Abstract
Background
The aim of this study was to investigate the clinical outcome and especially costs of hospitalisation for community-acquired pneumonia (CAP) in relation to microbial aetiology. This knowledge is indispensable to estimate cost-effectiveness of new strategies aiming to prevent and/or improve clinical outcome of CAP.
Methods
We performed our observational analysis in a cohort of 505 patients hospitalised with confirmed CAP between 2004 and 2010. Hospital administrative databases were extracted for all resource utilisation on a patient level. Resource items were grouped in seven categories: general ward nursing, nursing on ICU, clinical chemistry laboratory tests, microbiology exams, radiology exams, medication drugs, and other.linear regression analyses were conducted to identify variables predicting costs of hospitalisation for CAP.
Results
Streptococcus pneumoniae was the most identified causative pathogen (25%), followed by Coxiella burnetii (6%) and Haemophilus influenzae (5%). Overall median length of hospital stay was 8.5 days, in-hospital mortality rate was 4.8%.
Total median hospital costs per patient were €3,899 (IQR 2,911-5,684). General ward nursing costs represented the largest share (57%), followed by nursing on the intensive care unit (16%) and diagnostic microbiological tests (9%). In multivariate regression analysis, class IV-V Pneumonia Severity Index (indicative for severe disease), Staphylococcus aureus, or Streptococcus pneumonia as causative pathogen, were independent cost driving factors. Coxiella burnetii was a cost-limiting factor.
Conclusions
Median costs of hospitalisation for CAP are almost €4,000 per patient. Nursing costs are the main cause of these costs.. Apart from prevention, low-cost interventions aimed at reducing length of hospital stay therefore will most likely be cost-effective.
Keywords: Pneumonia, Bacterial infection, Health economist, Respiratory infection
Background
Community-acquired pneumonia (CAP) is one of the most common infectious diseases worldwide; in the developed world, CAP, combined with influenza, is the primary cause of death due to infection [1]. Incidence of CAP is high in young children, then decreases and in adults, again increases with age; consequently, CAP carries a high burden, in particular in the elderly [2,3]. As 20-40% of all CAP episodes in the elderly are treated in-hospital [4], hospital admissions for pneumonia result in considerable health care costs [2,5]. In 1997, these costs were estimated to be €115 million in Spain [6] and almost £400 million in the United Kingdom [7]. With the post Second World War generation approaching senescence and the rise of life expectancy in general, the number of hospital admissions for pneumonia and associated health care costs will continue to rise [8].
Many studies have been conducted to assess the effect of interventions with the aim of reducing the risk and improving the outcome of CAP. For instance, the introduction of vaccination against Influenza has reduced severity and mortality of secondary pneumonia [9], adjunctive therapies such as corticosteroids have been shown to reduce length of hospital stay [10] and some studies showed lowering of incidence and mortality of pneumococcal pneumonia in nursing home residents through use of pneumococcal vaccines [11] although others found no protective effect [12-14]. In order to determine overall cost-effectiveness of such interventions, knowledge of the association between microbial aetiology, outcomes, and costs of CAP is indispensable.
The objectives of the present study were to analyse microbial aetiology and clinical outcomes of a large cohort of patients hospitalised for CAP, to determine individual hospital resource utilization, to quantify total costs of hospitalisation for CAP and to explore possible associations between microbial aetiology and the corrsponding costs.
Methods
Patients
Patients with CAP above 18 years of age admitted to the St. Antonius Hospital in Nieuwegein or the Gelderse Vallei Hospital in Ede (both teaching hospitals in the Netherlands), between October 2004 and August 2006 (n = 201), and between November 2007 and September 2010 (n = 304), who participated in two consecutive clinical studies were enrolled. The first study was a prospective cohort study on clinical characteristics and polymorphisms in innate immunity genes in patients with CAP; the second study was a placebo controlled double blind randomized clinical trial evaluating dexamethasone as adjunctive therapy (NCT00471640). In both studies, the same clinical inclusion criteria were used and patient characteristics of the patients studied resembled data from another large CAP cohort (over 20,000 patients admitted to hospital for pneumonia) from the same time period [15]. CAP was defined as a new pulmonary infiltrate on chest radiograph, in combination with at least two of the following criteria: cough, sputum production, temperature above 38°C or below 35°C, auscultatory findings consistent with pneumonia, C-reactive protein concentration of more than 15 mg/L, and white blood cell count of above 10 × 109 cells/L or below 4 × 109 cells/L, or >10% of rods in leukocyte differentiation. Patients who were immunocompromised, had been directly admitted to the intensive care unit (ICU), or who had received immunosuppressive therapy (including the use of >20 mg prednisone equivalent per day for >3 days) were excluded. More detailed inclusion and exclusion criteria are described elsewhere [10,16]. Comorbidities were recorded of each patient and pneumonia severity index (PSI) score was calculated on admission. The present study has been approved by the Medical Ethical Committees of the St. Antonius Hospital (Nieuwegein) and the Gelderse Vallei Hospital (Ede), both in The Netherlands.
