Abstract
Purpose
Given the shortage of palliative care specialists in the U.S., to ensure quality of care for patients with serious, life-threatening illness, generalist-level palliative care competencies need to be defined and taught. The purpose of this study was to define essential competencies for medical students and internal medicine and family medicine (IM/FM) residents through a national survey of palliative care experts.
Method
Proposed competencies were derived from existing Hospice and Palliative Medicine fellowship competencies, and revised to be developmentally appropriate for students and residents. In spring 2012, the authors administered a web-based, national cross-sectional survey of palliative care educational experts to assess ratings and rankings of proposed competencies and competency domains.
Results
The authors identified 18 comprehensive palliative care competencies for medical students and IM/FM residents, respectively. Over 95% of survey respondents judged the competencies as comprehensive and developmentally appropriate (survey response rate=72%, 71/98). Using predefined cut-off criteria, experts identified 7 medical student and 13 IM/FM resident competencies as essential. Communication and pain/symptom management were rated as the most critical domains.
Conclusions
This national survey of palliative care experts defines comprehensive and essential palliative care competencies for medical students and IM/FM residents that are specific, measurable, and can be used to report educational outcomes; provide a sequence for palliative care curricula in undergraduate and graduate medical education; and highlight the importance of educating medical trainees in communication and pain management. Next steps include seeking input and endorsement from stakeholders in the broader medical education community.
A growing body of evidence suggests that incorporating specialty-level palliative care into the care of patients with serious or life-threatening illness improves quality of life, dying, and bereavement; and also affects larger social issues such as inappropriate use of ineffective and burdensome medical interventions for seriously ill patients and underuse of interventions that promote quality of life such as timely hospice referrals.1–4 However, there is a shortage of palliative care specialists across the United States compared to the growing number of patients facing serious and life-threatening illnesses.5 As national health care reform unfolds, with its emphasis on patient-centered care and “bending the cost curve,” experts highlight the need for improvements in palliative care service delivery.6 Improved generalist physician training in palliative care competencies is a critical need to attain these objectives.7–8
Introduction
Good evidence now demonstrates that palliative care competencies can be successfully taught at the undergraduate,9–12 graduate,13–15 and practicing physician level16–18; however, the content of existing curricula and methods of instruction are inconsistent across academic centers,19–22 and national standards for medical school and residency palliative care education are needed. Other fields, including geriatrics, pulmonary and critical care medicine, and emergency medicine, have published specialty-based consensus competencies for medical students, residents, and fellows.23–27 The purpose of this study was to create palliative care specialty-defined competencies for medical students and internal medicine and family medicine (IM/FM) residents.
This study builds on an extensive body of work over the past decade to define consensus-based clinical palliative care competencies, and to standardize required competencies for hospice and palliative medicine (HPM) fellowship. In 2004, after a rigorous consensus process, the National Consensus Project for Quality Palliative Care published clinical guidelines for palliative care; and in 2007 the National Quality Forum released a set of preferred practices for palliative care based on these guidelines.28,29 Within the same time period, in accord with the Accreditation Council for Graduate Medical Education (ACGME)’s Outcome Project30 mandate for competency-based curriculum and assessment, leaders in academic palliative care began a process of iterative review to create comprehensive HPM fellowship competencies.31 The fellowship competencies, and more recently competency-based measurable outcomes and assessment methods, have been endorsed by the American Academy of Hospice and Palliative Medicine (AAHPM) and published on their website.32–33
Method
In this study, we used medical student and resident competencies derived from published HPM fellowship competencies as the basis for a national survey34,35 to assess content validity (i.e., were the proposed competencies comprehensive and developmentally appropriate?), to prioritize essential graduation competencies, and to rank the importance of palliative care domains for each learner group.
Drafting proposed competencies
In April 2010 we convened palliative care educators (KS, EC, VP, SS, LM, ECC) from six academic medical centers across the United States and a senior leader (SDB) to form the Medical Student and IM/FM Residency Competencies Workgroup. All members were leaders in medical student or residency palliative care education at their institutions, and had expertise with competencies and/or learner evaluation. We designed a multi-step process to generate a list of comprehensive competencies for medical students and residents, respectively, using the published HPM fellowship competencies as a starting point. First, two members of the workgroup (EC, KS) reviewed each fellowship competency and categorized it as a general medicine competency, a fellowship-level competency beyond the scope of generalist-level practice, or a fellowship-level competency that could be transformed into developmentally appropriate resident and medical student competencies. Next (from April 2010 through March 2011), through a process of emails, seven conference calls, and in-person meetings, we iteratively reviewed and revised each competency in the third category, and derived corresponding developmentally appropriate medical student and IM/FM resident competencies. The language of each competency was kept as true to the published fellowship competencies as possible, and crafted to be “SMART” (specific, measureable, achievable, relevant, and timely).36 We sorted the resulting 18 medical student competencies and 18 corresponding resident competencies into five domains (pain and symptom management; communication; psychosocial, spiritual, and cultural aspects of care; terminal care and bereavement; and palliative care principles and practice), and presented in a side-by-side table format to emphasize the developmental trajectory of knowledge, skills, and attitudes expected over the course of undergraduate and graduate training (see Supplemental Digital Appendix 1).
