapel Hill, NC, and Department of Orthopedics, University of North Carolina, Chapel Hill, NC.
References
- 1.Centers for Disease Control and Prevention. Health-related quality of life among adults with arthritis--Behavioral Risk Factor Surveillance System, 11 states, 1996–1998. Morb Mortal Wkly Rep. 2000;49:366–369. [PubMed] [Google Scholar]
- 2.deBock GH, Kaptein AA, Touw-Otten F, Mulder JD. Health-related quality of life in patients with osteoarthritis in a family practice setting. Arthritis Care Res. 1995;8:88–93. doi: 10.1002/art.1790080206. [DOI] [PubMed] [Google Scholar]
- 3.Dominck KL, Ahern FM, Gold CH, Heller DA. Health-related quality of life among older adults with arthritis. Health Qual Life Outcomes. 2004;2:5. doi: 10.1186/1477-7525-2-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Felson DT, Lawrence RC, Dieppe PA, Hirsch R, Helmick CG, Jordan JM. Osteoarthritis: New insights. Part 1: The disease and its risk factors. Ann Intern Med. 2000;133:635–646. doi: 10.7326/0003-4819-133-8-200010170-00016. [DOI] [PubMed] [Google Scholar]
- 5.Health, United States, 2008, with Chartbook on Trends in the Health of Americans. [Accessed June 2, 2009]; at http://www.cdc.gov/nchs/data/hus/hus08.pdf.)
- 6.Cerejo R, Dunlop DD, Cahue S, Channin D, Song J, Sharma L. The influence of alignment on risk of knee osteoarthritis progression according to baseline stage of disease. Arthritis Rheum. 2002;46 doi: 10.1002/art.10530. [DOI] [PubMed] [Google Scholar]
- 7.Sharma L. The role of proprioceptive deficits, ligamentous laxity, and malalignment in development and progression of knee osteoarthritis. J Rheumatol. 2004;31:87–92. [PubMed] [Google Scholar]
- 8.Sharma L, Lou C, Felson DT, et al. Laxity in healthy and osteoarthritis knees. Arthritis Rheum. 1999;42:861–870. doi: 10.1002/1529-0131(199905)42:5<861::AID-ANR4>3.0.CO;2-N. [DOI] [PubMed] [Google Scholar]
- 9.Sharma L, Song J, Felson DT, Cahue S, Shamiyeh E, Dunlop DD. The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA. 2001;286:188–195. doi: 10.1001/jama.286.2.188. [DOI] [PubMed] [Google Scholar]
- 10.Golightly YM, Allen KD, Renner JB, Helmick CG, Salazar A, Jordan JM. Relationship of limb length inequality with radiographic knee and hip osteoarthritis. Osteoarthritis Cartilage. 2007;15:824–829. doi: 10.1016/j.joca.2007.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Golightly YM, Allen KD, Helmick CG, Renner JB, Jordan JM. Symptoms of the knee and hip in individuals with and without limb length inequality. Osteoarthritis Cartilage. 2009;17:596–600. doi: 10.1016/j.joca.2008.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Brady RJ, Dean JB, Skinner TM, Gross MT. Limb length inequality: clinical implications for assessment and intervention. J Orthop Sports Phys Ther. 2003;33:221–234. doi: 10.2519/jospt.2003.33.5.221. [DOI] [PubMed] [Google Scholar]
- 13.Friberg O. Clinical symptoms and biomechanics of lumbar spine and hip joint in leg length inequality. Spine. 1982;8:643–651. doi: 10.1097/00007632-198309000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Jordan JM, Linder GF, Renner JB, Fryer JG. The impact of arthritis in rural populations. Arthritis Care Res. 1995;8:242–250. doi: 10.1002/art.1790080407. [DOI] [PubMed] [Google Scholar]
- 15.Hoyle DA, Latour M, Bohannon RW. Intraexaminer, interexaminer, and interdevice comparability of leg length measurements obtained with measuring tape and metrecom. J Orthop Sports Phys Ther. 1991;14:263–268. doi: 10.2519/jospt.1991.14.6.263. [DOI] [PubMed] [Google Scholar]
- 16.Jordan JM, Helmick CG, Renner JB, et al. Prevalence of knee symptoms and radiographic and symptomatic knee osteoarthritis in African Americans and Caucasians: the Johnston County Osteoarthritis Project. J Rheumatol. 2007;34:172–180. [PubMed] [Google Scholar]
- 17.Kellgren JH, Lawrence JS. The epidemiology of chronic rheumatism, atlas of standard radiographs. Oxford: Blackwell Scientific; 1963. [Google Scholar]
- 18.Odell PM, Anderson KM, D'Agostino RB. Maximum likelihood estimation for interval-censored data using a Weibull-based accelerated failure time model. Biometrics. 1992;48:951–959. [PubMed] [Google Scholar]
- 19.Harvey WF, Yang M, Cooke TDV, et al. Association of leg-length inequality with knee osteoarthritis. Ann Int Med. 2010;152:287–295. doi: 10.1059/0003-4819-152-5-201003020-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gogia PP, Braatz JH. Validity and reliability of leg length measurements. J Orthop Sports Phys Ther. 1986;8:185–188. doi: 10.2519/jospt.1986.8.4.185. [DOI] [PubMed] [Google Scholar]
- 21.Cibere J, Thorne A, Bellamy N, et al. Reliability of the hip examination in osteoarthritis: effect of standardization. Arthritis Rheum. 2008;59:373–381. doi: 10.1002/art.23310. [DOI] [PubMed] [Google Scholar]