Abstract
BACKGROUND:
Measures of physical function, daily physical activity, and exercise capacity have been proposed for the care of patients with COPD but are not used routinely in daily office care. Gait speed is a powerful and simple measure of physical function in elderly patients and seems to be a promising measure for the daily care of patients with COPD. The objective of this study was to comprehensively evaluate the determinants and factors influencing gait speed in COPD, particularly the association of gait speed with objectively measured physical activity and the most used exercise capacity field test in cardiopulmonary disease: the 6-min walk test (6MWT).
METHODS:
One hundred thirty patients with stable COPD performed two different 4-m gait speed protocols (usual and maximal pace). We modeled gait speed using demographics, lung function, dyspnea, quality of life, physical activity monitoring, exercise capacity, mood, cognitive function, and health-care use.
RESULTS:
Gait speed was independently associated with 6MWT but not with daily physical activity. The correlation between gait speed and 6MWT was high regardless of protocol used (r = 0.77-0.80). Both 6MWT and gait speed shared similar constructs. Gait speed had an excellent ability to predict poor (≤ 350 m) or very poor (≤ 200 m) 6MWT distances (areas under the curve, 0.87 and 0.98, respectively). Gait speed was not independently associated with quality of life, mood, or cognitive function.
CONCLUSIONS:
Gait speed is more indicative of exercise capacity (6MWT) than daily physical activity in COPD. Despite its simplicity, gait speed has outstanding screening properties for detecting poor and very poor 6MWT performance, making it a useful and informative tool for the clinical care of patients with COPD.
Gait speed, or measuring how long it takes for a patient to walk a short distance, takes very little time and space1 and is a proven indicator of physical disability in elderly patients.2 Moreover, gait speed has been proposed as the next vital sign in older adults3 because of its association with health-care use4,5 and survival.6,7 Although daily physical activity and exercise capacity are key factors independently associated with morbidity and mortality in COPD,8‐11 they are not routinely measured in daily office care. Gait speed may be a simple way to assess and screen such important outcomes in COPD.
Although gait speed has been associated with exercise capacity in COPD as measured by the shuttle test,12 knowledge gaps still exist regarding the association of gait speed with numerous clinically meaningful factors in COPD. The relationship between gait speed and daily physical activity level, general perception of health, cognitive function, mindfulness, and mood states is yet to be determined. Additionally, a comprehensive evaluation of the relationship between gait speed and the 6-min walk test (6MWT), the most prevalent field test in cardiopulmonary disease, has not been described.13,14 Therefore, we prospectively evaluated the possible determinants of gait speed in COPD, particularly, two important measures of physical function in COPD: objectively measured daily physical activity and 6MWT.
Materials and Methods
Subjects
Patients were prospectively recruited from an outpatient pulmonary clinic. Inclusion criteria were (1) a diagnosis of COPD based on the GOLD (Global Initiative for Chronic Obstructive Lung Disease) 2011 guidelines,15 (2) age ≥ 18 years, and (3) ability to complete questionnaires. Patients were excluded if they had an unstable respiratory condition 1 month prior to the study or if they had a walking limitation from a significant orthopedic or neurologic disease (limited by pain, unsteadiness, or weakness when walking). The study was approved by the Mayo Foundation Institutional Review Board (12-006156), and informed written consent was obtained from all participants.
Gait Speed Measurements
Gait speed measurements were performed in a flat and unobstructed clinic hallway. Each walk was performed with a 2-m rolling start where the participant is already walking as he or she enters the measuring area (Fig 1).
Figure 1 .
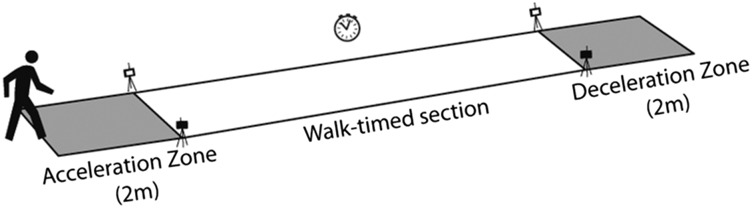
– Gait speed measurement setup.
