Abstract
Background
Tobacco use is still the leading preventable cause of death and morbidity in the U.S. Web-assisted tobacco interventions are an effective but underutilized tool in assisting smokers with quitting. The dental visit is an excellent opportunity to assist smokers in quitting by referring them to these tobacco cessation online programs.
Purpose
The study purpose was to test two patient referral methods—paper referrals (information prescriptions) versus paper plus e-referrals—to a web-assisted smoking cessation induction system.
Design
An RCT that used implementation research methods.
Participants/setting
100 community-based dental practices were enrolled and 1814 smokers were referred to the web-assisted tobacco induction system.
Intervention
The study intervention was a proactive e-referral of smokers to a web-assisted tobacco induction system called Decide2Quit.org and the control group used paper referrals (information prescriptions) to refer smokers to the Decide2Quit.org.
Main outcome measurements
The outcome measurements were the referral numbers, Decide2Quit registration numbers, and the smokers’ quit rate. Data were collected in 2010–2011 and analyses were completed in 2012.
Results
Although total referrals from intervention practices was lower than control, subsequent proportion of registrations among smokers referred to Decide2Quit.org was nearly fourfold higher (adjusted mean percentages: 29.5% vs 7.6%, p< 0.01) in intervention compared with control practices. Subsequent rates of cessation among referred smokers were threefold higher (adjusted mean percentages: 3.0% vs 0.8%, p=0.03) in intervention practices as compared with control.
Conclusions
Intervention practices using the e-referral system had higher smoker registration numbers and higher quit smoking rates than the control practices. This study finds that e-referrals are effective in getting smokers to the web-assisted smoking cessation induction system and in assisting with quitting that more than compensates for any additional effort that e-referrals require on the part of the practitioner.
Clinical Trial Registration
DPBRN Hygienists Internet Quality Improvement in Tobacco Cessation (HiQuit); NCT01108432
Introduction
Tobacco use continues to be the leading preventable cause of death and morbidity in the U.S.1,2 In 2010, about 58.3 million Americans were cigarette smokers.3 Although cigarette smoking declined from 2005 to 2010, the decline was modest (20.9% to 19.3%) and additional efforts are needed to reduce tobacco use.1,4
For patients, the Internet has become an important channel for obtaining information on healthcare issues, including tobacco cessation.5–9 Web-assisted tobacco interventions can support smoking cessation8, 10–13 and reach a broader group of smokers than telephone-based cessation programs,8 but few smokers take advantage of such systems.
For providers, quit smoking resources are available to assist in delivering tobacco cessation services to their patients14 but these resources are often underutilized.15 Referrals to web-assisted tobacco interventions are easy to make, accessible wherever Internet connections are available and potentially cost effective.8,9 Smokers feel a greater need for dental care when compared to nonsmokers putting dental practices in a unique position to refer smokers to these resources.16 In 2010–2011 an RCT was conducted among 100 community-based dental practices of two patient referral methods—paper referrals (information prescriptions) versus paper plus e- referrals—to a web-assisted smoking cessation induction system. All referred patients could access Decide2Quit.org, a multi-modal, evidence-based smoking cessation induction system available via the Internet. The study hypotheses were that (1) the proactive e-referral in intervention dental practices would have a higher number and proportion of referred smokers registering with Decide2Quit.org, as compared with the control practices; and (2) this higher registration number would result in a higher rate of smoking cessation among those referred.
Methods
To optimize use by the dental practices, implementation research methods to design the study outcome of smoker e-referrals was used. Implementation research refers to scientific methods that facilitate the adoption of evidence-based research findings into routine practice with the ultimate goal of improving health. 17 The study was designed to be pragmatic in that it could be implemented into the usual care. The protocol development was guided by the pragmatic-explanatory continuum indicator summary (PRECIS), which is a tool to assist in designing studies that are conducted under usual conditions.18 Consistent with the PRECIS tool, the practice eligibility criteria were broad in that all general dental practices interested, saw at least five smokers per week and have office-based Internet access were included. Overall, the study implementation was flexible. There was flexibility with participant compliance. For example, the practices could assign a staff member to implement the study as they deemed appropriate. The practitioner adherence to the intervention was also flexible in that the practice could use the e-referral (intervention) or could use a written prescription as a method of referral to the smoking cessation website. And, there were no special strategies to improve study compliance or use of the intervention. However, because this was a research study, the method of data collection was a standard protocol and not pragmatic.