Microbial aetiology
At least two sets of separate blood and sputum samples of each patient were Gram stained and cultured. Streptococcus (S.) pneumoniae cultured from either sputum or blood was serotyped by the Quellung reaction. Moreover, sputum samples were analysed with TaqMan real-time polymerase chain reactions (PCRs) in order to detect DNA of Mycoplasma (M.) pneumoniae, Legionella (L.) pneumophila, Coxiella (C.) burnetii, and Chlamydophila species. Antigen testing of S. pneumoniae and L. pneumophila was performed in urine samples. Furthermore, pharyngeal swabs were taken for viral culture and viral PCR. Finally, patients were analysed for a serotype specific rise in S. pneumoniae antibodies when two blood samples (one drawn at admission and one after discharge) were available. Antibodies against pneumococcal polysaccharides were measured on a Luminex platform (Luminex Corporation, Austin, TX), using a quantitative multiplex immunoassay: the xMAP pneumococcal immunity panel. More detailed information can be found elsewhere [17].
If both a bacterium and virus were detected in a patient, the bacterial species was classified as the causative pathogen. If two different bacterial species were identified, the pathogen known to most likely cause CAP was considered causative. For the purpose of this study, aetiological agents were classified into ten groups: the first seven groups consist of the most frequently identified bacteria (S. pneumoniae, C. burnetii, Haemophilus (H.) influenzae, L. pneumophila, Chlamydophila species, M. pneumoniae, and Staphylococcus aureus), group eight contains remaining bacteria (‘Other pathogen’), group nine comprises viruses (‘Viral pathogen’), and the last group consists of CAPs with unidentified aetiology (‘No pathogen identified’).
Clinical outcomes
ICU admission during hospitalisation, length of stay, in-hospital mortality, 30-day and one-year mortality were documented for each patient.
Resource utilization and cost calculation
Hospital administrative databases were extracted for all resource utilisation on a patient level. Resource items were grouped in seven categories: general ward nursing, nursing on ICU, clinical chemistry laboratory tests, microbiology exams, radiology exams, medication drugs, and other. Except for nursing, only resources plausibly related to pneumonia treatment were selected. For example, medication drug use only included antibiotics, analgesics, bronchodilators, sedatives, blood products and antithrombotic drugs. The category “other” comprised physical therapy sessions, electro and echocardiograms, bronchoscopy and laryngoscopy and invasive empyema diagnostic and treatment procedures. For duration of nursing, the unit of measurement was number of days.
Total costs per patient were calculated by summing the number of resources multiplied by the costs per item. Costs per resource item were based on the National Diagnosis Treatment Combination rates valued in 2011 or 2012 [18], except for nursing costs during hospital stay and costs of medication drugs. Nursing costs for general ward and ICU stay were based on mean costs per hospital unit prices belonging to diagnostic treatment combination code 401 (‘pneumonia’) for the year 2011. Costs of drugs were based on the lowest medication drug price according to the College for Health Insurance website valued in 2012 [19]; if not available on this website, the hospital’s purchase price was recorded.
Data analyses
Overall, descriptives were stated as number (%), mean (standard deviation (SD)) or median (interquartile range (IQR)), and compared using independent samples T-test, Chi-square test, or Mann–Whitney U test, where appropriate. Kruskall Wallis test was used to assess overall differences in length of stay and costs between aetiologic groups.
