Abstract
Objective
To test the association between pulmonary dead-space fraction (VD/VT) and mortality in patients with ARDS (Berlin Definition, PaO2/FiO2 ≤ 300 mm Hg; PEEP ≥ 5 cm H2O) enrolled into a clinical trial incorporating lung-protective ventilation.
Design
Prospective, multi-center study.
Setting
Medical-surgical intensive care units in the United States.
Subjects
126 ALI patients enrolled into a phase III randomized, placebo-controlled study of aerosolized albuterol.
Interventions
None
Measurements and Main Results
VD/VT and pulmonary mechanics were measured within 4 hours of enrollment and repeated daily on study days 1 and 2 in subjects requiring arterial blood gases for clinical management. At baseline, non-survivors had a trend towards higher VD/VT compared to survivors (0.62 ± 0.11 vs. 0.56 ± 0.11 respectively, p = 0.08). Differences in VD/VT between non-survivors and survivors became significant on study days 1 (0.64 ± 0.12 vs. 0.55 ± 0.11 respectively, p = 0.01) and 2 (0.67 ± 0.12 vs. 0.56 ± 0.11 respectively, p=0.004). Likewise, the association between VD/VT and mortality was significant on study day 1 (odds ratio per 0.10 change in VD/VT [95% confidence interval]: 6.84 [1.62–28.84] p = 0.01; and study day 2: 4.90 [1.28–18.73] p = 0.02) after adjusting for VD/VT, PaO2/FiO2, oxygenation index, vasopressor use and the primary risk for ARDS. Using a Cox proportional hazard model, VD/VT was associated with a trend towards higher mortality (HR = 4.37 [CI: 0.99 – 19.32]; p = 0.052) that became significant when the analysis was adjusted for daily oxygenation index (HR = 1.74 [95% CI: 1.12 – 3.35] p = 0.04).
Conclusions
Markedly elevated VD/VT (≥ 0.60) in early ARDS is associated with higher mortality. Measuring VD/VT may be useful in identifying ARDS patients at increased risk of death who are enrolled into a therapeutic trial.
Keywords: Acute lung injury, acute respiratory distress syndrome, mechanical ventilation, physiologic dead-space fraction, single-breath test for carbon dioxide
INTRODUCTION
Physiologic dead-space fraction (VD/VT) is the portion of tidal volume that does not participate in gas exchange and therefore consists of expired gas without carbon dioxide. Historically, elevated VD/VT in patients with ARDS was thought to be a late-occurring phenomenon associated with the fibroproliferative stage of injury.1 However, recent evidence indicates that VD/VT is markedly elevated within 24 h of ARDS onset and is significantly elevated in non-survivors.2–8 Moreover, sustained elevation of VD/VT in ARDS has been associated with higher mortality.5,6
A pulmonary-specific physiologic variable such as VD/VT, that is strongly associated with mortality, could be useful in assessing the efficacy of new therapies for ARDS in prospective clinical trials. Prior studies examining the prognostic value of VD/VT have had limitations that prevent the generalizability of their results to patients eligible for therapeutic clinical trials, including the fact that patients were studied at only one or two hospitals.2–8 Older studies2,6 in which patients were managed with traditional higher VT ventilation, did not always include patients with less severe oxygenation defects (i.e. these studies focused only on patients with moderate or severe ARDS by the current Berlin Definition),9 and included patients who had risk factors for mortality that would have excluded them from enrollment in a therapeutic clinical trial.
More recent, small, prospective studies3–5,10 enrolled patients spanning the spectrum of ARDS from mild to severe, who were managed with lung-protective ventilation. In these studies, early elevation in VD/VT was associated with increased mortality. However, the results of these studies differed in whether abnormalities in VD/VT differentiated patients with mild versus severe oxygenation defects. In one study,10 elevated VD/VT alone did not predict mortality unless it was associated with elevated plasma markers for endothelial damage.
To our knowledge, only one study has incorporated VD/VT into a therapeutic clinical trial to assess mortality risk. In a phase II randomized controlled, multi-centered study of 75 patients with ARDS,11 VD/VT was used to assess the physiologic effects of recombinant activated protein C on pulmonary function. In that trial, which managed patients with the ARDS Network lung-protective ventilation protocol, 12 there was a significant decline in VD/VT among patients who received recombinant activated protein C.11 However, mortality was exceptionally low (13%), and the association between VD/VT and mortality was not addressed specifically.
The current study was designed to determine whether VD/VT in patients with ARDS (PaO2/FiO2 ≤ 300 mm Hg)9 is associated with mortality in the context of a large clinical trial using lung-protective ventilation. We prospectively studied patients enrolled into a multi-center, phase III, randomized-controlled trial of the National Heart, Lung and Blood Institutes’ ARDS Network.13 Our primary objective was to determine whether elevated VD/VT early in the clinical course was associated with mortality.