Recruitment
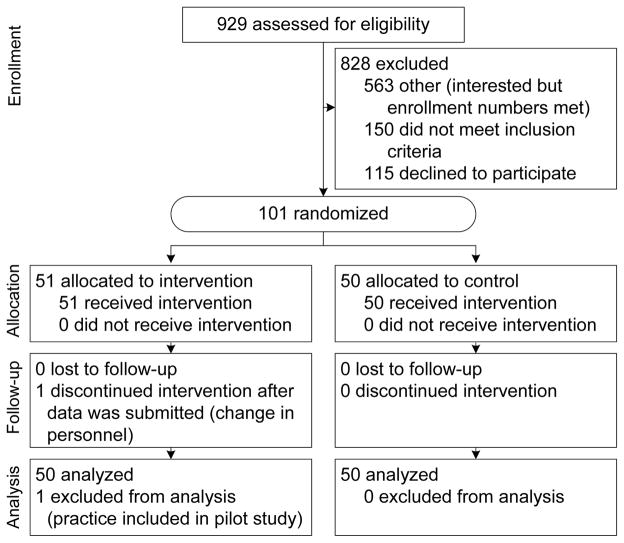
Dental practices were recruited from a pool of dentists in the National Dental Practice-Based Research Network (Alabama, Florida, and Georgia) and Dental Board lists (Tennessee, North Carolina, South Carolina, Mississippi, and Minnesota). A letter describing the study and a brief survey to ascertain eligibility and interest were mailed to 23,300 dentists between March and May of 2010. To be eligible for the study, practices had to be general dentistry, have office-based Internet access, see five adult smokers per week and express interest in participating. Of the recruitment surveys sent, 929 (4%) were returned; of which 779 were eligible and expressed interest in participating. Eligible practices responding to the initial invitation within 4 weeks (n=468) were then mailed a detailed-recruitment letter and consent form. Once a consent form was returned, a baseline practice survey was mailed. The first 101 practices to return the baseline survey (Figure 1) were enrolled. One practice was eliminated from analyses because it had participated in the pilot study. Practices were given a total of $1500 over a 1-year period for completion of a baseline, qualitative and follow-up surveys, training on use of the provider website; and responding to emails from the research coordinator. The study was approved by the University of Alabama at Birmingham (UAB) IRB.
Figure 1.
Dental PBRN Hygiene CONSORT 2012 Diagram
Practice Randomization, Referral, and Treatment Protocol
Practices were randomized when they completed study protocol training on (1) using the provider website, ReferASmoker.org, and (2) referring smokers to the Decide2Quit.org tobacco cessation website. For training on ReferASmoker.org provider website, the research coordinator set up a 30-minute telephone appointment with the designated contact person (dentist or hygienist). The contact person was called the practice coordinator because they managed the study and made referrals to Decide2Quit. Both control and intervention practices were trained on how to complete a paper information prescription that provided patients who smoke with the web address and advised the patient to visit the Decide2Quit.org site; a carbon copy of the information prescription was included, with a perforated section for both the dental provider and the study staff. Smokers could use the web address provided on the information prescription to visit Decide2Quit.org on their own, after leaving the dental office. Because this was a cessation induction study, all smokers were referred regardless of their interest in quitting. During the training session, the research coordinators also reviewed the provider website resources, which included printable quit smoking posters, information on nicotine replacement therapy, the treating tobacco use guidelines,19 and case-based continuing education. Although both intervention and control practices could access the provider website, only the intervention practices could access the e-referral system.
Intervention practices were trained on how to electronically refer a smoker (e-referrals) using the ReferASmoker.org website and practiced electronically referring fake patients. The practice coordinator referred their patients who smoke by obtaining his or her permission and entering their email address directly into an e-referral portal on ReferASmoker.org. The e-referrals are programmatically tracked by the system. This patient referral system triggered several automated processes, one of which is that the patient’s email is automatically entered into the database of the patient online smoking-cessation system, enabling the patient to register and login to the patient system. The development and programming of the ReferASmoker.org is described in a prior publication.20 Electronically referred (e-referred) smokers from intervention practices received weekly automated emails from the system that provided a direct link to the Decide2Quit.org website and encouragement to logon. The emails continued for 4 weeks or until the smoker logged onto Decide2Quit.org. These e-referrals were tracked electronically, as were all smoker registrations on Decide2Quit.org. To further support referral behavior within ReferASmoker.org, intervention practices also received feedback electronically about the number of smokers referred, number of smokers who registered on the Decide2Quit.org website and how their number of referrals (number per practice) compared to their peers.
Eight to twelve weeks after randomization and training, the research coordinators sent a booster email to intervention and control practices, asking for an update on the number of smokers referred and inquired about any problems with the study implementation (Appendix A, available online at www.ajpmonline.org). If research coordinators did not receive a response from the original email, a second email was sent 7–10 days following the original email. If no response was received 1–2 weeks following the second email, the research coordinator contacted the practice by telephone to record self-reported referrals.
