Abstract
Purpose
To explore two issues that are relevant to inclusion of PQRS reporting in a value-based payment system: (1) what are the characteristics of PQRS reports and the providers who file them; and (2) could PQRS provide active attribution information to supplement existing attribution algorithms?
Design and Methods
Using data from five states for the years 2008 (the first full year of the program) and 2009, we examined the number and type of providers who reported PQRS measures and the types of measures that were reported. We then compared the PQRS reporting provider to the provider who supplied the plurality of the beneficiary’s non-hospital evaluation and management (NH-E&M) visits.
Results
Although PQRS-reporting providers provide only 17 percent of the beneficiary’s NH-E&M visits on average in 2009, the provider who provided the plurality of visits supplied only 50 percent of such visits, on average.
Implications
PQRS reporting alone cannot solve the attribution problem that is inherent in traditional fee-for-service Medicare, but as PQRS participation increases, it could help improve both attribution and information regarding the quality of health care services delivered to Medicare beneficiaries.
Keywords: Medicare, physician, payment, value, PQRS, attribution
Introduction
Under the Patient Protection and Affordable Care Act of 2010 or ACA (P.L. 111–148), the Medicare program is required to incorporate measures of “value” into the payment systems for health care providers, including physicians and hospitals in traditional fee-for-service (FFS) Medicare. “Value” implies consideration of both cost and quality—a major change in the philosophy underlying Medicare payment. Although considerable progress has been made in recent years developing measures of health care quality, until recently information on the quality of health care services at the provider level in the Medicare program was limited to measures computable from administrative claims data.
The 2006 Tax Relief and Health Care Act (P.L. 109–432) authorized CMS to establish the Physician Quality Reporting System (PQRS),1 which enables “eligible professionals”2 to report additional data not only measures of process quality, but actual health outcomes. PQRS reports are the primary data source in the Quality Reporting option of the Medicare value-based modifier physician payment system.
The contribution of PQRS reporting to the value-based modifier will depend first on the content of PQRS reports and the types of providers who file them. In addition, however, payment systems based on provider performance require the experience of individual patients to be linked to specific providers through some type of attribution algorithm. In this paper, we analyze data from five states for the first two full years of PQRS reporting (2008 and 2009), in order to address these two questions:
What are the characteristics of PQRS reports and the providers who file them?
Could PQRS reports provide useful information to supplement existing attribution algorithms?
The PQRS System
PQRS reports are submitted on standard Part B claims forms. Each PQRS measure has a numeric code. Each measure is accompanied by a definition of the “denominator;” i.e., the beneficiaries who are eligible for reporting on that measure.
The measures CMS has selected for PQRS are developed and approved by organizations such as the National Quality Form (NQF). Some measures represent undesirable outcomes, while others represent desirable outcomes. New measures are added each year and measures from previous years can be updated or deleted. A list of the 267 measures for 2012 can be found at http://www.cms.gov/PQRS/15_MeasuresCodes.asp#TopOfPage. The PQRS measures include both process quality measures and outcome measures, such as the patient’s blood pressure and HbA1c level. Examples include:
Diabetes Mellitus: Hemoglobin A1c Poor Control in Diabetes Mellitus. Developed by the NCQA. A patient aged 18 through 75 years with diabetes mellitus whose most recent hemoglobin A1c was greater than nine percent.
Coronary Artery Disease (CAD): Oral Antiplatelet Therapy Prescribed for Patients with CAD. Developed by the American Medical Association-sponsored Physician Consortium on Performance Improvement. A patient aged 18 years and older with a diagnosis of CAD who was prescribed oral antiplatelet therapy.
Participation in PQRS is voluntary, but there are rewards and penalties associated with participation. Currently, providers earn an incentive payment simply for reporting PQRS measures. Originally, in order to earn an incentive payment, providers were required to report on at least three quality measures and report on at least eighty percent of the beneficiaries who were eligible for each measure. The percentage was reduced to fifty percent in 2011 (Centers for Medicare & Medicaid Services, 2012c).
The first PQRS reporting period was the second half of 2007 (Centers for Medicare & Medicaid Services, 2008). In 2008, providers who successfully completed the reporting requirements received an incentive payment equal to 1.5 percent of their Part B allowed charges furnished during the reporting period. The percentage was increased to 2 percent in 2009 and 2010. Under the provisions of ACA in 2010, PQRS will provide bonuses of 1.0 percent for 2011 and 0.5 percent for 2012 through 2014. In 2015 PQRS switches from bonuses for reporters to penalties for non-reporters. The penalty is 1.5 percent for 2015 and increases to 2.0 percent for 2016 and subsequent years (Centers for Medicare & Medicaid Services, 2011).3 The rewards and penalties for 2015 are based on the 2013 reporting year.