METHODS
Patients 18 years or older were co-enrolled into this observational sub-study of VD/VT within 48h of meeting the American-European Consensus Conference criteria for acute lung injury or ARDS.14 Specific inclusion and exclusion criteria have been previously published.13 To qualify for the study, patients had to meet all 3 American-European Consensus Conference Criteria (PaO2/FiO2 < 300, bilateral infiltrates on chest radiograph during invasive mechanical ventilation, and the absence of evidence of elevated left atrial pressures) within the same 24 h period. In addition, enrollment, randomization and initial protocol-directed therapies had to be initiated with 48h of meeting acute lung injury or ARDS criteria. Of the 22 specific exclusion criteria, those most relevant to the dead-space sub-study were severe chronic respiratory disease which was defined as chronic hypercapnia with PaCO2 > 45 mmHg, chronic hypoxemia with PaO2 < 55 mm Hg on room air, secondary polycythemia, severe pulmonary hypertension with mean PAP > 40 mm Hg, or ventilator-dependency; diffuse alveolar hemorrhage from vasculitis, severe morbid obesity, and moribund condition (i.e. not expected to survive 24 h). A complete list of criteria can be found online at http://www.clinicaltrials.gov/ct2/show/NCT00434993.13
Patients were enrolled between August 6, 2006 and July 7, 2008 at 24 hospitals of the National Heart, Lung, and Blood Institute ARDS Network (Appendix). The VD/VT sub-study was approved by the data safety monitoring board for the parent clinical trial,13 as well as by the institutional review board of each participating hospital. Written informed consent was obtained from patients or their surrogates at the time of enrollment into the clinical treatment trial.
Measurements
Measurements of VD/VT were performed within 4h of enrollment and repeated daily on study days 1 and 2 if arterial blood gas measurements were indicated for clinical management. An automated volumetric capnography monitor was used (NICO™, Respironics/Philips Healthcare, Wallingford, CT) that had been previously validated in patients with ARDS.15 Mean expired carbon dioxide measurements with the NICO monitor coincided with arterial blood gas procurement and a ventilator systems check.
Assessments were made only when patients were managed with a ventilator mode providing full support (i.e.: volume, pressure or dual-mode assist/control ventilation), so that inspiratory time and VT were likely to be relatively stable, and measurements of respiratory system compliance could be made. Patients were studied in the semi-recumbent position, in the absence of nursing care activities and when they were observed to be calm and synchronous with the ventilator.
In addition to VD/VT, the mean expired carbon dioxide partial pressure, volume of carbon dioxide excretion per minute and expired VT was recorded from the NICO monitor. We also recorded arterial blood gas values and standard ventilator data such as ventilator mode, plateau pressure, positive end-expiratory pressure, mean airway pressure, inspired oxygen fraction, and total respiratory frequency.
VD/VT was calculated by the monitor using the Enghoff modification of the Bohr equation as the difference between arterial and mean expired carbon dioxide partial pressure divided by the arterial carbon dioxide partial pressure:16 VD/VT = [PaCO2 - PeCO2] ÷ PaCO2. Minute ventilation was calculated as the product of expired VT and total respiratory rate. Respiratory system compliance was calculated as VT divided by the end-inspiratory plateau pressure minus positive end-expiratory pressure. Oxygenation Index (OI) was calculated as the product of mean airway pressure and the percent of inspired oxygen divided by the partial pressure of arterial oxygen.17
Each participating site received formal training on the use of the NICO monitor provided by clinical research specialists from Respironics/Philips Healthcare. The training material and presentation was designed by Respironics/Philips Healthcare and ARDS Network investigators, and was based on the same training program developed for a previous multi-centered clinical trial.11
Because numerous clinicians across multiple research centers were making measurements of VD/VT, two simple quality control measures were used to verify data prior to the analysis. The first was to confirm that dead space measurements were made on a full support mode of ventilation. Second, to lessen the possibility of inadvertent transcription error, the recorded VD/VT was verified by independent calculation using the Enghoff-Bohr equation and the corresponding recorded values for PaCO2 and PeCO2. Although recording errors could have occurred in either direction, a pre hoc decision was made that both calculations had to be in agreement in order for data to be included in the analysis.
Death prior to hospital discharge (or hospital Day 90) was the primary outcome variable in this study. Patients were followed until death or discharge from the hospital.
Statistical Analysis
Continuous variables were expressed as mean ± standard deviation or median with interquartile range, and were compared using Student t-test or the Wilcoxon rank sum test, where appropriate. Categorical variables were reported as percentages and compared using chi-square tests or Fisher exact tests where appropriate. Multivariate logistic regression models were used to test the association of VD/VT with mortality. A pre hoc decision was made to adjust the analyses for ARDS etiology, OI, ratio of arterial oxygen tension-to-inspired oxygen fraction (PaO2/FiO2), and for the presence of shock (defined as the use of vasopressors except for dopamine at a dose of < 5 mcg/kg/minute) as a measure of severity of illness. Although the acute physiology and chronic health evaluation (APACHE) III score was calculated, it was not used in the modeling for practical reasons as the score is not available in clinical practice; whereas information regarding vasopressor use is and is associated with higher mortality.18 However, the primary etiology causing ARDS was categorized as pneumonia, sepsis, aspiration, trauma and other, and then entered into the model as dummy variables. The etiology of ARDS was determined by study investigators through review of the medical record and recorded for all study subjects. The odds ratio for death was calculated per 0.10 increases in VD/VT.