Patient (Smokers) Registration and Follow-Up
Patients entered the study by referral through their dental provider participating in the study. To be eligible, patients had to: (1) be smokers, (2) be aged ≥19 years, (3) speak English, and (4) consent to participate. Patient eligibility and baseline smoking habits were assessed at first logon to the Decide2Quit.org website. At 6 months post-registration, patients completed an online survey. If patients did not complete the online survey after four email reminders, the research coordinators attempted to conduct a telephone interview.
Data sources for this report included an interest card, dental practice baseline survey, information prescription data, patient online baseline survey (registration), and patient 6-month follow-up survey. All data-collection instruments and the protocols are publicly available at nationaldentalpbrn.org/peer-reviewed-publications.php. A timeline for data-collection points is presented in Figure 2.
Measuring Referral Numbers, Patient Registration, and 6-Month Smoking Cessation
Practice referral numbers were assessed using three different methods: practice self-report, electronic referrals, and information prescriptions. For both intervention and control practices the practice coordinator, who was usually the dental hygienist, managed the study. For the practice self-report, the assigned practice coordinator reported the number of patients referred via telephone interview at 6–8 weeks post-training. All e-referrals were logged using the ReferASmoker.org system. Finally, both intervention and control practices could provide the patient with an information prescription that referred the smoker to the tobacco cessation website: Decide2Quit.org. The designated section of the information prescriptions was returned to the UAB research staff via U.S. mail in pre-addressed, postage-paid envelopes. Although both intervention and control had information prescriptions, some intervention practices chose to use only the e-referral portal.
Using Decide2Quit.org web analytics, patient registrations were monitored, and linked to the referring practice for both intervention and control practices. Six months after registrations, patients were sent an email requesting completion of an online follow-up survey. If not completed within 3 weeks, and up to four reminder emails, participants were called. To assess smoking cessation, patients were asked, at 6 months: Did you smoke any cigarettes during the past 30 days? Patients for whom a follow-up survey was not completed were presumed to have not quit smoking in the analysis.21
Analyses
Practice-level data from interest cards and the baseline survey, as well as patient registration data, were compared to assess equalization of randomization. Chi-square, t-tests, or corresponding nonparametric tests were used to assess significance of differences found. The analyses presented are based on self-reported number of patient referrals, as it was the only method consistently used by both intervention and control. Using web analytics from Decide2Quit.org, the number of patients who registered was obtained, and the proportion of patients referred who registered was calculated, all by practice, and then compared by randomization group. Multivariable linear regression (ANCOVA), with number of referrals as the dependent variable, and randomization group as the primary independent variable, for adjusted measures was performed. Variables of a priori interest in the model were adjusted for, namely, practice size and composition (number of patients and smokers seen per week, patient demographics), tobacco cessation protocols in place and perceived barriers to tobacco cessation services by the practice personnel. This process was repeated for the number and proportion of patients who registered on Decide2Quit.org. Similarly, among patients referred, the proportion who had not smoked within the past 30 days was compared between the randomization groups. Chi-square test was used to assess significance of differences in overall proportions found; ANCOVA was used to assess significance of difference in proportion of patients referred, per practice, who had quit.
Results
Practice Characteristics
Intervention and control practices were similar in most characteristics assessed, for example, majority were solo practices, employed two or more hygienists, about one fourth said that their practice was not busy enough in the prior year, and had similar estimation of patient ages, payment method and number of barriers to referral. They differed in that intervention practices estimated having a higher proportion of African-American patients, saw more patients who smoked per week than did control practices, and had fewer office procedures in place to enhance referral and/or smoking cessation counseling (Table 1).
Table 1.
Dental practice self-reported proportion of patient demographics among 100 participating dental practicesa
| Patient demographics | INTERVENTION (50 practices) | CONTROL (50 practices) | |
|---|---|---|---|
| mean % | mean % | p | |
| Estimated percent of patients in practice | |||
| By age (years) | |||
| 1 – 18 | 20 | 16 | 0.2 |
| 19 – 44 | 33 | 30 | 0.14 |
| 45 – 64 | 30 | 34 | 0.26 |
| 65 and older | 17 | 21 | 0.15 |
| By race/ethnicity | |||
| White | 60 | 64 | 0.2 |
| African American/Black | 26 | 20 | 0.02 |
| All other | 15 | 17 | 0.6 |
| By insurance | |||
| Private insurance with at least some dental coverage | 60 | 63 | 0.6 |
| Practice staff and patient load (past 12 months) | |||||
|---|---|---|---|---|---|
| N | % | N | % | p | |
| Solo practitioners | 38 | 76 | 39 | 78 | 0.99 |
| Employ 2 or more hygienists | 29 | 58 | 29 | 58 | 0.8 |
| Not busy enough | 14 | 29 | 11 | 22 | |
| Median # of patients/week [IQRb] | 100 | [64–136] | 87 | [60–130] | 0.6 |
| Median # of smokers/week [IQR] | 20 | [12–30] | 16 | [12–25] | <0.001 |
| Had ever referred patient to quit line | 14 | 28 | 11 | 22 | 0.5 |
| Median # of barriersc to referral agreed with | 3 | [2–3] | 2 | [2–3] | 0.2 |
| Median # of office proceduresd in place that enhance referral/counseling | 1 | [1–2] | 2 | [1–3] | 0.02 |
All data-collection instruments and the protocols are publicly available at nationaldentalpbrn.org/peer-reviewed-publications.php.