To identify variables predicting costs of hospitalisation for CAP, linear regression analyses were conducted with log-transformed data. Costs were log-transformed to correct for skewness of the data. First, the following variables were examined in a univariate model (with reference group): male gender (female), chronic obstructive pulmonary disease (no chronic obstructive pulmonary disease), congestive heart failure (no congestive heart failure), diabetes mellitus (no diabetes mellitus), PSI classes IV-V (classes I-III), and admission in ‘Gelderse Vallei Hospital’ (St. Antonius Hospital). The ten aetiologic groups were included separately in the model; reference value per group was composed of the other nine aetiologic groups. Subsequently, variables significant in univariate models (p < 0.10) were inserted in a multivariate model, applying a backwards elimination technique retaining variables with a p-value < 0.10. For the final model, effects (costs) were stated as beta with corresponding standard error for each independent variable. Data were analysed with SPSS statistical software for Windows, version 21.0. For all analyses, a p-value of <0.05 was considered statistically significant.
Results
A total of 505 patients with CAP were subject in this study, with a mean age of 63.4 ± 18.0 years and a male/female ratio of 1.4/1. Patient characteristics are presented in Table 1.
Table 1.
Characteristics of 505 patients hospitalised with community-acquired pneumonia
| Characteristics | All patients ( n = 505) |
|---|---|
| Age in years (SD) |
63.4 (18.0) |
| Male sex (%) |
295 (58.4) |
| Comorbidities (%) |
|
| Chronic obstructive pulmonary disease |
98 (19.4) |
| Congestive heart failure |
68 (13.5) |
| Renal disease |
40 (7.9) |
| Diabetes mellitus |
77 (15.2) |
| Liver disease |
2 (0.4) |
| Pneumonia Severity Index class I-III (%) |
279 (55.2) |
| Pneumonia Severity Index class IV-V (%) |
226 (44.8) |
| Pathogens (%) |
|
|
Streptococcus pneumoniae |
124 (24.6) |
|
Coxiella burnetii |
28 (5.5) |
|
Haemophilus influenzae |
27 (5.3) |
|
Legionella pneumophila |
20 (4.0) |
|
Chlamydophila species |
16 (3.2) |
|
Mycoplasma pneumoniae |
9 (1.8) |
|
Staphylococcus aureus |
9 (1.8) |
| Only viral pathogen |
35 (6.9) |
| Other pathogen |
27 (5.3) |
| No pathogen identified |
210 (41.6) |
| Empirical antibiotic treatment (%) |
|
| Beta-lactam, penicillins (monotherapy) |
254 (50.3) |
| Other beta-lactam (monotherapy) |
86 (17.0) |
| Beta-lactam, penicillins + quinolone |
34 (6.7) |
| Beta-lactam, penicillins + macrolides |
33 (6.5) |
| Other beta-lactam + aminoglycoside |
20 (4.0) |
| Other beta-lactam + quinolone |
16 (3.2) |
| Quinolone (monotherapy) |
11 (2.2) |
| Macrolides, lincosamides and streptogramins (monotherapy) |
11 (2.2) |
| Beta-lactam, penicillin + aminoglycoside |
7 (1.4) |
| Other beta-lactam, penicillin + macrolides |
7 (1.4) |
| Sulfanomides and trimethoprim (monotherapy) |
6 (1.2) |
| Tetracyclines (monotherapy) |
6 (1.2) |
| Other |
14 (2.8) |
| Outcomes |
|
| Length of hospital stay (IQR) |
8.5 (6.0-13.0) |
| Intensive care unit admission (%) |
38 (7.5) |
| In-hospital mortality (%) |
24 (4.8) |
| 30-Day mortality (%) |
26 (5.1) |
| One-year mortality (%) | 73 (14.5) ⟂ |
Data are presented as number (%), mean (SD) or median (IQR).
Abbreviations: IQR interquartile range, SD standard deviation.
⟂7 patients were lost to follow-up.
Aetiology and clinical outcomes
In 294/505 (58.2%) patients, a causative pathogen was identified. Table 2 lists the microbiological test results of most frequently identified pathogens. Overall, S. pneumoniae was most prevalent (124/505, 24.6%). In 51 of these 124 patients, S. pneumoniae serotyping could be performed. Type 1 was the most common serotype. A complete overview of the pneumococcal serotypes is given in Additional file 1: Table S1. In 43/505 patients a mixed infection was found. No penicillin resistant S. pneumoniae, methycillin-resistant Staphylococcus aureus or multi-resistant gram-negative pathogens were identified.
Table 2.
