Abstract
Background
Concurrent sexual partnerships can increase sexually transmitted diseases (STD) transmission on a population level. However, different concurrency types may be associated with differential risk for transmission. To investigate this, we describe the prevalence and correlates of four specific concurrency types.
Methods
Between 2001 and 2004, 1098 young adults attending 3 STD clinics were interviewed and tested for STDs. Characteristics associated with concurrency types were identified using logistic regression.
Results
Approximately one-third of respondents reported reactive (34%), transitional (36%), compensatory (32%), and experimental (26%) concurrency. Among men, reactive concurrency was associated with not identifying as heterosexual, drug use, and having sex the same day as meeting a partner. Among women, reactive concurrency was associated with African American race and having >3 lifetime partners. Transitional concurrency was associated with >3 lifetime partners for men and women. Among men, compensatory was associated with African American race; whereas, among women there were no associations with compensatory concurrency. Among men, experimental concurrency was associated with >3 lifetime partners and having sex the same day as meeting a partner. Among women, experimental concurrency was associated with not identifying as heterosexual, drug use, and having sex the same day as meeting a partner.
Conclusions
All concurrency types were common in this population and each was associated with a set of demographic and risk factors. Reactive and experimental concurrency types were associated with other high-risk behaviors, such as drug use.
Introduction
A concurrent sexual partnership is one in which one or both of the members have other sex partners while continuing sexual activity with the original partner.(1) Concurrency may play a role in potentiating the spread of sexually transmitted infections (STIs) such as chlamydial infections,(2) gonorrhea,(3) syphilis(4) and HIV infection(1, 5, 6) at the population level in some populations. The prevalence of concurrency ranges from 11-54%, depending on the study population and measure employed. In the National Survey of Family Growth (NSFG), 12% of U.S. women 15-44 years of age(7) and approximately 25% of those women who reported >2 lifetime sex partners(8) reported concurrent sex partners during the preceding 5 years. Concurrency was reported more often by males than by females in urban adults,(9) and prevalence of concurrency during the preceding year among men participating in the NSFG was 11%.(10) The prevalence of concurrency among adolescents participating in Waves I and II of the National Longitudinal Study of Adolescent Health was 54% in the preceding 3 years among those reporting at least two sexual partners(11), whereas the 6-month prevalence of concurrency among adolescents in San Francisco was 31%.(12) These varying estimates of concurrency prevalence are partly explained by inconsistent definitions of concurrency. The time frame varies as well as the method of obtaining the information; i.e. direct question versus indirect ascertainment by asking the start and end dates of all relationships.(13) Recently a UNAIDS working group developed a consensus definition of concurrency that standardizes the time frame and method of obtaining concurrency information(14), which should provide for more comparable assessments in the future.
Individuals who had concurrent partners were at higher risk of transmitting STIs in some studies after adjusting for the number of partners.(2) Moreover, among individuals with comparable numbers of recent sex partners, those whose partners had concurrent sex partners or those who did not know their partner's concurrency status were at increased risk of STI.(15) Modeling studies have also demonstrated that concurrent sexual partners as opposed to serial partners results in more rapid spread of HIV.(1, 16) Thus, concurrency has been associated not only with transmission and prevalence of STI at the individual and partnership level, but also at the population level. Despite this evidence, some have questioned the role of concurrency in the spread of HIV/STIs(17), sparking an intense debate as to the relevance of sex partner concurrency. On one side of the debate are questions about the plausibility of the assumptions made in the mathematical models simulating concurrency and assertions that there is no evidence demonstrating concurrency is higher in sub-Saharan Africa where HIV prevalence is high than in parts of the world with lower HIV prevalence. On the other side of the debate is evidence that the weaknesses of the first simulation models have been addressed (18, 19) and that partner rather than individual concurrency is associated with STI/HIV acquisition. In addition, some modeling (20) and empirical studies (21) suggest that some forms of concurrency may actually be protective, such as polygamy. This concept supports the hypothesis that not all concurrency is the same.
Our initial study of concurrency patterns collected qualitative data from STD clinic patients and members of high and low STI prevalence communities in Seattle, WA.(22) A taxonomy of concurrent partnerships emerged consisting of five types: transitional, reactive, compensatory, experimental and reciprocal (Table 1). Transitional concurrency was defined as an overlapping partnership that occurred when a committed relationship was ending and one of the partners began a second partnership while the first was still ongoing. Reactive concurrency occurred when one partner discovered that the other had been non-monogamous and then had sex with someone else in retaliation. Compensatory concurrency occurred when an individual sought an additional partner to compensate for some perceived deficiency in a primary relationship. Experimental concurrency was defined as having several overlapping, non-committed, short-term relationships. Finally, reciprocal concurrency occurred when both partners mutually agreed to see outside people (this was not assessed here and is not discussed further). These types of concurrency may have different effects on the transmission of STIs due to variation in length of overlap and potential differences in condom use patterns. Concurrent partnerships with longer overlap likely have a greater impact on the spread of STIs than those with shorter overlaps.(23) Additionally, condom use was more common in experimental concurrency than in either “contained” (similar to reactive or compensatory) or transitional concurrency in analyses of the 2002 NSFG.(24) This suggests that experimental concurrency may carry a lower risk of STI transmission.
