Abstract
Purpose
To examine the effects of various cardiovascular, ocular, and lifestyle factors on retinal vessel diameters over short periods of time.
Methods
Subjects were invited to have photographs of their retina taken at each of 3 study visits. The same eye was photographed each time. The photographs were digitized and the retinal vessel diameters were measured. Measurements from the retinal photographs taken consecutively (at visit 2 and visit 3), and 1, 3, and 4 weeks apart (between visits 1 and 2, 2 and 3, and 1 and 3, respectively) were compared.
Results
There were 63 persons who participated in all study visits and had gradable vessel measurements from all 5 images used in analysis. Correlations for pairs of study visits were high, and decreased slightly with increasing length of the time interval. For photographs taken approximately 3 minutes, 1 week, 3 weeks, and 4 weeks apart, correlations were 0.95, 0.90, 0.91, and 0.86 for central retinal arteriolar equivalent (CRAE) and 0.95, 0.90, 0.91, and 0.87 respectively for central retinal venular equivalent (CRVE). We examined the associations of blood pressure levels, smoking habits, time since last eating, exercising, consuming caffeine, and taking anti-hypertensive medication, and image focus with CRAE and CRVE. We found no consistent pattern of association of any of these characteristics with short-term changes in CRAE and CRVE.
Conclusion
Retinal vessel diameters are stable over short intervals of time and none of the factors studied were consistently associated with change in the diameters of either vessel type.
Introduction
Retinal vessel diameters are associated with many cardiovascular characteristics and ocular characteristics and diseases.1–4 Retinal arteriolar diameters are narrower in persons with hypertension5,6 and retinal venular diameters are wider in persons with diabetes.7 The latter has been attributed to hypoxia. Retinal arteriolar and venular diameters have been shown to change over time.4,8 Age, higher blood pressure, history of cardiovascular disease and chronic kidney disease are associated with narrower retinal venules, while current smoking and white blood cell count (WBC) are associated with wider retinal venules.4 Specific time of imaging in the cardiac cycle affects retinal vessel diameters with differences in retinal vessel diameters of about 10%9 and there may be other physiological factors, such as circadian changes, that influence retinal vessel diameters. In addition, there may be differences in image focus and pupil diameters that could result in the variability of vessel measurements, and these may not have been included in models of associations of retinal vessel diameters and systemic or ocular conditions. This study aims to investigate the extent to which some of these characteristics influence retinal vessel diameters and changes in them over short periods of time.
Materials and Methods
Participants
Volunteers aged 40 years and older were invited to have photographs taken of the retina of a randomly selected eye at 3 separate study visits: baseline, 1 week after the baseline visit, and 4 weeks after the baseline visit. All examinations for an individual were scheduled for the same time of day. The mean difference in start time for 2 examinations for the same participant was 3 ± 33 minutes. Visual acuity was measured and only those with visual acuity better than 20/200 in the study eye were eligible to participate.
Approval for this study was granted by the Institutional Review Board at the University of Wisconsin. Informed consent was obtained from each participant before every examination. The tenets of the Declaration of Helsinki were observed.
Procedures
Questions about factors that were not expected to change significantly over the 4 weeks of the study were asked only at the first visit. These included questions about age, history of current smoking, history of glaucoma and retinal diseases and treatment for them, history of cataract and cataract surgery, and history of cardiovascular disease. At each of the 2 follow-up visits, participants were asked if there was any significant change to their health history. Blood pressure, pulse rate, intraocular pressure, pupil size and axial length were measured at each visit and questions about recent smoking, recent intake of caffeine and food, recent medication use (including anti-hypertensive medications and glaucoma drops) were recorded at each visit. With few exceptions, the same examiner completed each of the 3 examinations on the same study participant. Eye-specific variables (e.g., history of cataract and cataract surgery, history of refractive surgery, intraocular pressure, axial length) were recorded for the study eye.
Intraocular pressure was measured by applanation tonometry using a Goldmann tonometer. Axial length was measured by the Zeiss IOL Master (Carl Zeiss Meditec Inc., Dublin, California, USA). Mean arterial blood pressure (MABP) was defined as systolic blood pressure + (2 × diastolic blood pressure) ÷ 3. Figure 1 describes the type of retinal images captured, the examination questions asked, and the measurements recorded by examiners.
Figure 1.
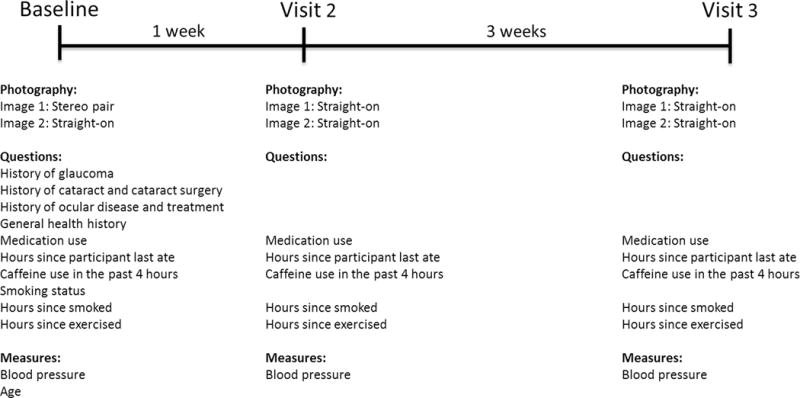
Description of the type of retinal images captured and the characteristics analyzed from each respective study visit.
