Abstract
Obesity is recognized as a major worldwide health problem. Excess weight gain is the most common cause of elevated blood pressure (BP) and markedly increases the risk of metabolic, cardiovascular and renal diseases. Although the mechanisms linking obesity with hypertension have not been fully elucidated, increased sympathetic nervous system (SNS) activity contributes to elevated BP in obese subjects. Recent evidence indicates that leptin and the central nervous system (CNS) melanocortin system, including melanocortin 4 receptors (MC4R), play a key role in linking obesity with increased SNS activity and hypertension. Leptin, a peptide-hormone produced by adipose tissue, crosses the blood–brain barrier and activates brain centers that control multiple metabolic functions as well as SNS activity and BP via the CNS melanocortin system. The crosstalk between peripheral signals (e.g., leptin) and activation of CNS pathways (e.g., MC4R) that regulate energy balance, SNS activity and BP represents an important target for treating obesity and its metabolic and cardiovascular consequences.
Keywords: obesity, hypertension, blood pressure, glucose regulation, sympathetic activity
Introduction
Obesity has become one of the most serious health problems worldwide in developing as well as in industrialized countries. Excess weight gain enhances the risk for many diseases such as diabetes, cancer, kidney disease and hypertension. Epidemiological studies show that obesity affects 17% of children and adolescents in the United States, a number that has tripled from one generation ago. Approximately, 36% of adults are obese with a body mass index (BMI) of >30 and more than 65% of the adult population is overweight with a BMI of >25 (1–3). Similar trends have been noted in many other countries (1).
Obesity and Hypertension
The higher risk for cardiovascular diseases in overweight and obese subjects is associated with increased incidence of diabetes, dyslipidemia, atherosclerosis, renal disease and hypertension (4,5). For example, it is estimated that excess weight may contribute as much as 85% of the risk for developing diabetes and up to 75% of the risk for essential hypertension (4,6–8).
Although the precise mechanisms by which obesity elevates blood pressure (BP) are still not fully understood, excess weight gain increases renal sodium reabsorption and impairs pressure-natriuresis, ultimately requiring increased BP to reestablish sodium and fluid balance (5). The factors that alter renal sodium reabsorption and pressure natriuresis during excess weight gain are still unclear but involve, among other mechanisms, activation of the sympathetic nervous system (SNS). In this review, we focus on two main factors, leptin and the brain melanocortin system, that appear to play a key role in linking obesity with elevations in SNS and BP.
Activation of the SNS in Obesity
Clinical and experimental studies have demonstrated that excess weight gain is associated with increased SNS activity (6,10). Obesity induced by high-fat diets in dogs or rodents enhances SNS activity as early as the first week of feeding (6,7) and modest weight gain in lean human subjects is associated with increased SNS activity (9,10). Evidence of increased SNS activity in obesity also comes from the studies, showing that chronic pharmacological blockade of adrenergic receptors causes greater reductions in BP in obese compared to lean hypertensive subjects (11,12). However, in obesity the rise in SNS activity is modest and occurs in specific tissues such as skeletal muscle and the kidneys, whereas cardiac sympathetic activity is reduced (9). Increased renal SNS activity leading to sodium retention and impaired pressure-natriuresis is the primary mechanism for elevated BP with excess weight gain as renal denervation abolishes sodium retention and hypertension during the development of obesity (13).
The degree of increased SNS activity in obesity appears to vary according to body fat distribution with visceral obesity causing greater SNS activation than subcutaneous obesity (14). However, in most human studies only muscle SNS activity has been evaluated rather than renal SNS activity which appears to mediate increased BP associated with obesity (7,12). Therefore, more studies are needed to determine the influence of body fat distribution on the regulation of renal SNS activity, and its association with obesity-induced hypertension in various populations.
Many factors have been proposed to contribute to elevated SNS activity in obesity including impaired baroreflex sensitivity, angiotensin II, hyperinsulinemia, sleep apnea, hypoghrelinemia and hypoadiponectemia (the role of these factors in contributing to obesity–hypertension has been reviewed elsewhere) (6,12,15,16). However, mounting evidence suggests that two key mechanisms by which weight gain increases SNS activity are hyperleptinemia and activation of melanocortin 4 receptors (MC4R) in the central nervous system (CNS). In this review, we discuss how leptin, a peptide produced by white adipose tissue in proportion to the amount of body fat, activates its receptors on pro-opiomelanocortin (POMC) neurons, located mainly in the hypothalamus and brainstem, to stimulate release of alpha-melanocyte-stimulating hormone (α-MSH), the endogenous agonist of MC4R, to increase SNS activity and BP. The MC4R, a G protein-coupled receptor which activates adenylyl cyclase, leading to increased intracellular level of cAMP, is expressed in the hypothalamus as well as in brainstem neurons that regulate cardiovascular function.
Leptin and Cardiometabolic
Leptin crosses the blood–brain barrier, apparently via a receptor-mediated process, and activates its receptors in several regions of the CNS including the hypothalamus and brainstem. The most studied CNS action of leptin is its ability to reduce appetite and to increase energy expenditure. Leptin deficiency or leptin receptor (LR) mutations that prevent normal activation of its intracellular signaling events lead to early-onset, morbid obesity (17–19).