Table 1.
Characteristics of concurrency types elicited through qualitative research.(22)
| Type of concurrency | Main partner | Casual partners | Duration of overlap | Condom use | |
|---|---|---|---|---|---|
| w/ main | w/ casual | ||||
| Reactive | Yes | Yes | Typically short | No | Sometimes |
| Transitional | Yes | No | Often long | No | -- |
| Compensatory | Yes | Yes | Typically short | No | Sometimes |
| Experimental | No | Yes | Short | -- | Yes |
Given the qualitative nature of the study in which these concurrency types were identified, neither the frequency with which they occurred, nor associated behaviors could be determined.(22) Therefore, we conducted a subsequent study in STD clinics in three cities with different STI prevalence (Seattle-low prevalence, and St. Louis and New Orleans-high prevalence) to estimate the prevalence of each of four concurrency types (transitional, reactive, compensatory, experimental), identify individual characteristics associated with each type, and evaluate the degree to which they were differentially distributed in low- and high-STD prevalence locations. We hypothesized that community STI prevalence would be higher if transitional, reactive, and compensatory concurrency types were common, due to lower expected condom use with these types of concurrency. We also hypothesized that experimental concurrency, where condom use may be practiced more frequently, would be more common than other types of concurrency in populations with low STI prevalence.
Methods
Between November 2001 and May 2004, 1220 young adults attending public STD clinics in Seattle (n=605), New Orleans (n=367) and St. Louis (n=248) were interviewed and tested for STIs. This group was selected for study because of their high risk of STI. Eligibility criteria were age 18-26 years and a “new problem” consisting of symptoms of or suspected contact to someone with an STI. A study interviewer approached potential participants in clinic waiting rooms at each site. Eligible, interested individuals were given further details on the study and provided written informed consent in a private room. The study procedures were approved by institutional review boards at the University of Washington, Washington University in St. Louis, and Louisiana State University.
All study subjects completed an interview that was a combination of face-to-face and computer-assisted self-interview (CASI). Demographic and non-sensitive questions were posed by an interviewer, whereas questions about sexual practices were asked by CASI. The survey included questions from Wave III of the National Longitudinal Study of Adolescent Heath.(25) In addition, four questions were developed based on the qualitative findings of our previous study to estimate the prevalence and correlates of the concurrent partnership types defined above.(22) Participants were asked to indicate if they had ever done any of the following: ‘My partner had sex with someone else, so I had sex with someone else too.’(reactive); ‘Problems developed in the relationship, so I started up a new relationship as soon as possible to make sure I was always with someone.’ (transitional); ‘Something was missing in the relationship, so I found someone else to meet that need so I could continue with my current partner.’ (compensatory); and ‘I have had a number of sexual partners at the same time to figure out who is worth being with.’ (experimental).
We assessed sexual orientation, race/ethnicity, lifetime number of sex partners, having sex the same day as meeting a partner, and drug use as potential correlates of the concurrency types, based on previous associations with concurrency (10, 13, 26) and/or hypothesized risk for concurrency. Heterosexual orientation was defined as a response of ‘100% heterosexual (straight)’ to the question ‘Please choose the description that best fits how you think about yourself’, unless same-sex sexual partners were reported. African American race was defined as non-Hispanic and African American/black versus any other type of racial/ethnic identity. Lifetime number of sex partners was assessed by asking, ‘With how many partners have you ever had vaginal intercourse, even if only once?’, which was dichotomized into greater than three partners versus three or fewer. Having sex on the same day as meeting a partner was defined by the yes/no answer to, ‘Have you ever had sexual intercourse with someone the same day that you met him/her?’ Drug use was defined as a positive response to the any of the following questions, ‘Since June 1995, have you used (1) any kind of cocaine – including crack, freebase, or powder; (2) crystal meth; (3) any other types of illegal drugs, such as LSD, PCP, ecstasy, mushrooms, inhalants, ice, heroin, or prescription medicines not prescribed to you?’
All participants underwent a clinical exam for STI screening. The clinician inquired about sexual history and symptoms, and inspected the external genitalia. In Seattle, urine from men was tested for Chlamydia trachomatis and Neisseria gonorrhoeae using the APTIMA CT/NG TMA assay (Gen-Probe Inc., San Diego, CA). Among New Orleans and St. Louis men, a urethral swab was tested for C. trachomatis and N. gonorrhoeae using the Gen-Probe Pace2 and APTIMA CT/NG TMA assays, respectively. All women received a speculum exam during which the clinician collected three cervical swabs. C. trachomatis was detected by culture and N. gonorrhoeae by Gram stain and culture in Seattle, by the Pace2 assay in New Orleans, and by the APTIMA TMA assay in St. Louis. M. genitalium PCR and TMA assays(27) were performed on a cervical swab, a urine sample, and a self-obtained vaginal swab for all women and on a urine sample for all men. Trichomonas vaginalis was diagnosed by the presence of motile trichomonads on wet-mount microscopy. “Any STI” was defined as a positive test for any of the above.
