Abstract
Gastric cancer is one of the most frequent cancers in the world; almost two-thirds of gastric cancer cases and deaths occur in less developed regions. In China, based on two national mortality surveys conducted in 1970s and 1990s, there is an obvious clustering of geographical distribution of gastric cancer in the country, with the high mortality being mostly located in rural areas, especially in Gansu, Henan, Hebei, Shanxi and Shaanxi Provinces in the middle-western part of China. Despite a slight increase from the 1970s to early 1990s, remarkable declines in gastric cancer mortality were noticed in almost the entire population during the last decade in China. These declines were largely due to the dramatic improvements in the social-economic environment, lifestyle, nutrition, education and health care system after economic reforms started two decades ago. Nevertheless, gastric cancer will remain a significant cancer burden currently and be one of the key issues in cancer prevention and control strategy in China. It was predicted that, in 2005, 0.3 million deaths and 0.4 million new cases from gastric cancer would rank the third most common cancer. The essential package of the prevention and control strategy for gastric cancer in China would focus on controlling Helicobacter pylori (H pylori) infection, improving educational levels, advocating healthy diet and anti-tobacco campaign, searching for cost-effective early detection, diagnosis and treatment programs including approaches for curable management and palliative care.
Keywords: Gastric cancer, Incidence, Mortality
GASTRIC CANCER IN THE WORLD
Gastric cancer is one of the most frequent cancers in the world, in both men and women. In the year 2002, the age standardized incidence rate was 22.0 per 100 000 in men, and 10.4 per 100 000 in women, and mortality rate was 16.3 per 100 000 in men, and 7.9 per 100 000 in women, according to the latest global estimation-GLOBOCAN 2002[1]. Despite a marked decrease, especially in mortality rate in many countries, the absolute number of gastric cancer cases and deaths is still a big burden of the local health program, since the world population and life expectancy are increasing. In 2002, it was estimated that there were 0.9 million new gastric cancer cases (0.60 million in men and 0.33 million in women) and 0.7 million deaths (0.45 million in men and 0.25 in women) from gastric cancer in the world. In men, gastric cancer ranks the third among the commonest cancers in incidence rate (after cancers of lung and prostate) and the second in mortality rate (after lung cancer), while in women, it is the fifth most common cancer in incidence and the fourth in mortality (after cancers of breast, cervix, lung and/or colon-rectum)[1].
In terms of geographic distribution, almost two-thirds of gastric cancer cases and deaths occur in less developed regions. High rates apply to Japan, China, Korea, Central and South America, Eastern Europe, and parts of the Middle East, and low rates to North America, Australia and New Zealand, Northern Europe, and India[1,2]. Five-year relative survivals of around 20% or less are frequently reported. The incidence ratios of men to women generally range between 1.5 and 2.5, with higher ratios for intestinal than diffuse cancers and in high-risk populations[2].
NATIONAL GASTRIC CANCER MORTALITY PATTERN IN THE 1970s AND 1990s
In China, two national mortality surveys were conducted in 1973-1975 and 1990-1992, respectively, both organized by the National Office for Cancer Prevention of Control, the Ministry of Public Health, China. These two surveys showed the detail pattern and distribution of mortality rates for cancers in China at that time[3-7]. The first mortality survey was a nation-wide study. An atlas was published based on the survey results[4], providing a visual geographic distribution of gastric cancer profile in early 1970s. A map of the gastric cancer mortality distribution for males is shown in(Figure 1)as an example. An obvious clustering of geographical distribution of gastric cancer appears in China, with the high mortality being mostly located in the north (Liaodong Peninsula, Shandong Peninsula, Yangtze River Delta and middle-western provinces along Taihang Mountain and ‘Hexi Zoulang”).
Figure 1.
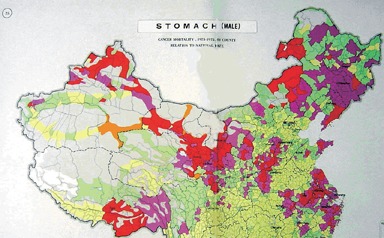
Mortality rates of gastric cancer in men in China, 1973-1975[4].