Usual and Maximal 4-M Gait Speed
Two cones were placed 8 m apart, and an automated timing system was set up 2 m after the first cone and 2 m before the second cone (Fig 1). We used the Dual Beam Wireless Infrared Timing System (TracTronix) set up on 15-cm (6-in) tripods, which provided a 2-m acceleration zone, a 4-m timing area, and a 2-m deceleration zone. To measure usual 4-m gait speed, patients were instructed to walk at a comfortable and natural pace from one cone to the other. To measure maximal 4-m gait speed, patients were instructed to walk as fast as they could safely, without running from one cone to the other. The excellent reliability of this method has been previously described.16
6-Min Walk Test
One 6MWT was performed 15 min after the completion of the 4-m gait speed test according to American Thoracic Society protocol.17 The outcome was distance (in meters) walked in 6 min.
Daily Physical Activity Level
Patients were asked to wear armbands (SenseWear; BodyMedia, Inc)8,10 for 7 days all the time (except for when they showered or swam). The sensor includes a triaxial accelerometer plus other sensors that integrate signals to record energy expenditure. The physical activity level, a recognized measure of physical activity, is calculated by dividing total energy expenditure measured by the basal metabolic rate.10 Levels ≥ 1.7 indicate an active person, 1.69-1.4 indicate a sedentary person, and < 1.4 indicate a very inactive person.18
Other Measures
Demographic information was collected at the initiation of the study, including pulmonary function test results. The BODE (BMI, airflow obstruction, dyspnea, exercise capacity) index score and quartile were calculated for each patient.19 Dyspnea was measured with the modified Medical Research Council (mMRC) dyspnea scale.20,21 Quality of life was measured with the disease-specific Chronic Respiratory Questionnaire (CRQ)22 and a generic tool, the Linear Analog Self-Assessment-6 questionnaire (Likert scales evaluating well-being in six domains: overall quality of life, physical, mental, emotional, social activity, and spiritual).23 We measured depressive symptoms with the Patient Health Questionnaire-2, a validated two-item questionnaire.24 Mindfulness traits were measured by two components of the Five Facet Mindfulness Questionnaire (mind wandering and reactivity to inner thoughts).25 Cognitive function was evaluated with the Digit Symbol Substitution Test (DSST), where the subject copies as many novel symbols corresponding to numbers as possible in 90 s, providing a reliable measure of psychomotor speed, attention, and visual scanning.26‐28 A general survey was also used, addressing smoking status, frequency of COPD exacerbations, and health-care use (number of ED or hospital visits in the prior year).
Statistical Analysis
Statistical analyses were performed by JMP and SAS, version 9.3 (SAS Institute Inc) software. Data are summarized as mean ± SD, median (interquartile range), or percentages. Pearson correlation test (r) with 95% CI was used to evaluate the correlation among the gait speed measurements, physical activity level, and 6MWT. Univariate analysis was performed to identify variables associated with gait speed and 6MWT. The statistically significant univariate variables were then entered into a stepwise multivariate linear model to identify the independent variables influencing gait speed or 6MWT. The capability of gait speed to predict poor exercise capacity (6MWT ≤ 350 m) or very poor exercise capacity (6MWT ≤ 200 m) was evaluated with the C statistic (area under the curve [AUC]) of the logistic models. Bootstrap analysis with 5,000 iterations was performed to validate the logistic model. The sample size calculation was based on the literature, with the expected correlation (r) between 6MWT and gait speed assumed to be 0.714 and the correlation between physical activity level and gait speed assumed to be 0.3.29 We selected the lowest correlation in the sample size calculation. Determined with a probability of type I error (α) of 0.05, power (1 − β) of 0.9, and correlation of 0.3, the calculated sample size was 113, and considering a possible 15% dropout rate, the final sample size was 130.
Results
Baseline demographics for the 130 participants enrolled are shown in Table 1. The severity of COPD was moderate to severe, and on the basis of the combined GOLD COPD assessment,30 58 participants (45%) were in group D, 25 (19%) in group C, 16 (12%) in group B, and 31 (24%) in group A. The average gait speeds were 1.11 ± 0.25 m/s for usual pace and 1.63 ± 0.38 m/s for maximal pace. Eighty-five participants were able to wear the activity monitors for the required time. There were no differences in sex (P = .512), age (P = .935), % FEV1 (P = .767), BMI (P = .226), 6MWT (P = .658), or gait speed (P = .935) between participants who used the physical activity monitor for the required time and those who were unable.
TABLE 1 .