In univariate analyses, categorical associations were assessed using either Fisher's Exact or Pearson's chi square test of association, while continuous variables were assessed using the Wilcoxon rank-sum test. First, the association of each concurrency type with demographic characteristics and with sexual risk behaviors was assessed. Then, multivariate logistic regression was conducted to identify factors independently associated with each concurrency type. Previous data suggest that types of concurrency may differ by gender(7, 10, 26). Therefore, we developed separate multivariate models for men and women. All analyses were performed with Stata version 11.2 (StataCorp, College Station, TX).
Results
Of the 1220 young adults who took part in the study, 1098 reported ever being sexually active and responded to the concurrency questions (90%) and, therefore, were included in these analyses. Fifty-six percent of these subjects were male, among whom 84% self-identified as ‘100% heterosexual’ with no same sex partners, 26% as white, 64% as African American, and 10% as Hispanic or of other ethnicity. Among women, 65% self-identified as ‘100% heterosexual’ with no same sex partners, 30% as white, 55% as African American, and 15% as Hispanic or of other ethnicity (Table 2). The majority of participants from New Orleans (99%) and St. Louis (81%) were African American. The median life-time number of partners was 10 [IQR: 4-21] for men and 7 [IQR: 4-15] for women.
Table 2.
Demographics and Sexual Behaviors among Young Adults at 3 STD Clinics
| Total No. (%) N = 1098 | Men No. (%) N = 619 | Women No. (%) N = 479 | |
|---|---|---|---|
| Age+ | 21 [20-23] | 21 [20-23] | 21 [20-23] |
| Race/ethnicity** | |||
| NH† White | 300 (27.6) | 160 (26.1) | 140 (29.5) |
| NH† African American | 656 (60.3) | 394 (64.3) | 262 (55.2) |
| NH† Other | 62 (5.7) | 26 (4.2) | 36 (7.6) |
| Hispanic | 70 (6.4) | 33 (5.4) | 37 (7.8) |
| Heterosexual~∫ | 835 (76.1) | 522 (84.3) | 313 (65.3) |
| Total number of sex partners+∫ | 8 [4-20] | 10 [4-21] | 7 [4-15] |
| >3 lifetime partners | 830 (77.1) | 473 (78.1) | 357 (76.0) |
| Drug use (since June 1995)∥ | 323 (30.0) | 196 (32.3) | 127 (26.9) |
| Sex same day as meeting - ever∫ | 603 (54.9) | 412 (66.6) | 191 (39.9) |
| Reactive concurrency* | 371 (33.9) | 224 (36.3) | 147 (30.7) |
| Transitional concurrency* | 398 (36.3) | 244 (39.4) | 154 (32.2) |
| Compensatory concurrency | 353 (32.2) | 213 (34.4) | 140 (29.2) |
| Experimental concurrency** | 290 (26.4) | 183 (29.6) | 107 (22.3) |
| No concurrency* | 439 (40.0) | 228 (36.8) | 211 (44.1) |
p<0.05
p<0.01
p<0.001
Heterosexual = anyone who considered themselves 100% heterosexual and did not report any same sex partners
NH = Non-Hispanic
median [IQR]
drugs include: cocaine, crystal meth, LSD, PCP, ecstasy, mushrooms, inhalants, ice, heroin
All four concurrency types were reported by fewer women than men; 31% of women and 36% of men reported reactive (p=0.05), 32% of women and 39% of men transitional (p=0.01), 29% of women and 34% of men compensatory (p=0.07), and 22% of women and 30% of men reported experimental concurrency (p=0.01). Forty-four percent of women and 37% of men reported no concurrency (p=0.02). Of women reporting any concurrency, 39% reported only one type, 29% two types, and 33% three or more. Among the men reporting concurrency, 32% reported one type; 31% two types; and 37% three or more.
Reported concurrency types differed by demographic and behavioral characteristics (Table 3). Men and women reporting each of the concurrency types reported more lifetime sex partners than those not reporting each type of concurrency. Overall, those reporting experimental concurrency reported the highest median lifetime number of sexual partners (men: 20, women: 15). Drug use was more prevalent among men reporting reactive and experimental concurrency compared to men who did not report those types of concurrency. In contrast, all four types of concurrency were associated with drug use among women. Men reporting reactive or experimental concurrency were less likely to be heterosexual compared to men who did not report those types of concurrency (Table 3). Women reporting transitional, compensatory, and experimental concurrency were less likely to be heterosexual compared to women who did not report those types of concurrency. Having sex the same day as meeting a partner was associated with all types of concurrency among both men and women (Table 3).
Table 3.