Survey design and implementation
We used Qualtrics (a web-based tool) to develop the survey of experts’ ratings and rankings of proposed competencies and competency domains (survey available upon request). Eighteen student competencies and 18 resident competencies were sorted into the five domains. To minimize the risk of order bias, the five domains were presented in random order in each survey, and items within each domain were also presented in random order. To minimize social desirability bias and protect confidentiality, survey instructions detailed that workgroup members would not have access to respondent identifiers, and all survey data would be de-identified and stored on a secure server after data collection. The study was approved by the Partners Institutional Review Board, and met requirements of institutional review boards for each of our institution at the time.
We asked respondents to rate each competency at each training level as “essential for all,” “important for all,” “important for some,” or “not appropriate for this level,” with no more than 10 competencies in each learner group as “essential for all.” A running tally of items selected as “essential” was shown on each survey page to assist in this process. Survey instructions defined a competency as “essential for all” if it was a prerequisite for graduation from medical school or residency. We provided a reference table to respondents showing medical student and corresponding resident competencies presented side-by-side by domain. To assess content validity—that is, whether the 18 competencies were comprehensive and covered important palliative care content—we gave respondents the opportunity to make comments to revise or refine competencies or to suggest additional competencies they felt were missing.
Finally, to assess the relative weight that the group of educators collectively assigned to each domain, we asked each respondent to weigh the importance of each of the five palliative care domains for each learner group. The survey program automatically added the weights to ensure that the sum could not be greater than 100%. These domains were also presented in random order to minimize order bias. We requested the following demographic information of respondents: gender, number of years practicing clinical palliative care, proportion of clinical practice spent in palliative care, board certification in palliative care, faculty appointment, and length of time teaching various palliative care learner groups. Potential participants received advance notice about the study by email from one of us (SDB), followed by an email invitation to participate with an embedded link to the survey. We sent the survey by email in February 2012 with three email reminder notices over a three week period. No incentives were offered for participation.
Survey participant selection process
We identified a cohort of 98 expert palliative care physician educators using the three inclusion criteria below. Physicians who met any of the three criteria were eligible to participate (several participants met more than one selection criteria). No authors participated in the survey. Inclusion criteria were defined as follows.
Evidence of leadership role in medical student or resident education at the local or national level
To fulfill this criterion, a participant could serve as a leader of a palliative care program or course, or have developed a curriculum or assessment tool. In addition, s/he had to have taught as a faculty member for at least two years. We identified 49 educators fulfilling this criterion by emailing the AAHPM Fellowship Director listserv, Medical School Palliative Care Education project scholars,37 and educators who participated in the AAHPM Leadership Education and Academic Development (LEAD) leadership development program.
Evidence of publications related to medical student and IM/FM resident palliative care education
To qualify, participants needed one publication as first or last author and board certification in HPM, or two or more publications as first or last author with any board certification. We performed a PubMed search using the keywords “palliative care” and “medical education, undergraduate and graduate,” and included articles from 1996 to the present. Board certification was confirmed with the American Board of Medical Specialties.38 We identified 32 potential participants by this process.
Evidence of a national leadership role in palliative care and significant experience teaching medical students and IM/FM residents
To qualify, the 73 participants we identified needed to be a leader of a palliative care program or to have participated in medical education projects or committees at a national level, and have greater than five years’ experience teaching medical students or residents.
Data analysis
We carried out a descriptive analysis of survey items, reporting frequencies and percentages for categorical variables and means and standard deviations for continuous variables. To classify a competency as required for graduating medical students or residents, we specified a predetermined cutoff of 50% or greater percentage of experts rating that competency as “essential for all” and no more than 5% of respondents rating the item as “not appropriate for this level.” To assess within-group differences across individual competency ratings or across the five domains, as well as between groups by faculty rank, we carried out repeated-measures multivariate analysis of variance with contrasts. We specified a pre-determined level of α=0.05 (two-tailed) for tests of significance. Statistical analyses were performed using SAS/STAT Version 9.3 (SAS Inc., 2012).
Results
The survey response rate was 72% (71/98) (79% of those invited to participate responded to the survey; however, 6 of these surveys were incomplete and not included in the analysis). Demographic characteristics of respondents are shown in Table 1. Most respondents reported spending the majority of their clinical time in palliative care. Both junior and senior faculty members are represented in this sample, and most have taught students, residents, fellows, and faculty for more than 5 years. At the time of data collection, 93% of respondents were board certified in HPM.
Table 1.
Characteristics of 71 Palliative Care Experts Who Participated in a Survey about Essential Competencies for Medical Students and Residents, 2012
| Characteristic | Measure |
|---|---|
| Female gender, no. (%) | 36 (50.7) |
| Academic rank, no. (%) | |
| Instructor | 6 (8.4) |
| Assistant professor | 27 (38.0) |
| Associate professor | 22 (31.0) |
| Professor | 16 (22.5) |
| Proportion of current practice in palliative care, no. (%) | |
| 75–100% | 51 (71.8) |
| 50–74% | 10 (14.1) |
| 25–49% | 7 (9.8) |
| 0–24% | 3 (4.2) |
| Years in practice, mean (SD) | 11.7 (6.6) |
| Have taught for more than 5 years, no. (%) | |
| Medical students | 53 (79.1) |
| IM/FM residents | 49 (74.2) |
| Other residents | 44 (74.6) |
| Fellows | 47 (72.3) |
| Faculty | 50 (76.9) |
| Board certified in palliative care, no. (%) | 66 (93.0) |
| Primary board specialty, no. | |
| Internal medicine | 56 |
| Family medicine | 7 |
| Pediatrics | 4 |
| Geriatrics | 4 |
| Surgery, emergency medicine, medical oncology | 3 |
Abbreviations: SD = standard deviation; IM = internal medicine; FM = family medicine.