] Demographics
| Demographic | Value |
| No. patients | 130 |
| Male sex | 77 (59) |
| Age, y | 68 ± 10 |
| BMI, kg/m2 | 29 ± 6 |
| FEV1 % predicted | 50 ± 20 |
| mMRC dyspnea scale | 2 ± 1 |
| 6MWT distance, m | 410 ± 120 |
| PALa | 1.4 ± 0.3 |
| BODE index | 3.6 ± 2.8 |
| Supplemental oxygen use | 22 (17) |
Data are presented as No. (%) or mean ± SD unless otherwise indicated. 6MWT = 6-min walk test; BODE = BMI, obstruction, dyspnea, and exercise; mMRC = modified Medical Research Council; PAL = physical activity level.
Calculated as total energy expenditure/resting metabolic rate.
Correlations Between Gait Speed Measures and Physical Activity
The univariate analysis identified a statistically significant association between usual and maximal gait speed and physical activity level (P = .025 and P = .011, respectively). However, the Pearson correlation between usual and maximal gait speed and physical activity level was only modest (r = 0.24 [95% CI, 0.03-0.43] and r = 0.28 [95% CI, 0.07-0.46], respectively).
Correlations Between Gait Speed Measures and 6MWT
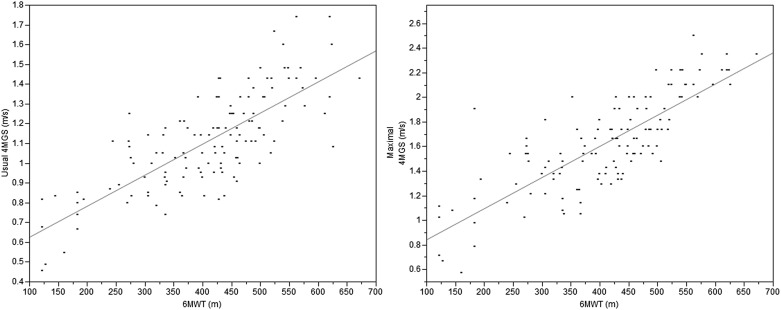
The Pearson correlation between usual and maximal gait speed with 6MWT was very good (r = 0.77 [95% CI, 0.66-0.85; P < .001] and r = 0.80 [95% CI, 0.70-0.87; P < .001], respectively) (Fig 2). The internal validity of the correlations was confirmed by bootstrap modeling, showing identical correlations and CIs as the original cohort.
Figure 2 .
– Correlation between 6MWT and usual and maximal 4MGS. 4MGS = 4-m gait speed; 6MWT = 6-min walk test.
Prediction of Poor and Very Poor 6MWT Distances
Usual 4-m gait speed was excellent in predicting poor exercise capacity (6MWT ≤ 350 m) or very poor exercise capacity (6MWT ≤ 200 m), with an AUC of 0.87 (95% CI, 0.80-0.92) and 0.98 (95% CI, 0.94-0.99), respectively. Validation with bootstrap analysis (5,000 iterations) confirmed the results, with an AUC of 0.87 (95% CI, 0.80-0.93) for 6MWT < 350 m and 0.98 (95% CI, 0.96-1.00) for 6MWT < 200 m. For the prediction of poor exercise capacity (6MWT ≤ 350 m), a usual 4-m gait speed of 0.9 m/s had a sensitivity and specificity of 64% and 90%, respectively, yielding a positive predictive value of 72% and a negative predictive value of 87%. For the prediction of very poor exercise capacity (6MWT ≤ 200 m), a usual 4-m gait speed of 0.8 m/s had a sensitivity and specificity of 82% and 97%, respectively, yielding a positive predictive value of 69% and a negative predictive value of 98%.
Construct and Determinants of Gait Speed
The univariate linear regression model identified numerous significant associations between usual gait speed and clinical outcomes (Table 2). The first stepwise multivariate linear model with all significant univariate variables included only 6MWT as an independent determinant of usual 4-m gait speed because of the strength of association between gait speed and 6MWT (r2 = 0.60). When the model was repeated excluding 6MWT (to evaluate whether the construct of gait speed was similar to the one of 6MWT), the strongest determinants of gait speed were diffusing capacity of lung for carbon monoxide (Dlco) percent, mMRC dyspnea scale, age, and CRQ fatigue scale. Physical activity level and health-care use were not significant determinants of gait speed on multivariate analysis.
TABLE 2 .