Two additional tests were done to assess the potential impact of VD/VT on mortality over time. First, analysis of covariance was used to assess differences in VD/VT between non-survivors vs. survivors at day 2, adjusting for baseline VD/VT. Second, Cox proportional-hazards models were used to test the association between VD/VT and mortality in the subgroup of patients who had complete data over the first 3 days. For this purpose, we constructed 3 models. Model 1 was unadjusted and only included VD/VT measured on a daily basis over the first 3 days as a time-varying covariate. Model 2 included daily VD/VT and baseline OI as the covariates. Model 3 included daily VD/VT and daily OI as time-varying covariates. We selected OI as a covariate in these models because of prior studies showing a strong association with mortality.19
All results were considered to be statistically significant at two-tailed p < 0.05. Stata 12.0 (Stata Corp, College Station, Texas) computer software was used for statistical analysis.
RESULTS
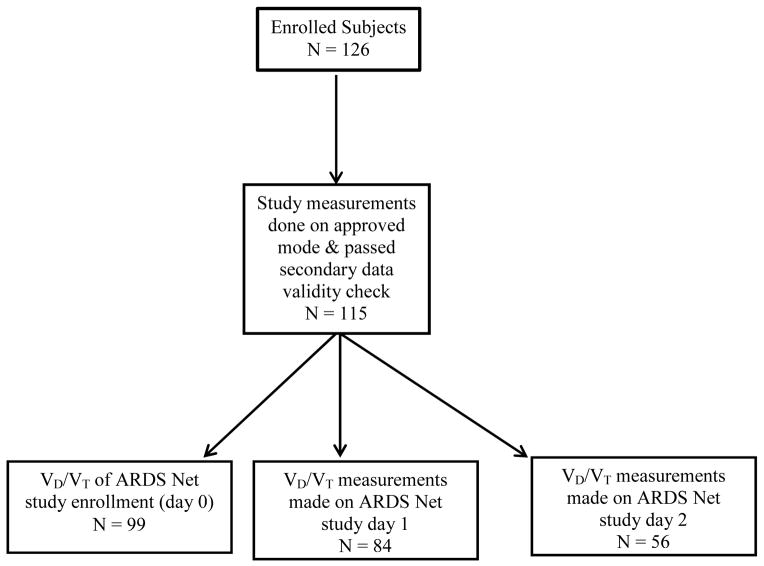
When the primary clinical trial was stopped, a total of 354 dead space measurements had been made in 126 patients. The quality control assessment revealed that 308 measurements (87%) in 115 patients (90%) were done on an approved full-support mode of ventilation, and also passed the secondary data-validity check. For these 115 patients the 60-day mortality was 19%. Sixteen patients did not have baseline measurements made on the day of study enrollment. Therefore 99 subjects had dead-space measurements made at baseline. On study day 1 dead-space measurements were made in 84 patients and in 56 patients on study day 2 (Figure 1). The primary etiology for lung injury was pneumonia followed by sepsis, aspiration, and trauma. Non-survivors were older age and at baseline had both significantly higher APACHE III scores as well as higher vasopressor use (Table 1). Over the duration of the study pulmonary gas exchange dysfunction was characterized by elevated VD/VT and diminished PaO2/FiO2; as well as markedly decreased respiratory system compliance (Table 2).
FIG 1.
Enrollment and dead-space measurements
Table 1.
Patient Characteristics (N= 115).
| Demographics | Survivors N = 93 |
Non-Survivors N = 22 |
|
|---|---|---|---|
| Age | 50 ± 16 | 47 ± 16 | 55 ± 14* |
| Female Gender | 47% | 49% | 36% |
| Caucasian | 63% | 65% | 59% |
| African-American | 21% | 17% | 36% |
| Hispanic | 8% | 10% | - |
| Asian | 4% | 5% | - |
| Native American | 1% | - | 5% |
| Primary ARDS Etiology | |||
| Pneumonia | 41% | 44% | 27% |
| Sepsis | 25% | 23% | 36% |
| Aspiration | 17% | 16% | 18% |
| Trauma | 9% | 9% | 9% |
| Other | 9% | 9% | 9% |
| Lung Injury Score | 2.71 ±0.48 | 2.73 ± 0.47 | 2.61 ± 0.50 |
| APACHE III | 91.8 ± 27.7 | 87.4 ± 25.4 | 111.9 ± 29.2†* |
| Vasopressors | 39% | 33% | 64%‡ |
Key: APACHE = acute physiology and chronic health evaluation score, - = no data;
p = 0.01;
p = 0.0002;
p = 0.009
Table 2.
Pulmonary dead-space fraction and other respiratory variables.