IQR: Interquartile range
Barriers: list of 9 queried, for example, do not have resources needed, cannot get reimbursed
Procedures: list of 8 queried, for example, have patient intake forms for smoking
Referral and Registration Numbers
Overall, 96% of the 100 practices referred at least one smoker to Decide2Quit.org. By 6 months after the practice had been enrolled, of the 50 intervention practices, 24 made referrals using both information prescriptions and e-referrals, 20 used only e-referral, and one used only information prescription referrals. Most self-reports were within one of the number documented by the electronic capture or receipt of paper (prescription) referral. All but two control practices returned information prescriptions. Among the intervention group, the (Spearman rank) correlation between number of e-referrals and the number based on the practice’s self-report was r =0.8 (p<0.001). Similarly, among the control group, the correlation between the number of information prescription referrals and the practice’s self-report was also r =0.8 (p<0.001). These high correlations suggest a high convergent validity of the practice’s self-reported measure of the number of referrals.
A total of 1814 smokers were referred by control (1120) and intervention (694) practices during a 12-month period. The mean number of smokers referred per practice was higher for control than intervention practices (Table 2). In contrast to smoker referral being higher among control than intervention practices, more smokers from intervention practices subsequently registered than smokers from control practices, 179 and 79, respectively; the adjusted number of smokers registered per practice was 3.5 vs 1.8, p=0.001. This difference between intervention and control practices was even greater when assessed as proportion of smokers referred who registered, namely, 29.5% vs 7.6% (p<0.001; Table 2). Potential confounding variables included the estimated number of smokers seen per week, estimated proportion of patients by age, race, insurance groups, number of barriers regarding smoking cessation and number of procedures to aide in smoking cessation. None of the potential confounders adjusted for were significant in any model examining the number of smokers registered or the proportion of smokers referred who registered.
Table 2.
Mean number of patients referred and who registered, by randomization group
| INTERVENTION | CONTROL | p | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Referral | |||||
| Referred ANY patient | 48 | 96 | 48 | 96 | |
| Total # of pts referred | 694 | 1120 | |||
| Number of patients referred per practice | |||||
| Mean (±SE) - adjusted* | 13.3 (±1.7) | 22.7 (±1.6) | <0.001 | ||
| Register (Go) - ALL | |||||
| Any patients registered | 42 | 84 | 35 | 70 | 0.08 |
| Total # pts registered | 179 | 79 | |||
| Number of patients registered per practice | |||||
| Mean (±SE) - adjusted* | 3.5 (±0.4) | 1.8 (±0.4) | 0.001 | ||
| Proportion of referred patients who registered (calculated within each practice) | |||||
| Mean (±SE) - adjusted* | 29.5 (±3.0) | 7.6 (±2.9) | <0.001 | ||
Mean - adjusted for estimated number of smokers, estimated patients’ age, race, and private insurance; number of barriers and number of procedures in use
SE: Standard error
Smoker Characteristics
The intervention and control groups were similar in that of the patients who registered, the majority were female, non-Hispanic white, had either some college education or a college degree and expressed interest in quitting smoking. Although this was a cessation induction program, not all smokers (8.5%; 22/258) expressed interest in quitting even though they logged on to the site. Also recognizing the chronic nature of smoking, namely, that most smokers require multiple attempts before truly quitting,19 and not all smokers reported smoking at baseline (Table 3). The groups differed in average number of cigarettes smoked per day for the prior year. The control group smoked fewer cigarettes per day and had a higher proportion of smokers who had ever visited a smoking cessation website.
Table 3.