PQRS reports also are the basis for Medicare’s quality-tiering methodology in the new physician value-based modifier payment system. As Centers for Medicare & Medicaid Services (2013a) explains:
“Our overall approach to implementing the Value Modifier is based on participation in the PQRS. Groups of physicians with 100 or more eligible professionals must participate in the PQRS by self-nominating/registering for the PQRS as a group and reporting at least one measure, or electing PQRS Administrative Claims option in order to avoid the –1.0% downward Value Modifier payment adjustment. If the group elects quality-tiering, then calculation of the Value Modifier could result in an upward, downward, or no payment adjustment based on performance.”
Most practices opted not to participate in PQRS in the early years, although the participation rate of eligible professionals increased from 15 percent in 2007, the first year of the program, to 24 percent in 2010. In 2010, CMS made incentive payments to reporting professionals totaling nearly $400 million (Centers for Medicare & Medicaid Services, 2012a). Participation was expected to grow substantially in 2013, because 2013 is the base year for payments and penalties that begin in 2015.
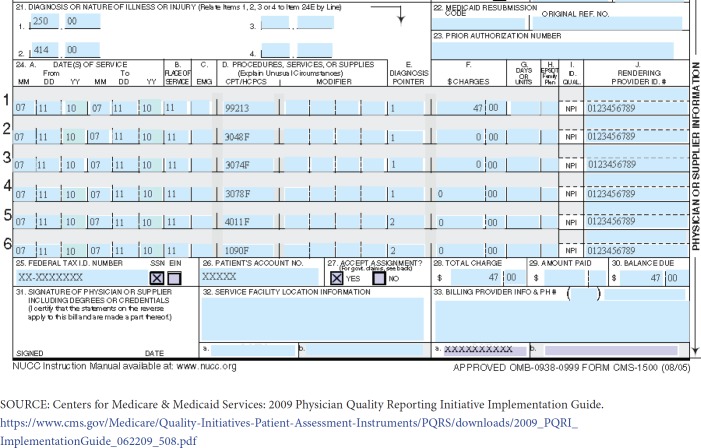
PQRS measures initially were reported by individual providers, but beginning in 2010, group practices had the option to report at the group level, with the same incentive award applied to the Part B allowed charges furnished by the group. Individual physicians can choose to report either as individuals or part of a group practice, but not both. In 2009, providers could report PQRS measures in two different ways: through their Part B claims (Exhibit 1) or through a PQRS-qualified registry. Starting in 2010, practices also could report PQRS measures through electronic health records.
Exhibit 1. A PQRS Claims-Based Report.
Attributing Quality Measures to Providers
Provider-level measures of cost and quality begin with the experience of individual patients. Individual patients’ experiences then are aggregated up to the provider level through some type of patient attribution rule. There are two main dimensions along which attribution rules can be classified. First, attribution can occur before or after the care has been provided. An attribution system is ex ante if providers know at the beginning of a reporting period which beneficiaries will be attributed to their practices. In ex post systems, beneficiaries are assigned to providers at the end of a reporting period, using some type of algorithm that generally reflects the frequency or consistency of encounters or dollars.
Second, attribution systems vary in the degree to which the provider explicitly takes the responsibility for the patient. In active attribution systems, the patient, provider, or both explicitly agree that the beneficiary’s care will be attributed to the specific provider. In passive attribution systems, beneficiaries could be assigned to providers without either the beneficiary’s or provider’s consent.
Any health plan or health care system that requires enrollees to designate a primary care physician “gatekeeper” has adopted an active, ex ante attribution system. The United Kingdom’s National Health Service is another example of an active, ex ante system (Roland, 2004).
Examples of passive, ex post attribution include the CMS Medicare Physician Group Practice Demonstration (Centers for Medicare & Medicaid Services, 2009), the CMS Shared Savings Program under the Accountable Care Organization initiative (Centers for Medicare & Medicaid Services, 2013b), the CMS Resource Use Report initiative (Centers for Medicare & Medicaid Services, 2010), and the physician value-based modifier payment system (Centers for Medicare & Medicaid Services, 2013a). Active, ex ante attribution would be difficult to implement in the traditional FFS Medicare program, because beneficiaries have unrestricted access to providers.