| Day 0 | Day 1 | Day 2 | |
|---|---|---|---|
| N | 99 | 84 | 56 |
| VD/VT | 0.57 ± 0.11 | 0.57 ± 0.11 | 0.58 ± 0.12 |
| V̇CO2 (mL/min) | 207 ± 66 | 202 ± 62 | 198 ± 51 |
| V̇E (L/min) | 11.1 ± 4.4 | 10.3 ± 3.2 | 10.6 ± 2.8 |
| pH | 7.36 ± 0.08 | 7.37 ± 0.09 | 7.39 ± 0.09 |
| PaCO2 (mmHg) | 40 ± 8 | 40 ± 8 | 41 ± 9 |
| PaO2 (mmHg) | 87 ± 33 | 88 ± 27 | 79 ± 17 |
| PaO2 /FiO2 | 166 ± 66 | 188 ± 68 | 187 ± 73 |
| FiO2 | 0.59 ± 0.19 | 0.49 ± 0.14 | 0.48 ± 0.14 |
| OI | 11.8 ± 7.9 | 8.8 ± 5.4 | 10.0 ± 6.5 |
| VT (mL) | 417 ± 119 | 381 ± 85 | 383 ± 88 |
| f | 27 ± 7 | 28 ± 7 | 28 ± 7 |
| Pplat (cmH2O) | 24 ± 6 | 22 ± 6 | 23 ± 6 |
| PEEP (cmH2O) | 9.7 ± 3.4 | 8.5 ± 3.0 | 8.5 ± 3.0 |
| P̄aw (cmH2O) | 16 ± 3 | 15 ± 5 | 15 ± 4 |
| Crs (mL/cmH2O) | 26 ± 8 | 26 ± 11 | 27 ± 11 |
Key: Crs = respiratory system compliance, FiO2 = inspired oxygen fraction, f = total respiratory frequency, N = number of patients, OI = oxygenation index, PaO2/FiO2 = ratio of arterial oxygen partial pressure to inspired oxygen fraction, PaCO2 = arterial carbon dioxide partial pressure, PaO2 = arterial oxygen partial pressure, P̄aw= mean airway pressure, PEEP = positive end-expiratory pressure, Pplat = end-inspiratory plateau pressure, V̇CO2 = volume of carbon dioxide excretion per minute, VD/VT = physiologic dead-space fraction, V̇E = minute ventilation.
When analyzed by outcome, there was a trend towards higher baseline VD/VT in non-survivors compared to survivors (0.62 ± 0.11 vs. 0.56 ± 0.11 respectively, p = 0.08). However, VD/VT was significantly higher among non-survivors on study day 1 (0.64 ± 0.12 vs. 0.55 ± 0.11 respectively, p = 0.01) and day 2 (0.67 ± 0.12 vs. 0.56 ± 0.11 respectively, p = 0.004) (Figure 2). Likewise, the odds ratio for death in the unadjusted logistic regression model approached statistical significance on the day of study enrollment (OR = 1.59 [95% CI: 0.94 – 2.72] for every 0.10 increase in VD/VT; p = 0.08); thereafter the association between VD/VT and mortality was stronger; becoming statistically significant on study days 1 (OR = 1.94 [95% CI: 1.16 – 3.27]; p = 0.01) and day 2 (OR = 2.50 [95% CI: 1.26 – 4.97]; p = 0.009) (Table 3).
FIG 2.
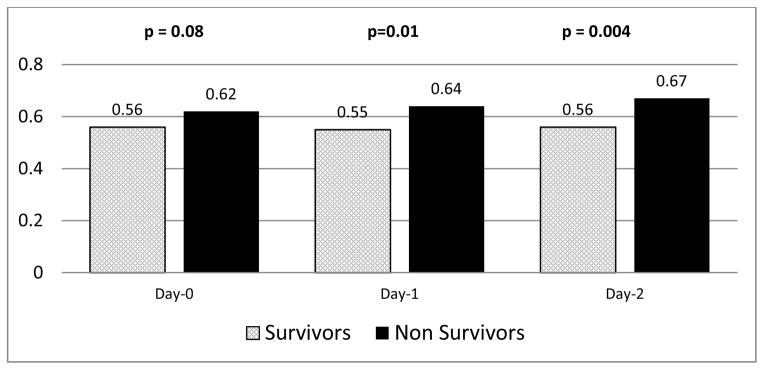
Dead-space fraction and outcome by study day.
Table 3.
Mortality as a function of dead-space fraction by unadjusted and adjusted analyses
| Day 0 | Day 1 | Day 2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | OR | 95% CI | p | |
| Unadjusted model | |||||||||
| VD/VT | 1.59 | 0.94 – 2.72 | 0.08 | 1.94 | 1.16 – 3.27 | 0.01 | 2.50 | 1.26 – 4.97 | 0.009 |
| Adjusted model | |||||||||
| VD/VT | 1.73 | 0.82 –3.63 | 0.15 | 6.84 | 1.62 – 28.84 | 0.01 | 4.90 | 1.28 – 18.73 | 0.02 |
| PaO2/FiO2 | 1.02 | 1.00 – 1.04 | 0.03 | 1.02 | 0.99 – 1.04 | 0.15 | 1.01 | 0.99 – 1.03 | 0.45 |
| OI | 1.10 | 0.98 – 1.24 | 0.09 | 0.95 | 0.67 – 1.35 | 0.79 | 1.06 | 0.81 – 1.38 | 0.66 |
| Vasopressor | 6.71 | 1.44 – 31.14 | 0.02 | 3.46 | 0.36 – 33.05 | 0.28 | 4.66 | 0.53 – 40.80 | 0.16 |
Key: CI = confidence interval, OI = oxygenation index; OR = odds ratio, PaO2/FiO2 = arterial oxygen tension-to-inspired oxygen fraction ratio; VD/VT = dead-space fraction
OR per 0.1 increase in VD/VT. The OR is reported per unit change for both PaO2/FiO2 and OI
Adjusting the analysis for ARDS etiology, PaO2/FiO2, OI, and baseline vasopressor use produced a modest increase in the baseline OR for VD/VT: 1.73 [0.82 – 3.63 p = 0.09]. However, the strength of association between VD/VT and mortality in the adjusted model increased markedly on study day 1 (OR=6.84 [1.62 – 28.84]; p=0.01) and study day 2 (OR = 4.90 [1.28 – 18.73 (p = 0.02), (Table 3). In contrast, only baseline PaO2/FiO2 and vasopressor use was significantly associated with mortality in the adjusted model.