Microbiology tests results of 505 patients hospitalised with community-acquired pneumonia
| Sputum culture | Sputum PCR | Blood culture | Blood PCR | Urinary antigen test | Serology | |
|---|---|---|---|---|---|---|
|
S. pneumoniae n = 124 |
46 |
- |
42 |
- |
78 |
1 |
|
Haemophilus influenzae n = 27 |
25 |
1 |
- |
- |
- |
1 |
|
Legionella pneumophila n = 20 |
1 |
3 |
- |
- |
15 |
6 |
|
Mycoplasma pneumoniae n = 9 |
- |
4 |
- |
- |
- |
7 |
|
Coxiella burnetii n = 28 |
1 |
12 |
2 |
12 |
- |
20 |
|
Chlamydophila spp. n = 16 |
- |
8 |
- |
- |
- |
12 |
|
Staphylococcus aureus n = 9 |
8 |
- |
1 |
- |
- |
- |
| Other pathogen n = 27 |
23 |
- |
5 |
- |
- |
- |
| Viral pathogen n = 35 | 3 | 2 | - | - | - | 19 |
Abbreviations: n number, S. pneumoniae Streptococcus pneumoniae, spp species.
Clinical outcomes categorized by aetiology group are listed in Table 3. Overall, LOS differed significantly between the major aetiological groups (p < 0.001). CAP caused by either M. pneumoniae or C. burnetii was associated with a significantly shorter LOS compared to the other aetiologic groups (p:0.007 and p < 0.001, respectively), while S. pneumoniae CAPs resulted in a significantly longer duration of hospital stay (p:0.03).
Table 3.
Clinical outcomes per pathogen of 505 patients hospitalised with community-acquired pneumonia
| Length of hospital stay (IQR) | ICU admission (%) | In-hospital mortality (%) | 30-day mortality (%) | One-year mortality (%) | |
|---|---|---|---|---|---|
|
Streptococcus pneumoniae (n = 124) |
8.5 (6.5-14.9) |
10 (8.1) |
4 (3.2) |
4 (3.2) |
12 (9.7) |
|
Coxiella burnetii (n = 28) |
5.5 (3.5-7.5) |
0 |
0 |
1 (3.6) |
1 (3.6) |
|
Haemophilus Influenzae (n = 27) |
9.0 (7.5-14.0) |
2 (7.4) |
0 |
0 |
3 (11.1) |
|
Legionella pneumophila (n = 20) |
11.0 (6.5-17.0) |
3 (15.0) |
1 (5.0) |
1 (5.0) |
2 (10.0) |
|
Chlamydophila species (n = 16) |
8.5 (6.6-13.3) |
2 (12.5) |
0 |
0 |
1 (6.3) |
|
Mycoplasma pneumoniae (n = 9) |
5.0 (4.5-7.3) |
0 |
0 |
0 |
0 |
|
Staphylococcus aureus (n = 9) |
10.5 (7.3-14.5) |
1 (11.1) |
3 (33.3) |
3 (33.3) |
4 (44.4) |
| Other pathogen (n = 27) |
8.0 (5.0-15.8) |
7 (25.9) |
2 (7.4) |
2 (7.4) |
9 (33.3) |
| Viral pathogen (n = 35) |
8.5 (6.3-13.5) |
1 (2.9) |
2 (5.7) |
3 (8.6) |
6 (17.1) |
| No pathogen found (n = 210) | 8.5 (5.5-12.6) | 12 (5.7) | 12 (5.7) | 12 (5.7) | 35 (16.7) |
Data are presented as number (%) or median (IQR). For calculation of median length of stay patients who died during admission where excluded from the analysis.
Abbreviations: ICU intensive care unit, IQR interquartile range, n number.
Hospital costs
For 361/505 (71.5%) of the patients complete resource utilization data were available for analysis. The clinical characteristics of the 144 patients who could not be included, as compared to the included patients can be found in Additional file 1: Table S2.
Total costs
Table 4 lists the top 10 most frequent and the top 10 most expensive resource items. In the Additional file 1, the top 5 most frequent used items for each individual category can be found in Table S3.Figure 1 shows the total distribution of hospital costs per patient. Total median hospital costs per patient were €3,899 (IQR 2,911-5,684) with minimum costs of €901 and maximum costs of €112,634. Figure 2 shows the share per category in the total costs: general ward nursing represented the largest share (56.5%), followed by nursing on ICU (16.4%) and diagnostic microbiology exams (9.4%).
Table 4.