There are many different passive attribution rules. Mehrotra et al. (2010) compares eleven alternatives. However, the most common attribution rule in current CMS initiatives is the plurality rule. The plurality rule assigns each beneficiary to the provider from whom she obtained the largest amount of ambulatory care, often measured by non-hospital evaluation and management (NH-E&M) visits. The plurality rule assigns beneficiaries to one, and only one, provider.
Pham et al. (2007) provide descriptive statistics on a number of different attribution algorithms, including the plurality of evaluation and management visits, including and excluding visits to specialists, and the majority of visits. The authors found that care for Medicare beneficiaries was widely dispersed among many providers, which limits “the effectiveness of pay-for-performance initiatives that rely on a single retrospective method of assigning responsibility for patient care.” That finding applies to passive, ex post attribution rules, but because PQRS reporting is provider-initiated, it has the potential to provide attribution information that is at active, and perhaps to some degree, ex ante, as well.
In the attribution portion of this analysis, we use a single dataset to compare two methods of assigning beneficiaries to providers: (1) the provider who accounted for the plurality of the beneficiary’s non-hospital evaluation and management (NH-E&M) visits; and (2) beneficiaries for whom the provider reported a PQRS measure.
Data
Our analyses are based on a 100 percent sample4 of 2008 and 2009 Medicare claims data from five states: California, Colorado, New Jersey, North Dakota, and Florida. The states were chosen by CMS for use in a larger analysis of Medicare provider payment policy and represent a mix of regions, average levels of utilization and cost, and urbanicity. We obtained PQRS data directly from the Part B claims submitted by providers, rather than from registry data. The registry data were deemed by CMS to be less reliable during 2008 and we excluded registry data in 2009 to maintain consistency across the two years’ results. In order to apply the “plurality of NH-E&M visits” attribution rule, we aggregated claims into visits using the rule that all claims with the same dates of service made to the same provider constituted one visit.
Results
What are the characteristics of PQRS reports and the providers who file them?
Exhibit 2 shows the percent of providers who submitted PQRS reports in 2008 and 2009. Providers were classified into four categories (primary care, medical specialist, surgical specialist, and practitioner assistant) based on the specialty codes in claims data.5 The number of NPIs falling outside these categories was less than 0.01 percent in both 2008 and 2009. Those NPIs were excluded from subsequent analyses.
Exhibit 2. Percent of NPIs Filing at Least One PQRS Report.
| Percent of all NPIs reporting a PQRS measure | Percent of PQRS-reporting NPIs by type of provider | |||
|---|---|---|---|---|
| Type of NPI | 2008 | 2009 | 2008 | 2009 |
| Primary care | 9.0 | 22.3 | 14.0 | 21.0 |
| Medical specialist | 16.0 | 23.9 | 67.0 | 59.1 |
| Surgical specialist | 6.8 | 14.8 | 5.9 | 7.7 |
| Practitioner asst. | 20.3 | 29.0 | 13.1 | 12.2 |
| Total | 13.8 | 23.0 | 100.0 | 100.0 |
| Total # of PQRS-reporting NPIs | 24,154 | 40,428 | 24,154 | 40,428 |
SOURCE: Authors’ analyses.
Practitioner assistants had the highest PQRS participation rates in both years, but the percentage of providers filing at least one PQRS report increased substantially in all four groups, particularly among primary care providers and surgeons.
Exhibit 2 also shows that medical specialists filed more PQRS reports than any other provider group in both 2008 and 2009—well over half of all reports. However, primary care providers5 increased their percentage of all reports by seven percentage points from 2008 to 2009, from 14 percent to 21 percent of all reports. A table showing greater detail on the types of providers reporting PQRS measures can be found in the Appendix (Exhibit A1).
Exhibit 3 shows the fifteen most frequently reported non-hospital PQRS measures cross-tabulated by the type of provider. The first four measures could be termed administrative process measures and can be completed easily by the provider or the practice. The remainder of the most frequent measures, however, could be termed either process quality of care measures or health outcome measures. Altogether, these fifteen measures account for approximately 67 percent of all reported measures in 2008 and 2009. Most of the top 15 measures were filed by medical specialists (65.9 percent) or providers in primary care (24.7 percent).