Retinal Photography
Images for this project were taken of Early Treatment of Diabetic Retinopathy Study field 1 after pupil dilation. Kodak Ektachrome 100 Plus Professional film (Eastman Kodak Company, Rochester, NY) was used. Participants were photographed twice at each of the 3 visits. At the baseline visit, 1 set of stereo images of the study eye were taken to check for pathology, and another image was taken which focused directly on the optic nerve for the best view of the retinal vessels. At the second and third visits, both photographs were taken focused directly on the optic nerve. Because of potential optical differences between the photography styles, only the photographs focused on the optic nerve were used to obtain vessel measurements for this analysis. On average, the 2 study images taken within the same visit were separated by 3.13 ± 0.96 minutes (range: 1 to 7 minutes).
Grading Retinal Vessel Caliber
The film images were digitized into a lossless file format prior to vessel measurement grading. The size and resolution of the images were as follows: width 2529 pixels; height 2337 pixels; resolution 2540 pixels per inch.
Grading of the retinal vessel diameters from the digitized images was done by a trained grader (CDM) who was masked to subject characteristics. He measured retinal arterioles and venules located 0.5 to 1.0 optic disc diameters from the disc margin using a semi-automated computer program (IVAN, University of Wisconsin-Madison; Ferrier NJ). Following a standard protocol, the grader determined each vessel to be an arteriole or venule using the original color photographs for reference. On average, 9 arterioles and 9 venules were measured per eye. Vessel measurements were summarized using measurements from the 6 largest arterioles and 6 largest venules to produce the central retinal arteriolar equivalent (CRAE) and the central retinal venular equivalent (CRVE), respectively.10 Once grading was completed for each eye, screen shots (retinal photograph and all numerical arteriole and venule measurements) were copied and pasted to a Microsoft Word document. This document was saved and used for quality assurance.
Grading Image Focus
Following vessel caliber grading, all images were graded for focus on a scale from 1 to 6 (1 being excellent focus quality, 6 being ungradable) with comparison of focus of a given image against 5 standard photographs of field 1. To create the focus standards, we selected a field 1 image with excellent focus from the Beaver Dam Eye Study11 and then methodically decreased the focus using the Box Blur function in Adobe Photoshop CS2 (Adobe Systems Inc., San Jose, California, USA), which blurs an image based on the average color value of neighboring pixels. The size of the area used to calculate the average value for a given pixel is adjustable; a larger radius results in greater blurring. The image focus quality that we considered borderline gradable had a blur radius of 24 pixels; therefore, we chose this to be the lowest gradable focus standard. Knowing that we wanted a 5-step scale, we determined that a 6-pixel step between levels was most appropriate. That produced the following photographic standards: no blur radius (0 pixels; Standard 1), blur radius = 6 pixels (Standard 2), blur radius = 12 pixels (Standard 3), blur radius = 18 pixels (Standard 4), and blur radius = 24 pixels (Standard 5).
Images were categorized as having excellent focus (better than or equal to Standard 1), good focus (better than or equal to Standard 2 but not as good as Standard 1), fair or worse (better than or equal to standard 3, 4, or 5 but not as good as Standard 2), and ungradable (worse than Standard 5). Generally, images that were graded as equal to Standard 1 or 2 have good enough focus to consider the measurements to be very reliable, images graded as equal to Standard 3 or 4 have compromised quality and the data may be less reliable, and images graded as equal to Standard 5 or 6 have unreliable and ungradable measurements, respectively. Grading of focus was performed independently of the vessel measurements.
Statistical Analysis
Study visits were scheduled so that the second visit occurred 1 week after the first and the third visit occurred 4 weeks after the first. However, in 3 cases, the participant’s schedule required that the 3-week interval be between the first and second visits, and the 1-week interval be between the second and third visits. Except in Table 1, we analyzed the data by the amount of time between the vessel measurements, not the order in which the visits occurred. In cases where few individuals had one value of a covariate (e.g., reporting to have exercised < 12 hours ago), we collapsed the categories in our analyses to improve estimates. SAS version 9.2 was used for all analyses.