Rating of specific competencies
The proposed comprehensive palliative care competencies and essential competencies are shown in Supplemental Digital Appendix 1.
Medical student competencies
Table 2 shows that the majority of respondents rated all 18 medical student competencies as either “essential for all” or “important for all.” Seven medical student competencies, covering all five palliative care domains, were identified by 50% or more of respondents as essential for graduation. Only five items were rated as “not appropriate for this level,” and no more than four respondents gave this rating to an individual competency. Four respondents suggested items that were missing, and these suggestions were reviewed by the workgroup and assessed to be not meaningfully different from the 18 competencies already proposed. The number one ranked competency for medical students was to demonstrate the ability to describe ethical principles that inform decision-making at the end of life. Two of the top seven medical student competencies fell within the domain of communication: using patient-centered techniques when giving bad news and discussing resuscitation preferences, and exploring patient and family understanding of illness, concerns, goals and values that inform the plan of care. Two of the top seven competencies were in the domain of principles and practice of palliative care: developing the ability for self-reflection, especially when caring for patients at high risk for dying, and defining the philosophy and role of palliative care and hospice. Identifying psychosocial distress in patients and families and assessing pain systematically were also ranked in the top seven.
Table 2.
Palliative Care Competencies for Graduating Medical Students, Developed from a Survey of 71 Palliative Care Experts, 2012a
| Competency | Essential for all, no. (%) | Important for all, no. (%) | Important for some, no. (%) |
|---|---|---|---|
| 1. Describes ethical principles that inform decision-making in serious illness, including the right to forgo or withdraw life-sustaining treatment and the rationale for obtaining a surrogate decision maker. (TCB)b | 48 (67.6) | 21 (29.6) | 2 (2.8) |
| 2. Reflects on personal emotional reactions to patients’ dying and deaths. (PCPP)b | 40 (58.0) | 25 (36.2) | 4 (5.8) |
| 3. Identifies psychosocial distress in patients and families. (PSC)b | 40 (57.1) | 25 (35.7) | 5 (7.1) |
| 4. Explores patient and family understanding of illness, concerns, goals, and values that inform the plan of care. (C)b | 39 (57.3) | 25 (36.8) | 4 (5.9) |
| 5. Defines the philosophy and role of palliative care across the life cycle and differentiates hospice from palliative care. (PCPP)b | 37 (53.6) | 30 (43.5)) | 2 (2.9) |
| 6. Demonstrates patient-centered communication techniques when giving bad news and discussing resuscitation preferences. (C)b | 36 (56.2) | 24 (37.5) | 4 (6.2) |
| 7. Assesses pain systematically and distinguishes nociceptive from neuropathic pain syndromes. (PSM)b | 35 (50.0) | 31 (44.3) | 4 (5.7) |
| 8. Describes key issues and principles of pain management with opioids, including equianalgesic dosing, common side effects, addiction, tolerance, and dependence. | 33 (47.1) | 30 (42.9) | 7 (10.0) |
| 9. Demonstrates basic approaches to handling emotion in patients and families facing serious illness. | 32 (46.4) | 32 (46.4) | 5 (7.2) |
| 10. Identifies common signs of the dying process and describes treatments for common symptoms at the end of life. | 28 (39.4) | 28 (39.4) | 15 (21.1) |
| 11. Identifies patients’ and families’ cultural values, beliefs, and practices related to serious illness and end-of-life care. | 24 (34.8) | 39 (56.5) | 6 (8.7) |
| 12. Describes disease trajectories for common serious illnesses in adult and pediatric populations. | 22 (32.8) | 34 (50.7) | 11 (16.4) |
| 13. Describes the communication tasks of a physician when a patient dies, such as pronouncement, family notification, and request for autopsy. | 21 (31.3) | 36 (53.7) | 10 (14.9) |
| 14. Describes an approach to the diagnosis of anxiety, depression, and delirium. | 19 (27.5) | 37 (53.6) | 13 (18.8) |
| 15. Assesses non-pain symptoms and outlines a differential diagnosis, initial work-up and treatment plan. | 18 (25.7) | 41 (58.6) | 11 (15.7) |
| 16. Identifies spiritual and existential suffering in patients and families. | 12 (18.2) | 41 (62.1) | 13 (19.7) |
| 17. Describes the roles of members of an interdisciplinary palliative care team, including nurses, social workers, case managers, chaplains, and pharmacists. | 9 (13.8) | 36 (55.4) | 20 (30.8) |
| 18. Describes normal grief and bereavement, and risk factors for prolonged grief disorder. | 7 (10.8) | 38 (58.5) | 20 (30.8) |
Abbreviations: C = communication; PSM = pain and symptom management; PCPP= palliative care principles and practice; PSC = psychosocial, spiritual, and cultural aspects of care; TCB = terminal care and bereavement.