Demographics and Sexual Behaviors among Young Adults at 3 STD Clinics: By Type of Concurrency Reported
| Male | Reactive No. (%) N = 224 | Transitional No. (%) N = 244 | Compensatory No. (%) N = 213 | Experimental No. (%) N = 183 | No concurrency No. (%) N = 228 |
|---|---|---|---|---|---|
| Age+ | 22 [20-24]* | 22 [20-24] | 22 [20-24]** | 22 [20-24]** | 21 [20-22] |
| Race/ethnicity: | |||||
| NH† White | 47 (21.4) | 52 (21.7) | 32 (15.3)∫ | 42 (23.3) | 70 (31.0) |
| NH† African American | 154 (70.0) | 164 (68.3) | 156 (74.6)∫ | 116 (64.4) | 135 (59.7) |
| NH† Other | 8 (3.6) | 10 (4.2) | 7 (3.4)∫ | 6 (3.3) | 12 (5.3) |
| Hispanic | 11 (5.0) | 14 (5.8) | 14 (6.7)∫ | 16 (8.9) | 9 (4.0) |
| Heterosexual~ | 178 (79.5)* | 207 (84.8) | 175 (82.2) | 146 (79.8)* | 198 (86.8) |
| Total number of sex partners+ | 15 [6.5-30]∫ | 15 [6-28]∫ | 15 [5-30]∫ | 20 [9.5-30]∫ | 5 [3-11] |
| >3 lifetime partners | 184 (85.2)** | 209 (87.5)∫ | 173 (84.0)* | 157 (89.2)∫ | 149 (66.2) |
| Drug use (since June 1995)∥ | 85 (38.8)* | 86 (36.0) | 73 (34.8) | 71 (39.7)* | 55 (24.4) |
| Sex same day as meeting - ever | 183 (81.7)∫ | 187 (76.6)∫ | 170 (79.8)∫ | 159 (86.9)∫ | 108 (47.4) |
| Female | N = 147 | N = 154 | N = 140 | N = 107 | N = 211 |
| Age+ | 21 [19-23] | 21 [19-23] | 21 [19.5-23] | 22 [20-24]** | 21 [20-23] |
| Race/ethnicity: | |||||
| NH† White | 32 (21.9) | 49 (32.0) | 41 (29.7) | 49 (46.7)∫ | 55 (26.3) |
| NH† African American | 91 (62.3) | 84 (54.9) | 76 (55.1) | 42 (40.0)∫ | 120 (57.4) |
| NH† Other | 10 (6.9) | 8 (5.2) | 10 (7.3) | 6 (5.7)∫ | 17 (8.1) |
| Hispanic | 13 (8.9) | 12 (7.8) | 11 (8.0) | 8 (7.6)∫ | 17 (8.1) |
| Heterosexual~ | 89 (60.5) | 90 (58.4)* | 75 (53.6)** | 42 (39.3)∫ | 160 (75.8) |
| Total number of sex partners+ | 11 [6-22.5]∫ | 12 [7-20]∫ | 12 [6-20]∫ | 15 [10-25]∫ | 4 [2-7] |
| >3 lifetime partners | 136 (94.4)∫ | 141 (92.8)∫ | 122 (89.1)∫ | 96 (94.1)∫ | 123 (59.1) |
| Drug use (since June 1995)∥ | 53 (36.6)** | 57 (38.3)∫ | 50 (36.8)** | 57 (53.8)∫ | 33 (15.8) |
| Sex same day as meeting – ever | 83 (56.5)∫ | 91 (59.1)∫ | 82 (58.6)∫ | 77 (72.0)∫ | 43 (20.4) |
p<0.05
p<0.01
p<0.001, the comparison group for each type of concurrency was everyone who did not report that type of concurrency
Heterosexual = anyone who considered themselves 100% heterosexual and did not report any same sex partners
NH = Non-Hispanic
median [IQR]
drugs include: cocaine, crystal meth, LSD, PCP, ecstasy, mushrooms, inhalants, ice, heroin
Population-level analysis
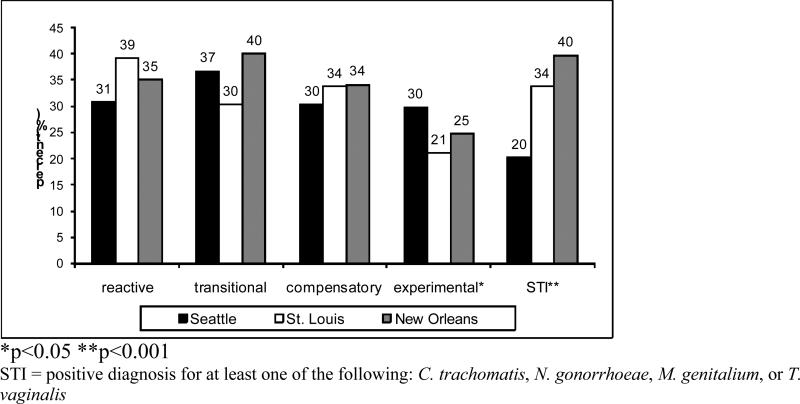
Overall, 28.8% tested positive for any of the STIs assessed; 30% of men and 27% of women. In New Orleans the STI prevalence was 39.7%; in St. Louis 33.8%, and in Seattle 20.2% (Figure 1). The association between prevalence of STI in each city and the prevalence of hypothesized high and low risk types of concurrency was not consistent. The prevalence of reactive concurrency in Seattle, St. Louis, and New Orleans was 31%, 39%, and 35%, respectively. The prevalence of transitional concurrency in Seattle, St. Louis, and New Orleans was 37%, 30%, and 40%, respectively. The prevalence of compensatory concurrency was about one-third in all three cities. Experimental concurrency was most common in Seattle (30%) compared to St. Louis (21%) and New Orleans (25%). Reactive concurrency was reported by significantly more individuals from St. Louis (odds ratio (OR) 1.45, 95% confidence interval (CI) 1.06-2.00) than by those from Seattle; while experimental concurrency was reported by more individuals from Seattle and fewer individuals from St. Louis (OR 0.63, 95% CI 0.44-0.91) and New Orleans (OR 0.77, 95% CI 0.57-1.06).