Table 1.
Characteristics of the Study Participants.
| Visit 1 | Visit 2 | Visit 3 | ||||
|---|---|---|---|---|---|---|
|
|
||||||
| Characteristic | Total N | N (%) or Mean ± SD | Total N | N (%) or Mean ± SD | Total N | N (%) or Mean ± SD |
| Age, years | 63 | 61.6 ± 9.5 | ||||
| Sex | 63 | |||||
| Women | 48 (76.2) | |||||
| Men | 15 (23.8) | |||||
| Study eye | 63 | |||||
| Right | 35 (55.6) | |||||
| Left | 28 (44.4) | |||||
| CRAE, μm | 63 | 144.0 ± 13.7 | 63 | 144.6 ± 15.4 | 63 | 146.1 ± 15.6 |
| CRVE, μm | 63 | 213.7 ± 21.0 | 63 | 211.6 ± 21.8 | 63 | 213.8 ± 21.3 |
| Time of day examined | 63 | 63 | 63 | |||
| Before 10:00 AM | 19 (30.2) | 20 (31.8) | 21 (33.3) | |||
| Between 10:00 AM and noon | 15 (23.8) | 15 (23.8) | 14 (22.2) | |||
| Between noon and 2:00 PM | 17 (27.0) | 15 (23.8) | 16 (25.4) | |||
| After 2:00 PM | 12 (19.1) | 13 (20.6) | 12 (19.1) | |||
| Image focus quality | 63 | 63 | 63 | |||
| Excellent | 40 (63.5) | 37 (58.7) | 36 (58.1) | |||
| Good | 20 (31.8) | 22 (34.9) | 21 (33.9) | |||
| Fair or worse | 3 (4.8) | 4 (6.4) | 5 (8.1) | |||
| Systolic blood pressure, mmHg | 63 | 133.8 ± 18.7 | 63 | 134.1 ± 20.1 | 63 | 130.2 ± 18.2 |
| Diastolic blood pressure, mmHg | 63 | 78.9 ± 8.9 | 63 | 78.1 ± 9.8 | 63 | 77.1 ± 8.2 |
| Taking antihypertensive medication | 63 | 63 | 63 | |||
| No | 35 (55.6) | 35 (55.6) | 36 (57.1) | |||
| Yes | 28 (44.4) | 28 (44.4) | 27 (42.9) | |||
| Last used antihypertensive medication | 63 | 63 | 63 | |||
| Not taking | 35 (55.6) | 35 (55.6) | 36 (57.1) | |||
| <2 hours ago | 3 (4.8) | 5 (7.9) | 4 (6.4) | |||
| 2 to 12 hours ago | 22 (34.9) | 21 (33.3) | 20 (31.8) | |||
| >12 to 24 hours ago | 3 (4.8) | 1 (1.6) | 2 (3.2) | |||
| >24 hours ago | 0 (0.0) | 1 (1.6) | 1 (1.6) | |||
| Pulse rate, heartbeats per minute | 63 | 74.3 ± 12.4 | 63 | 75.2 ± 13.1 | 63 | 73.1 ± 11.8 |
| Blood oxygen level, % | 63 | 97.1 ± 1.7 | 63 | 97.6 ± 1.9 | 63 | 97.7 ± 1.8 |
| Time since last exercised | 63 | 63 | 63 | |||
| >12 hours | 40 (63.5) | 45 (71.4) | 44 (69.8) | |||
| 4 to 12 hours | 8 (12.7) | 5 (7.9) | 5 (7.9) | |||
| 2 to 3 hours | 3 (4.8) | 3 (4.8) | 3 (4.8) | |||
| < 2 hours | 3 (4.8) | 2 (3.2) | 3 (4.8) | |||
| Not sure | 9 (14.3) | 8 (12.7) | 8 (12.7) | |||
| Currently smoking | 63 | |||||
| No | 60 (95.2) | |||||
| Yes | 3 (4.8) | |||||
| Time since last smoked | 3 | 3 | 3 | |||
| >24 hours | 0 (0.0) | 1 (33.3) | 1 (33.3) | |||
| 12 to 24 hours | 0 (0.0) | 0 (0.0) | 0 (0.0) | |||
| 2 to 12 hours | 1 (33.3) | 1 (33.3) | 1 (33.3) | |||
| <2 hours | 2 (66.7) | 1 (33.3) | 1 (33.3) | |||
| Used caffeine in last 4 hours | 63 | 63 | 63 | |||
| No | 27 (42.9) | 29 (46.0) | 30 (47.6) | |||
| Yes | 36 (57.1) | 34 (54.0) | 33 (52.4) | |||
| Time since last using caffeine | 36 | 34 | 33 | |||
| < 1 hour | 10 (27.8) | 4 (11.8) | 6 (18.2) | |||
| 1 hour | 9 (25.0) | 10 (29.4) | 6 (18.2) | |||
| 2 hours | 10 (27.8) | 7 (20.6) | 9 (27.3) | |||
| 3 hours | 7 (19.4) | 9 (26.5) | 8 (24.2) | |||
| 4 hours | 0 (0.0) | 4 (11.8) | 4 (12.1) | |||
| Glaucoma present | 63 | |||||
| No | 59 (93.7) | |||||
| Yes | 4 (6.4) | |||||
| Using glaucoma drops | 63 | 63 | 63 | |||
| No | 60 (95.2) | 59 (93.7) | 59 (93.7) | |||
| Yes | 3 (4.8) | 4 (6.4) | 4 (6.4) | |||
| Time since last using glaucoma drops | 3 | 4 | 4 | |||
| <2 hours | 1 (33.3) | 2 (50.0) | 2 (50.0) | |||
| 2–12 hours | 2 (66.7) | 2 (50.0) | 2 (50.0) | |||
| >12 hours | 0 (0,0) | 0 (0,0) | 0 (0,0) | |||
| Time since last eating, hours | 63 | 5.2 ± 5.2 | 63 | 5.3 ± 5.4 | 63 | 4.7 ± 4.6 |
CRAE, central retinal arteriolar equivalent; CRVE, central retinal venular equivalent; SD, standard deviation.
Our first study aim was to quantify the amount of variability (or lack thereof) between vessel measurements taken over different time periods. We calculated the correlation between and mean difference in vessel measurements from photographs taken over 4 time periods: consecutive, 1 week, 3 weeks, and 4 weeks (Figure 2 A–D). Because only 1 straight-on image was taken at the baseline visit, comparisons between measurements over 1 week, 3 weeks, and 4 weeks were made using only the second image taken at each visit (Figure 1). Correlation between and difference in measures taken from consecutive photographs were based only on data collected at visit 2.
Figure 2.