Because of missing item-level data some rows contain fewer than 71 responses.
Competencies given a rating of “essential” by 50% or more of respondents.
Resident competencies
Table 3 shows the competencies for graduating IM/FM residents. Similar to the medical student competencies, the majority of respondents rated each competency as either “essential for all” or “important for all” residents. No competency was rated as inappropriate for the residency-level, and no respondents suggested items that were missing. Thirteen competencies were identified by 50% or more of respondents as essential for graduation. As with the essential medical student competencies, essential competencies represented all 5 palliative care domains. The top two resident competencies related to patient-centered communication and shared decision-making. Three of the thirteen essential competencies were in the terminal care and bereavement domain. Of note, seven of the thirteen essential resident competencies were the more advanced versions of the essential medical student competencies. Other competencies identified as essential for IM/FM residents included more detailed expertise in opioid use, diagnosis and initial management of psychiatric symptoms, handling strong patient and family emotion, integrating cultural values into the treatment plan, symptom management at the end of life, and communication with family after a patient dies.
Table 3.
Palliative Care Competencies for Graduating Residents, Developed from a Survey of 70 Palliative Care Experts, 2012a
| Competency | Essential for all, no. (%) | Important for all, no. (%) | Important for some, no. (%) |
|---|---|---|---|
| 1. Explores patient and family understanding of illness, concerns, goals, and values, and identifies treatment plans that respect and align with these priorities. (C) b | 58 (84.0) | 11 (15.9) | 0 (0.0) |
| 2. Demonstrates effective patient-centered communication when giving bad news or prognostic information, discussing resuscitation preferences, and coaching patients through the dying process. (C)b | 54 (79.4) | 13 (19.1) | 1 (1.5) |
| 3. Assesses pain systematically and treats pain effectively with opioids, non-opioid analgesics, and non-pharmacologic interventions. (PSM)b | 52 (74.3) | 16 (22.9) | 2 (2.9) |
| 4. Defines and applies principles of opioid prescription, including equianalgesic dosing and common side effects, and demonstrates an understanding that appropriate use of opioids rarely leads to respiratory depression or addiction when treating cancer-related pain. (PSM)b | 52 (73.9) | 16 (22.9) | 2 (2.9) |
| 5. Defines and explains the philosophy and roles of palliative care and hospice, and appropriately refers patients. (PCPP)b | 51 (73.9) | 16 (23.)1 | 2 (2.9) |
| 6. Describes and performs communication tasks effectively at the time of death, including pronouncement, family notification and support, and request for autopsy. (TCB)b | 51 (72.9) | 18 (25.7) | 1 (1.4) |
| 7. Describes and applies ethical and legal principles that inform decision-making in serious illness, including: a) the right to forgo or withdraw life-sustaining treatment; b) decision-making capacity and substituted judgment; and c) physician-assisted death. (TCB)b | 50 (71.4) | 15 (21.4) | 5 (7.1) |
| 8. Identifies and manages common signs and symptoms at the end of life. (TCB)b | 43 (61.4) | 24 (34.3) | 3 (4.3) |
| 9. Evaluates psychological distress in individual patients and families, and provides support and appropriate referral. (PSC)b | 42 (60.0) | 26 (37.1) | 2 (2.9) |
| 10. Reflects on his or her own emotional reactions, models self-reflection, and acknowledges team distress when caring for dying patients and their families. (PCPP)b | 40 (58.0) | 27 (39.1) | 2 (2.9) |
| 11. Assesses and diagnoses anxiety, depression, and delirium and provides appropriate initial treatment and referral. (PSM)b | 39 (56.5) | 29 (42.0) | 10(1.4) |
| 12. Demonstrates effective approaches to exploring and handling strong emotions in patients and families facing serious illness. (C)b | 37 (54.4) | 30 (44.1) | 1 (1.5) |
| 13. Identifies patients’ and families’ values, cultural beliefs, and practices related to serious illness and end-of-life care, and integrates these into the care plan. (PSC)b | 35 (50.0) | 32 (45.7) | 3 (4.3) |
| 14. Assesses and manages non-pain symptoms and conditions including, but not limited to, dyspnea, nausea, bowel obstruction, and cord compression using current best practices. | 32 (45.7) | 34 (48.6) | 4 (5.7) |
| 15. Applies the evidence base and knowledge of disease trajectories to estimate prognosis in individual patients. | 26 (37.7) | 37 (53.6) | 6 (8.7) |
| 16. Identifies spiritual and existential distress in individual patients and families, and provides support and appropriate referral. | 18 (26.1) | 43 (62.3) | 8 (11.6) |
| 17. Describes the roles of and collaborates with members of an interdisciplinary care team when creating a palliative patient care plan. | 16 (23.2) | 44 (63.8) | 9 (13.0) |
| 18. Differentiates normal grief from prolonged grief disorder, and makes appropriate referrals. | 12 (17.6) | 45 (66.2) | 11 (16.2) |
Abbreviations: C = communication; PSM = pain and symptom management; PCPP= palliative care principles and practice; PSC = psychosocial, spiritual, and cultural aspects of care; TCB = terminal care and bereavement.
One participant did not provide responses for resident-level competencies
Competencies given a rating of “essential” by 50% or more of respondents.