] Univariate Associations Between Usual Gait Speed and Clinical Outcomes
| Characteristic | P Value |
| Sex | .296 |
| Age | < .001 |
| BMI | .228 |
| FEV1 % predicted | .003 |
| Dlco % predicted | < .001 |
| mMRC dyspnea scale | < .001 |
| CRQ dyspnea | < .001 |
| CRQ fatigue | < .001 |
| CRQ emotion | .016 |
| CRQ mastery | .002 |
| Mean PAL | .025 |
| Average steps/d | < .001 |
| DSST | < .001 |
| ED visit history | .026 |
| Hospitalization history | < .001 |
| Exacerbation history | .046 |
| PHQ-2 | .032 |
| Mind wandering score | .358 |
| Reactivity to inner thoughts score | .254 |
| General QoL measure (LASA-6) | .092 |
CRQ = Chronic Respiratory Questionnaire; Dlco = diffusing capacity of lung for carbon monoxide; DSST = Digit Symbol Substitution Test; LASA-6 = Linear Analog Self-Assessment-6; PHQ-2 = Patient Health Questionnaire-2; QoL = quality of life. See Table 1 legend for expansion of other abbreviations.
Construct and Determinants of 6MWT
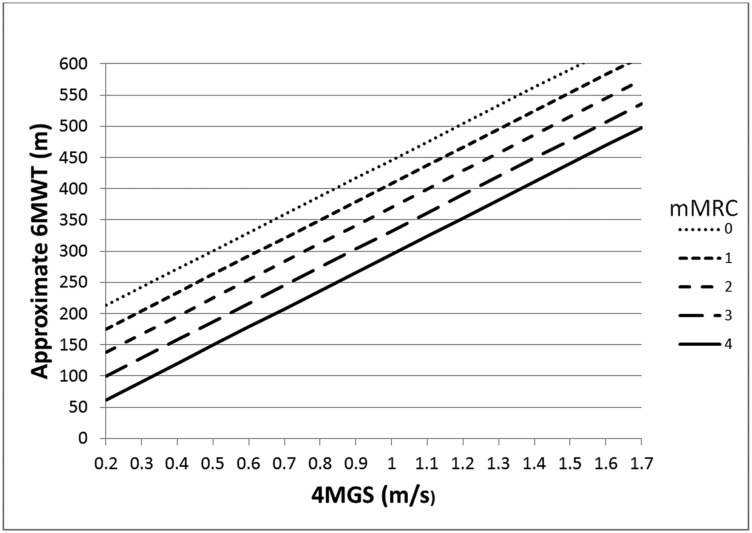
The stepwise multivariate linear regression model included gait speed, mMRC dyspnea scale, % FEV1, DSST, and %Dlco as independent determinants of 6MWT, generating an r2 of 0.75 (Table 3). Gait speed was the strongest determinant of 6MWT, explaining 60% of the variance (r2 = 0.60). When the model was repeated excluding gait speed (to evaluate whether the construct of 6MWT was similar to the one of gait speed), the primary determinants of 6MWT were mMRC dyspnea scale, %Dlco, DSST, Patient Health Questionnaire-2, and age. By modeling 6MWT using only the two strongest determinants (gait speed and mMRC dyspnea scale), we were able to create a graph (Fig 3) that can be used in daily practice to approximate 6MWT (r2 = 0.67).
TABLE 3 .
] Determinants of 6MWT Distance
| Determinant | Estimate | P Value |
| Usual gait speed | 216.9 ± 29.2 | < .001 |
| mMRC dyspnea scale | −28.7 ± 6.2 | < .001 |
| Dlco % predicted | 1.0 ± 0.3 | .005 |
| DSST | 1.2 ± 0.5 | .011 |
| FEV1 % predicted | 0.9 ± 0.3 | .011 |
Figure 3 .
– Approximate 6MWT distance using usual 4MGS and the mMRC dyspnea scale. mMRC = modified Medical Research Council. See Figure 2 legend for expansion of other abbreviations.