Characteristics of dental patients participating in an online smoking cessation program by randomization group
| INTERVENTION | CONTROL | p | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
|
| |||||
| ALL | N=179 | N=79 | |||
| Age (years) | 0.5 | ||||
| <35 | 52 | 29 | 26 | 33 | |
| 35–44 | 39 | 22 | 11 | 14 | |
| 45–54 | 53 | 30 | 26 | 33 | |
| 55+ | 35 | 20 | 16 | 20 | |
| Gender | 0.3 | ||||
| Male | 58 | 33 | 31 | 39 | |
| Female | 120 | 67 | 48 | 61 | |
| Non-Hispanic white race/ethnicity | 0.7 | ||||
| Yes | 134 | 75 | 61 | 77 | |
| No | 45 | 25 | 18 | 23 | |
| Education | 0.4 | ||||
| High school/GED or less | 51 | 29 | 19 | 24 | |
| Some college | 79 | 44 | 32 | 41 | |
| College graduate (4 year) | 49 | 27 | 28 | 35 | |
| Number of cigarettes/day past 12 months | 0.04 | ||||
| zero | 8 | 5 | 11 | 14 | |
| 1–9 | 36 | 20 | 18 | 23 | |
| 10–19 | 70 | 39 | 28 | 35 | |
| 20+ | 65 | 36 | 22 | 28 | |
| Allow smoking in home | 0.15 | ||||
| Yes | 64 | 36 | 21 | 27 | |
| No | 115 | 64 | 58 | 73 | |
| Had ever visited smoking cessation website | 0.02 | ||||
| Yes | 16 | 9 | 15 | 19 | |
| No | 163 | 91 | 64 | 81 | |
| Had stopped smoking >= 1 day past yr b/c want to quit | 0.5 | ||||
| Yes | 103 | 58 | 42 | 53 | |
| No | 76 | 42 | 37 | 47 | |
| Want to stop smoking | 0.13 | ||||
| Yes | 154 | 86 | 60 | 76 | |
| No | 12 | 7 | 10 | 13 | |
| Do not smoke now | 13 | 7 | 9 | 11 | |
Quit Rates
The 6-month follow-up survey queried about when last smoked, amount smoked, and satisfaction with program. Overall, 53% of the smokers who registered completed this survey, either online or by telephone, similar for both randomization groups. At follow-up, 11.6% (30/258) of participants reported not having smoked in the 30 days prior to the call. This 11.6% was the overall quit rate for the web assisted smoking cessation induction system. Among smokers who registered, the proportions who quit were similar for control and intervention groups (Table 4). Among smokers referred (compared to those registered), the proportion who quit was higher for intervention than control group (Table 4). This significant difference is strengthened when assessed as mean proportion (of referred smokers) per practice adjusted for number of smokers seen per week (3.0% vs 0.8%; p=0.03) (Table 4).
Table 4.
Six-month follow-up of dental patients referred to an online smoking cessation by practice randomization group
| INTERVENTION | CONTROL | P | |||
|---|---|---|---|---|---|
| N | % | N | % | ||
| Total number referrals | 694 | 1120 | |||
| Number quit | 20 | 2.9 | 10 | 0.9 | 0.002 |
| Proportion of referred patients who QUIT per practice | |||||
| Mean ±SE - adjusted* | 3.0 ±0.7 | 0.8 ±0.7 | 0.03 | ||
Adjusted for number of protocols in place to enhance referral
SE: Standard error
Discussion
This implementation study was successful in that 98% of all practices referred smokers to the Decide2Quit website. The intervention practices did better than the control practices with regard to quit rates in both absolute numbers (20 vs 10) and the proportion of smokers referred (3% vs 1%). The higher quit rate was a reflection of the intervention practices using e-referrals, achieving higher smoker registration numbers to the web-assisted smoking cessation induction system, than control practices.
The higher referral numbers among the control practices may be due to the ease of handing out the information prescription compared to collecting and entering an email address. In addition, collecting emails from patients may be an additional burden to the practices in that it requires additional time; whereas handing out the written information prescription may be more consistent with routine care. Regarding the lower registration in the control practices, it may be that some of the smokers who received paper referrals did not have readily available access to the Decide2Quit website. E-referrals, by virtue of obtaining an email address from the patient, confirm that these smokers have some access to and use of the Internet. Thus, the automatic linkage to the website required minimal effort on the part of the smoker to register. The control group required more effort, as they had to keep track of the prescription slip and type in the web address. Thus, higher registration numbers among intervention practices were expected. What warrants attention is the magnitude of these differences. Intervention practices referred at a 40% lower level (13.3/22.7 = 0.6) than control practices. However registration numbers for intervention practices were nearly twice (3.5/1.8 = 1.9) those of control practices.