Leptin may Link Obesity with Increased Sympathetic Activity and Hypertension
Despite marked obesity and many other characteristics of the metabolic syndrome including hyperinsulinemia, dyslipidemia, hyperglycemia, visceral adiposity and insulin resistance, rodents and humans with leptin gene or LR mutations are not hypertensive and do not exhibit increased SNS activity (19–22). In fact, humans with leptin gene mutation show postural hypotension and attenuated renin–angiotensin–aldosterone system responses to upright posture (18). Mice with leptin deficiency (ob/ob mice) tend to have lower BP than lean control mice despite severe obesity and metabolic abnormalities that would normally tend to raise BP (20,22). These findings suggest that a functional leptin system may be necessary for obesity to increase SNS activity and raise BP. Further evidence supporting a role for leptin in contributing to SNS activation and hypertension in obesity also comes from the studies, showing that leptin administration, either peripherally or directly into the brain, raises renal SNS activity and BP (2,23–28). Moreover, chronic leptin infusion in lean rodents causes gradual and sustained increases in BP that can be completely prevented by chronic α and β adrenergic receptor blockade (28). Transgenic mice that overexpress leptin also exhibit increased BP which can be reversed by adrenergic blockade (29). Taken together, these observations indicate that 1) increased circulating levels of leptin, comparable to those found in obesity, can raise BP and SNS activity and 2) a functional leptin system is required for obesity to increase SNS activity and BP.
Selective Leptin Resistance in Obesity
The fact that most obese humans have high circulating leptin levels and continue to ingest excess calories is consistent with the concept that obesity causes resistance to the anorexic effects of leptin. Experimental studies have also shown that leptin is much less effective in suppressing appetite in obese than in lean animals (30,31). To the extent that obesity induces global resistance to leptin, including the SNS response to leptin, one would expect the chronic hypertensive actions of leptin to also be attenuated in obese subjects. However, it appears that obesity may induce “selective” leptin resistance, whereby the renal SNS responses to leptin are maintained, whereas the appetite suppressant effects of leptin are attenuated (31). Although there is experimental support for this concept (23–26,30), there have been few studies that have tested whether the chronic effects of hyperleptinemia on BP and SNS activity are attenuated in obese compared to lean subjects. The CNS pathways and cell signaling mechanisms that underlie selective leptin resistance in obesity are only beginning to be elucidated and represent an important area for investigation.
Intracellular Signaling Events and Selective Activation of LRs in Specific Areas of the CNS may Contribute to Selective Leptin Resistance in Obesity
The LR is a cytokine receptor that activates Janus tyrosine kinases (JAKs), especially JAK2 (32). Activation of LR increases activity of intracellular JAK2. In the CNS, LR-induced activation of JAK2 triggers three major intracellular pathways: 1) phosphorylation of tyrosine (Tyr) residue 1138 leads to recruitment of latent signal transducers and activators of transcription 3 (STAT3) to the LR–JAK2 complex, resulting in phosphorylation and nuclear translocation of STAT3 to regulate transcription. This pathway is thought to play a major role in the regulation of body weight homeostasis by leptin; 2) insulin receptor substrate (IRS2) phosphorylation activates phosphatidylinositol 3-kinase (PI3K) which appears to be involved in regulating rapid nongenomic events affecting neuronal activity and neuropeptide release and 3) Tyr985 phosphorylation recruits the tyrosine phosphatase (SHP2) to activate the ERK (MAPK) pathway (Fig. 1) which may contribute to the effects of leptin on thermogenesis and peripheral glucose utilization.
FIG 1.
LR signaling pathways. Shp2, tyrosine phosphatase; IRS, insulin receptor substrate; STAT3, signal transducers and activators of transcription 3; SOCS, suppressor of cytokine signaling; PTP1B, protein tyrosine phosphatase; NPY, neuropeptide Y; AgRP, agouti-related protein. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Deletion of each of these signaling pathways in the CNS results in varying degrees of obesity although only neuron-specific deletion of the STAT3 pathway appears to mimic the obese phenotype found in ob/ob mice (33). Deletion of STAT3 in the entire CNS also causes hyperphagia and attenuated leptin-induced anorexia. We recently showed that deletion of STAT3 specifically in POMC neurons results only in mild obesity associated with normal responses to leptin on appetite and thermogenesis (34). However, deletion of STAT3 in POMC neurons markedly attenuated leptin’s ability to raise BP (34). These observations suggest that leptin-induced STAT3 activation in POMC neurons is important for BP regulation, whereas STAT3 activation in other groups of neurons is more important in mediating the effects of leptin on appetite and energy expenditure.
Previous acute studies also suggest that activation of the IRS2–PI3K pathway may contribute to leptin’s ability to increase SNS activity and BP. For instance, pharmacological blockade of PI3K abolished the acute effects of leptin to increase renal SNS activity (35). To our knowledge, however, no long-term studies have been conducted to test whether chronic blockade of the IRS2–PI3K pathway abolishes or attenuates the chronic effects of sustained hyperleptinemia to increase SNS activity and BP. Deletion of IRS2 in the entire CNS causes only moderate obesity and slight hyperphagia associated with normal anorexic and weight loss responses to leptin (36–38). These observations indicate that although IRS2–PI3K signaling modestly contributes to body weight homeostasis but may mediate, at least in part, the action of leptin on SNS activity. Further studies are needed, however, to assess the role of this pathway in mediating the chronic effects of leptin on renal SNS activity and BP in obesity.