The second mortality survey covered 10% of the whole population that proved as a representative sample to reflect national cancer profile[5-7]. The crude mortality rate of gastric cancer in China was 25.2 per 100 000 (32.8 per 100 000 in men and 17.0 per 100 000 in women), which accounted for 23.2% of the total cancer deaths in 1990-1992, making gastric cancer the first leading cause of cancer death[8]. The geographic variety in the distribution was similar to that in the first survey in the 1970s. Table 1 shows the first 20 areas with high mortality rates for the gastric cancer (rates adjusted by the 1982 national census population). Most of these high-risk areas are located in rural areas, especially in Gansu, Henan, Hebei, Shanxi and Shaanxi Provinces in the middle-western part of China.
Table 1.
The first 20 areas with high mortality rate for gastric cancer in China - according to the second national mortality survey in 1990-1992 (rate per 100 000)
| Area | Rate | Area | Rate |
| Wuwei town, Gansu | 117.78 | Jiyuan town, Henan | 66.59 |
| Yangcheng county, Shanxi | 104.01 | Zhangye town, Gansu | 64.43 |
| Pingshun county, Shanxi | 96.95 | Jiaxian county, Shaanxi | 64.36 |
| Changle county, Fujian | 93.38 | Tianchang county, Anhui | 63.04 |
| Shexian county, Hebei | 85.64 | Tianzhu Tibet Autho county, Gansu | 59.18 |
| Lujiang county, Anhui | 84.46 | Putian county, Fujian | 58.83 |
| Zanghuang county, Hebei | 77.67 | Linxian county, Henan | 58.56 |
| Neixiang county, Henan | 77.45 | Wudu county, Gansu | 58.54 |
| Yuanqu county, Shanxi | 74.22 | Tianjian Dist.,Fuzhou city, Fujian | 57.52 |
| Linze county, Gansu | 66.69 | Xianju county, Zhejiang | 53.99 |
By comparing the above two national mortality surveys, an increasing trend for the age-standardized mortality rates of gastric cancer was shown in the entire population in China during the two decades. Nevertheless, the increase only appeared in rural areas, while a decreasing trend was noticed in urban population[9,10] (Table 2). In terms of age-specific mortality rates, a decreasing trend was noticed among almost all age groups (except age group 70-79 years) in urban residents, while an increasing trend was seen among most of age groups (except age group 30-44 years) in rural areas[10]. Nevertheless, with almost two-thirds of the population reside in rural areas, gastric cancer was still the first most common cancer in the entire population in China during 1970s and early 1990s, although it dropped to the third in urban areas.
Table 2.
Changes in the age-standardized mortality rates of gastric cancer between 1973 and 1975 and between 1990 and1992 in China (rate per 100 000)
| Area |
Year 1973-1975 |
Year 1990-1992 |
Changes (%) |
||||||
| Men | Women | Total | Men | Women | Total | Men | Women | Total | |
| Whole country | 27.1 | 13.0 | 19.8 | 30.1 | 13.8 | 21.8 | 11.0 | 6.3 | 10.0 |
| Urban | 27.3 | 13.3 | 20.1 | 21.2 | 9.8 | 15.3 | -22.2 | -26.7 | -23.8 |
| Rural | 26.7 | 12.6 | 19.4 | 33.7 | 15.4 | 24.4 | 26.4 | 22.1 | 25.8 |
In addition to the above two national mortality surveys, there were a few publications on gastric cancer mortality trends at local levels, either in big cities such as Beijing, Shanghai, or in high-risk areas such as in Henan and Hebei Provinces[11-14]. Similarly, the mortality rates of gastric cancer remain high although there was a slight decreasing trend during different time periods among those areas. Therefore, gastric cancer is still the major common cancer and a big burden for local health resources and facilities.
GASTRIC CANCER INCIDENCE AND MORTALITY PATTERNS AT THE NATIONAL LEVEL IN RECENT YEARS
Based on a routine mortality reporting system, covering 10% of the Chinese population, from the Ministry of Public Health which was submitted to the World Health Organization[15], the gastric cancer mortality trends in China were analyzed from 1987 to 1999, using the joinpoint model. The trends were further combined with the ratio of incidence to mortality from data in seven cancer registries in China that were published in the 8th edition of Cancer Incidence in Five Continents[16], to estimate and project the mortality and incidence for gastric cancer in 2000 and 2005 (by site, age, sex and area) at the national level, using the log-linear regression model with Poisson distribution assumption. These results have been serially published recently[17-19].