The overall quit rate of 11.6% for this web-assisted smoking cessation induction system is similar to those reported by others. 8,22,23 A cohort study from the Minnesota QUITPLAN Program reported a 12.5% quit rate 6 months post-web intervention when measuring smoking within last 30 days.22 In addition, the Minnesota QUITPLAN Program reported participation for the web-assisted tobacco intervention was much larger than participation via helpline, treatment centers, and worksite interventions. At a 6-month follow-up survey post–web-assisted tobacco intervention, Saul et al.8 reported that 13.2% had not smoked in the previous 7 days. The quit rate in this study is comparable to the Saul study, but was based on the more-conservative estimate of not having smoked in past 30 days; this e-referral study also included smokers who stated that they were not interested in quitting when they registered on the Decide2Quit website. In contrast to other smoking cessation programs, which focused only on smokers with stated interest in quitting, the present study was an induction cessation study, recognizing that smoking, even smoking cessation, is a chronic condition usually requiring several attempts before quitting.19
This study tested the use of e-referrals in a dental setting and to the knowledge of the investigators, it is the first pragmatic study of this type, that is, implementing the study into usual care of the dental practice which is consistent with the PRECIS tool. Because this was an implementation study, the findings are conservative in that the dental practices had control over how to implement the study into their regular practice, including who was responsible for providing tobacco cessation services and when to provide such services. In addition, this was an induction study and referrals to the Decide2Quit.org included smokers who were not necessarily interested in quitting. The study findings are especially exciting because this was a pragmatic and an induction study, both of which produce conservative results.
The study has limitations in that data collection did not include information on whether or not smokers had email addresses or Internet access because the main focus of the trial was practice-level effects. Since patients in the intervention group readily provided an email address when asked, practice coordinators rarely reported problems with collecting the email address from patients, this is considered to be a minor limitation. In addition, the patient demographics were the practices estimate. However, any error in estimation should be similar for both groups by virtue of randomization. Also, data were not collected on patients who were referred but who did not register on the Decide2Quit website—thus comparability of patients referred cannot be assessed.
Although the number of patients completing the follow-up survey is small, the estimated quit rates were conservative with the assumption that those not contacted continued to smoke. However, the loss to follow-up proportion (46% of 258 who registered) was lower than that reported from similar Internet studies. Web-assisted tobacco intervention attrition has been fairly high, ranging from 69% to 84% 5,24–31 and as noted by Eysenbach,32 high dropout may be typical for Internet studies. These issues might limit the generalizability of the practitioner and patient sample. Although the practitioners in the Dental Practice-Based Research Network are similar to other non-network dentists33,34 and participating practitioners were recruited from state licensing lists as well as from the network, there is no evidence suggesting any systematic difference. A limitation of any web-assisted intervention is that it may not reach some disadvantaged people, but the advantages of reaching a broad population and being effective at minimal or no cost to the provider and patient can still have a substantive impact on tobacco use.
Although e-referrals require slightly more effort on the part of the practitioner than handing the smoker a prescription or information sheet, this study suggests that e-referrals are effective in getting the smokers to the web-assisted smoking cessation induction system and in assisting smokers with quitting. The process of e-referrals and direct linkage to online health education resources needs to be more fully explored with dental practices so that the barriers to the e-referrals are better understood. As online resources are effective and available at no cost, strategies to support health providers in utilizing the resources to assist their patients in quitting should be explored. This study also supports the utility of engaging dental practices as a portal of entry into the healthcare system at large, which would allow interventions with a different patient population group than those who visit medical practices.35
Supplementary Material
Acknowledgments
More details about The National Dental PBRN are publicly available at www.NationalDentalPBRN.org and www.DPBRN.org.
The authors would like to recognize the contributions of Anne Hubbell, Ariana Kamberi, and Kathryn Delaughter to the data collection.
This investigation was supported by NIH grants U01-DE-16746, U01-DE-16747, and U19-DE-22516.
Footnotes
Opinions and assertions contained herein are those of the authors and are not to be construed as necessarily representing the views of the respective organizations or the National Institutes of Health. More details about The National Dental PBRN are publicly available at www.NationalDentalPBRN.org and www.DPBRN.org.