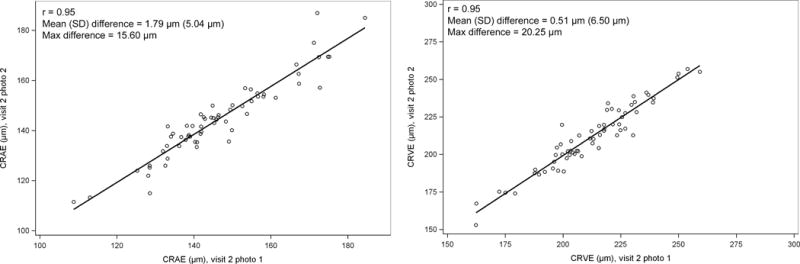
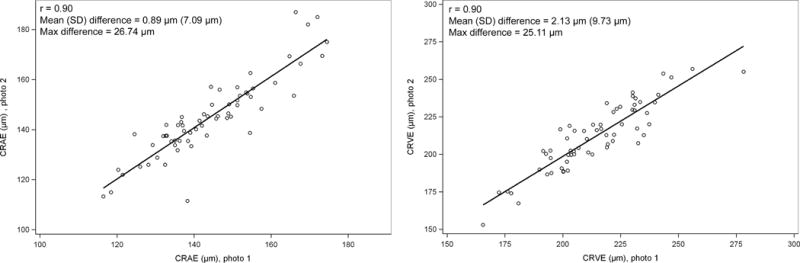
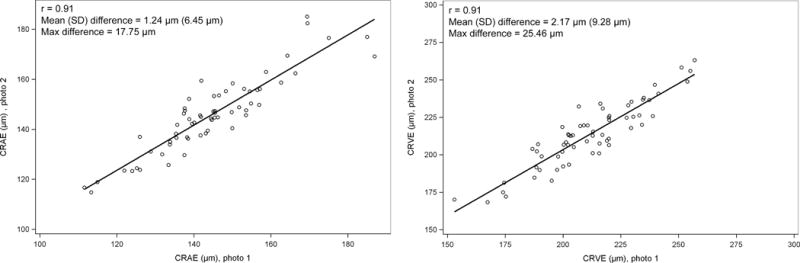
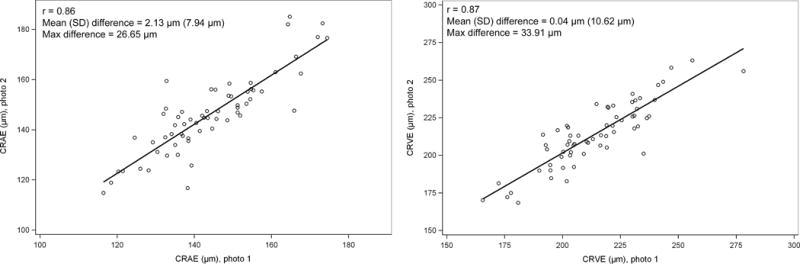
Change in central retinal arteriolar equivalent (CRAE) and central retinal venular equivalent (CRVE) between 2 retinal photographs taken A. approximately 3 minutes apart at the same visit; B. 1 week apart; C. 3 weeks apart; D. 4 weeks apart.
Because we were interested in the amount of change between the two measurements and not the direction of the change (e.g. whether CRAE became smaller or larger), our outcome of interest was the absolute difference in CRAE and CRVE between the two consecutive photographs. We examined the relationship of image focus of the two photographs taken at visit 2 to the absolute difference in CRAE and CRVE measured over 3 minutes visit 2 and similarly examined the relationship of each covariate measured at visit 3 to the absolute difference in CRAE and CRVE at visit 3. To increase power, data from both visit 2 and 3 were analyzed together in generalized estimating equation models accounting for correlation between measurements taken from the same individual using an exchangeable working correlation structure.
To determine if changes in CRAE and CRVE might be related to changes in any of our measured covariates, we calculated the mean change in CRAE and CRVE over 1 week, 3 weeks and 4 weeks stratified by the change in the covariate of interest over the same time interval. This would allow us to answer a question such as, “Do individuals who have an increase in SBP over a 1-week period tend to have a decrease in CRAE over the same period compared to individuals whose blood pressure stays within ± 10 mmHg?” P-values for overall differences in mean CRAE and CRVE between the groups using the “no change” group as a reference were calculated using the score test in Proc Genmod.
Results
Characteristics of Study Participants
Of the 76 individuals seen at the baseline visit, 74 participated in the second visit, and 71 (55 women and 16 men) participated at all 3 visits. Of these, 9 individuals had at least 1 photo where vessels could not be measured due to poor image focus or an artifact that prevented the grader from measuring any of the 6 largest arterioles or venules in the eye, leaving 63 individuals who participated in all 3 visits and had gradable vessel measurement data in all 5 images. The average age of study participants was 61.6 ± 9.5 years. The majority of participants were female (76.2%). Most (n=21) were women aged 60–69 years. The distributions of characteristics of the study group are given in Table 1. Most characteristics were selected because of a potential association with vessel diameters in the eye.
Of the 63 eligible participants, the left eye was the study eye in 28. Two individuals had had refractive surgery; 4 persons had glaucoma (all of whom were taking medications for it, though 1 participant reported taking drops only at the second and third visits); 15 had history of cataract; 3 had cataract surgery with intraocular lens implants; 1 had a history of macular degeneration in the study eye; 5 had been told they had diabetes or were suspected of having diabetes.
Factors Associated with Variability of CRAE and CRVE
CRAE and CRVE measures remained stable over all time periods studied. Correlations were very high and decreased from r = 0.95 for both CRAE and CRVE for photographs taken consecutively to r = 0.86 and r = 0.87 for CRAE and CRVE, respectively, for photographs taken 4 weeks apart. The mean difference in CRAE and CRVE was less than 2.5 μm over all time intervals (Figure 2).
The only factors that were considered for differences in CRAE and CRVE from photographs taken consecutively were age, sex and image focus (Table2). Age and sex had no effect. In consecutive photographs, when both photos had fair or worse focus there was a greater difference in CRAE than when both photos had good or excellent focus (p=0.04).
Table 2.