The Shp2–MAPK pathway plays an important role in controlling energy balance and metabolism as evident by the finding that pan-neuronal deletion of Shp2 causes obesity associated with hyperphagia and diabetes (39). Deletion of Shp2 specifically in forebrain neurons, however, has been reported to cause early-onset obesity and metabolic syndrome mainly by reducing energy expenditure rather than promoting increased food intake (40). Although these observations support an important role for Shp2 signaling in regulation of appetite, energy expenditure and glucose homeostasis, no previous studies, to our knowledge, have directly examined the role of Shp2 in mediating the actions of leptin on appetite, metabolism and cardiovascular regulation including regulation of SNS activity and BP.
Collectively, these observations are consistent with the possibility that differential activation of these three intracellular signaling pathways by the LR may mediate divergent control of appetite, energy balance, glucose homeostasis and cardiovascular function and may help explain the development of selective leptin resistance in obesity. LR activation in different regions of the CNS may also contribute to the development of selective leptin resistance in obesity. High levels of LR mRNA and protein are expressed in the forebrain, especially in the ventromedial hypothalamus, arcuate nucleus (ARC) and dorsomedial hypothalamus (41). However, LR mRNA and immunoreactivity are also highly expressed in extra-hypothalamic brain regions, including the vasomotor centers of the brainstem (17). Thus, depending on its site of action leptin may control appetite independently of its effect to increase SNS activity and BP.
Vong et al. (42) showed that LR deletion in gabaergic neurons mimics most of the obese phenotypes observed in ob/ob mice. Although the authors suggest that leptin’s action on pre-synaptic gabaergic neurons decreases inhibitory tone to post-synaptic POMC neurons, the mechanism responsible for obesity in these mice remains unclear. In addition, gabaergic neurons are widely distributed in the CNS and further studies are still needed to examine which neuronal types and brain sites are most important in mediating the effects of leptin on appetite and body weight homeostasis as well as on SNS activity. Deletion of LRs in the ARC of the hypothalamus markedly reduced the acute effects of leptin to increase renal SNS activity and attenuated the rise in BP induced by high-fat feeding (43). We have shown that activation of LRs specifically in POMC neurons, which are present in the ARC and brainstem, is critical for leptin’s ability to increase BP and improve glucose homeostasis but not for its effect to reduce appetite (44). These findings suggest that activation of LR in POMC neurons is necessary for the chronic effects of leptin on BP regulation and certain metabolic functions, whereas LR activation in other neurons appears to play a more important role in mediating the effects of leptin on appetite and energy balance (44) (Fig. 2).
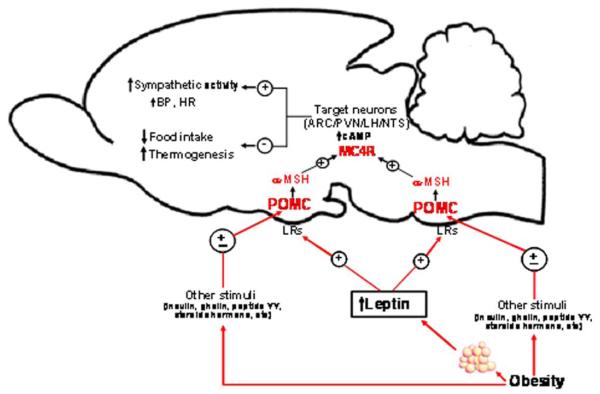
FIG 2.

Leptin–brain melanocortin system interaction. Schematic representation of the metabolic and cardiovascular effects of the leptin–melanocortin system pathway. CNS, central nervous system; Na, sodium; MC4R, melanocortin-4 receptor; POMC, proopiomelanocortin; SNS, sympathetic nervous system. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Another potential mechanism contributing to selective leptin resistance in obesity is differential control of LR signaling by negative regulators such as protein tyrosine phosphatase-1B (PTP1B) and suppressor of cytokine signaling (Socs3) (Fig. 1), both of which may be altered in obesity. PTP1B regulates the JAK/STAT3 signaling pathway by dephosphorylation of JAK2 (38), whereas Socs3 negatively regulates LR signaling by inhibiting JAK activity (45). Deletion of PTP1B enhances leptin sensitivity and confers resistance to high-fat-diet-induced obesity and type II diabetes (46). Mice with whole-body PTP1B deficiency also exhibit higher baseline BP and amplified BP response to leptin compared to wild-type controls (46). In addition, specific deletion of PTP1B in POMC neurons does not alter food intake but increases energy expenditure, suggesting that alterations in PTP1B levels in certain areas of the brain or in specific neuronal types (e.g., POMC neurons) may modulate SNS activity and BP with minimal effect on the anorexic action of leptin.