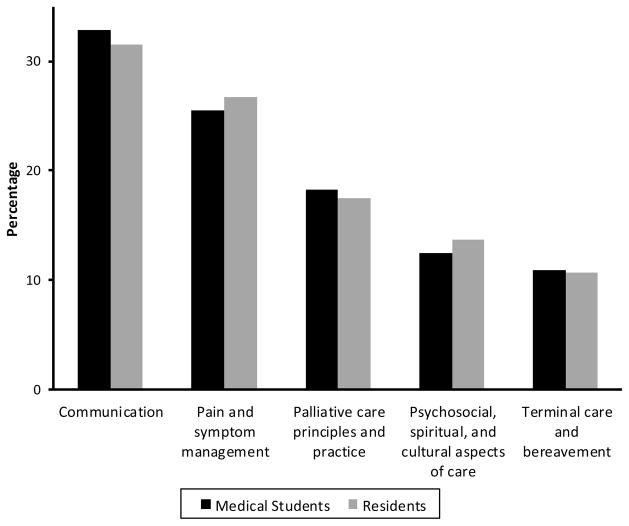
Ranking of palliative care domains
Figure 1 shows the relative weights assigned to each of the palliative care domains, for both medical students and residents. For both learner groups, the competency domains of communication and pain and symptom management received the highest weights. Differences between rankings for competency domains were statistically significant for all domains except between the two least weighted categories, psychosocial care and terminal care (student competencies, Wilk’s lambda for within-group difference F = 54.8, P < .0001; resident competences F = 71.7, P < .0001).
Figure 1.
Relative weight of importance of competencies assigned by 68 experts to each of five palliative care domains. Developed from a survey of 71 palliative care experts (data from 3 participants were missing or not given).
Discussion
Based on a national survey of expert palliative care physician educators, we have defined comprehensive and essential palliative care competencies specifically for medical students and IM/FM residents that can be applied to standardize the content and assessment of palliative care curricula at both levels, and can be the basis for future research to validate new assessment tools for all levels of learners. The palliative care competencies derived from our survey were crafted to be specific, measurable, achievable, and relevant for each learner group, and can be linked to existing ACGME competencies and standardized assessment tools already used in HPM fellowship training.33 Further, the developmental framework of the competencies is consistent with the ACGME’s New Accreditation System (NAS) mandate to identify “milestones,” or educational outcomes that can be demonstrated by the learner as s/he progresses through novice and advanced beginner levels, towards proficient and expert levels of competency.39,40 As residency programs strive to meet new ACGME credentialing requirements, these new palliative care competencies may be used to define reportable educational outcomes.41,42
In addition, the essential medical student and resident competencies suggest a developmental sequence for teaching and assessing palliative care competencies over the course of medical education. Developmentally, medical students must first establish an ethical compass to use when caring for seriously ill patients, and integrate their clinical experiences and the meaning of this work into their identity as physicians.43 Building on this foundation, residents need to revisit and deepen the knowledge, skills, and attitudes defined in the essential student competencies. For example, residents must not only be able to explain palliative care, but must also appropriately refer to hospice; residents need to not only recognize psychosocial distress, but also evaluate and appropriately refer patients and families with such distress; and residents must not only reflect on their own emotional reactions to caring for patients at the end of life, but also model self-reflection for their team. In addition, the essential resident competencies include more complex symptom management, patient-centered communication to clarify goals of care, and an understanding of how hospice and palliative care fit into the health care system. Assessment approaches could also reflect these developmental differences. For example, a standardized patient simulation could be used to assess medical student proficiency with an algorithm for delivering bad news, whereas a 360° evaluation might be used to assess a resident on multiple communication competencies after an interdisciplinary family meeting.
Understanding that undergraduate and graduate learners will be at different skill levels at different times, these new expert-derived competencies should be applied with flexibility during training, based on the individual trajectory of each learner. It would be anticipated, for example, that a second year resident might have attained minimum level competency in some palliative care competencies, but by the end of the residency training, should be required to attain minimum level competency in all 13 of the essential competencies. The competencies can also be used to assess for gaps in training throughout the course of medical education, including continuing medical education for practicing physicians. For example, all practicing internists should be able to demonstrate all of the 13 essential competencies, and continuing medical education programs can target ones that may not have been addressed effectively during residency training.
Finally, this study reinforces the need to teach and reinforce patient-centered communication techniques and symptom management at all levels of training. Patients with serious or life-threatening illnesses consistently rate communication with their physician and symptom management as high priorities for their care.44 Therefore, rigorous physician training in these and other basic palliative care competencies will be essential to the development and implementation of patient-centered models of care delivery for seriously ill patients.45
This study has some limitations. The drafting of the proposed comprehensive competencies mainly represented the work of 7 palliative care experts. However, we derived the medical student and residency competencies from the HPM fellowship competencies, which were vetted widely by expert palliative care physician educators and leaders in a separate iterative process. In addition, the 72% response rate and balanced demographics of the survey respondents support the generalizability of the outcomes. Finally, despite the important and highly-valued role non-physician members of the interdisciplinary team play in the training of medical students and residents, we decided not to include representation from other disciplines in the survey. We believe that defining competencies required for independent physician practice is best done by physician experts. A critical next step to maximize the impact of this project and disseminate the results will be to seek input and endorsement from stakeholders in the broader medical education community. This will then allow for optimal integration of the competencies into medical training.