Next, we used analysis of covariance to test whether differences in VD/VT between non-survivors and survivors at day 2 remained significant after controlling for baseline VD/VT. Indeed, day 2 VD/VT remained significantly associated with mortality in this model, p = 0.03. In an alternate analysis, we used Cox proportional hazard modeling with VD/VT as a time-varying covariate, VD/VT was associated with a trend towards higher mortality (HR =4.37 [CI: 0.99 – 19.32]; p = 0.052) per 0.10 VD/VT increase. This difference became significant when the analysis was adjusted for daily OI (HR = 5.69 [95% CI: 1.13 – 28.62] p = 0.04). The HR of mortality for VD/VT after adjusting for baseline OI was 4.28 (95% CI: 0.86 – 21.39; P=0.08).
Finally, since this study was done within a larger randomized, placebo-controlled clinical trial assessing the efficacy of aerosolized albuterol,13 analysis of covariance was used to assess the potential influence of albuterol on VD/VT at day 2, controlling for baseline level. Aerosolized albuterol therapy did not affect VD/VT (p = 0.84).
DISCUSSION
The primary objective of this study was to assess whether VD/VT was associated with mortality in patients with ARDS enrolled into a prospective clinical trial, and whether subsequent measurements were equally useful compared to those made at study entry. On the day of study enrollment there was a trend towards higher VD/VT in non-survivors. On both study days 1 and 2, VD/VT was significantly higher in non-survivors. These results suggest the possibility that VD/VT measured on the first few days following enrollment might be an even better tool for assessing mortality risk. Of note, the association between VD/VT and mortality was independent of the degree of oxygenation impairment, a finding that is consistent with other studies.2,5 Moreover, the adjusted analyses demonstrated that, in contrast to measures of oxygenation, the association between VD/VT and mortality was stronger and remained significant over the first 3 study days.
The difference in VD/VT between non-survivors and survivors of ARDS in this study is similar to that reported by several other investigators. In three prior studies,4–6 the average VD/VT on study enrollment was 0.61 to 0.62 in non-survivors and 0.53 to 0.54 in survivors. In another study3 of patients with mild ARDS, the difference was 0.55 and 0.48 for non-survivors and survivors respectively. Among studies that made repeated measurements over several days, the gap in VD/VT between non-survivors and survivors was sustained or increased.3,5,6 In these studies, the initial difference in VD/VT between non-survivors and survivors was 0.06 to 0.08, and increased to 0.1 or greater over the disease course.3,5,6 These previous findings are similar to our results in which the initial difference in mean VD/VT between non-survivors and survivors was 0.06 and subsequently increased to 0.09 – 0.11. A plausible explanation for the consistent results across studies is that pathophysiologic changes in ARDS (as manifested by VD/VT) may be more severe in non-survivors and appear to progress, whereas among survivors the pathophysiologic changes are less severe and/or self-limiting.
In ARDS, PEEP has a variable effect upon VD/VT: alveolar recruitment decreases dead-space while alveolar over-distension increases it.20 It is difficult to predict the impact of PEEP because both phenomena can occur simultaneously. In our study, PEEP and FiO2 were adjusted according to the ARDS Network low VT protocol based upon a target PaO2 range of 55–80 mmHg, rather than optimizing either pulmonary oxygenation or pulmonary mechanics. Therefore, it is uncertain how protocol-directed changes in PEEP may have influenced VD/VT, particularly in patients whose pulmonary function was deteriorating. However, measurements obtained during the first three days of study showed no difference between non-survivors and survivors in PEEP, VT or plateau pressure (surrogates of potential pulmonary over-distension). These findings suggest that there was no systematic difference in how these variables were adjusted between non-survivors and survivors that may have influenced dead space measurements.
The major limitation of this study was that a sufficient number of patients could not be enrolled to adequately test whether the association between VD/VT and mortality was different depending on the initial severity of hypoxemia (ie. in subgroups as per the Berlin definition according to a PaO2/FiO2 ratio < 100 mmHg, 100–200 mmHg, or > 200 mmHg).9 Another potential limitation stems from the fact that daily measurements occurred only in subjects who had arterial blood gas analysis ordered for clinical management. Therefore, a potential bias is that our study sample may have represented more patients, who by clinical presentation may have been judged to be deteriorating by clinicians caring for them, or at least more tenuous than those who did not have arterial blood gas measurements. Regardless these would encompass the very patients in whom the predictive potential of dead-space measurements would be most useful.