Exhibit 3. Most Frequently Reported PQRS Quality Data Codes (QDC) in 2008 and 2009.
| Percent of Each Type of PQRS Report Filed ByProviders | |||||
|---|---|---|---|---|---|
| PQRS # and Description | Primary Care | Medical Specialists | Surgical Specialists | Practitioner Assistants | Total |
| #125: HIT - Adoption/Use of e-Prescribing | 37.6 | 35.7 | 50.5 | 19.3 | 36.4 |
| #124: HIT - Adoption/Use of Health Information Technology (Electronic Health Records) | 10.0 | 8.8 | 12.3 | 7.9 | 9.3 |
| #125: HIT - Adoption/Use of e-Prescribing | 17.0 | 5.5 | 7.5 | 6.4 | 8.5 |
| #125: HIT - Adoption/Use of e-Prescribing | 16.8 | 5.1 | 5.6 | 5.2 | 8.0 |
| #12: Primary Open Angle Glaucoma: Optic Nerve Evaluation | 0.0 | 7.5 | 0.0 | 0.0 | 4.9 |
| #14: Age-Related Macular Degeneration: Dilated Macular Examination | 0.0 | 6.8 | 0.0 | 0.0 | 4.5 |
| #20/#30: Perioperative Care: Timing of Antibiotic Prophylaxis - Ordering Physician/Administering Physician | 0.1 | 4.8 | 3.1 | 25.8 | 4.3 |
| #54/#55: Electrocardiogram Performed for Non-Traumatic Chest Pain/for Syncope | 1.2 | 5.5 | 0.2 | 3.9 | 4.1 |
| #124: HIT - Adoption/Use of Health Information Technology (Electronic Health Records) | 0.6 | 5.4 | 1.2 | 1.1 | 3.8 |
| #6: Oral Antiplatelet Therapy Prescribed for Patients with Coronary Artery Disease | 1.5 | 4.1 | 0.3 | 5.4 | 3.3 |
| #114: Inquiry Regarding Tobacco Use | 3.8 | 2.5 | 5.4 | 1.8 | 3.0 |
| #114: Inquiry Regarding Tobacco Use | 3.6 | 2.5 | 4.3 | 1.6 | 2.9 |
| #20/#30: Perioperative Care: Timing of Antibiotic Prophylaxis - Ordering Physician/Administering Physician | 0.0 | 3.0 | 6.0 | 13.2 | 2.8 |
| #47: Advance Care Plan | 6.0 | 0.8 | 1.0 | 6.9 | 2.3 |
| #130: Universal Documentation and Verification of Current Medications in the Medical Record | 1.7 | 2.0 | 2.5 | 1.5 | 1.9 |
| Percent of top measures reported by each type of provider | 24.7 | 65.9 | 5.9 | 3.5 | 100.0 |
| Top 15 measures as a percent of all measures reported | 67.4 | 67.5 | 64.8 | 66.5 | 67.2 |
| Total number of 2008 and 2009 reports of the top 15 measures | 3,587,713 | 9,596,699 | 857,167 | 512,788 | 14,554,367 |
SOURCE: Authors’ analyses.
The usefulness of PQRS reporting as a source of quality information could be attenuated if providers selectively choose beneficiaries on whom to file PQRS reports. Exhibit 4 compares the age, sex, and Hierarchical Condition Category (HCC) risk scores6 for reported and non-reported beneficiaries, all of whom saw a PQRS reporting provider. The results show that reported beneficiaries were slightly older and more likely to be male. They also were significantly less likely to be non-White and dually enrolled in Medicare and Medicaid.
Exhibit 4. Comparison of PQRS Reported and Non-reported Beneficiaries.
| 2008 | 2009 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Variable | Non-reported beneficiaries | Reported beneficiaries | Difference | Non-reported beneficiaries | Reported beneficiaries | Difference | |||||
| Age (years) | 74.83 | 76.55 | 1.72 | 75.12 | 76.00 | 0.87 | |||||
| Male (percent) | 41.19 | 42.70 | 1.52 | 41.91 | 40.93 | –0.98 | |||||
| Non-White (%) | 15.18 | 13.84 | –1.34 | 15.27 | 13.40 | –1.87 | |||||
| Dually Enrolled (%) | 20.09 | 17.83 | –2.26 | 19.45 | 16.07 | –3.38 | |||||
| HCC Risk Score | |||||||||||
| Overall | 2.03 | 2.40 | 0.37 | 2.00 | 2.07 | 0.07 | |||||
| Diabetes cohort | 3.58 | 3.79 | 0.21 | 3.48 | 3.50 | 0.01 | |||||
| CHF cohort | 4.95 | 5.16 | 0.21 | 4.89 | 4.90 | 0.00 | |||||
| Arthritis cohort | 3.58 | 3.89 | 0.32 | 3.51 | 3.54 | 0.03 | |||||
| Depression cohort | 3.97 | 4.53 | 0.56 | 3.90 | 4.01 | 0.11 | |||||
| M.I. cohort | 4.56 | 4.77 | 0.21 | 4.50 | 4.48 | –0.02 | |||||
| Stroke cohort | 5.01 | 5.29 | 0.29 | 4.94 | 4.92 | –0.02 | |||||
| COPD cohort | 4.22 | 4.53 | 0.31 | 4.15 | 4.17 | 0.02 | |||||
NOTES: M.I.=Myocardial Infarction. All differences are statistically significant at the 0.05 minimum with the exception of the CHF and stroke HCC scores in 2009. Statistical tests for percent Male, White, and Dually Enrolled were based on chi-squared statistics for the difference in k proportions. Statistical tests for the remaining variables were based on separate-sample variance t-statistics.