According to the data from the Center of Health Information Statistics (CHIS) under the Ministry of Public Health, gastric cancer mortality rates were higher in rural than urban areas, and in men than in women. During 1987-1999, slight but significant declines in mortality were noticed in almost the entire subpopulation (except in urban men before 1991) and for most age groups (except age group 15-34) in rural areas (Figures 2 and 3). In 2000, 0.3 million deaths and 0.4 million new cases were estimated for gastric cancer, similar to what was projected in 2005, while the latter had a slight decrease in men but increase in women (Table 3). In 2005, in terms of incidence rates, gastric cancer would rank the third among the most common cancers in China (after cancers of lung and liver in men and after cancers of breast and lung in women)[19].
Figure 2.
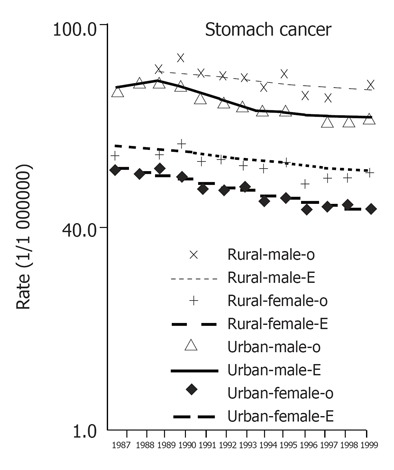
Time trends for age-standardized mortality rates (both observed and expected by model) of gastric cancer during 1987-1999 in China, by areas (rural and urban) and sex (per 100 000)
Figure 3.
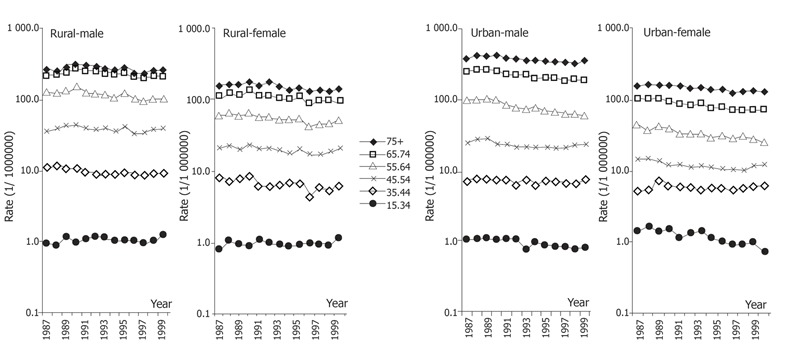
Time trends for age-specific mortality rates of gastric cancer during 1987-1999 in China, by areas (rural and urban) and sex, in CHIS data (rates per 100 000).
Table 3.
Gastric cancer incidence and mortality in China in 2000 and 2005
|
Men |
Women |
||||
| Year2000 | Year2005 | Year2000 | Year2005 | ||
| Mortality (per 100 000) | |||||
| rates | Age 45-54 | 45.5 | 43.3 | 20.5 | 19.0 |
| Age 55-64 | 109.4 | 89.4 | 46.6 | 40.1 | |
| Age 65-74 | 229.4 | 198.3 | 104.6 | 91.3 | |
| Age 75+ | 289.6 | 261.9 | 133.3 | 116.3 | |
| ASR1 | 32.7 | 288 | 15.0 | 13.3 | |
| Number of deaths | 200518 | 197222 | 95942 | 97843 | |
| Incidence (per 100 000) | |||||
| rates | Age 45-54 | 70 | 66.7 | 31.6 | 29.3 |
| Age 55-64 | 145.7 | 11.9 | 62.1 | 53.4 | |
| Age 65-74 | 264.3 | 228.5 | 120.5 | 105.2 | |
| Age 75+ | 288.8 | 261.2 | 133 | 116 | |
| ASR1 | 41.9 | 37.1 | 19.5 | 17.4 | |
| Number of cases | 256256 | 253110 | 121485 | 123883 | |
ASR: Age-standardized rate (adjusted by the world standard population).