Socs3 expression is regulated by the STAT3 pathway and, like PTP1B, is a negative regulator of LR signaling that may contribute to leptin resistance. For example, Socs3 deficiency increases leptin sensitivity and attenuates development of obesity caused by a high-fat diet (47,48). The importance of Socs3 signaling in regulating SNS activity, however, remains unclear. Together, PTP1B and Socs3 could play an important role in modulating the appetite, metabolic and cardiovascular actions of leptin and contribute to the development of selective leptin resistance in obesity. However, additional studies are needed to explore how obesity alters PTP1B and Socs3 expression and whether these negative regulators of LR signaling may be potential targets for novel therapies to treat obesity and its metabolic and cardiovascular abnormalities.
The CNS Melanocortin System Mediates Most of the Effects of Leptin on SNS Activity and BP Regulation
Although the precise intracellular events and brain regions by which leptin regulates body weight homeostasis and cardiovascular function are not completely understood, strong evidence shows that leptin requires activation of the brain melanocortin system, including activation of POMC neurons and MC4R, to exert most of its effects on renal SNS activity and BP regulation (49,50). POMC neurons are located in the ARC of the hypothalamus and in the nucleus of the tractus solitarius (NTS) which are important sites for controlling metabolic and cardiovascular functions. Acute and chronic studies have shown that activation of MC4R using synthetic agonists increases renal SNS activity, BP and HR in experimental animal models as well as in humans (51–55). Moreover, mice with whole-body MC4R deficiency are hyperphagic and obese, and have many characteristics of metabolic syndrome including hyperglycemia, hyperinsulinemia, visceral adiposity and dislypidemia despite markedly elevated blood leptin levels (49–51,56); these mice are also completely unresponsive to the effects of leptin to reduce appetite and to raise BP (50). In addition, mutations in POMC or MC4R genes lead to severe early-onset obesity and dysregulation of appetite in humans who, despite pronounced obesity, exhibit reduced BP, HR and 24-h urinary catecholamine excretion, lower prevalence of hypertension and reduced SNS activity in response to acute stress (53–55). Taken together, these studies strongly suggest that a functional MC4R is necessary for obesity and hyperleptinemia to increase SNS activity and cause hypertension (Fig. 3).
FIG 3.
Leptin–melanocortin pathway in obesity-induced hypertension. Schematic representation of the interactions of obesity, leptin and melanocortin system. LRs, leptin receptors; (±), stimulation or attenuation; POMC, pro-opiomelanocortin; α-MSH, alpha melanocyte-stimulating hormone; MC4R, melanocortin-4 receptor; ARC, arcuate nucleus of the hypothalamus; PVN, paraventricular nucleus of the hypothalamus; LH, lateral hypothalamus; NTS, nucleus of the tractus solitarius; cAMP, cyclic adenosine monophosphate; BP, blood pressure; HR, heart rate. [Color figure can be viewed in the online issue, which is available at wileyonlinelibrary.com.]
Divergent Control of Metabolic and Cardiovascular Functions by MC4R Activation in Specific Areas of the CNS
Another factor that may contribute to selective leptin resistance in obesity is differential control of appetite, metabolic and cardiovascular function by MC4R activation in various regions of the brain. For example, MC4R located in PVN neurons appear to be more important in regulating appetite while exerting minimal role in the control of thermogenesis, whereas MC4R located in POMC neurons seem to play a more prominent role in regulating thermogenesis and energy expenditure (56,57). Although the previous studies using acute microinjections of MC4R agonists and antagonists suggest that MC4R in the PVN and brainstem modulate SNS activity and BP, additional long-term studies are needed to examine the brain regions where MC4R regulate SNS activity and cardiovascular function.
The Brain Melanocortin System also Contributes to Appetite and BP Regulation Independent of Leptin’s Actions
MC4R also appear to exert an important role in modulating SNS activity and regulating appetite independent of leptin’s actions. For instance, pharmacological antagonism of MC4R causes greater reductions in BP in obese compared to lean Zucker rats while increasing food intake in both obese and lean rats (58), demonstrating a role for MC4R in regulating SNS activity and BP as well as food intake in rats with mutated LRs. We also observed that chronic MC4R antagonism markedly reduced BP and heart rate to the same extent achieved by adrenergic receptor blockade in lean spontaneously hypertensive rats (SHRs), a well-known model of hypertension associated with high sympathetic tone with nearly normal leptin levels (51). These results suggest that the CNS melanocortin pathway is active in obese Zucker rats as well as in nonobese SHRs via mechanisms that are not dependent on LR activation. Thus, MC4R may play a more fundamental role in the control of SNS activity that goes beyond its role in contributing to leptin’s effects on BP and obesity-induced hypertension.
Although leptin is the most recognized activator of the brain melanocortin system, other factors also modulate the activity of this pathway. POMC neuronal activity is altered by glucose, insulin, ghrelin, peptide YY, nesfatin-1, steroid hormones and nicotine (59–64). Also, little is known about the downstream mediators of MC4R effects on cardiovascular regulation. Previous acute studies suggest that brain-derived neurotrophic factor, corticotrophin-releasing hormone and oxytocin may mediate, at least in part, the physiologic actions of MC4R activation (65–67). However, no chronic studies, to our knowledge, have been conducted to examine which of these potential factors mediates the long-term effect of MC4R on appetite, SNS activity and BP regulation.