Discussion
The main finding of this study is that gait speed is not independently associated with objectively measured daily physical activity in COPD but is strongly and independently associated with exercise capacity as measured by 6MWT, regardless of pace instructions (maximal or usual gait speed). We found that gait speed may be an easy-to-use and clinically relevant screening tool for poor and very poor exercise capacity in routine COPD office practice. The gait speed benchmarks of 0.9 and 0.8 m/s can provide clinicians with useful information to assess patients with COPD because they inform about poor (6MWT < 350 m)31 and very poor (6MWT < 200 m)32,33 exercise capacity. This simple measure may provide guidance on the need to perform a 6MWT, trigger discussion regarding referral for pulmonary rehabilitation, or help the clinician in overall patient assessment.
We extend the findings of a recent report12 stating the association between gait speed and the shuttle walk test as a measure of exercise capacity by investigating the determinants of gait speed and evaluating a more comprehensive set of variables believed to influence gait speed, including objectively measured physical activity and one of the most commonly implemented measures of exercise capacity, the 6MWT. The value of 6MWT in daily office care of COPD, and for that matter in cardiopulmonary disease, is unquestionable.11,34‐38 The 6MWT is used regularly in pulmonary rehabilitation programs and research but is not routinely obtained during daily clinic and office visits due to time, space, and equipment requirements.17 Gait speed is simple and feasible, allowing for repeat measures (every clinic visit), and could provide clinicians with a trend over time. Our group and others have previously demonstrated that a decline in gait speed and 6MWT over time is a strong independent predictor of short-term survival in severe COPD.36,39
Figure 3 and the thresholds of 0.9 and 0.8 m/s are not intended to predict exact measures of 6MWT or to replace 6MWT; instead, they provide a simple and inexpensive screening test for poor and very poor exercise capacity, respectively. We found that those gait speeds have a strong negative predictive value (ideal for a screening test) to identify clinically meaningful thresholds of 6MWT while fulfilling numerous criteria for screening tests, including simple to perform, inexpensive, reliable, and accurate.3,40 The current finding that the usual gait speed of 0.8 m/s is associated with very poor exercise capacity is novel in the field of COPD because prior research in this population has used values based on expert consensus groups.12 The current findings are consistent with prior studies for other disease states.41 In a large review of gait speed in numerous disease cohorts, the most commonly used cut point for adverse health outcomes was a usual gait speed of 0.8 m/s.41
It is important to emphasize that beyond the value of a single gait speed measure, we also suspect that further meaningful information will come from the trend in gait speed over time, as has been shown both in COPD39 and in other groups.7 The simple 4-m gait speed measures have been easily implemented in our outpatient clinic and in other outpatient settings.1,16 We believe that the minimal space requirements and short time of administration are key in the feasibility and use of the measurement.
This work adds to the field of COPD outcome assessment because we comprehensively investigated multiple possible determinants and factors influencing gait speed. To our knowledge, this study is the first in COPD to look at the relationship between gait speed and daily physical activity, cognitive function, depression, and quality of life (generic and disease specific). The findings highlight unique and important pertinent negatives, particularly for objectively measured daily physical activity.
Daily physical activity level is an increasingly studied predictor of mortality in COPD,8 and the relationship between daily physical activity and the described gait speed protocols have not been previously evaluated in a COPD cohort. We found a significant univariate association between physical activity level and gait speed (P = .025). However, it became clear based on the multivariate models that gait speed does not independently inform about daily physical activity, which is a novel finding of this study.
The results also indicate that maximal and usual gait speeds are equally informative of exercise capacity, an important practical finding from our work. To our knowledge, this study is the first to investigate the differential value of usual vs maximal 4-m gait speed in relation to clinical outcomes in COPD.13,14 In the current study, the maximal gait speed was, on average, 0.50 m/s faster than the usual gait speed, which contrasts a previous report12 that assumed that usual gait speed would be close to maximal speed in symptomatic patients with COPD and, therefore, did not measure maximal gait speed.
Finally, we identified several seminal, significant relationships on univariate analysis for further research in gait speed. The significant univariate association between cognitive function with gait speed and 6MWT in COPD is a novel finding. This result suggests that 6MWT and gait speed provide insight into other domains of COPD and may represent overall markers of well-being. Cognitive dysfunction is becoming recognized as an important comorbidity in COPD42 linked to mortality in patients with stable COPD, worse health status, and increased hospital length of stay during COPD exacerbations.43,44
The strong univariate association with all four CRQ domains again shows that gait speed is an informative measure in COPD. Gait speed was also slower for patients with increased health-care use (ED visits and hospitalizations). The association between gait speed and important clinical outcomes in COPD, as in other disease states, provides a further basis for the use of gait speed as a screening measure of overall well-being.