SOURCE: Authors’ analyses.
One would expect the sample of beneficiaries on whom a report is filed to be in worse health, on average, than non-reported beneficiaries, because many PQRS measures are appropriate only for beneficiaries who have a health problem. The data on HCC risk scores in Exhibit 4 show that is indeed the case. Both the overall HCC risk score and the HCC scores for disease-specific cohorts of beneficiaries are uniformly higher for reported than non-reported beneficiaries. These results suggest that providers were not in fact “cherry picking” healthy beneficiaries during the early years of PQRS reporting. However, if the health outcomes reported in PQRS are incorporated into the value-based modifier payment system, the incentives for selective reporting could change.
Can PQRS reporting improve attribution?
As noted earlier, reporting a PQRS quality measure on a beneficiary could be interpreted as an indication that the provider is willing to take responsibility for at least one aspect of the beneficiary’s care, although there is no formal acknowledgment of that responsibility in the PQRS system. Because providers voluntarily link themselves to individual patients under PQRS, PQRS attribution could constitute a form of active attribution. PQRS attribution could be somewhat ex ante, as well, because the provider may continue to provide care to the beneficiary after filing a PQRS report.
There are several dimensions of PQRS reporting that bear on its usefulness in attribution. We refer to these dimensions as uniqueness, consistency, and overlap. An attribution system is “unique” if it assigns a beneficiary to only one provider. CMS’s choice of the plurality rule suggests a preference for unique attribution. Exhibit 5 shows that in 2008, nearly three quarters of the beneficiaries had a PQRS report from only one provider. However, that percentage fell to just over half the beneficiaries in 2009, as participation in PQRS reporting increased. The percentage of beneficiaries receiving PQRS reports from 2 or 3 providers increased dramatically from 2008 to 2009. Thus, it appears that PQRS reporting is unlikely to provide unique pairings of beneficiaries and providers in the future.
Exhibit 5. Number of Different NPIs Submitting PQRS Reports on the Same Beneficiary.
| Number of NPIs submitting a PQRS report on the same beneficiary | 2008 (Percent) | 2009 (Percent) |
|---|---|---|
| 1 | 73.4 | 52.8 |
| 2 | 18.0 | 25.1 |
| 3 | 5.4 | 11.6 |
| 4 | 1.9 | 5.4 |
| 5 or more | 1.3 | 5.1 |
| Total Percent | 100 | 100 |
| Total number of beneficiaries | 1,213,249 | 2,906,515 |
| Average Number of NPIs | 1.4 | 1.9 |
| 53 percent of beneficiaries received a PQRS report in both 2008 and 2009 who had at least one PQRS report from the same NPI in both 2008 and 2009 | ||
NOTE: The unit of analysis is the beneficiary.
SOURCE: Authors’ analyses.
Next, we examined the consistency of provider and patient linkages based on PQRS reporting in 2008 versus 2009. Overall, 53 percent of all beneficiaries who had a PQRS report in both 2008 and 2009 had at least one report from the same NPI in both years (Exhibit 5).
Finally, we examined the issue of overlap between PQRS reports and the plurality attribution rule. First, we examined the degree of commonality between the PQRS reporting provider and the plurality provider. Among primary care physicians, 50.2 percent of the beneficiaries on whom the physician reported a PQRS measure also saw that physician for the plurality of their NH-E&M visits. That percentage increased for primary care and medical specialists in 2009 versus 2008, but decreased for surgical specialists and practitioner assistants (Exhibit 6).