FACTORS INFLUENCING THE GASTRIC CANCER PATTERN IN CHINA
Despite a slight increase from 1970s to early 1990s, remarkable declines in gastric cancer mortality were shown during the last decade in China. These declines were largely due to the dramatic improvements in the social-economic environment, lifestyle, nutrition, education and health care system after economic reforms started two decades ago. These include better socio-economic circumstances, higher educational levels, better refrigeration, reduced consumption of salted, smoked, and chemically preserved foods, eating more fruit and vegetables and remarkably improved sanitary conditions of the house and living standards, supplement intake nutrients such as vitamin C, vitamin E, beta-carotene, selenium and decreased intake of nitrosamine, which was strongly suspected as a major risk factor for gastric cancer[20-31]. H pylori infection, which is defined by the World Health Organization as a definite gastric carcinogen, is linked to crowded living conditions, family size, sharing a bedroom, low socio-economic status, low educational level and poor sanitation, and infrequent hand washing before meals. The prevalence of H pylori infection has reduced dramatically due to the improved socio-economic status and lifestyle changes during last decades, especially among urban areas. In addition, widespread prescription of antibiotics may be responsible for reducing H pylori infection. Finally, some locally popular customs, such as drinking green tea, consuming tofu, and ginger have been suggested to have a possible protective effect on gastric cancer[32-35].
However, huge demographic changes in China make the total number of incident cases and deaths from gastric cancer slightly declined in men between 2000 and 2005, while the number increased in women, despite the significant declining trends in rates among all age groups (Table 2)[17-19].
CONCLUSION
It is estimated that gastric cancer currently ranks the third among most common cancers, and will remain a significant cancer burden in China during the next decade. It will be, undoubtedly, one of the keys in cancer prevention and control strategy in China. The essential package would focus on controlling H pylori infection, improving educational levels, advocating healthy diet and anti-tobacco campaign, searching for cost-effective early detection, diagnosis and treatment programs including approaches for curable management and palliative care[36].
Footnotes
S- Editor Guo SY L- Editor Elsevier HK E- Editor Wang J
References
- 1.Ferlay J, Bray F, Pisani P, Parkin DM. GLOBOCAN 2002: Cancer incidence, mortality and prevalence worldwide. Lyon: IARC Press, Cited 2005-04-15; Available from: http: //www-dep.iarc.fr/
- 2.Roder DM. The epidemiology of gastric cancer. Gastric Cancer. 2002;5 Suppl 1:5–11. doi: 10.1007/s10120-002-0203-6. [DOI] [PubMed] [Google Scholar]
- 3.National Office for Cancer Prevention and Control of the Chinese Ministry of Health (NOCPC) Investigate for malignant tumor mortality in China. Beijing: People’s Health Publishing House; 1979. pp. 175–201. [Google Scholar]
- 4.Editorial Committee for the Atlas of Cancer Mortality. Atlas of cancer mortality in the People's Republic of China. Beijing: China Map Press; 1979. pp. 23–30. [Google Scholar]
- 5.Li L, Lu F, Zhang S. [Analysis of cancer modality and distribution in China from year 1990 through 1992--an epidemiologic study] Zhonghua Zhongliu Zazhi. 1996;18:403–407. [PubMed] [Google Scholar]