Limitations
The main limitation of this study is that we found several significant determinants of gait speed on univariate analysis that were not significant in the multivariate model. This suggests that a larger cohort may further show the impact and richness of gait speed in other domains of COPD.
Conclusions
Gait speed may be used as a screening measure of poor exercise capacity but is not informative of daily physical activity in COPD. Usual 4-m gait speed is a simple measure with a similar construct as 6MWT and is accurate in detecting poor and very poor 6MWT, which makes it a powerful and informative tool in the routine clinical care of COPD.
Acknowledgments
Author contributions: R. P. B. served as principal investigator, had full access to all of the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. C. K., Z. S. D., N. K. L., and R. P. B. contributed to study design; C. K. and R. P. B. contributed to data collection; C. K., Z. S. D., and R. P. B. contributed to data analysis; P. J. N. contributed to statistical analysis; and C. K., Z. S. D., N. K. L., P. J. N., and R. P. B. contributed to the writing of the manuscript.
Financial/nonfinancial disclosures: The authors have reported to CHEST that no potential conflicts of interest exist with any companies/organizations whose products or services may be discussed in this article.
Role of sponsors: The sponsor had no role in the design of the study, the collection and analysis of the data, or the preparation of the manuscript.
Other contributions: The authors thank Marnie M. Wetzstein, RN; Johanna P. Hoult; and the Mayo Clinic Pulmonary Function Laboratory for assistance with logistical management and recruitment for the study. The authors also thank Molly E. McMahon from the Mayo Clinic Center for Innovation for creating the gait speed illustration used in this manuscript.
ABBREVIATIONS
- 6MWT
6-min walk test
- AUC
area under the curve
- CRQ
Chronic Respiratory Questionnaire
- Dlco
diffusing capacity of lung for carbon monoxide
- DSST
Digit Symbol Substitution Test
- mMRC
modified Medical Research Council
Footnotes
Part of this article has been presented in poster form at the American Thoracic Society International Conference, May 17-22, 2013, Philadelphia, PA.
FUNDING/SUPPORT: This work was supported by the National Heart, Lung, and Blood Institute of the National Institutes of Health [Grant 5R01HL094680-05 to Dr Benzo].
Reproduction of this article is prohibited without written permission from the American College of Chest Physicians. See online for more details.
References
- 1.Studenski S, Perera S, Wallace D, et al. Physical performance measures in the clinical setting. J Am Geriatr Soc. 2003;51(3):314-322 [DOI] [PubMed] [Google Scholar]
- 2.Cesari M, Kritchevsky SB, Penninx BWHJ, et al. Prognostic value of usual gait speed in well-functioning older people—results from the Health, Aging and Body Composition Study. J Am Geriatr Soc. 2005;53(10):1675-1680 [DOI] [PubMed] [Google Scholar]
- 3.Fritz S, Lusardi M. White paper: “walking speed: the sixth vital sign.” J Geriatr Phys Ther. 2009;32(2):46-49 [PubMed] [Google Scholar]
- 4.Montero-Odasso M, Schapira M, Soriano ER, et al. Gait velocity as a single predictor of adverse events in healthy seniors aged 75 years and older. J Gerontol A Biol Sci Med Sci. 2005;60(10):1304-1309 [DOI] [PubMed] [Google Scholar]
- 5.Ostir GV, Berges I, Kuo YF, Goodwin JS, Ottenbacher KJ, Guralnik JM. Assessing gait speed in acutely ill older patients admitted to an acute care for elders hospital unit. Arch Intern Med. 2012;172(4):353-358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Studenski S, Perera S, Patel K, et al. Gait speed and survival in older adults. JAMA. 2011;305(1):50-58 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hardy SE, Perera S, Roumani YF, Chandler JM, Studenski SA. Improvement in usual gait speed predicts better survival in older adults. J Am Geriatr Soc. 2007;55(11):1727-1734 [DOI] [PubMed] [Google Scholar]
- 8.Waschki B, Kirsten A, Holz O, et al. Physical activity is the strongest predictor of all-cause mortality in patients with COPD: a prospective cohort study. Chest. 2011;140(2):331-342 [DOI] [PubMed] [Google Scholar]