No financial disclosures were reported by the authors of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Centers for Disease Control and Prevention. Vital signs: Current cigarette smoking among adults aged > 18 years—United States, 2005–2010. MMWR Morb Mortal Wkly Rep. 2011;60(35):1207–12. [PubMed] [Google Scholar]
- 2.Fiore MC, Croyle RT, Curry SJ, et al. Preventing 3 million premature deaths and helping 5 million smokers quit: a national action plan for tobacco cessation. Am J Public Health. 2004 Feb;94(2):205–10. doi: 10.2105/ajph.94.2.205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Substance Abuse and Mental Health Services Administration. Results from the 2010 National Survey on Drug Use and Health: Summary of National Findings. Substance Abuse and Mental Health Services Administration; 2011. [Google Scholar]
- 4.Bjartveit K, Tverdal A. Health consequences of smoking 1–4 cigarettes per day. Tobacco Control. 2005 Oct;14(5):315–20. doi: 10.1136/tc.2005.011932. Epub 2005/09/27.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leykin Y, Aguilera A, Torres LD, Perez-Stable EJ, Munoz RF. Interpreting the outcomes of automated Internet-based randomized trials: example of an International Smoking Cessation Study. J Med Internet Res. 2012;14(1):e5. doi: 10.2196/jmir.1829. Epub 2012/02/09.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller PM, Heideman PW, Ravenel MC, et al. Preliminary development and evaluation of online tobacco and alcohol modules for dental students. J Dent Educ. 2011 Jun;75(6):791–6. Epub 2011/06/07.eng. [PubMed] [Google Scholar]
- 7.Munoz RF, Lenert LL, Delucchi K, et al. Toward evidence-based Internet interventions: A Spanish/English Web site for international smoking cessation trials. Nicotine Tob Res. 2006 Feb;8(1):77–87. doi: 10.1080/14622200500431940. Epub 2006/02/25.eng. [DOI] [PubMed] [Google Scholar]
- 8.Saul JE, Schillo BA, Evered S, et al. Impact of a statewide Internet-based tobacco cessation intervention. J Med Internet Res. 2007;9(3):e28. doi: 10.2196/jmir.9.4.e28. Epub 2007/10/19.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Murray E, Khadjesari Z, White IR, et al. Methodological challenges in online trials. J Med Internet Res. 2009;11(2):e9. doi: 10.2196/jmir.1052. Epub 2009/05/01.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feil EG, Noell J, Lichtenstein E, Boles SM, McKay HG. Evaluation of an Internet-based smoking cessation program: lessons learned from a pilot study. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2003 Apr;5(2):189–94. doi: 10.1080/1462220031000073694. Epub 2003/05/15.eng. [DOI] [PubMed] [Google Scholar]
- 11.Lenert L, Munoz RF, Perez JE, Bansod A. Automated e-mail messaging as a tool for improving quit rates in an Internet smoking cessation intervention. J Am Med Inform Assoc. 2004 Jul-Aug;11(4):235–40. doi: 10.1197/jamia.M1464. Epub 2004/04/06.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lenert L, Skoczen S. The Internet as a research tool: worth the price of admission? Annals of Behavior Medicine. 2002 Fall;24(4):251–6. doi: 10.1207/S15324796ABM2404_01. Epub 2002/11/19.eng. [DOI] [PubMed] [Google Scholar]
- 13.Munoz RF, Barrera AZ, Delucchi K, Penilla C, Torres LD, Perez-Stable EJ. International Spanish/English Internet smoking cessation trial yields 20% abstinence rates at 1 year. Nicotine Tob Res. 2009 Sep;11(9):1025–34. doi: 10.1093/ntr/ntp090. Epub 2009/07/31.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Houston TK, Richman JS, Ray MN, et al. Internet delivered support for tobacco control in dental practice: randomized controlled trial. J Med Internet Res. 2008;10(5):e38. doi: 10.2196/jmir.1095. Epub 2008/11/06.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wadland WC, Holtrop JS, Weismantel D, Pathak PK, Fadel H, Powell J. Practice-based referrals to a tobacco cessation quit line: assessing the impact of comparative feedback vs general reminders. Ann Fam Med. 2007 Mar-Apr;5(2):135–42. doi: 10.1370/afm.650. Epub 2007/03/29.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dye BA, Morin NM, Robison V. The relationship between cigarette smoking and perceived dental treatment needs in the United States, 1988–1994. J Am Dent Assoc. 2006 Feb;137(2):224–34. doi: 10.14219/jada.archive.2006.0148. Epub 2006/03/09.eng. [DOI] [PubMed] [Google Scholar]
- 17.Rubenstein LV, Pugh J. Strategies for promoting organizational and practice change by advancing implementation research. J Gen Intern Med. 2006 Feb;21(Suppl 2):S58–64. doi: 10.1111/j.1525-1497.2006.00364.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thorpe KE, Zwarenstein M, Oxman AD, et al. A pragmatic-explanatory continuum indicator summary (PRECIS): a tool to help trial designers. J Clin Epidemiol. 2009 May;62(5):464–75. doi: 10.1016/j.jclinepi.2008.12.011. [DOI] [PubMed] [Google Scholar]