Figure 1.
Percent of Concurrency Type and Percent with an STI in Seattle, St. Louis, and New Orleans among Young Adults Attending STD Clinics *p<0.05 **p<0.001 STI = positive diagnosis for at least one of the following: C. trachomatis, N. gonorrhoeae, M. genitalium, or T. vaginalis
Multivariate Analyses
In multivariate analysis adjusted for age, site, and the other concurrency types, each concurrency type was associated with a set of demographic and behavioral characteristics, which differed by respondent gender (Table 4). The reference group for each model was all participants who did not report that type of concurrency. Reactive concurrency among men was more common among men not identifying as heterosexual (OR 0.4, 95% CI 0.3-0.8), using drugs (OR 1.7, 95% CI 1.1-2.8), and ever having sex with a partner the same day as meeting (OR 2.1, 95% CI 1.3-3.3). Reactive concurrency among women was associated with having more than three lifetime partners (OR 4.5, 95% CI 2.0-10.0) and being African American (OR 2.6, 95% CI 1.4-4.8). Transitional concurrency among men and women was associated with having more than three lifetime partners (men: OR 2.1, 95% CI 1.2-3.6; women: OR 3.8, 95% CI 1.7-8.2). Compensatory concurrency among men was associated with being African American (OR 3.6, 95% CI 1.9-6.8). In contrast, none of the evaluated characteristics were associated with compensatory concurrency among women. Experimental concurrency among men was associated with having more than three lifetime partners (OR 2.0, 95% CI 1.1-3.6) and ever having sex the same day as meeting a partner (OR 3.4, 95% CI 2.0-5.9). Experimental concurrency among women was associated with not identifying as heterosexual (OR 0.5, 95% CI 0.3-0.8), drug use (OR 2.4, 95% CI 1.2-4.5), and ever having sex the same day as meeting a partner (OR 3.1, 95% CI 1.7-5.8).
Table 4.
Multivariate Models of Characteristics & Behaviors Associated with Reporting Types of Concurrency among Young Adults from 3 STD Clinics Who Reported Sexual Activity in their Lifetime (AOR (95% CI))*
| Reactive | Transitional | Compensatory | Experimental | |||||
|---|---|---|---|---|---|---|---|---|
| Men (N = 585) | Women (N = 458) | Men (N = 585) | Women (N = 458) | Men (N = 585) | Women (N = 458) | Men (N = 585) | Women (N = 458) | |
| African American | 1.27 (0.69-2.32) | 2.60 (1.41-4.79) | 0.83 (0.44-1.56) | 1.57 (0.81-3.03) | 3.58 (1.89-6.80) | 0.83 (0.43-1.60) | 0.92 (0.50-1.70) | 0.60 (0.29-1.23) |
| Heterosexual | 0.43 (0.25-0.76) | 1.20 (0.72-2.01) | 1.54 (0.84-2.84) | 1.25 (0.71-2.19) | 0.74 (0.41-1.36) | 0.68 (0.40-1.17) | 0.61 (0.34-1.09) | 0.45 (0.25-0.80) |
| > 3 Lifetime sex partners | 1.25 (0.73-2.14) | 4.45 (1.98-10.0) | 2.07 (1.20-3.59) | 3.75 (1.71-8.22) | 0.85 (0.49-1.48) | 0.85 (0.41-1.77) | 1.95 (1.06-3.55) | 2.13 (0.80-5.72) |
| Drug use** (since June 1995) | 1.71 (1.06-2.76) | 1.77 (0.96-3.26) | 1.06 (0.65-1.73) | 1.28 (0.67-2.44) | 1.22 (0.74-2.02) | 0.98 (0.51-1.86) | 1.03 (0.64-1.66) | 2.37 (1.24-4.52) |
| Ever have sex the same day as meeting a partner | 2.06 (1.29-3.29) | 1.58 (0.93-2.67) | 0.94 (0.59-1.50) | 1.72 (0.99-2.99) | 1.50 (0.92-2.45) | 1.36 (0.77-2.40) | 3.44 (2.03-5.85) | 3.12 (1.70-5.76) |
All models are controlled for age, site, and the three other concurrency types; the reference group for each model is all people who did not report that type of concurrency
drugs include: cocaine, crystal meth, LSD, PCP, ecstasy, mushrooms, inhalants, ice, and heroin
Discussion
These findings provide a quantitative assessment of the distribution of and characteristics associated with concurrency types that were first identified qualitatively.(22) The proportion of these STD clinic attendees reporting any given concurrency type was high, ranging from 22-39%. Overall, more men reported concurrency than women and the most commonly reported type for both men and women was transitional. Previous reports have shown higher rates of concurrency reported by African Americans compared to other racial/ethnic groups.(7, 8, 16, 28) However, this association was only seen in this study for reactive concurrency among women and compensatory concurrency among men in multivariate models.