- 9.Garcia-Aymerich J, Lange P, Benet M, Schnohr P, Antó JM. Regular physical activity reduces hospital admission and mortality in chronic obstructive pulmonary disease: a population based cohort study. Thorax. 2006;61(9):772-778 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Watz H, Waschki B, Meyer T, Magnussen H. Physical activity in patients with COPD. Eur Respir J. 2009;33(2):262-272 [DOI] [PubMed] [Google Scholar]
- 11.Polkey MI, Spruit MA, Edwards LD, et al. ; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Study Investigators. Six-minute-walk test in chronic obstructive pulmonary disease: minimal clinically important difference for death or hospitalization. Am J Respir Crit Care Med. 2013;187(4):382-386 [DOI] [PubMed] [Google Scholar]
- 12.Kon SS, Patel MS, Canavan JL, et al. Reliability and validity of the 4-metre gait speed in COPD. Eur Respir J. 2013;42(2):333-340 [DOI] [PubMed] [Google Scholar]
- 13.Ilgin D, Ozalevli S, Kilinc O, Sevinc C, Cimrin AH, Ucan ES. Gait speed as a functional capacity indicator in patients with chronic obstructive pulmonary disease. Ann Thorac Med. 2011;6(3):141-146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andersson M, Moberg L, Svantesson U, Sundblom A, Johansson H, Emtner M. Measuring walking speed in COPD: test-retest reliability of the 30-metre walk test and comparison with the 6-minute walk test. Prim Care Respir J. 2011;20(4):434-440 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Vestbo J, Hurd SS, Rodriguez-Roisin R.The 2011 revision of the global strategy for the diagnosis, management and prevention of COPD (GOLD)–why and what? Clin Respir J. 2012;6(4):208-214 [DOI] [PubMed] [Google Scholar]
- 16.Karpman C, LeBrasseur NK, DePew ZS, Novotny PJ, Benzo RP. Measuring gait speed in the out-patient clinic: methodology and feasibility. Respir Care. 2014;59(4):531-537 [DOI] [PubMed] [Google Scholar]
- 17.ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: guidelines for the six-minute walk test. Am J Respir Crit Care Med. 2002;166(1):111-117 [DOI] [PubMed] [Google Scholar]
- 18.Manini TM, Everhart JE, Patel KV, et al. Daily activity energy expenditure and mortality among older adults. JAMA. 2006;296(2):171-179 [DOI] [PubMed] [Google Scholar]
- 19.Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005-1012 [DOI] [PubMed] [Google Scholar]
- 20.Bestall JC, Paul EA, Garrod R, Garnham R, Jones PW, Wedzicha JA. Usefulness of the Medical Research Council (MRC) dyspnoea scale as a measure of disability in patients with chronic obstructive pulmonary disease. Thorax. 1999;54(7):581-586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hajiro T, Nishimura K, Tsukino M, Ikeda A, Koyama H, Izumi T. Analysis of clinical methods used to evaluate dyspnea in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1998;158(4):1185-1189 [DOI] [PubMed] [Google Scholar]
- 22.Aaron SD, Vandemheen KL, Clinch JJ, et al. Measurement of short-term changes in dyspnea and disease-specific quality of life following an acute COPD exacerbation. Chest. 2002;121(3):688-696 [DOI] [PubMed] [Google Scholar]
- 23.Locke DE, Decker PA, Sloan JA, et al. Validation of single-item linear analog scale assessment of quality of life in neuro-oncology patients. J Pain Symptom Manage. 2007;34(6):628-638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Löwe B, Kroenke K, Gräfe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2). J Psychosom Res. 2005;58(2):163-171 [DOI] [PubMed] [Google Scholar]
- 25.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27-45 [DOI] [PubMed] [Google Scholar]