The Relationship of Covariates to Absolute Differences in Retinal Vessel Measurements from Two Photographs Taken Consecutively.
| Absolute Difference in Vessel Measurements
|
||
|---|---|---|
| Covariate | β estimate (SE)* | P value |
|
|
|
|
| Central Retinal Arteriolar Equivalent | ||
| Age (per 5 years) | 0.20 (0.14) | 0.15 |
| Sex (men vs. women) | 0.69 (0.70) | 0.33 |
| Image focus | ||
| Both photos fair or worse vs. both photos good or excellent | 5.03 (2.51) | 0.04 |
| Photos have different quality vs. both photos good or excellent | −0.07 (0.70) | 0.92 |
| Central Retinal Venular Equivalent | ||
| Age (per 5 years) | −0.02 (0.18) | 0.89 |
| Sex (men vs. women) | 0.09 (1.03) | 0.93 |
| Image focus | ||
| Both photos fair or worse vs. both photos good or excellent | −0.74 (1.23) | 0.54 |
| Photos have different quality vs. both photos good or excellent | 0.69 (0.65) | 0.28 |
SE, standard error.
The mean change in each covariate between visits was small but increased as the time between visits increased. For example, the mean change in systolic blood pressure over 1 week was −0.05 mmHg and the mean change over 4 weeks was −3.69 mmHg (Table 3). Image quality was consistent (nearly always excellent or good) across each pair of visits, as were participant medication use, exercise habits, and caffeine use within the past 4 hours. In cases where a covariate did change between two study visits, there was a borderline significant relationship of change in diastolic blood pressure to change in CRAE over a 1-week interval (P=0.07) and between change in image focus and change in CRAE (P=0.04) and CRVE (P=0.02) over a 4-week interval.
Table 3.
The Relationship of Changes in Covariates to One-, Three-, and Four-Week Changes in Retinal Vessel Measurements.
| One-week change | Three-week change | Four-week change | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| In covariate | In vessel measurement | In covariate | In vessel measurement | In covariate | In vessel measurement | |||||||
|
|
||||||||||||
| Covariate | Mean (SD) | N | Mean (SD) | P | Mean (SD) | N | Mean (SD) | P | Mean (SD) | N | Mean (SD) | P |
|
|
|
|||||||||||
| CRAE | ||||||||||||
| Systolic BP, mmHg | −0.05 (15.01) | 0.41 | −3.64 (14.85) | 0.91 | −3.69 (14.99) | 0.82 | ||||||
| Decreased >10 | 17 | 2.23 (5.53) | 19 | 1.77 (7.07) | 20 | 2.25 (6.91) | ||||||
| Within 10 | 31 | 0.66 (8.69) | 33 | 1.06 (6.39) | 33 | 1.73 (9.15) | ||||||
| Increased >10 | 15 | −0.15 (4.70) | 11 | 0.89 (6.03) | 10 | 3.22 (5.88) | ||||||
| Diastolic BP, mmHg | −0.59 (6.43) | 0.75 | −1.21 (6.66) | 0.07 | −1.79 (7.67) | 0.41 | ||||||
| Decreased >5 | 13 | 1.60 (5.09) | 14 | 1.11 (7.09) | 16 | 4.49 (8.28) | ||||||
| Within 5 | 38 | 0.38 (8.01) | 40 | 2.54 (5.54) | 39 | 1.33 (7.66) | ||||||
| Increased >5 | 12 | 1.73 (6.08) | 9 | −4.30 (6.95) | 8 | 1.31 (8.73) | ||||||
| MABP, mmHg | −0.41 (8.23) | 0.13 | −2.02 (8.30) | 0.27 | −2.43 (9.05) | 0.65 | ||||||
| Decreased >5 | 19 | 2.29 (5.35) | 19 | 1.63 (6.33) | 24 | 2.06 (8.12) | ||||||
| Within 5 | 33 | 0.81 (8.59) | 30 | 2.26 (5.91) | 29 | 1.65 (8.65) | ||||||
| Increased >5 | 11 | −1.30 (3.80) | 14 | −1.47 (7.38) | 10 | 3.71 (5.49) | ||||||
| Intraocular pressure, mmHg | −0.24 (2.64) | 0.85 | 0.13 (2.29) | 0.53 | −0.11 (2.72) | 0.41 | ||||||
| Decreased >1 | 17 | 1.50 (5.87) | 12 | 2.42 (4.82) | 18 | 0.72 (8.57) | ||||||
| Within 1 | 34 | 0.41 (7.55) | 37 | 0.69 (6.69) | 31 | 2.10 (7.83) | ||||||
| Increased >1 | 11 | 1.08 (8.09) | 13 | 2.44 (6.96) | 13 | 4.57 (7.53) | ||||||
| Blood oxygen level, % | 0.49 (1.32) | 0.39 | 0.16 (1.48) | 0.16 | 0.65 (1.37) | 0.37 | ||||||