Exhibit 6. Average percent of visits provided by the PQRS-reporting and plurality NPIs and attribution overlap.
| 2008 | 2009 | |||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Type of NPI | Type of NPI | |||||||||||||||||||||||||||||||
| Primary Care | Medical Specialist | Surgical Specialist | Practitioner Assistant | Total | Primary Care | Medical Specialist | Surgical Specialist | Practitioner Assistant | Total | |||||||||||||||||||||||
| Average percent of NH-E&M visits provided by the PQRS-reporting NPI | 28.4 | 7.9 | 15.4 | 6.9 | 10.9 | 38.9 | 11.1 | 17.7 | 8.8 | 17.0 | ||||||||||||||||||||||
| Number of beneficiary/PQRS NPI combinations | 219,556 | 1,323,682 | 85,401 | 85,731 | 1,714,370 | 1,110,993 | 3,792,557 | 387,436 | 235,768 | 5,526,754 | ||||||||||||||||||||||
| Average percent of NH-E&M visits provided by the plurality NPI | 59.3 | 41.5 | 47.3 | 42.9 | 50.5 | 58.6 | 40.9 | 46.7 | 43.2 | 50.0 | ||||||||||||||||||||||
| Number of beneficiary/plurality NPI combinations | 3,584,333 | 3,113,751 | 646,006 | 219,101 | 7,563,191 | 3,495,845 | 2,957,612 | 622,020 | 237,334 | 7,312,811 | ||||||||||||||||||||||
| Overlap of PQRS and plurality NPI (percent) | 50.2 | 24.9 | 33.6 | 16.1 | 28.2 | 55.0 | 26.4 | 26.7 | 12.7 | 31.5 | ||||||||||||||||||||||
SOURCE: Authors’ analyses.
Second, we examined the percent of a beneficiary’s NH-E&M visits provided by the PQRS-reporting NPI versus the plurality NPI. The percent of NH-E&M visits provided by the plurality NPI is virtually certain to be higher than the percent provided by the PQRS-reporting NPI, but the former provides a useful benchmark percentage for FFS Medicare beneficiaries. The results also are shown in Exhibit 6. The unit of analysis in Exhibit 6 is a beneficiary-NPI combination, because the beneficiary could have received a PQRS report for NH-E&M visits from more than one provider. On average, the PQRS-reporting provider (NPI) received 10.9 percent of NH-E&M visits for beneficiaries on whom they submitted a PQRS report in 2008 and 17.0 in 2009. The highest percentage in 2009 was for primary care providers (38.9 percent) and the lowest was for practitioner assistants (8.8 percent). Although these percentages are small, they need to be kept in perspective. Only about half of a beneficiary’s NH-E&M visits were provided by the plurality NPI in both 2008 and 2009. These results reflect the diversity of providers that Medicare beneficiaries see for their basic care.
If attribution is used for payment purposes then it is important to know how many providers are assigned beneficiaries under different attribution systems. We found that in 2008, 80.5 percent of NPIs would have been assigned beneficiaries under plurality of the NH-E&M visits rule versus only 13.8 percent under PQRS-based attribution (The latter percentage is shown in Exhibit 2). The same percentages for 2009 were 80.7 percent for the plurality rule and 23.0 percent for PQRS-based attribution.
These percentages mask an important potential contribution of PQRS reporting to attribution, however. We found that 31 percent of beneficiaries with a PQRS report from a primary care provider had no other NH-E&M visits with that provider in 2008. Thus, it is possible that the addition of PQRS information to the current plurality-based attribution system could increase the number of providers to whom some beneficiaries can be attributed.
Conclusions
PQRS participation was limited in 2008, the first full year of the program, but increased substantially in 2009, and the penalties for non-participation, coupled with the PQRS into the value-based modifier for physician payment in 2015 (based on 2013 data), likely will result in a dramatic, further increase in participation.
PQRS measures include administrative process, process of care, and health outcome measures. The most frequently reported measures in 2008 and 2009 were administrative process measures involving health information technology and e-prescribing, but a number of process quality and health outcome measures also are found in the fifteen most frequently reported measures.
Among the beneficiaries of PQRS-reporting providers, HCC risk scores generally are higher for reported beneficiaries than non-reported beneficiaries, in part, because the “denominator” conditions for many PQRS measure are illness-based. At this time, there does not seem to be strong evidence that providers “cherry-pick” healthy patients on which to report PQRS measures, though that issue bears close monitoring in the future, especially when PQRS-reporting is incorporated fully into the value-based modifier payment system.