In conclusion, using expert iterative review and a national survey, we have defined comprehensive and essential generalist-level palliative care competencies that are specific, measurable, and relevant, and can be integrated into undergraduate and graduate medical education in internal medicine and family medicine. We propose that the academic medical community should “raise the bar” to require that all graduating medical students and IM/FM residents demonstrate a minimum level of competence in the five domains of palliative care. Introducing these competencies early and in a thoughtful developmental sequence may improve physicians’ sense of clinical efficacy in these essential areas, and more importantly, improve the quality of care for patients with serious or life-threatening illness.
Supplementary Material
Acknowledgments
Funding/Support: Dr. Periyakoil’s work is supported in part by the National Institutes of Health Grants RCA115562A and 1R25MD006857 and the Department of Veterans Affairs.
Footnotes
Other disclosures: None reported.
Ethical approval: The study was approved by the Partners Institutional Review Board and met requirements of institutional review boards for each author’s institution. Dr. Morrison was on the Baylor College of Medicine faculty during the active project phase of this work. Thus, the Baylor College of Medicine IRB approved this study.
Previous presentations: Preliminary data from this study have been presented at the following: as an abstract at the 2012 Annual Assembly of the American Academy of Hospice and Palliative Medicine and as a paper presentation at the 19th International Congress on Palliative Care, 2012; in Schaefer KG, Chittenden EH, Periyakoil VS, Carey EC, Morrison LJ, Sanchez-Reilly S, Block S. Defining And Validating Palliative Care Competencies For Medical Students And Residents: A National Consensus Project, J Pain Symptom Manage 2012;43(2):363 (a paper given at the Annual Assembly of the American Academy of Hospice and Palliative Medicine and Hospice and Palliative Nurses Association, Denver, Colorado, March 8, 2012); and in Chittenden E, Schaefer K, Morrison L, Carey E, Block S. Medical Student and Resident Palliative Care Competencies. Proffered paper presentation at the 19th International Congress on Palliative Care, Montreal, Canada, October 11, 2012.
Contributor Information
Dr. Kristen G. Schaefer, Director of medical student and resident education, Division of Adult Palliative Care, Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute; and instructor, Department of Medicine, Harvard Medical School, Boston Massachusetts.
Dr. Eva H. Chittenden, Associate director and director of education, Palliative Care Division, Department of Medicine, Massachusetts General Hospital; and assistant professor, Department of Medicine, Harvard Medical School, Boston Massachusetts.
Dr. Amy M. Sullivan, Director for research, The Academy at Harvard Medical School; director for education research, Shapiro Institute for Education and Research, Beth Israel Deaconess Medical Center; and assistant professor, Department of Medicine, Harvard Medical School, Boston Massachusetts.
Dr. Vyjeyanth S. Periyakoil, Director of palliative care education and training; and director, Internet-based Successful Aging and End of Life (iSAGE) mini-fellowship, Stanford University School of Medicine; and associate director of palliative care services, Veterans Administration Palo Alto Health Care System, Palo Alto, California.
Dr. Laura J. Morrison, Director of hospice and palliative medicine education, and director, Hospice and Palliative Medicine Fellowship, Department of Medicine, Section of Geriatrics, Yale University School of Medicine, Yale-New Haven Hospital, New Haven, Connecticut.
Dr. Elise C. Carey, Chair, Section of Palliative Medicine, Division of General Internal Medicine, Mayo Clinic Rochester, Rochester, Minnesota.
Dr. Sandra Sanchez-Reilly, Associate director for education and evaluation, Geriatric Research, Education Clinical Center, South Texas Veterans Health Care System; and clinical associate professor of geriatrics and palliative care, University of Texas Health Science Center at San Antonio, San Antonio, Texas.
Dr. Susan D. Block, Chair, Department of Psychosocial Oncology and Palliative Care, Dana-Farber Cancer Institute and Brigham and Women’s Hospital; co-director, Harvard Medical School Center for Palliative Care; and professor of psychiatry and medicine, Harvard Medical School, Boston, Massachusetts.