Conclusions
Excess weight gain is a major cause of human essential hyper-tension and is associated with SNS activation, renal sodium retention and impaired pressure natriuresis. Hyperleptinemia and activation of the brain melanocortin system (e.g., POMC neurons and MC4R) are key factors that link obesity with increased renal SNS activity and hypertension. However, the neuronal and molecular pathways by which the leptin–MC4R axis exerts differential control of appetite, metabolic and cardiovascular functions in obesity have not been fully elucidated. Understanding this differential control of metabolism and cardiovascular function is critical for the development of better therapies to treat obesity and its associated metabolic and cardiovascular disorders.
Acknowledgements
The authors’ research was supported by a grant from the National Heart, Lung and Blood Institute (PO1 HL 51971) and by American Heart Association Scientist Development Grants to Jussara M. do Carmo and Alexandre A. da Silva.
References
- [1].Yach D, Stuckler D, Brownell KD. Epidemiologic and economic consequences of the global epidemics of obesity and diabetes. Nat Med. 2006;12:62–66. doi: 10.1038/nm0106-62. [DOI] [PubMed] [Google Scholar]
- [2].Department of Health and Human Services—Center for disease Control and Prevention Obesity and overweight trends in the U.S. 2011 Available at: http://www.cdc.gov/nccdphp/dnpa/obesity/trend/index.htm.
- [3].Anderson SE, Whitaker RC. Prevalence of obesity among US preschool children in different racial and ethnic groups. Arch. Pediatr. Adolesc. Med. 2009;163:344–348. doi: 10.1001/archpediatrics.2009.18. [DOI] [PubMed] [Google Scholar]
- [4].Wilson PWF, D’Agostino RB, Sullivan L, Parise H, Kannel WB. Overweight and obesity as determinants of cardiovascular risk—the Framingham experience. Arch. Intern. Med. 2002;162:1867–1872. doi: 10.1001/archinte.162.16.1867. [DOI] [PubMed] [Google Scholar]
- [5].Hall JE, Crook ED, Jones DW, Wofford MR, et al. Mechanisms of obesity-associated cardiovascular and renal disease. Am. J. Med. Sci. 2002;324:127–137. doi: 10.1097/00000441-200209000-00003. [DOI] [PubMed] [Google Scholar]
- [6].Davy KP, Hall JE. Obesity and hypertension: two epidemics or one? Am. J. Physiol. Regul. Integr. Comp. Physiol. 2004;286:R803–R813. doi: 10.1152/ajpregu.00707.2003. [DOI] [PubMed] [Google Scholar]
- [7].Hall JE. The kidney, hypertension, and obesity. Hypertension. 2003;41:625–633. doi: 10.1161/01.HYP.0000052314.95497.78. [DOI] [PubMed] [Google Scholar]
- [8].Hypponen E, Virtanen SM, Kenward MG, Knip M, Akerblom HK, et al. Obesity, increased linear growth, and risk of type 1 diabetes in children. Diab. Care. 2000;23:1755–1760. doi: 10.2337/diacare.23.12.1755. [DOI] [PubMed] [Google Scholar]
- [9].Vaz M, Jennings G, Turner A, Cox H, Lambert G, et al. Regional sympathetic nervous activity and oxygen consumption in obese normotensive subjects. Circulation. 1997;18:3423–3429. doi: 10.1161/01.cir.96.10.3423. [DOI] [PubMed] [Google Scholar]
- [10].Davy KP, Orr JS. Sympathetic nervous system behavior in human obesity. Neurosci. Biobehav. Rev. 2009;33:116–124. doi: 10.1016/j.neubiorev.2008.05.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Hall JE, da Silva AA, do Carmo JM, Dubinion J, Hamza S, et al. Obesity-induced hypertension: role of sympathetic nervous system, leptin, and melanocortins. J. Biol. Chem. 2010;285:17271–17276. doi: 10.1074/jbc.R110.113175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wofford MR, Anderson DC, Brown CA, Jones DW, Miller ME, et al. Antihypertensive effect of alpha and beta adrenergic blockade in obese and lean hypertensive subjects. Am. J. Hypertens. 2001;14:694–698. doi: 10.1016/s0895-7061(01)01293-6. [DOI] [PubMed] [Google Scholar]
- [13].Kassab S, Kato T, Wilkins FC, Chen R, Hall JE, et al. Renal denervation attenuates the sodium retention and hypertension associated with obesity. Hypertension. 1995;25:893–897. doi: 10.1161/01.hyp.25.4.893. [DOI] [PubMed] [Google Scholar]
- [14].Straznicky NE, Eikelis N, Lambert EA, Esler MD. Mediators of sympathetic activation in metabolic syndrome obesity. Curr. Hyper-tens. Rep. 2008;10:440–447. doi: 10.1007/s11906-008-0083-1. [DOI] [PubMed] [Google Scholar]
- [15].Mancia G, Bousquet P, Elghozi JL, Esler M, Grassi G, et al. The sympathetic nervous system and the metabolic syndrome. J. Hypertens. 2007;25:909–920. doi: 10.1097/HJH.0b013e328048d004. [DOI] [PubMed] [Google Scholar]