The greatest degree of provider accountability likely will be achieved by an active, ex ante designation of a primary care provider by Medicare beneficiaries. In the absence of that politically difficult modification to FFS Medicare, policymakers may be interested in marginal improvements to passive, ex post attribution algorithms. Because PQRS reporting is provider-initiated and links providers to patients, it has the potential to add active attribution information to the passive, ex post attribution algorithms currently used in Medicare Accountable Care Organizations (ACOs) and value-based modifier physician payment systems. Supplementing existing algorithms with PQRS information also might allow CMS to attribute some patients who have a PQRS report but no other NH-E&M visits.
In 2009, the PQRS-reporting provider received only seventeen percent of the beneficiary’s NH-E&M visits, although the percentage for primary care PQRI reporters was nearly forty percent. But the plurality provider supplied only 50 percent of NH-E&M visits to their attributed beneficiaries, on average.
It is clear from these results that in its current form with current participation rates, PQRS-based attribution alone cannot solve FFS Medicare’s inherent attribution problem. In FFS Medicare, all attribution systems represent an attempt to impose some type of provider accountability on an essentially uncoordinated care system.
At this point, it would be premature to draw conclusions regarding the problems and opportunities represented by the PQRS system. Taking the longer view, it is important to appreciate the accomplishment of having over 250 consensus-based quality measures available for reporting. Any attempt to improve the value of health care services in the U.S. requires data on quality. PQRS reporting is an important step in that direction.
Disclosure
This work was completed under Medicare/Medicaid Research and Demonstration Task Order Contract (MRAD/TOC) HHSM-500-2005-000271 Task Order 0004. Project Officer: Craig Caplan. All of the authors had full access to the data and none of the authors have a conflict of interest.
Acknowledgment
The authors would like to acknowledge the important contributions of David Knutson, Robert Kane, Medha Karmarkar, Shri Parashuram, and Craig Caplan.
Appendix
Exhibit A1. Specialty of PQRS-Reporting NPIs.
| Provider Specialty | Type | 2008 (Percent) | 2009 (Percent) |
|---|---|---|---|
| Emergency medicine | MS | 20.91 | 13.41 |
| Internal medicine | PC | 7.45 | 11.00 |
| Anesthesiology | MS | 11.30 | 9.18 |
| Family practice | PC | 5.33 | 8.76 |
| Diagnostic radiology | MS | 6.65 | 5.43 |
| Physician assistant | PA | 5.05 | 4.53 |
| Ophthalmology | MS | 4.82 | 4.43 |
| Cardiology | MS | 2.96 | 4.24 |
| CRNA | PA | 5.31 | 3.81 |
| Nurse practitioner | PA | 2.55 | 3.73 |
| Optometry | MS | 2.96 | 2.57 |
| Physical therapist | MS | 4.08 | 2.41 |
| Orthopedic surgery | SS | 1.40 | 2.13 |
| Pathology | MS | 3.05 | 2.05 |
| Dermatology | MS | 0.28 | 1.66 |
| Obstetrics/gynecology | SS | 0.41 | 1.53 |
| Hematology/oncology | MS | 1.54 | 1.44 |
| Gastroenterology | MS | 0.48 | 1.40 |
| General surgery | SS | 1.35 | 1.30 |
| Urology | SS | 1.12 | 1.28 |
| Pulmonary disease | MS | 0.61 | 1.12 |
| Neurology | MS | 0.63 | 1.11 |
| Podiatry | MS | 0.26 | 1.07 |
| Other | 13.95 | 17.64 | |
| Total | 100.00 | 100.00 |
NOTES: PC=Primary care; MS = Medical specialty; SS = surgical specialty; PA = physician assistant
SOURCE: Authors’analyses.
Footnotes
http:/www.cms.hhs.gov/pqri/ (Centers for Medicare & Medicaid Services, 2012a). Note that, when first introduced, PQRS was termed the Physician Quality Reporting Initiative, a name that was changed in 2011 to Physician Quality Reporting System. For simplicity, we will use PQRS when referring to either version throughout this report.
Throughout the paper, we use the term “provider” to refer to the reporting unit; however, “eligible professionals” include those listed at the following Web page: http://www.cms.hhs.gov/PQRI/Downloads/EligibleProfessionals.pdf
There now is a second quality reporting system run by Medicare: the Electronic Prescribing (eRx) Incentive Program, authorized under Section 132 of the Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) (P.L. 110–275). eRX was introduced in 2009 as a separate incentive vehicle for reporting physicians and other professionals who are successful electronic prescribers. Prior to 2009, the eRx measure was an individual measure within the 2008 Physician Quality Reporting System. By 2010, incentive payments to participating prescribers totaled almost $271 million (Centers for Medicare & Medicaid Services, 2012b).