| Decreased >0.5 | 9 | −1.74 (10.69) | 16 | 2.05 (5.91) | 9 | 0.06 (4.72) | ||||||
| Within 0.5 | 30 | 2.18 (7.57) | 24 | −0.73 (6.45) | 28 | 2.06 (9.96) | ||||||
| Increased >0.5 | 24 | 0.27 (4.25) | 23 | 2.74 (6.54) | 26 | 2.93 (6.33) | ||||||
| Mean pupil diameter, mm | −0.04 (0.46) | 0.63 | 0.13 (0.30) | 0.19 | 0.09 (0.42) | 0.44 | ||||||
| Decreased >0.25 | 12 | −0.27 (11.33) | 5 | −2.13 (4.95) | 9 | 1.32 (3.96) | ||||||
| Within 0.25 | 42 | 1.39 (6.19) | 41 | 2.17 (6.50) | 35 | 1.48 (9.25) | ||||||
| Increased >0.25 | 9 | 0.08 (3.45) | 17 | 0.01 (6.48) | 19 | 3.71 (6.72) | ||||||
| Time since last eating, hours | 0.02 (4.67) | 0.99 | −0.54 (5.46) | 0.46 | −0.52 (4.75) | 0.32 | ||||||
| >1 sooner | 11 | 1.16 (8.80) | 12 | 0.37 (5.98) | 12 | 0.63 (6.40) | ||||||
| Within 1 | 41 | 0.84 (7.49) | 40 | 0.92 (6.60) | 42 | 2.96 (8.95) | ||||||
| >1 later | 11 | 0.80 (3.04) | 11 | 3.38 (6.51) | 9 | 0.28 (3.41) | ||||||
| Image focus | 0.26 | 0.62 | 0.04 | |||||||||
| Worsened | 13 | 2.98 (5.34) | 11 | 2.40 (5.81) | 15 | 2.10 (5.47) | ||||||
| Same | 41 | 0.67 (7.66) | 40 | 1.44 (5.99) | 37 | 3.87 (8.40) | ||||||
| Improved | 9 | −1.13 (6.42) | 12 | −0.48 (8.46) | 11 | −3.67 (6.85) | ||||||
| Time of day examined | 0.36 | 0.74 | 0.71 | |||||||||
| Earlier | 4 | 0.78 (5.85) | 5 | 2.33 (5.28) | 4 | 2.89 (8.94) | ||||||
| Same | 56 | 1.05 (7.36) | 55 | 1.25 (6.63) | 57 | 2.03 (8.08) | ||||||
| Later | 3 | −1.96 (1.89) | 3 | −0.62 (6.22) | 2 | 3.55 (2.21) | ||||||
| Antihypertensive medication use | NA | 0.31 | 0.34 | |||||||||
| Stayed the same | 63 | 0.89 (7.09) | 62 | 1.39 (6.39) | 62 | 2.09 (8.00) | ||||||
| Changed | 0 | NA (NA) | 1 | −8.05 (NA) | 1 | 4.98 (NA) | ||||||
| Last antihypertensive medication use | 0.22 | 0.62 | 0.89 | |||||||||
| Sooner | 5 | 4.78 (5.38) | 4 | −1.95 (8.41) | 3 | 2.55 (2.24) | ||||||
| Same | 56 | 0.46 (7.25) | 54 | 1.28 (6.06) | 58 | 2.13 (8.26) | ||||||
| Later | 2 | 3.17 (3.10) | 5 | 3.43 (9.38) | 2 | 1.50 (3.65) | ||||||
| Amount of time since last exercising | 0.16 | 0.90 | 0.20 | |||||||||
| Less | 10 | 0.36 (3.69) | 7 | 0.66 (10.76) | 11 | 1.06 (3.51) | ||||||
| Same | 42 | 2.19 (6.21) | 46 | 1.46 (6.01) | 39 | 3.48 (8.25) | ||||||
| More | 11 | −3.61 (10.54) | 10 | 0.67 (5.26) | 13 | −0.99 (9.08) | ||||||
| Amount of time since last consuming caffeine | 0.35 | 0.31 | 0.15 | |||||||||
| Less | 8 | 3.79 (8.46) | 7 | −1.23 (4.08) | 8 | 1.38 (11.91) | ||||||
| Same | 45 | 0.10 (7.15) | 48 | 1.73 (6.43) | 44 | 1.07 (6.60) | ||||||
| More | 10 | 2.14 (5.26) | 8 | 0.49 (8.28) | 11 | 6.94 (8.61) | ||||||
| One-week change | Three-week change | Four-week change | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
||||||||||||
| In risk | In vessel measurement | In risk | In vessel measurement | In risk | In vessel measurement | |||||||
|
|
||||||||||||
| Covariate | Mean (SD) | N | Mean (SD) | P | Mean (SD) | N | Mean (SD) | P | Mean (SD) | N | Mean (SD) | P |
|
|
|
|||||||||||
| CRVE | ||||||||||||
| Systolic BP, mmHg | −0.05 (15.01) | 0.19 | −3.64 (14.85) | 0.42 | −3.69 (14.99) | 0.75 | ||||||
| Decreased >10 | 17 | 1.43 (10.97) | 19 | 3.89 (8.21) | 20 | 1.46 (9.80) | ||||||
| Within 10 | 31 | −2.79 (9.58) | 33 | 1.89 (10.37) | 33 | −0.66 (11.29) | ||||||
| Increased >10 | 15 | −4.81 (7.80) | 11 | 0.06 (7.63) | 10 | −0.50 (10.67) | ||||||
| Diastolic BP, mmHg | −0.59 (6.43) | 0.55 | −1.21 (6.66) | 0.74 | −1.79 (7.67) | 0.46 | ||||||
| Decreased >5 | 13 | 0.43 (10.45) | 14 | 0.94 (9.40) | 16 | −0.57 (10.93) | ||||||
| Within 5 | 38 | −2.39 (9.04) | 40 | 2.83 (9.62) | 39 | −0.33 (11.26) | ||||||
| Increased >5 | 12 | −4.09 (11.28) | 9 | 1.17 (8.21) | 8 | 3.09 (6.46) | ||||||