- [16].da Silva AA, do Carmo JM, Dubinion J, Hall JE. The role of the sympathetic nervous system in obesity-related hypertension. Curr. Hypertens. Rep. 2009;11:206–11. doi: 10.1007/s11906-009-0036-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Schwartz MW, Woods SC, Porte D, Jr., Seeley RJ, Baskin DG. Central nervous system control of food intake. Nature. 2000;404:661–671. doi: 10.1038/35007534. [DOI] [PubMed] [Google Scholar]
- [18].Farooqi S, O’Rahilly S. Genetics of obesity in humans. Endocr. Rev. 2006;27:710–718. doi: 10.1210/er.2006-0040. [DOI] [PubMed] [Google Scholar]
- [19].Ozata M, Ozdemir IC, Licinio J. Human leptin deficiency caused by a missense mutation: multiple endocrine defects, decreased sympathetic tone, and immune system dysfunction indicate new targets for leptin action, greater central than peripheral resistance to the effects of leptin, and spontaneous correction of leptin-mediated defects. J. Clin. Endocrinol. Metab. 1999;10:3686–3695. doi: 10.1210/jcem.84.10.5999. [DOI] [PubMed] [Google Scholar]
- [20].Mark AL, Shafer RA, Correia ML, Morgan DA, Sigmund CD, et al. Contrasting blood pressure effects of obesity in leptin deficient ob/ob mice and agouti yellow obese mice. J. Hypertens. 1999;17:1949–1953. doi: 10.1097/00004872-199917121-00026. [DOI] [PubMed] [Google Scholar]
- [21].Cohen P, Connie Z, Cai X, Montez JM, Rohani SC, et al. Selective deletion of leptin receptor in neurons leads to obesity. J. Clin. Invest. 2001;108:1113–1121. doi: 10.1172/JCI13914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].do Carmo JM, Bassi M, da Silva AA, Hall JE. Control of cardiovascular, metabolic and respiratory functions during prolonged obesity in leptin-deficient and diet-induced obese mice. Hypertension. 2008;15:109. [Google Scholar]
- [23].Kalil GZ, Haynes WG. Sympathetic nervous system in obesity-related hypertension: mechanisms and clinical implications. Hypertens. Res. 2012;35:4–16. doi: 10.1038/hr.2011.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Correia ML, Haynes WG, Rahmouni K, Morgan DA, Sivitz WI, et al. The concept of selective leptin resistance: evidence from agouti yellow obese mice. Diabetes. 2002;51:439–442. doi: 10.2337/diabetes.51.2.439. [DOI] [PubMed] [Google Scholar]
- [25].Rahmouni K, Fath MA, Seo S, Thedens DR, Berry CJ, et al. Leptin resistance contributes to obesity and hypertension in mouse models of Bardet-Biedl syndrome. J. Clin. Invest. 2008;118:1458–1467. doi: 10.1172/JCI32357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Rahmouni K, Morgan DA, Morgan GM, Mark AL, Haynes WG. Role of selective leptin resistance in diet-induced obesity hypertension. Diabetes. 2005;54:2012–2018. doi: 10.2337/diabetes.54.7.2012. [DOI] [PubMed] [Google Scholar]
- [27].Shek EW, Brands MW, Hall JE. Chronic leptin infusion increases arterial pressure. Hypertension. 1998;31:409–414. doi: 10.1161/01.hyp.31.1.409. [DOI] [PubMed] [Google Scholar]
- [28].Carlyle M, Jones OB, Kuo JJ, Hall JE. Chronic cardiovascular and renal actions of leptin-role of adrenergic activity. Hypertension. 2002;39:496–501. doi: 10.1161/hy0202.104398. [DOI] [PubMed] [Google Scholar]
- [29].Aizawa-Abe M, Ogawa Y, Masuzaki H, Ebihara K, Satoh N, et al. Pathophysiological role of leptin in obesity-related hypertension. J. Biol. Chem. 2000;105:1243–1252. doi: 10.1172/JCI8341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [30].Prior LJ, Eikelis N, Armitage JA, Davern PJ, Burke SL, et al. Exposure to a high-fat diet alters leptin sensitivity and elevates renal sympathetic nerve activity and arterial pressure in rabbits. Hypertension. 2010;55:862–868. doi: 10.1161/HYPERTENSIONAHA.109.141119. [DOI] [PubMed] [Google Scholar]
- [31].Mark AL, Correia ML, Rahmouni K, Haynes WG. Selective leptin resistance: a new concept in leptin physiology with cardiovascular implications. J. Hypertens. 2002;20:1245–1250. doi: 10.1097/00004872-200207000-00001. [DOI] [PubMed] [Google Scholar]
- [32].Ghilardi N, Skoda RC. The leptin receptor activates Janus kinase 2 and signals for proliferation in a factor-dependent cell line. Mol. Endocrinol. 1997;11:393–399. doi: 10.1210/mend.11.4.9907. [DOI] [PubMed] [Google Scholar]