By “100 percent sample,” we mean that the data were selected by first identifying physicians, in the five states, who submitted FFS physician claims in 2008 or 2009 and then collecting all claims for those beneficiaries served by those physicians.
Primary Care Providers include: general practice, family practice and internal medicine.
Medical Specialists include: allergy/immunology, otolaryngology, anesthesiology, cardiology, dermatology, interventional pain management, gastroenterology, osteopathic manipulative therapy, neurology, ophthalmology, pathology, physical medicine and rehabilitation, psychiatry, pulmonary disease, diagnostic radiology, chiropractic, nuclear medicine, nephrology, optometry, infectious disease, endocrinology, podiatry, psychologist, audiologist, physical therapist, rheumatology, occupational therapist, registered dietician, pain management, addiction medicine licensed clinical social worker, critical care, hematology, hematology/oncology, preventive medicine, neuropsychiatry, radiation oncology, emergency medicine, interventional radiology, optician, gynecologist/oncologist, and medical oncology.
Surgical Specialists include: general surgery, obstetrics gynecology, oral surgery, orthopedic surgery, plastic and reconstructive surgery, colorectal surgery, thoracic surgery, urology, hand surgery, peripheral vascular disease, vascular surgery, cardiac surgery, maxillofacial surgery, and surgical oncology.
Practitioner Assistants include: anesthesiologist assistance, certified nurse midwife, CRNA, clinical laboratory, certified clinical nurse specialist, physician assistant, and nurse practitioner..
The HCC risk scores are used to adjust payments to Accountable Care Organizations and private health plans (Medicare Advantage) contracting with the Medicare program.
References
- Centers for Medicare & Medicaid Services. Quality Reporting Initiative: 2007 reporting experience. 2008 Retrieved from https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/2007_PQRI_Program.html.
- Centers for Medicare & Medicaid Services. PGP fact sheet. 2009 Retrieved from http://www.cms.gov/Medicare/Demonstration-Projects/DemoProjectsEvalRpts/downloads//PGP_Fact_Sheet.pdf. [PubMed]
- Centers for Medicare & Medicaid Services. 2010 http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/downloads//2010_QRUR_FAQ.pdf [PubMed]
- Centers for Medicare & Medicaid Services. Medicare EHR Incentive Program, Physician Quality Reporting System and e-Prescribing Comparison. 2011 Retrieved from https://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNProducts/downloads/EHRIncentivePayments-ICN903691.pdf.
- Centers for Medicare & Medicaid Services. Physician Quality Reporting System. 2012a Retrieved from http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/PQRS/index.html?redirect=/pqri/
- Centers for Medicare & Medicaid Services. 2010 Reporting Experience Including Trends (2007–2011) Physician Quality Reporting System and Electronic Prescribing (eRx) Incentive Program 2/22/2012. 2012b Retrieved from http://web.mdinteractive.com/files/uploaded/2010%20PQRS%20and%20eRx%20Experience%20Report_03162012.pdf.
- Centers for Medicare & Medicaid Services. 2010 Reporting Experience Including Trends (2007–2011) 2012c Retrieved from http://www.mdinteractive.com/files/uploaded/2010%20PQRS%20and%20eRx%20Experience%20Report_03162012.pdf.
- Centers for Medicare & Medicaid Services. “Summary of 2015 Physician Value-based Payment Modifier Policies,”. 2013a Retrieved from http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/PhysicianFeedbackProgram/Downloads/CY2015ValueModifierPolicies.pdf.
- Centers for Medicare & Medicaid Services. “Medicare Shared Savings Program: Frequently Asked Questions,”. 2013b Retrieved from http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/MSSP-FAQs.pdf.
- Mehrotra A, Adams JL, Thomas W, Mcglynn E. The effect of different attribution rules on individual physician cost profiles. Annals of Internal Medicine. 2010;152:649–654. doi: 10.7326/0003-4819-152-10-201005180-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pham HH, Schrag D, O’Malley AS, Wu B, Bach PB. Care Patterns in Medicare and Their Implications for Pay for Performance. The New England Journal of Medicine. 2007;356(11):1130–1139. doi: 10.1056/NEJMsa063979. [DOI] [PubMed] [Google Scholar]
- Roland M. Linking physicians’ pay to the quality of care—A major experiment in the United Kingdom. The New England Journal of Medicine. 2004;351(14):1448–1454. doi: 10.1056/NEJMhpr041294. [DOI] [PubMed] [Google Scholar]