| MABP, mmHg | −0.41 (8.23) | 0.13 | −2.02 (8.30) | 0.35 | −2.43 (9.05) | 0.97 | ||||||
| Decreased >5 | 19 | 1.78 (10.61) | 19 | 3.30 (8.88) | 24 | −0.29 (11.35) | ||||||
| Within 5 | 33 | −3.30 (8.60) | 30 | 2.70 (10.36) | 29 | 0.11 (10.29) | ||||||
| Increased >5 | 11 | −5.40 (10.11) | 14 | −0.47 (7.22) | 10 | 0.64 (10.85) | ||||||
| Intraocular pressure, mmHg | −0.24 (2.64) | 0.35 | 0.13 (2.29) | 0.77 | −0.11 (2.72) | 0.02 | ||||||
| Decreased >1 | 17 | −5.13 (9.42) | 12 | 4.07 (11.16) | 18 | −2.52 (10.82) | ||||||
| Within 1 | 34 | −0.98 (10.13) | 37 | 1.68 (9.24) | 31 | −1.58 (10.16) | ||||||
| Increased >1 | 11 | −1.97 (8.75) | 13 | 2.70 (7.74) | 13 | 7.55 (8.98) | ||||||
| Blood oxygen level, % | 0.49 (1.32) | 0.13 | 0.16 (1.48) | 0.28 | 0.65 (1.37) | 0.10 | ||||||
| Decreased >0.5 | 9 | −3.70 (12.94) | 16 | 3.89 (11.75) | 9 | 1.59 (8.87) | ||||||
| Within 0.5 | 30 | 0.33 (8.57) | 24 | 3.16 (9.39) | 28 | 2.76 (9.75) | ||||||
| Increased >0.5 | 24 | −4.62 (9.43) | 23 | −0.05 (6.94) | 26 | −3.43 (11.40) | ||||||
| Mean pupil diameter, mm | −0.04 (0.46) | 0.23 | 0.13 (0.30) | 0.42 | 0.09 (0.42) | 0.50 | ||||||
| Decreased >0.25 | 12 | −5.30 (8.83) | 5 | 5.23 (10.54) | 9 | 2.99 (8.72) | ||||||
| Within 0.25 | 42 | −0.67 (9.25) | 41 | 1.11 (9.77) | 35 | −1.05 (11.50) | ||||||
| Increased >0.25 | 9 | −4.72 (12.41) | 17 | 3.85 (7.66) | 19 | 0.66 (9.89) | ||||||
| Time since last eating, hours | 0.02 (4.67) | 0.88 | −0.54 (5.46) | 0.58 | −0.52 (4.75) | 0.32 | ||||||
| >1 sooner | 11 | −3.38 (9.78) | 12 | 0.06 (11.01) | 12 | −5.38 (14.58) | ||||||
| Within 1 | 41 | −2.04 (9.27) | 40 | 3.15 (7.84) | 42 | 1.49 (9.16) | ||||||
| >1 later | 11 | −1.24 (12.01) | 11 | 0.93 (12.27) | 9 | 0.51 (9.77) | ||||||
| Image focus | 0.33 | 0.97 | 0.33 | |||||||||
| Worsened | 13 | −2.23 (8.37) | 11 | 2.58 (13.20) | 15 | −1.53 (12.09) | ||||||
| Same | 41 | 0.90 (9.29) | 40 | 2.24 (7.78) | 37 | 1.75 (9.15) | ||||||
| Improved | 9 | −7.61 (12.46) | 12 | 1.59 (10.59) | 11 | −3.56 (12.80) | ||||||
| Time of day examined | 0.14 | 0.52 | 0.18 | |||||||||
| Earlier | 4 | 1.90 (7.09) | 5 | 7.08 (10.04) | 4 | 3.06 (5.42) | ||||||
| Same | 56 | −2.03 (9.98) | 55 | 1.80 (9.14) | 57 | −0.78 (10.50) | ||||||
| Later | 3 | −9.37 (3.06) | 3 | 0.77 (12.08) | 2 | 17.53 (6.67) | ||||||
| Antihypertensive medication use | 0.32 | 0.32 | ||||||||||
| Stayed the same | 63 | −2.13 (9.73) | 62 | 2.10 (9.34) | 62 | −0.05 (10.68) | ||||||
| Changed | 0 | NA (NA) | 1 | 7.03 (NA) | 1 | 5.48 (NA) | ||||||
| Last antihypertensive medication use | 0.21 | 0.44 | 0.64 | |||||||||
| Sooner | 5 | 3.49 (11.73) | 4 | 4.09 (7.96) | 3 | 0.41 (4.39) | ||||||
| Same | 56 | −2.77 (9.63) | 54 | 2.56 (9.23) | 58 | 0.22 (10.91) | ||||||
| Later | 2 | 1.76 (1.36) | 5 | −3.48 (10.64) | 2 | −5.77 (9.71) | ||||||
| Amount of time since last exercising | 0.42 | 0.66 | 0.55 | |||||||||
| Less | 10 | 0.97 (8.45) | 7 | 2.55 (9.13) | 11 | −2.19 (6.93) | ||||||
| Same | 42 | −2.34 (9.84) | 46 | 2.56 (9.78) | 39 | 0.79 (10.89) | ||||||
| More | 11 | −4.17 (10.55) | 10 | 0.15 (7.38) | 13 | −0.30 (12.66) | ||||||
| Amount of time since last consuming caffeine | 0.80 | 0.54 | 0.39 | |||||||||
| Less | 8 | −2.92 (9.65) | 7 | −0.28 (11.54) | 8 | 2.64 (9.14) | ||||||
| Same | 45 | −2.37 (9.96) | 48 | 2.21 (9.54) | 44 | −1.09 (11.04) | ||||||
| More | 10 | −0.41 (9.50) | 8 | 4.12 (5.22) | 11 | 2.67 (9.87) | ||||||
BP, blood pressure; CRAE, central retinal arteriolar equivalent; CRVE, central retinal venular equivalent; MABP, mean arterial blood pressure; NA, not applicable; P, P value; SD, standard deviation.