References
- 1.Temel JS, Greer JA, Muzikansky A, et al. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363:733–42. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 2.Morrison RS, Penrod JD, Cassel JB, et al. Cost savings associated with U.S. hospital palliative care consultation programs. Arch Intern Med. 2008;168:1783–90. doi: 10.1001/archinte.168.16.1783. [DOI] [PubMed] [Google Scholar]
- 3.Meier D. Increased access to palliative care and hospice services: opportunities to improve value in health care. Milbank Q. 2011;89:343–80. doi: 10.1111/j.1468-0009.2011.00632.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Casarett D, Pickard A, Bailey FA, et al. Do palliative consultations improve patient outcomes? J Am Geriatr Soc. 2008;56:593–99. doi: 10.1111/j.1532-5415.2007.01610.x. [DOI] [PubMed] [Google Scholar]
- 5.Lupu D. Estimate of current hospiceand palliative medicine physician workforce shortage. J Pain Symptom Manage. 2010;40:899–911. doi: 10.1016/j.jpainsymman.2010.07.004. [DOI] [PubMed] [Google Scholar]
- 6.McCormick E, Chai E, Meier DE. Integrating palliative care into primary care. Mt Sinai J Med. 2012;79:579–85. doi: 10.1002/msj.21338. [DOI] [PubMed] [Google Scholar]
- 7.Weissman DE. Next gen palliative care. J Palliat Med. 2012;15:2–4. doi: 10.1089/jpm.2011.0312. [DOI] [PubMed] [Google Scholar]
- 8.Quill TE, Abernethy AP. Generalist plus specialist palliative care: Creating a more sustainable model. N Engl J Med. 2013;368:1173–75. doi: 10.1056/NEJMp1215620. [DOI] [PubMed] [Google Scholar]
- 9.von Gunten CF, Mullan P, Nelesen RA, et al. Development and evaluation of a palliative medicine curriculum for third-year medical students. J Palliat Med. 2012;15:1198–217. doi: 10.1089/jpm.2010.0502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schulz C, Möller MF, Seidler D, Schnell MW. Evaluating an evidence-based curriculum in undergraduate palliative care education: piloting a phase II exploratory trial for a complex intervention. BMC Med Educ. 2013;13:1. doi: 10.1186/1472-6920-13-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morrison LJ, Thompson BM, Gill AC. A required third-year medical student palliative care curriculum impacts knowledge and attitudes. J Palliat Med. 2012;15:784–9. doi: 10.1089/jpm.2011.0482. [DOI] [PubMed] [Google Scholar]
- 12.Radwany SM, Stovsky EJ, Frate DM, et al. A 4-year integrated curriculum in palliative care for medical undergraduates. Am J Hosp Palliat Care. 2011;28:528–535. doi: 10.1177/1049909111406526. [DOI] [PubMed] [Google Scholar]
- 13.Szmuilowicz E, el-Jawahri A, Chiappetta L, Kamdar M, Block S. Improving residents’ end-of-life communication skills with a short retreat: a randomized controlled trial. J Palliat Med. 2010;13:439–52. doi: 10.1089/jpm.2009.0262. [DOI] [PubMed] [Google Scholar]
- 14.Fischer SM, Gozansky WS, Kutner JS, Chomiak A, Kramer A. Palliative care education: An intervention to improve medical residents’ knowledge and attitudes. J Palliat Med. 2003;6:391–99. doi: 10.1089/109662103322144709. [DOI] [PubMed] [Google Scholar]
- 15.Olden AM, Quill T, Bordley D, Ladwig S. Evaluation of a required palliative care rotation for internal medicine residents. J Palliat Med. 2009;12:150–54. doi: 10.1089/jpm.2008.0246. [DOI] [PubMed] [Google Scholar]
- 16.Sullivan AM, Lakoma MD, Billings JA, Peters AS, Block SD. Teaching and learning end-of-life care: evaluation of a faculty development program in palliative care. Acad Med. 2005;80:657–68. doi: 10.1097/00001888-200507000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Claxton R, Marks S, Buranosky R, Rosielle D, Arnold RM. The educational impact of weekly e-mailed fast facts and concepts. J Palliat Med. 2011;14:475–481. doi: 10.1089/jpm.2010.0418. [DOI] [PubMed] [Google Scholar]
- 18.Stevens DP, Jones DH, Salerno JA, Ryan BJ. A strategy for improvement in care at the end of life: The VA Faculty Leaders Project. J Palliat Med. 1999;2:5–7. doi: 10.1089/jpm.1999.2.5. [DOI] [PubMed] [Google Scholar]
- 19.Lloyd-Williams M, MacLeod RD. A systematic review of teaching and learning in palliative care within the medical undergraduate curriculum. Med Teach. 2004;26:683–90. doi: 10.1080/01421590400019575. [DOI] [PubMed] [Google Scholar]
- 20.Case AA, Orange SM, Weissman DE. Palliative medicine physician education in the United States: A historical review. J Palliat Med. 2013;24:230–36. doi: 10.1089/jpm.2012.0436. [DOI] [PubMed] [Google Scholar]
- 21.Weissman DE, Quill TE, Block SD. Missed opportunities in medical student education. J Palliat Med. 2010;13:489–90. doi: 10.1089/jpm.2010.9838. [DOI] [PubMed] [Google Scholar]
- 22.Mullan PB, Weissman DE, Ambuel B, von Gunten C. End-of-life care education in internal medicine residency programs: an interinstitutional study. J Palliat Med. 2002;5:487–96. doi: 10.1089/109662102760269724. [DOI] [PubMed] [Google Scholar]
- 23.Leipzig RM, Granville L, Simpson D, Anderson B, Sauvigne K, Soriano R. “Don’t Kill Granny.” A Consensus on Geriatric Competencies for Graduating Medical Students. Acad Med. 2009;84:604–610. doi: 10.1097/ACM.0b013e31819fab70. [DOI] [PubMed] [Google Scholar]