Another relevant issue has been the search for a readily available surrogate of VD/VT that eliminates the need for expired gas monitoring. This has been particularly important to those involved with population-based outcome studies of ARDS. Interest in the relationship of CO2 excretion to mortality is stymied by the fact that dead-space measurements are not yet standard clinical practice. For example, the ARDS Definition Task Force9 attempted to use corrected minute ventilation (i.e. [PaCO2 x minute ventilation] / 40) 21 as a potential surrogate for dead-space in defining those with severe lung injury. Yet this surrogate was not used in the final definition because of a “lack of evidence for predictive validity”.9
Others have reported that estimated VD/VT (by calculating carbon dioxide production from the Harris-Benedict equation, in conjunction with a modified alveolar air equation in order to derive mean PeCO2) was useful for predicting mortality in ARDS.22 This encouraging result seemingly obviates direct measurement of expired CO2 in clinical practice. However, these findings should be interpreted with caution because of issues concerning validation methodology23,24 In addition, there is clinical evidence that this method significantly underestimates actual dead-space; therefore it may not be an ideally suited tool for evaluating the true impact of impaired CO2 excretion on outcomes in ARDS.25
The uncertainty surrounding estimated versus measured VD/VT are based in part upon findings that equations used to predict metabolism agree poorly with measured energy expenditure in critically-ill, mechanically-ventilated patients.26 In addition, the measured volume of CO2 excreted by the lungs (which determines mean PeCO2) is unlikely to reflect CO2 production in the presence of severe ventilation:perfusion mismatching, intrapulmonary shunting and shock.27 This disparity between production and excretion during critical illness reflects the body’s considerably capacity to store CO2 (estimated to reach 20 L, or 11.6 mL/kg per 1 mmHg change in PaCO2); the dynamics of which are partly determined by muscle perfusion.28,29 In fact, even under normal physiologic conditions a “true” CO2 steady state is considered rare.29 Given these uncertainties, and until better methods of accurately estimating PeCO2 have been firmly established, VD/VT should be determined in patients with ARDS using direct measurements of expired CO2.
In summary, the results of this study demonstrate the practicality and utility of measuring VD/VT in patients with ARDS enrolled into a clinical trial. In addition, this relatively large multi-center observational study confirms the results of previous smaller, single-center studies,2–6 specifically that early and sustained elevations in VD/VT are associated with higher mortality in patients with ARDS. Therefore, measurement of VD/VT appears to provide important information that may be useful in therapeutic clinical trials.
Acknowledgments
Supported by: National Heart, Lung and Blood Institute contracts NO1-HR-56165-56713. Philips/Respironics provided material support (the loan of monitors, disposables and training) for this study. RH Kallet, MA Matthay have received similar past support from Philips/Respironics for other clinical trials.
This study was funded through the National Heart, Lung, and Blood Institute contracts NO1-HR-56165 – 56713. We thank Philips/Respironics for providing NICO capnography monitors, supplies and training. We would particularly like to thank Ivan Bustamante RRT and James Bement RRT for their extraordinary efforts in providing training to both Network personnel and staff at participating hospitals. We are indebted to intensive care unit personnel, especially respiratory therapists and nurses, and to our patients and their families, who supported this trial.
Network Participants
Baystate Medical Center- J. Steingrub*, M. Tidswell, L. DeSouza, C. Kardos, L. Kozikowski, K. Kozikowski,; Johns Hopkins Hospital- R. Brower*, H. Fessler, D. Hager, P. Mendez-Tellez, K. Oakjones, D Needham; Johns Hopkins Bayview Medical Center- J. Sevransky, A. Workneh, S. Han, S. Murray; University of Maryland- C. Shanholtz, G. Netzer, P. Rock, A. Sampaio, J. Titus, T Harrington; Washington Hospital Center-D. Herr, B. Lee, N. Bolouri, GR Khorjekar; Cleveland Clinic Foundation- H.P. Wiedemann*, R.W. Ashton, D.A. Culver, T. Frederick, J.J. Komara, J.A. Guzman, A.J. Reddy; University Hospitals of Cleveland- R. Hejal, M. Andrews, D. Haney; MetroHealth Medical Center- A.F. Connors, S. Lasalvia, J. D. Thornton, E.L. Warren; University of Colorado Health Science Centers- M. Moss*, A. Benson, E. Burnham, B. Clark, L. Gray, C. Higgins, B J. Maloney, M. Mealer; Denver Health Medical Center- I. Douglas, K. Overdier, K. Thompson, R. Wolken; University of North Carolina- S. Carson, L. Chang, J. Lanier; Wake Forest University- R.D. Hite*, P.E. Morris, A. Howard, A. Harvey, K. Bender; Moses