Characteristics associated with each concurrency type were different for men and women. Notably, among women no characteristics were associated with compensatory concurrency. In contrast, experimental concurrency, the concurrency type least affected by the dynamics of a relationship, was associated with risk-taking behaviors such as drug use and having sex the same day as meeting a partner. The other concurrency types represent situations that arise within ongoing partnerships, which may explain the limited number of risk factors found, given that the characteristics assessed were not tied to a specific relationship.
For men, transitional concurrency was only associated with a higher number of lifetime sex partners. This is the most relational concurrency type, occurring when the index is involved in two ongoing partnerships, ending an existing main partnership at the same time as forming a new main partnership. The absence of other risk factors associated with transitional concurrency in men suggests such a behavior is not one practiced in the context of other risky behaviors, such as drug use. Conversely, many risk factors were associated with reactive concurrency, suggesting that this is a behavior practiced among men who also practice other risky behaviors such as having sex the same day as meeting a partner and drug use.
Reactive concurrency among men and experimental concurrency among women were reported by more of those who also reported not being 100% heterosexual. Experimental concurrency seems to fit with those who do not define themselves as having one sexual orientation and may be “experimenting” with same-gender sexual activity, or merely enjoy having partners of different genders, which may end up occurring at the same time in more casual partnerships. Because norms of monogamy tend to differ between partnerships between men and heterosexual partnerships,(29, 30) the association of reactive concurrency with not being heterosexual is not surprising as men with male partners may face less relationship repercussions from reacting to their partner having other partners by acquiring a concurrent partner themselves.
These data were not able to test whether each type of concurrency was associated with transmitting STI because the data did not include this level of detail. However, concurrency may have more relevancy for the connectivity it provides to the underlying sexual network, potentially increasing population prevalence, rather than for individual- or partnership-level risk. While city was not consistently associated with specific concurrency types in multivariate analyses, an ecologic analysis of concurrency types in low- and high-STI prevalence cities provided some support for our hypothesis that population-level STI prevalence co-varied with concurrency types (Figure 1). We hypothesized that experimental concurrency would be most common in low-STI prevalence areas and this type was most common in Seattle, the city with the lowest STI prevalence. Furthermore, transitional concurrency was most common in New Orleans, the highest prevalence city (although not significantly). If transitional concurrencies are of longer duration because they involve two relatively established partnerships, this would provide a more stable network for disease transmission. Finally, reactive concurrency was most common in St. Louis, another high prevalence city, and it was also associated with risk behaviors such as drug use, which may increase overall disease transmission.
The proportion of individuals reporting concurrency was higher in our study of STD clinic patients than in national surveys; 60% reported at least one concurrency type (56% of women and 63% of men) compared to NSFG data where 23% of women 18-24 years old reported concurrency during the past 5 years.(7) While much of this is likely due to differences in study populations (STD clinics versus general population), one additional caveat is that our measure was cumulative, measuring concurrency over the life span as compared to the shorter time frames used in the NSFG. However, because we studied young adults this ‘ever’ period does not cover as long a time span as it would for older adults, so five years and ‘ever’ may be fairly similar time spans for young adults. Ideally, the comparison population would be a national study of young adults that included a lifetime measure of concurrency, but this was not available, so the 5-year estimate was the best approximation.
This study was not able to assess associations between condom use and types of concurrency because each was measured over a different timeframe; the concurrency measures were over the lifetime, but our condom measures were either partner specific or referred to the past year. In the future it would be beneficial to collect data on specific partnerships where these types of concurrency occur, which would allow for the collection of relevant condom use data as well as other partnership-specific information. These STD clinic attendees were generally homogenous in terms of their risk behaviors, making it more difficult to detect associations with high-risk behavior; thus we may have missed some correlates of concurrency types. Nevertheless, the associations we did identify are likely to be confirmed in the general population(31). In addition, we did not assess other concurrency types outside of relationships such as people who have multiple casual sex partners, but are not looking for a relationship, or people who have agreed upon an open relationship. Finally, it would be important in the future to test the reliability and validity of the concurrency measures to confirm we are using the most appropriate tool for gathering this information.