- 26.Lowry KA, Brach JS, Nebes RD, Studenski SA, VanSwearingen JM. Contributions of cognitive function to straight- and curved-path walking in older adults. Arch Phys Med Rehabil. 2012;93(5):802-807 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Rosano C, Newman AB, Katz R, Hirsch CH, Kuller LH. Association between lower digit symbol substitution test score and slower gait and greater risk of mortality and of developing incident disability in well-functioning older adults. J Am Geriatr Soc. 2008;56(9):1618-1625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Inzitari M, Newman AB, Yaffe K, et al. Gait speed predicts decline in attention and psychomotor speed in older adults: the health aging and body composition study. Neuroepidemiology. 2007;29(3-4):156-162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DePew ZS, Karpman C, Novotny PJ, Benzo RP. Correlations between gait speed, 6-minute walk distance, physical activity, and self-efficacy in patients with severe chronic lung disease. Respir Care. 2013;58(12):2113-2119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vestbo J, Hurd SS, Agustí AG, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: GOLD executive summary. Am J Respir Crit Care Med. 2013;187(4):347-365 [DOI] [PubMed] [Google Scholar]
- 31.Spruit MA, Watkins ML, Edwards LD, et al. ; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Study Investigators. Determinants of poor 6-min walking distance in patients with COPD: the ECLIPSE cohort. Respir Med. 2010;104(6):849-857 [DOI] [PubMed] [Google Scholar]
- 32.Szekely LA, Oelberg DA, Wright C, et al. Preoperative predictors of operative morbidity and mortality in COPD patients undergoing bilateral lung volume reduction surgery. Chest. 1997;111(3):550-558 [DOI] [PubMed] [Google Scholar]
- 33.Lederer DJ, Arcasoy SM, Wilt JS, D’Ovidio F, Sonett JR, Kawut SM. Six-minute-walk distance predicts waiting list survival in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med. 2006;174(6):659-664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Spruit MA, Polkey MI, Celli B, et al. ; Evaluation of COPD Longitudinally to Identify Predictive Surrogate Endpoints (ECLIPSE) Study Investigators. Predicting outcomes from 6-minute walk distance in chronic obstructive pulmonary disease. J Am Med Dir Assoc. 2012;13(3):291-297 [DOI] [PubMed] [Google Scholar]
- 35.Paggiaro PL, Dahle R, Bakran I, Frith L, Hollingworth K, Efthimiou J; International COPD Study Group. Multicentre randomised placebo-controlled trial of inhaled fluticasone propionate in patients with chronic obstructive pulmonary disease. Lancet. 1998;351(9105):773-780 [DOI] [PubMed] [Google Scholar]
- 36.Pinto-Plata VM, Cote C, Cabral H, Taylor J, Celli BR. The 6-min walk distance: change over time and value as a predictor of survival in severe COPD. Eur Respir J. 2004;23(1):28-33 [DOI] [PubMed] [Google Scholar]
- 37.Miyamoto S, Nagaya N, Satoh T, et al. Clinical correlates and prognostic significance of six-minute walk test in patients with primary pulmonary hypertension. Comparison with cardiopulmonary exercise testing. Am J Respir Crit Care Med. 2000;161(2 pt 1):487-492 [DOI] [PubMed] [Google Scholar]
- 38.Opasich C, Pinna GD, Mazza A, et al. Six-minute walking performance in patients with moderate-to-severe heart failure; is it a useful indicator in clinical practice? Eur Heart J. 2001;22(6):488-496 [DOI] [PubMed] [Google Scholar]
- 39.Benzo R, Siemion W, Novotny P, et al. ; National Emphysema Treatment Trial Research Group. Factors to inform clinicians about the end of life in severe chronic obstructive pulmonary disease. J Pain Symptom Manage. 2013;46(4):491-499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Herman CR, Gill HK, Eng J, Fajardo LL. Screening for preclinical disease: test and disease characteristics. AJR Am J Roentgenol. 2002;179(4):825-831 [DOI] [PubMed] [Google Scholar]
- 41.Abellan van Kan G, Rolland Y, Andrieu S, et al. Gait speed at usual pace as a predictor of adverse outcomes in community-dwelling older people an International Academy on Nutrition and Aging (IANA) Task Force. J Nutr Health Aging. 2009;13(10):881-889 [DOI] [PubMed] [Google Scholar]
- 42.Li J, Huang Y, Fei GH. The evaluation of cognitive impairment and relevant factors in patients with chronic obstructive pulmonary disease. Respiration. 2013;85(2):98-105 [DOI] [PubMed] [Google Scholar]
- 43.Dodd JW, Charlton RA, van den Broek MD, Jones PW. Cognitive dysfunction in patients hospitalized with acute exacerbation of COPD. Chest. 2013;144(1):119-127 [DOI] [PubMed] [Google Scholar]
- 44.Antonelli-Incalzi R, Corsonello A, Pedone C, et al. Drawing impairment predicts mortality in severe COPD. Chest. 2006;130(6):1687-1694 [DOI] [PubMed] [Google Scholar]