Cone Memorial Hospital- P. Wright, C Carter-Cole, S. Gross, J. McLean, A. Overton; University of Virginia- J. Truwit, K. Enfield, M. Marshall, CG Irvin; LDS Hospital- T. Clemmer, L. Weaver, J Gleed,; Cottonwood Hospital-M. Zenger, J. Krueger Intermountain Medical Center- A. Morris*, A. Ahmed, A. Austin, N. Dean, C. Grissom, E. Hirshberg, N. Kumar, R. Miller, L. Napoli J. Orme, S. Pandita, G. Schreiber, L. Struck, F. Thomas, G. Thomsen,; McKay-Dee Hospital- C. Lawton, F. Leung, P. Kim, T. Fujii, J. Baughman, B. Kerwin, D. Hanselman, J d’Hulst; Utah Valley Regional Medical Center- K. Sundar, W. Alward, T. Hill, E. Campbell, K. Ludwig, D. Nielsen, M. Pearce; University of California, San Francisco- M.A. Matthay*, C. Calfee, B. Daniel, M. Eisner, O. Garcia, E. Johnson, K. Kordesch, K. Liu, H. Zhou; University of California, San Francisco, Fresno- M. W. Peterson, J. Blaauw; University of California Davis- T. Albertson, E. Vlastelin; San Francisco General Hospital- J. Diaz, E. Johnson, RH. Kallet; Mayo Foundation- R. Hubmayr*, D. Brown, O. Gajic, R. Hinds, S. Holets, DJ Kor, M. Passe; Louisiana State University- B. deBoisblanc*, P. Lauto, C. Romaine, G. Meyaski, J. Hunt, A. Marr; Louisiana State University- Earl K. Long, Baton Rouge General Medical Center Mid- City and Baton Rouge General Medical Center Bluebonnet- S. Brierre, C. LeBlanc, T Jagneaux,; Alton-Ochsner Clinic Foundation- D. Taylor; S. Jain, L. Seoane; Tulane University- F. Simeone, J. Fearon, J. Duchesne; Clinical Coordinating Center (Massachusetts General Hospital and Harvard Medical School): D. Schoenfeld*, M. Aquino, D. Dorer, M. Guha, E. Hammond, N. Lavery, P. Lazar, I. Molina, R. Morse, C. Oldmixon, B. Rawal, N. Ringwood, A. Shui, E. Smoot, B. T. Thompson; National Heart, Lung and Blood Institute: A. Harabin, S. Bredow, M. Waclawiw, G. Weinmann; Data and Safety Monitoring Board: R. G. Spragg (chair), A. Slutsky, M. Levy, B. Markovitz, E. Petkova, C. Weijer, and Douglas Willson; Protocol Review Committee: J. Sznajder (chair), M. Begg, E. Israel, J. Lewis, P. Parsons
Footnotes
denotes site principal investigator
References
- 1.Luce JM. Acute lung injury and the acute respiratory distress syndrome. Crit Care Med. 1998;26(2):369–376. doi: 10.1097/00003246-199802000-00043. [DOI] [PubMed] [Google Scholar]
- 2.Nuckton T, Alonso J, Kallet R, Daniel B, Pittet JP, Eisner M, Matthay MA. Early elevation in dead-space ventilation is associated with mortality risk in patients with acute respiratory distress syndrome. N Engl J Med. 2002;346(17):1281–1286. doi: 10.1056/NEJMoa012835. [DOI] [PubMed] [Google Scholar]
- 3.Lucangelo U, Bernabe F, Vatua S, Degrassi G, Villagra A, Fernandez R, Romero PV, Saura P, Borelli M, Blanch L. Prognostic value of different dead space indices in mechanically ventilated patients with acute lung injury. Chest. 2008;133(1):62–71. doi: 10.1378/chest.07-0935. [DOI] [PubMed] [Google Scholar]
- 4.Cepkova M, Kapur V, Ren X, Quinn T, Zhuo H, Foster E, et al. Pulmonary dead space fraction and pulmonary artery systolic pressure as early predictors of clinical outcome in acute lung injury. Chest. 2007;132(3):836–842. doi: 10.1378/chest.07-0409. [DOI] [PubMed] [Google Scholar]
- 5.Raurich JM, Vilar M, Colomar A, Ibanez J, Ayestaran I, Perez-Barcena J, Llompart-Pou JA. Prognostic value of the pulmonary dead-space fraction during early and intermediate phases of acute respiratory distress syndrome. Respir Care. 2010;55(3):282–287. [PubMed] [Google Scholar]
- 6.Kallet RH, Alonso JA, Pittet JP, Matthay MA. Prognostic value of the pulmonary dead-space fraction during the first six days of acute respiratory distress syndrome. Respir Care. 2004;49(9):1008–1014. [PubMed] [Google Scholar]
- 7.Guo F, Chen J, Liu S, Yang C, Yang Y. Dead-space fraction changes during positive end-expiratory pressure titration following lung recruitment in acute respiratory distress syndrome patients. Respir Care. 2012;57(10):1578–1585. doi: 10.4187/respcare.01497. [DOI] [PubMed] [Google Scholar]
- 8.Philips CR, Chesnutt MS, Smith SM. Extravascular lung water in sepsis-associated acute respiratory distress syndrome: Indexing with predicted body weight improves correlation with severity of illness and survival. Crit Care Med. 2008;36(1):69–73. doi: 10.1097/01.CCM.0000295314.01232.BE. [DOI] [PubMed] [Google Scholar]
- 9.The ARDS Definition Taskforce. Acute Respiratory Distress Syndrome: The Berlin Definition. JAMA. 2012;307(23):2526–2533. doi: 10.1001/jama.2012.5669. [DOI] [PubMed] [Google Scholar]