Discussion
There were few characteristics among those considered that had a significant effect on the change in retinal vessel diameters, and none had a consistent effect at every time interval studied. These characteristics, listed in Tables 2 and 3, were chosen because of their potential to be associated with or causally affect the caliber of small blood vessels. The stability of the retinal vessel diameters is reassuring because it suggests that some of those characteristics may not be accounted for in studies that use retinal vessel diameters as risk indicators for cardiovascular, ocular, or other systemic diseases. We do note, however, that the correlation of retinal vessel diameters between 2 visits diminishes with increasing length of the interval. It is possible that with a sufficiently long interval, the correlation would be quite low. It may take longer than the 4 weeks we studied for covariates such as blood pressure to have an impact on changes in the vessel diameters. Further research to evaluate this phenomenon and to explore methods to compensate for this effect is important to improve the utility of retinal vessel diameters as predictors not only of future retinal vessel diameters but also likely as predictors of disease.
The current study has limitations. The number of study participants that were seen at all visits was relatively small, resulting in limited power for some analyses. Covariates changed simultaneously and such changes might partially cancel the effect of other covariates on change in diameters. The average age of our participants (61.6 ± 9.5 years) limits our inferences to middle and older age adults. It is possible that some of the characteristics we measured might have a greater influence on the vessel diameters in populations with different age distributions. It is also possible that a different sex distribution and racial/ethnic distribution would find different results.
In summary, we have found that retinal vessel diameters change little throughout intervals as long as 4 weeks, and that none of the characteristics we examined, including image focus, had a consistent effect across the intervals.
Acknowledgments
Financial Support: The National Institutes of Health grant EY06594 (R. Klein, B. E. K. Klein) provided funding for entire study, including collection and analyses of data; further support for data analyses was provided by Senior Scientific Investigator Awards from Research to Prevent Blindness, New York, New York (R. Klein, B. E. K. Klein) and a Mentor-Based Postdoctoral Fellowship Award from the American Diabetes Association, Alexandria, Virginia (R. Klein). B. E. K. Klein had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. The organizations that provided funding were in no way involved in the design and conduct of the study, in the collection, analysis, and interpretation of the data, or in the preparation, review, or approval of the manuscript. The content is solely the responsibility of the authors and does not necessarily reflect the official views of the National Eye Institute or the National Institutes of Health.
Footnotes
Conflict of Interest Statement: None of the authors have any proprietary interests or conflicts of interest related to this submission.
This submission has not been published anywhere previously and it is not simultaneously being considered for any other publication.
References
- 1.Wang JJ, Liew G, Klein R, Rochtchina E, Knudtson MD, Klein BE, et al. Retinal vessel diameter and cardiovascular mortality: pooled data analysis from two older populations. Eur Heart J. 2007;28(16):1984–1992. doi: 10.1093/eurheartj/ehm221. [DOI] [PubMed] [Google Scholar]
- 2.Cooper LS, Wong TY, Klein R, Sharrett AR, Bryan RN, Hubbard LD, et al. Retinal microvascular abnormalities and MRI-defined subclinical cerebral infarction: the Atherosclerosis Risk in Communities Study. Stroke. 2006;37(1):82–86. doi: 10.1161/01.STR.0000195134.04355.e5. [DOI] [PubMed] [Google Scholar]
- 3.Wong TY, Shankar A, Klein R, Klein BE, Hubbard LD. Retinal arteriolar narrowing, hypertension, and subsequent risk of diabetes mellitus. Arch Intern Med. 2005;165(9):1060–1065. doi: 10.1001/archinte.165.9.1060. [DOI] [PubMed] [Google Scholar]
- 4.Myers CE, Klein R, Knudtson MD, Lee KE, Gangnon R, Wong TY, et al. Determinants of retinal venular diameter: the Beaver Dam Eye Study. Ophthalmology. 2012;119(12):2563–2571. doi: 10.1016/j.ophtha.2012.06.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wang JJ, Rochtchina E, Liew G, Tan AG, Wong TY, Leeder SR, et al. The long-term relation among retinal arteriolar narrowing, blood pressure, and incident severe hypertension. Am J Epidemiol. 2008;168(1):80–88. doi: 10.1093/aje/kwn100. [DOI] [PubMed] [Google Scholar]
- 6.Hubbard LD, Brothers RJ, King WN, Clegg LX, Klein R, Cooper LS, et al. Methods for evaluation of retinal microvascular abnormalities associated with hypertension/sclerosis in the Atherosclerosis Risk in Communities Study. Ophthalmology. 1999;106(12):2269–2280. doi: 10.1016/s0161-6420(99)90525-0. [DOI] [PubMed] [Google Scholar]
- 7.Klein R, Myers CE, Lee KE, Gangnon R, Klein BE. Changes in retinal vessel diameter and incidence and progression of diabetic retinopathy. Arch Ophthalmol. 2012;130(6):749–755. doi: 10.1001/archophthalmol.2011.2560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Klein R, Myers CE, Knudtson MD, Lee KE, Gangnon R, Wong TY, et al. Relationship of blood pressure and other factors to serial retinal arteriolar diameter measurements over time: the Beaver Dam Eye Study. Arch Ophthalmol. 2012;130(8):1019–1027. doi: 10.1001/archophthalmol.2012.560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Knudtson MD, Klein BE, Klein R, Wong TY, Hubbard LD, Lee KE, et al. Variation associated with measurement of retinal vessel diameters at different points in the pulse cycle. Br J Ophthalmol. 2004;88(1):57–61. doi: 10.1136/bjo.88.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Knudtson MD, Lee KE, Hubbard LD, Wong TY, Klein R, Klein BE. Revised formulas for summarizing retinal vessel diameters. Curr Eye Res. 2003;27(3):143–149. doi: 10.1076/ceyr.27.3.143.16049. [DOI] [PubMed] [Google Scholar]
- 11.Klein R, Klein BE. The Beaver Dam Eye Study: Manual of Operations: Revised. Springfield, VA: National Technical Information Service; 1991. (Report No.: NTIS Publication PB91-149823). [Google Scholar]