- 6.Li L, Zhang S, Lu F. [Research on characteristics of mortality spectrum and type composition of malignant tumors in China] Zhonghua Zhongliu Zazhi. 1997;19:323–328. [PubMed] [Google Scholar]
- 7.Zhou YS, Zhang SW, Li LD. Analysis for death for all and malignant tumors for Chinese population. Bull Chin Cancer. 1997;6:9–11. [Google Scholar]
- 8.Sun X, Mu R, Zhou Y, Dai X, Qiao Y, Zhang S, Huangfu X, Sun J, Li L, Lu F. [1990-1992 mortality of stomach cancer in China] Zhonghua Zhongliu Zazhi. 2002;24:4–8. [PubMed] [Google Scholar]
- 9.Li L, Lu F, Zhang S. [Analyses of variation trend and short-term detection of Chinese malignant tumor mortality during twenty years] Zhonghua Zhongliu Zazhi. 1997;19:3–9. [PubMed] [Google Scholar]
- 10.Sun XD, Mu R, Zhou YS, Dai XD, Zhang SW, Huangfu XM, Sun J, Li LD, Lu FZ, Qiao YL. [Analysis of mortality rate of stomach cancer and its trend in twenty years in China] Zhonghua Zhongliu Zazhi. 2004;26:4–9. [PubMed] [Google Scholar]
- 11.Wang QJ, Zhu WX, Yuan GL. [Trend and prediction of cancer mortality in Beijing, China, during 1980-2001] Zhonghua Liuxingbingxue Zazhi. 1995;16:195–198. [PubMed] [Google Scholar]
- 12.Gao YT, Tu JT, Jin F, Gao RN. Cancer mortality in Shanghai during the period 1963-77. Br J Cancer. 1981;43:183–195. doi: 10.1038/bjc.1981.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lu JB, Sun XB, Dai DX, Zhu SK, Chang QL, Liu SZ, Duan WJ. Epidemiology of gastroenterologic cancer in Henan Province, China. World J Gastroenterol. 2003;9:2400–2403. doi: 10.3748/wjg.v9.i11.2400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Li M, Li ZS, Chen ZF, He YT, Zhao BS, Li ZY, Li YW, Hou J. Mortality report of malignant tumors in SheXian, Hebei Province, China, from the 1970's to the present. Asian Pac J Cancer Prev. 2004;5:414–418. [PubMed] [Google Scholar]
- 15.World Health Organization (WHO) WHO Mortality Database as is WHO Statistical Information System (WHOSIS), cited 2005-04-15; Available from: http: //www-depdb.iarc.fr/ and http: //www.who.int/whosis/
- 16.Parkin DM, Whelan SL, Ferlay J, Teppo L, Thomas DB. Cancer incidence in five continents Vol VIII. Lyon: IARC Press; 2002. pp. 212–232. [Google Scholar]
- 17.Yang L, Parkin DM, Li L, Chen Y. Time trends in cancer mortality in China: 1987-1999. Int J Cancer. 2003;106:771–783. doi: 10.1002/ijc.11300. [DOI] [PubMed] [Google Scholar]
- 18.Yang L, Parkin DM, Li LD, Chen YD, Bray F. Estimation and projection of the national profile of cancer mortality in China: 1991-2005. Br J Cancer. 2004;90:2157–2166. doi: 10.1038/sj.bjc.6601813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Yang L, Parkin DM, Ferlay J, Li L, Chen Y. Estimates of cancer incidence in China for 2000 and projections for 2005. Cancer Epidemiol Biomarkers Prev. 2005;14:243–250. [PubMed] [Google Scholar]
- 20.Kneller RW, Guo WD, Hsing AW, Chen JS, Blot WJ, Li JY, Forman D, Fraumeni JF. Risk factors for stomach cancer in sixty-five Chinese counties. Cancer Epidemiol Biomarkers Prev. 1992;1:113–118. [PubMed] [Google Scholar]
- 21.Ma JL, You WC, Gail MH, Zhang L, Blot WJ, Chang YS, Jiang J, Liu WD, Hu YR, Brown LM, et al. Helicobacter pylori infection and mode of transmission in a population at high risk of stomach cancer. Int J Epidemiol. 1998;27:570–573. doi: 10.1093/ije/27.4.570. [DOI] [PubMed] [Google Scholar]
- 22.You WC, Zhang L, Gail MH, Ma JL, Chang YS, Blot WJ, Li JY, Zhao CL, Liu WD, Li HQ, et al. Helicobacter pylori infection, garlic intake and precancerous lesions in a Chinese population at low risk of gastric cancer. Int J Epidemiol. 1998;27:941–944. doi: 10.1093/ije/27.6.941. [DOI] [PubMed] [Google Scholar]