These data affirm that concurrency is a nuanced behavior and relatively common among STD clinic populations, especially in young adults. Different concurrency types were characterized by different risk factors, suggesting all concurrent partnerships are not equal. Some types of concurrency may represent a higher risk of STI transmission than others. In order to have a better understanding of this more detailed study would be required, which would include concurrency, condom use, and other STI-risk behaviors at the partnership level. However, this study provides an initial understanding of the prevalence and correlates of these types of concurrency. Finally, while the earlier qualitative study concluded that “for some it takes a village” to meet their sexual needs, the present study helps us understand more about who lives in these villages and what else goes on inside them.
Acknowledgements
This work was supported by the UW STD CRC (NIH/NIAID AI31448).
Footnotes
Conflicts of Interest
None declared.
References
- 1.Morris M, Kretzschmar M. Concurrent partnerships and the spread of HIV. AIDS. Apr. 1997;11(5):641–8. doi: 10.1097/00002030-199705000-00012. [DOI] [PubMed] [Google Scholar]
- 2.Potterat JJ, Zimmerman-Rogers H, Muth SQ, Rothenberg RB, Green DL, Taylor JE, et al. Chlamydia transmission: concurrency, reproduction number, and the epidemic trajectory. Am J Epidemiol. Dec 15. 1999;150(12):1331–9. doi: 10.1093/oxfordjournals.aje.a009965. [DOI] [PubMed] [Google Scholar]
- 3.Ghani A, Swinton J, Garnett G. The role of sexual partnership networks in the epidemiology of gonorrhea. Sex Transm Dis. 1997;24(1):45–56. doi: 10.1097/00007435-199701000-00009. [DOI] [PubMed] [Google Scholar]
- 4.Koumans EH, Farley TA, Gibson JJ, Langley C, Ross MW, McFarlane M, et al. Characteristics of persons with syphilis in areas of persisting syphilis in the United States: sustained transmission associated with concurrent partnerships. Sex Transm Dis. Sep. 2001;28(9):497–503. doi: 10.1097/00007435-200109000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Hudson C. AIDS in rural Africa: a paradigm for HIV-1 prevention. Int J STD AIDS. Jul. 1996;7(4):236–43. doi: 10.1258/0956462961917906. [DOI] [PubMed] [Google Scholar]
- 6.Kretzschmar M, Morris M. Measures of concurrency in networks and the spread of infectious disease. Mathematical biosciences. Apr 15. 1996;133(2):165–95. doi: 10.1016/0025-5564(95)00093-3. [DOI] [PubMed] [Google Scholar]
- 7.Adimora AA, Schoenbach VJ, Bonas DM, Martinson FE, Donaldson KH, Stancil TR. Concurrent sexual partnerships among women in the United States. Epidemiology. May. 2002;13(3):320–7. doi: 10.1097/00001648-200205000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Kraut-Becher JR, Aral SO. Gap length: an important factor in sexually transmitted disease transmission. Sex Transm Dis. Mar. 2003;30(3):221–5. doi: 10.1097/00007435-200303000-00009. [DOI] [PubMed] [Google Scholar]
- 9.Manhart LE, Aral SO, Holmes KK, Foxman B. Sex partner concurrency: measurement, prevalence, and correlates among urban 18-39-year-olds. Sex Transm Dis. Mar. 2002;29(3):133–43. doi: 10.1097/00007435-200203000-00003. [DOI] [PubMed] [Google Scholar]
- 10.Adimora AA, Schoenbach VJ, Doherty IA. Concurrent sexual partnerships among men in the United States. Am J Public Health. 2007 Oct 30; doi: 10.2105/AJPH.2006.099069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ford K, Sohn W, Lepkowski J. American adolescents: sexual mixing patterns, bridge partners, and concurrency. Sexually transmitted diseases. 2002 Jan;29(1):13–9. doi: 10.1097/00007435-200201000-00003. [Research Support, Non-U.S. Gov't Research Support, U.S. Gov't, P.H.S.]. [DOI] [PubMed] [Google Scholar]
- 12.Rosenberg MD, Gurvey JE, Adler N, Dunlop MB, Ellen JM. Concurrent sex partners and risk for sexually transmitted diseases among adolescents. Sex Transm Dis. Apr. 1999;26(4):208–12. doi: 10.1097/00007435-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Nelson SJ, Manhart LE, Gorbach PM, Martin DH, Stoner BP, Aral SO, et al. Measuring sex partner concurrency: It's what's missing that counts. Sex Transm Dis. Oct. 2007;34(10):801–7. doi: 10.1097/OLQ.0b013e318063c734. [DOI] [PubMed] [Google Scholar]
- 14.UNAIDS Reference Group on Estimates M, and Projections: Working Group on Measuring Concurrent Sexual Partnerships HIV: consensus indicators are needed for concurrency. Lancet. Feb 20. 2010;375(9715):621–2. doi: 10.1016/S0140-6736(09)62040-7. [DOI] [PubMed] [Google Scholar]
- 15.Drumright LN, Gorbach PM, Holmes KK. Do people really know their sex partners? Concurrency, knowledge of partner behavior, and sexually transmitted infections within partnerships. Sex Transm Dis. Jul. 2004;31(7):437–42. doi: 10.1097/01.olq.0000129949.30114.37. [DOI] [PubMed] [Google Scholar]