- [33].Gao Q, Wolfgang MJ, Neschen S. Disruption of neural signal transducer and activator of transcription 3 causes obesity, diabetes, infertility, and thermal dysregulation. Proc. Natl. Acad. Sci. USA. 2004;101:4661–4666. doi: 10.1073/pnas.0303992101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Dubinion JH, do Carmo JM, Adi A, Hamza S, da Silva AA, et al. Role of proopiomelanocortin neuron Stat3 in regulating arterial pressure and mediating the chronic effects of leptin. Hypertension. 2013;61:1066–1074. doi: 10.1161/HYPERTENSIONAHA.111.00020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Rahmouni K, Haynes WG, Morgan DA, Mark AL. Intracellular mechanisms involved in leptin regulation of sympathetic outflow. Hypertension. 2002;41:763–767. doi: 10.1161/01.HYP.0000048342.54392.40. [DOI] [PubMed] [Google Scholar]
- [36].Choudhury AI, Heffron H, Smith MA, Al-Qassab H, Xu AW, et al. The role of insulin receptor substrate 2 in hypothalamic and beta cell function. J. Clin. Invest. 2005;15:940–950. doi: 10.1172/JCI24445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Lin X, Taguchi A, Park S, Kushner JA, Li F, et al. Dysregulation of insulin receptor substrate 2 in beta cells and brain causes obesity and diabetes. J. Clin. Invest. 2004;114:908–916. doi: 10.1172/JCI22217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [38].Burks D, de Mora JF, Schubert M, Withers DJ, Myers MG, et al. IRS-2 pathways integrate female reproduction and energy homeostasis. Nature. 2000;407:377–382. doi: 10.1038/35030105. [DOI] [PubMed] [Google Scholar]
- [39].Krajewska M, Banares S, Zhang EE, Huang X, Scadeng M, et al. Development of diabesity in mice with neuronal deletion of Shp2 tyrosine phosphatase. Am. J. Pathol. 172:1312–1324. doi: 10.2353/ajpath.2008.070594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [40].Zhang EE, Chapeau E, Hagihara K, Feng GS. Neuronal Shp2 tyrosine phosphatase controls energy balance and metabolism. Proc. Natl. Acad. Sci. USA. 2004;9:16064–16069. doi: 10.1073/pnas.0405041101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Kloek C, Haq AK, Dunn SL, Lavery HJ, Banks AS, et al. Regulation of Jak kinases by intracellular leptin receptor sequences. J. Biol. Chem. 2002;277:41547–41555. doi: 10.1074/jbc.M205148200. [DOI] [PubMed] [Google Scholar]
- [42].Vong L, Ye C, Yang Z, Choi B, Chua S, Jr., et al. Leptin action on GABAergic neurons prevents obesity and reduces inhibitory tone to POMC neurons. Neuron. 2011;71:142–154. doi: 10.1016/j.neuron.2011.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Harlan SM, Morgan DA, Agassandian K, Guo DF, Cassell MD, et al. Ablation of the leptin receptor in the hypothalamic arcuate nucleus abrogates leptin-induced sympathetic activation. Circ. Res. 2011;108:808–812. doi: 10.1161/CIRCRESAHA.111.240226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].do Carmo JM, da Silva AA, Cai Z, Lin S, Dubinion JH, et al. Control of blood pressure, appetite, and glucose by leptin in mice lacking leptin receptors in proopiomelanocortin neurons. Hypertension. 2011;57:918–926. doi: 10.1161/HYPERTENSIONAHA.110.161349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [45].Myers MP, Anderson JN, Cheng A, Tremblay ML, Horvath CM, et al. TYK2 and JAK2 are substrates of protein-tyrosine phosphatase 1B. J. Biol. Chem. 2001;276:47771–47774. doi: 10.1074/jbc.C100583200. [DOI] [PubMed] [Google Scholar]
- [46].Belin de Chantemele EJ, Muta K, Mintz J, Tremblay ML, Marrero MB, et al. Protein tyrosine phosphatase 1B, a major regulator of leptin-mediated control of cardiovascular function. Circulation. 2009;120:753–763. doi: 10.1161/CIRCULATIONAHA.109.853077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Bjorbaek C, El-Haschimi K, Frantz JD, Flier JS. The role of SOCS3 in leptin signaling and leptin resistance. J. Biol. Chem. 1999;274:30059–30065. doi: 10.1074/jbc.274.42.30059. [DOI] [PubMed] [Google Scholar]
- [48].Mori H, Hanada R, Hanada T, Aki D, Mashima R, et al. Socs3 deficiency in the brain elevates leptin sensitivity and confers resistance to diet-induced obesity. Nat. Med. 2004;10:739–743. doi: 10.1038/nm1071. [DOI] [PubMed] [Google Scholar]
- [49].Tallam LS, Stec DE, Willis MA, da Silva AA, Hall JE. Melanocortin-4 receptor-deficient mice are not hypertensive or salt-sensitive despite obesity, hyperinsulinemia, and hyperleptinemia. Hypertension. 2005;46:326–332. doi: 10.1161/01.HYP.0000175474.99326.bf. [DOI] [PubMed] [Google Scholar]
- [50].Tallam LS, da Silva AA, Hall JE. Melanocortin-4 receptor mediates chronic cardiovascular and metabolic actions of leptin. Hypertension. 2006;48:58–64. doi: 10.1161/01.HYP.0000227966.36744.d9. [DOI] [PubMed] [Google Scholar]