- 19.Fiore MC, Bailey WC, Cohen S. Treating Tobacco Use and Dependence: Clinical Practice Guideline 2008. Update 2008. :37. [Google Scholar]
- 20.Sadasivam RS, Delaughter K, Crenshaw K, et al. Development of an interactive, Web-delivered system to increase provider-patient engagement in smoking cessation. J Med Internet Res. 2011;13(4):e87. doi: 10.2196/jmir.1721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.West R, Hajek P, Stead L, Stapleton J. Outcome criteria in smoking cessation trials: proposal for a common standard. Addiction (Abingdon, England) 2005 Mar;100(3):299–303. doi: 10.1111/j.1360-0443.2004.00995.x. Epub 2005/03/01.eng. [DOI] [PubMed] [Google Scholar]
- 22.An LC, Betzner A, Schillo B, et al. The comparative effectiveness of clinic, work-site, phone, and Web-based tobacco treatment programs. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2010 Oct;12(10):989–96. doi: 10.1093/ntr/ntq133. Epub 2010/08/18.eng. [DOI] [PubMed] [Google Scholar]
- 23.Cobb NK, Graham AL, Bock BC, Papandonatos G, Abrams DB. Initial evaluation of a real-world Internet smoking cessation system. Nicotine & tobacco research: official journal of the Society for Research on Nicotine and Tobacco. 2005 Apr;7(2):207–16. doi: 10.1080/14622200500055319. Epub 2005/07/23.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Danaher BG, Smolkowski K, Seeley JR, Severson HH. Mediators of a successful web-based smokeless tobacco cessation program. Addiction (Abingdon, England) 2008 Oct;103(10):1706–12. doi: 10.1111/j.1360-0443.2008.02295.x. Epub 2008/08/22.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Mason D, Gilbert H, Sutton S. Effectiveness of web-based tailored smoking cessation advice reports (iQuit): a randomised trial. Addiction (Abingdon, England) 2012 Jun 12; doi: 10.1111/j.1360-0443.2012.03972.x. Epub 2012/06/14.Eng. [DOI] [PubMed] [Google Scholar]
- 26.McKay HG, Danaher BG, Seeley JR, Lichtenstein E, Gau JM. Comparing two web-based smoking cessation programs: randomized controlled trial. J Med Internet Res. 2008;10(5):e40. doi: 10.2196/jmir.993. Epub 2008/11/20.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Severson HH, Gordon JS, Danaher BG, Akers L. ChewFree.com: evaluation of a Web-based cessation program for smokeless tobacco users. Nicotine Tob Res. 2008 Feb;10(2):381–91. doi: 10.1080/14622200701824984. Epub 2008/02/01.eng. [DOI] [PubMed] [Google Scholar]
- 28.Smolkowski K, Danaher BG, Seeley JR, Kosty DB, Severson HH. Modeling missing binary outcome data in a successful web-based smokeless tobacco cessation program. Addiction (Abingdon, England) 2010 Jun;105(6):1005–15. doi: 10.1111/j.1360-0443.2009.02896.x. Epub 2010/02/13.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Strecher VJ, McClure J, Alexander G, et al. The role of engagement in a tailored web-based smoking cessation program: randomized controlled trial. J Med Internet Res. 2008;10(5):e36. doi: 10.2196/jmir.1002. Epub 2008/11/06.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Strecher VJ, Shiffman S, West R. Moderators and mediators of a web-based computer-tailored smoking cessation program among nicotine patch users. Nic tob res. 2006;8(Suppl 1):S95–S101. doi: 10.1080/14622200601039444. Epub 2007/05/12.eng. [DOI] [PubMed] [Google Scholar]
- 31.Etter JF. Comparing the efficacy of two Internet-based, computer-tailored smoking cessation programs: a randomized trial. J Med Internet Res. 2005;7(1):e2. doi: 10.2196/jmir.7.1.e2. Epub 2005/04/15.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Eysenbach G. The law of attrition. J Med Internet Res. 2005;7(1):e11. doi: 10.2196/jmir.7.1.e11. Epub 2005/04/15.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Makhija SK, Gilbert GH, Rindal DB, et al. Practices participating in a dental PBRN have substantial and advantageous diversity even though as a group they have much in common with dentists at large. BMC Oral Health. 2009;9:26. doi: 10.1186/1472-6831-9-26. Epub 2009/10/17.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Makhija SK, Gilbert GH, Rindal DB, Benjamin PL, Richman JS, Pihlstrom DJ. Dentists in practice-based research networks have much in common with dentists at large: evidence from the Dental Practice-Based Research Network. Gen Dent. 2009 May-Jun;57(3):270–5. Epub 2009/10/13.eng. [PMC free article] [PubMed] [Google Scholar]
- 35.Strauss SM, Alfano MC, Shelley D, Fulmer T. Identifying unaddressed systemic health conditions at dental visits: patients who visited dental practices but not general health care providers in 2008. Am J Public Health. 2012 Feb;102(2):253–5. doi: 10.2105/AJPH.2011.300420. Epub 2012/03/07.eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.