- 16.Morris M, Kurth AE, Hamilton DT, Moody J, Wakefield S. Concurrent partnerships and HIV prevalence disparities by race: linking science and public health practice. Am J Public Health. Jun. 2009;99(6):1023–31. doi: 10.2105/AJPH.2008.147835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Sawers L, Stillwaggon E. Concurrent sexual partnerships do not explain the HIV epidemics in Africa: a systematic review of the evidence. Journal of the International AIDS Society. [Review] 2010;13:34. doi: 10.1186/1758-2652-13-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Goodreau SM. A decade of modelling research yields considerable evidence for the importance of concurrency: a response to Sawers and Stillwaggon. Journal of the International AIDS Society. [Comment] 2011;14:12. doi: 10.1186/1758-2652-14-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Epstein H, Morris M. Concurrent partnerships and HIV: an inconvenient truth. Journal of the International AIDS Society. 2011;14:13. doi: 10.1186/1758-2652-14-13. [Research Support, N.I.H., Extramural Review]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Santhakumaran S, O'Brien K, Bakker R, Ealden T, Shafer LA, Daniel RM, et al. Polygyny and symmetric concurrency: comparing long-duration sexually transmitted infection prevalence using simulated sexual networks. Sexually transmitted infections. Dec. 2010;86(7):553–8. doi: 10.1136/sti.2009.041780. [Comparative Study Research Support, Non-U.S. Gov't] [DOI] [PubMed] [Google Scholar]
- 21.Reniers G, Watkins S. Polygyny and the spread of HIV in sub-Saharan Africa: a case of benign concurrency. Aids. Jan 16. 2010;24(2):299–307. doi: 10.1097/QAD.0b013e328333af03. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gorbach PM, Stoner BP, Aral SO, Whittington WLH, Holmes KK. “It takes a village”: understanding concurrent sexual partnerships in Seattle, Washington. Sex Transm Dis. Aug. 2002;29(8):453–62. doi: 10.1097/00007435-200208000-00004. [DOI] [PubMed] [Google Scholar]
- 23.Morris M, Epstein H, Wawer M. Timing is everything: international variations in historical sexual partnership concurrency and HIV prevalence. PloS one. 2010;5(11):e14092. doi: 10.1371/journal.pone.0014092. [Research Support, N.I.H., Extramural Research Support, Non-U.S. Gov't] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Doherty IA, Schoenbach VJ, Adimora AA. Condom use and duration of concurrent partnerships among men in the United States. Sexually transmitted diseases. May. 2009;36(5):265–72. doi: 10.1097/OLQ.0b013e318191ba2a. [Research Support, N.I.H., Extramural] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Udry J, The National Longitudinal Study of Adolescent Health (Add Health) Waves I & II, 1994-1996; Wave III, 2001-2002 [machine-readable data file and documentation] Carolina Population Center, University of North Carolina at Chapel Hill; Chapel Hill, NC: 2003. [Google Scholar]
- 26.Doherty IA, Minnis A, Auerswald CL, Adimora AA, Padian NS. Concurrent partnerships among adolescents in a Latino community: the Mission District of San Francisco, California. Sex Transm Dis. Jul. 2007;34(7):437–43. doi: 10.1097/01.olq.0000251198.31056.7d. [DOI] [PubMed] [Google Scholar]
- 27.Wroblewski JK, Manhart LE, Dickey KA, Hudspeth MK, Totten PA. Comparison of transcription-mediated amplification and PCR assay results for various genital specimen types for detection of Mycoplasma genitalium. J Clin Microbiol. Sep. 2006;44(9):3306–12. doi: 10.1128/JCM.00553-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Adimora AA, Schoenbach VJ, Martinson F, Donaldson KH, Stancil TR, Fullilove RE. Concurrent sexual partnerships among African Americans in the rural south. Ann Epidemiol. Mar. 2004;14(3):155–60. doi: 10.1016/S1047-2797(03)00129-7. [DOI] [PubMed] [Google Scholar]
- 29.Crawford I, Hammack PL, McKirnan DJ, Ostrow D, Zamboni BD, Robinson B, et al. Sexual sensation seeking, reduced concern about HIV and sexual risk behaviour among gay men in primary relationships. AIDS Care. Aug. 2003;15(4):513–24. doi: 10.1080/0954012031000134755. [DOI] [PubMed] [Google Scholar]
- 30.Galea J, Whittington W, Celum C. An ethnographic study of sexual practices and partnering characteristics of MSM with N. Gonorrhea in Seattle.. Paper presented at 13th Meeting of the International Society for Sexually Transmitted Disease Research; Denver. p. CO1999. [Google Scholar]
- 31.Manhart LE, Aral SO, Holmes KK, Critchlow CW, Hughes JP, Whittington WL, et al. Influence of study population on the identification of risk factors for sexually transmitted diseases using a case-control design: the example of gonorrhea. Am J Epidemiol. Aug 15. 2004;160(4):393–402. doi: 10.1093/aje/kwh220. [DOI] [PubMed] [Google Scholar]