- 24.Williams BC, Warshaw G, Fabiny AR, et al. Medicine in the 21st Century: Recommended Essential Geriatrics Competencies for Internal Medicine and Family Medicine Residents. Journal of Graduate Medical Education. 2010;2:3, 373–383. doi: 10.4300/JGME-D-10-00065.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hogan TM, Losman ED, Carpenter CR, et al. Development of geriatric competencies for emergency medicine residents using an expert consensus process. Acad Emerg Med. 2010;17:316–24. doi: 10.1111/j.1553-2712.2010.00684.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Buckley JD, Addrizzo-Harris DJ, Clay AS, et al. Multisociety task force recommendations of competencies in Pulmonary and Critical Care Medicine. Am J Respir Crit Care Med. 2009;15;180:290–5. doi: 10.1164/rccm.200904-0521ST. [DOI] [PubMed] [Google Scholar]
- 27.Chapman DM, Hayden S, Sanders AB, et al. Integrating the Accreditation Council for Graduate Medical Education Core competencies into the model of the clinical practice of emergency medicine. Ann Emerg Med. 2004;43:756–69. doi: 10.1016/j.annemergmed.2003.12.022. [DOI] [PubMed] [Google Scholar]
- 28.Ferrell B, Connor SR, Cordes A, et al. National Consensus Project for Quality Palliative Care Task Force Members. The national agenda for quality palliative care: the National Consensus Project and the National Quality Forum. J Pain Symptom Manage. 2007;33:737–44. doi: 10.1016/j.jpainsymman.2007.02.024. [DOI] [PubMed] [Google Scholar]
- 29.National Consensus Project for Quality Palliative Care. Clinical Practice Guidelines for Quality Palliative Care. 3. Pittsburgh, PA: 2013. [Accessed February 6, 2014]. http://www.nationalconsensusproject.org. [Google Scholar]
- 30.Swing SR. The ACGME outcome project: retrospective and prospective. Med Teach. 2007;29:648–654. doi: 10.1080/01421590701392903. [DOI] [PubMed] [Google Scholar]
- 31.Morrison LJ, Scott JO, Block SD for the ABHPM Competencies Workgroup. Developing initial competency-based outcomes for the hospice and palliative medicine subspecialist: phase 1 of the hospice and palliative medicine competencies project. J Palliat Med. 2007;10:313–330. doi: 10.1089/jpm.2006.9980. [DOI] [PubMed] [Google Scholar]
- 32.Hospice and Palliative Medicine Core Competencies Project Workgroup. [Accessed June 15, 2014];Hospice and Palliative Medicine Core Competencies, Version 2.3. 2009 http://aahpm.org/fellowships/competencies.
- 33.Hospice and Palliative Medicine Core Competencies Project Phase 2 Workgroup. [Accessed June 15, 2014];Measurable Outcomes for Hospice and Palliative Medicine Competencies Version 2.3. 2009 http://aahpm.org/fellowships/competencies.
- 34.Dillman DA, Smyth JD, Christian LM. Internet, Mail and Mixed-Mode Surveys: The Tailored Design Method. 3. Hoboken, NJ: John Wiley and Sons; 2009. [Google Scholar]
- 35.Fowler FJ. Survey Research Methods. 4. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 36.Doran GT. There’s a S.M.A.R.T. way to write management’s goals and objectives. Management Review. 1981;70:35–36. [Google Scholar]
- 37.Weissman DE, Quill TE, Block SD. Missed opportunities in medical student education. J Palliat Med. 2010;13:489–90. doi: 10.1089/jpm.2010.9838. [DOI] [PubMed] [Google Scholar]
- 38.American Board of Medical Specialties. [Accessed February 6, 2014];My Doctor Is Board Certified. Is Yours? http://www.certificationmatters.org/
- 39.Batalden P, Leach D, Swing S, Dreyfus H, Dreyfus S. General competencies and accreditation in graduate medical education. Health Aff. 2002;21:103–111. doi: 10.1377/hlthaff.21.5.103. [DOI] [PubMed] [Google Scholar]
- 40.Goroll AH, Sirio C, Duffy FD, et al. A new model for accreditation of residency programs in internal medicine. Ann Intern Med. 2004;140:902–9. doi: 10.7326/0003-4819-140-11-200406010-00012. [DOI] [PubMed] [Google Scholar]
- 41.Green ML, Aagaard EM, Caverzagie KJ, et al. Charting the road to competence: developmental milestones for internal medicine residency training. J Grad Med Educ. 2009;1:5–20. doi: 10.4300/01.01.0003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chang A, Bowen JL, Buranosky RA, et al. Transforming Primary Care Training-Patient-Centered Medical Home Entrustable Professional Activities for Internal Medicine Residents. J Gen Intern Med. 2013;28:801–809. doi: 10.1007/s11606-012-2193-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rabow MW, Remen RN, Parmelee DX, Inui TS. Professional formation: extending medicine’s lineage of service into the next century. Acad Med. 2010;85:310–7. doi: 10.1097/ACM.0b013e3181c887f7. [DOI] [PubMed] [Google Scholar]
- 44.Steinhauser KE, Clipp EC, McNeilly M, Christakis NA, McIntyre LM, Tulsky JA. In search of a good death: observations of patients, families, and providers. Ann Intern Med. 2000;132:825–32. doi: 10.7326/0003-4819-132-10-200005160-00011. [DOI] [PubMed] [Google Scholar]
- 45.Rittenhouse DR, Shortell SM. The Patient-Centered Medical Home: Will It Stand the Test of Health Reform? JAMA. 2009;301:2038–2040. doi: 10.1001/jama.2009.691. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.