- 10.Ong T, McClintock DE, Kallet RH, Ware LB, Matthay MA, Liu KD. Ratio of angiopoietin-2 to angiopoeitin-1 as a predictor of mortality in acute lung injury patients. Crit Care Med. 2010;38(9):1–7. doi: 10.1097/CCM.0b013e3181eaa5bf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liu KD, Levitt J, Zhuo H, Kallet RH, Brady S, Steingrub J, et al. Randomized clinical trial of activated protein C for the treatment of acute lung injury. Am J Respir Crit Care Med. 2008;178(6):618–623. doi: 10.1164/rccm.200803-419OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NHLBI Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as a compared with traditional tidal volumes for acute respiratory distress syndrome. N Engl J Med. 2000;342(18):1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 13.Matthay MA, Brower RG, Carson S, Douglas IS, Eisner M, Hite D, et al. for the The National Heart, Lung, and Blood Institute ARDS Clinical Trials Network. Randomized, Placebo-Controlled Clinical Trial of an Aerosolized Beta-2 Agonist for Treatment of Acute Lung Injury. Am J Respir Crit Care Med. 2011;184(5):561–568. doi: 10.1164/rccm.201012-2090OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bernard GR, Artigas A, Brigham KL, Carlet J, Falke C, Hudson L, et al. Report of the American European Consensus Conference on Acute Respiratory distress syndrome: Definitions mechanisms, relevant outcomes, and clinical trials coordination. Am J Respir Crit Care. 1994;149(1):818–824. doi: 10.1164/ajrccm.149.3.7509706. [DOI] [PubMed] [Google Scholar]
- 15.Kallet RH, Daniel B, Garcia O, Matthay MA. Accuracy of physiologic dead space measurements in patients with acute respiratory distress syndrome using volumetric capnography: Comparison with the metabolic monitor method. Respir Care. 2005;50 (4):462–467. [PubMed] [Google Scholar]
- 16.Enghoff H. Volumen inefficax: Bemerkungen zur frage des schädlichen raumes. Upsala Lakareforen Forh. 1938;44:191–218. [Google Scholar]
- 17.Bone RC, Maunder R, Slotman G, Silverman H, Hyers TM, Kerstein MD, Ursprung JJ. An early test of survival in patients with the adult respiratory distress syndrome. The PaO2/FiO2 ratio and its differential response to conventional therapy. Prostaglandin E1 Study Group. Chest. 1989;96(4):849–851. doi: 10.1378/chest.96.4.849. [DOI] [PubMed] [Google Scholar]
- 18.Vieillard-Baron A, Girou E, Valente E, Brun_Buisson C, Jardin F, Lemaire F, Brochard L. Predictors of mortality in acute respiratory distress syndrome. Focus on the role of right heart catheterization. Am J Respir Crit Care Med. 2000;161(5):1597–1601. [PubMed] [Google Scholar]
- 19.Seeley E, McAuley DF, Eisner M, Miletin M, Matthay MA, Kallet RH. Predictors of mortality in acute lung injury during the era of lung protective ventilation. Thorax. 2008;63(11):994–998. doi: 10.1136/thx.2007.093658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Suter PM, Fairley HB, Isenberg MD. Optimum end-expiratory airway pressure in patients with acute pulmonary failure. N Engl J Med. 1975;292(6):284–289. doi: 10.1056/NEJM197502062920604. [DOI] [PubMed] [Google Scholar]
- 21.Wexler HR, Lok P. A simple formula for adjusting arterial carbon dioxide tension. Canad Anaesth Soc J. 1981;28(4):370–372. doi: 10.1007/BF03007805. [DOI] [PubMed] [Google Scholar]
- 22.Siddiki H, Kojicic M, Li G, Yilmaz M, Thompson TB, Hubmayr RD, Gajic O. Bedside quantification of dead-space fraction using routine clinical data in patients with acute lung injury: secondary analysis of two prospective trials. Crit Care. 2010;14(4):R141. doi: 10.1186/cc9206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chiumello D, Gallazzi E. Estimation of dead space fraction can be simplified in the acute respiratory distress syndrome. Crit Care. 2010;14(4):R195. doi: 10.1186/cc9237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Matthay MA, Kallet RH. Prognostic value of pulmonary dead-space fraction in patients with the acute respiratory distress syndrome. Crit Care. 2011;15(5):R185. doi: 10.1186/cc10346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Charron C, Repesse X, Bouferrache K, Bodson I, Castro S, Page B, et al. A PaCO2 and alveolar dead space are more relevant than PaO2/FiO2 in monitoring the respiratory response to prone position and acute respiratory distress syndrome: a physiologic study. Crit Care. 2011;15(5):R175. doi: 10.1186/cc10324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kross EK, Sena M, Schmidt K, Stapleton RD. A comparison of predictive equations of energy expenditure and measured energy expenditure in critically ill patients. J Crit Care. 2012;27(3):321, e5–12. doi: 10.1016/j.jcrc.2011.07.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bakker J, Vincent J-L, Gris P, Leon M, Coffernils M, Kahn RJ. Veno-arterial carbon dioxide gradient in human septic shock. Chest. 1992;101(2):509–515. doi: 10.1378/chest.101.2.509. [DOI] [PubMed] [Google Scholar]
- 28.Henneberg S, Soderberg D, Groth T, Stjernstrom H, Wiklund L. Carbon dioxide production during mechanical ventilation. Crit Care Med. 1987;15(1):8–13. doi: 10.1097/00003246-198701000-00002. [DOI] [PubMed] [Google Scholar]
- 29.Fahri LE, Rahn H. Dynamics of changes in carbon dioxide stores. Anesthesiology. 1960;21(6):604–613. doi: 10.1097/00000542-196011000-00004. [DOI] [PubMed] [Google Scholar]