- [51].da Silva AA, do Carmo JM, Kanyicska B, Dubinion J, Brandon E, et al. Endogenous melanocortin system activity contributes to the elevated arterial pressure in spontaneously hypertensive rats. Hypertension. 2008;51:884–890. doi: 10.1161/HYPERTENSIONAHA.107.100636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Kievit P, Halem H, Marks DL, Dong JZ, Glavas MM, et al. Chronic treatment with a melanocortin 4 receptor agonist causes weight loss, reduces insulin resistance, and improves cardiovascular function in diet-induced obese Rhesus Macaques. Diabetes. 2013;62:490–497. doi: 10.2337/db12-0598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [53].Greenfield JR. Melanocortin signaling and the regulation of blood pressure in human obesity. J. Neuroendocrinol. 2011;23:186–193. doi: 10.1111/j.1365-2826.2010.02088.x. [DOI] [PubMed] [Google Scholar]
- [54].Sayk F, Heutling D, Dodt C, Iwen KA, Wellhoner JP, et al. Sympathetic function in human carriers of melanocortin-4 receptor gene mutations. J. Clin. Endocrinol. Metab. 2002;95:1998–2002. doi: 10.1210/jc.2009-2297. [DOI] [PubMed] [Google Scholar]
- [55].Greenfield JR, Miller JW, Keogh JM, Henning E, Satterwhite JH, et al. Modulation of blood pressure by central melanocortinergic pathways. N. Engl. J. Med. 2009;360:44–52. doi: 10.1056/NEJMoa0803085. [DOI] [PubMed] [Google Scholar]
- [56].Balthasar N, Dalgaard LT, Lee CE, Yu J, Funahashi H, et al. Divergence control of melanocortin pathways in the control of food intake and energy expenditure. Cell. 2005;123:493–505. doi: 10.1016/j.cell.2005.08.035. [DOI] [PubMed] [Google Scholar]
- [57].do Carmo JM, da Silva AA, Rushing JS, Dubinion J, Hall M, et al. Differential control of appetite and cardiovascular function after selective rescue of melanocortin-4 receptor in proopiomelanocortin neurons. Hypertension. 2011;12:380. [Google Scholar]
- [58].do Carmo JM, da Silva AA, Rushing JS, Hall JE. Activation of the central melanocortin system contributes to the increased arterial pressure in obese Zucker rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2012;302:R561–R567. doi: 10.1152/ajpregu.00392.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Ma X, Zubcevic L, Ashcroft FM. Glucose regulates the effects of leptin on hypothalamic POMC neurons. Proc. Natl. Acad. Sci. USA. 2008;105:9811–9816. doi: 10.1073/pnas.0800952105. [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- [60].Plum L, Belgardt B, Bruming J. Central insulin action in energy and glucose homeostasis. J. Clin. Invest. 2006;116:1761–1766. doi: 10.1172/JCI29063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Batterham RL, Cowley MA, Small CJ, Herzog H, Cohen MA, et al. Gut hormone PYY (3–36) physiologically inhibits food intake. Nature. 2002;418:650–654. doi: 10.1038/nature00887. [DOI] [PubMed] [Google Scholar]
- [62].Blum M, Roberts JL, Wardlaw SL. Androgen regulation of proopiomelanocortin gene expression and peptide content in the basal hypothalamus. Endocrinology. 1989;124:2283–2288. doi: 10.1210/endo-124-5-2283. [DOI] [PubMed] [Google Scholar]
- [63].Gao Q, Mezei G, Nie Y, Choi CS, Bechmann I, et al. Anorectic estrogen mimics leptin’s effect on rewiring of melanocortin cells and Stat3 signaling in obese animals. Nat. Med. 2007;13:89–94. doi: 10.1038/nm1525. [DOI] [PubMed] [Google Scholar]
- [64].Jo YH, Su Y, Gutierrez-Juarez G, Chua S. Oleic acid directly regulates POMC neuron excitability in the hypothalamus. J. Neurophysiol. 2009;101:2305–2316. doi: 10.1152/jn.91294.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Nicholson JR, Peter JC, Lecourt AC, Barde YA, Hofbauer KG. Melanocortin-4 receptor activation stimulates hypothalamic brain-derived neurotrophic factor release to regulate food intake, body temperature and cardiovascular function. J. Neuroendocrinol. 2007;19:974–982. doi: 10.1111/j.1365-2826.2007.01610.x. [DOI] [PubMed] [Google Scholar]
- [66].Shimizu H, Inoue K, Mori M. The leptin-dependent and -independent melanocortin signaling system: regulation of feeding and energy expenditure. J. Endocrinol. 2007;193:1–9. doi: 10.1677/JOE-06-0144. [DOI] [PubMed] [Google Scholar]
- [67].Tolson KP, GEmelli T, Elmquist JK, Zinn AR, Kublaoui BM. Postnatal Sim1 deficiency causes hyperphagic obesity and reduced MC4R and oxytocin expression. J. Neurosci. 2010;10:3803–3812. doi: 10.1523/JNEUROSCI.5444-09.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]