- 23.Yuan JM, Yu MC, Xu WW, Cockburn M, Gao YT, Ross RK. Helicobacter pylori infection and risk of gastric cancer in Shanghai, China: updated results based upon a locally developed and validated assay and further follow-up of the cohort. Cancer Epidemiol Biomarkers Prev. 1999;8:621–624. [PubMed] [Google Scholar]
- 24.Muñoz N. Is Helicobacter pylori a cause of gastric cancer An appraisal of the seroepidemiological evidence. Cancer Epidemiol Biomarkers Prev. 1994;3:445–451. [PubMed] [Google Scholar]
- 25.Limburg P, Qiao Y, Mark S, Wang G, Perez-Perez G, Blaser M, Wu Y, Zou X, Dong Z, Taylor P, et al. Helicobacter pylori seropositivity and subsite-specific gastric cancer risks in Linxian, China. J Natl Cancer Inst. 2001;93:226–233. doi: 10.1093/jnci/93.3.226. [DOI] [PubMed] [Google Scholar]
- 26.Yang CS. Vitamin nutrition and gastroesophageal cancer. J Nutr. 2000;130:338S–339S. doi: 10.1093/jn/130.2.338S. [DOI] [PubMed] [Google Scholar]
- 27.Guo W, Blot WJ, Li JY, Taylor PR, Liu BQ, Wang W, Wu YP, Zheng W, Dawsey SM, Li B. A nested case-control study of oesophageal and stomach cancers in the Linxian nutrition intervention trial. Int J Epidemiol. 1994;23:444–450. doi: 10.1093/ije/23.3.444. [DOI] [PubMed] [Google Scholar]
- 28.Ji BT, Chow WH, Yang G, McLaughlin JK, Zheng W, Shu XO, Jin F, Gao RN, Gao YT, Fraumeni JF. Dietary habits and stomach cancer in Shanghai, China. Int J Cancer. 1998;76:659–664. doi: 10.1002/(sici)1097-0215(19980529)76:5<659::aid-ijc8>3.0.co;2-p. [DOI] [PubMed] [Google Scholar]
- 29.Blot WJ, Li JY, Taylor PR, Guo W, Dawsey SM, Li B. The Linxian trials: mortality rates by vitamin-mineral intervention group. Am J Clin Nutr. 1995;62:1424S–1426S. doi: 10.1093/ajcn/62.6.1424S. [DOI] [PubMed] [Google Scholar]
- 30.International Agency for Research on Cancer (IARC) IARC Monograph Vol. 83. Tobacco smoke and involuntary smoking. Lyon: IARC Press, Cited 2005-04-15; Available from: http: //www-cie.iarc.fr/htdocs/monographs/vol83/01-smoking.html.
- 31.Ji BT, Chow WH, Yang G, McLaughlin JK, Gao RN, Zheng W, Shu XO, Jin F, Fraumeni JF, Gao YT. Body mass index and the risk of cancers of the gastric cardia and distal stomach in Shanghai, China. Cancer Epidemiol Biomarkers Prev. 1997;6:481–485. [PubMed] [Google Scholar]
- 32.Setiawan VW, Zhang ZF, Yu GP, Lu QY, Li YL, Lu ML, Wang MR, Guo CH, Yu SZ, Kurtz RC, et al. Protective effect of green tea on the risks of chronic gastritis and stomach cancer. Int J Cancer. 2001;92:600–604. doi: 10.1002/ijc.1231. [DOI] [PubMed] [Google Scholar]
- 33.Ji BT, Chow WH, Yang G, McLaughlin JK, Gao RN, Zheng W, Shu XO, Jin F, Fraumeni JF, Gao YT. The influence of cigarette smoking, alcohol, and green tea consumption on the risk of carcinoma of the cardia and distal stomach in Shanghai, China. Cancer. 1996;77:2449–2457. doi: 10.1002/(SICI)1097-0142(19960615)77:12<2449::AID-CNCR6>3.0.CO;2-H. [DOI] [PubMed] [Google Scholar]
- 34.Wu AH, Yang D, Pike MC. A meta-analysis of soyfoods and risk of stomach cancer: the problem of potential confounders. Cancer Epidemiol Biomarkers Prev. 2000;9:1051–1058. [PubMed] [Google Scholar]
- 35.Mahady GB, Pendland SL, Yun GS, Lu ZZ, Stoia A. Ginger (Zingiber officinale Roscoe) and the gingerols inhibit the growth of Cag A+ strains of Helicobacter pylori. Anticancer Res. 2003;23:3699–3702. [PMC free article] [PubMed] [Google Scholar]
- 36.World Health Organization (WHO) National cancer control programmes: policies and managerial guidelines. Second version. Geneva: World Health Organization; 2002. [Google Scholar]