Top 10 most frequent and top 10 most expensive resource items with prices in euro
| Resource | Mean frequency per patient | Price per item (in euro) | |
|---|---|---|---|
| |
10 Most frequent resource items |
|
|
|
1 |
Tissue obtainment (microbiology and clinical chemistry) |
18.1 |
13.73 |
|
2 |
Antibodies against any pathogen by using complement fixation test of haemagglutination inhibition essay |
10.4 |
4.84 |
|
3 |
General ward nursing (one day) |
9.4 |
375.00 |
|
4 |
Sodium |
8.2 |
1.76 |
|
5 |
Potassium |
8.2 |
1.76 |
|
6 |
Creatinine |
6.6 |
1.76 |
|
7 |
Glucose |
6.4 |
1.76 |
|
8 |
Leukocytes |
6.1 |
1.76 |
|
9 |
C-reactive protein |
6.0 |
4.84 |
|
10 |
Urea |
5.9 |
1.76 |
| |
10 Most expensive resource items |
|
|
|
1 |
Intensive care unit nursing (one day) |
0.6 |
1,730.00 |
|
2 |
Surgical treatment of thorax empyema |
0.2 |
1,084.75 |
|
3 |
Laryngoscopy |
0.0 |
999.00 |
|
4 |
Microbiological determination on isolated DNA/RNA |
0.0 |
867.61 |
|
5 |
General ward nursing (one day) |
9.4 |
375.00 |
|
6 |
Flexible bronchoscopy |
0.2 |
209.25 |
|
7 |
DNA/RNA amplification (qualitative) |
<0.1 |
208.60 |
|
8 |
Computer tomography of thorax |
0.2 |
195.83 |
|
9 |
Immunopathologic research |
<0.1 |
109.57 |
| 10 | Computer tomography airways | <0.1 | 160.01 |
Figure 1.
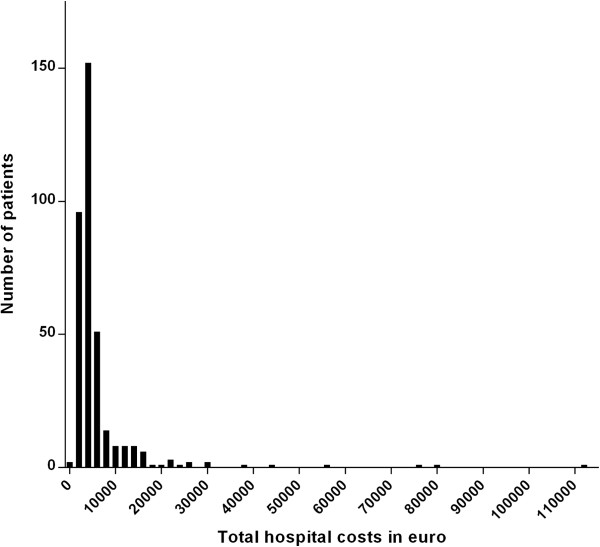
Distribution of total hospital costs in 361 patients hospitalised with community-acquired pneumonia.
Figure 2.
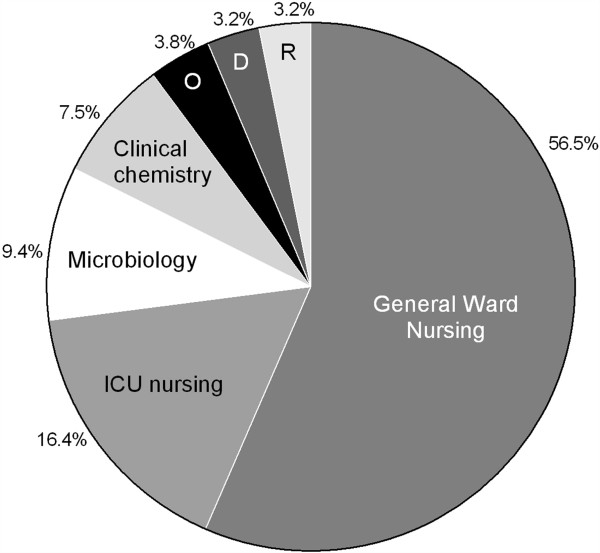
Distribution of costs of 361 patients hospitalised with community-acquired pneumonia expressed by their seven major resource categories. Legend: Abbreviations: D, drugs; ICU, intensive care unit nursing; O, other; R, radiology exams.
Costs categorized per aetiological group
Overall, total hospital costs differed between the 10 aetiological groups (p:0.002); costs for hospitalisation of CAP caused by C. burnetii were significantly lower (p < 0.001), while hospitalisation of patients with S. pneumoniae as causative agent represents significantly higher costs (p:0.03) compared to other aetiologies. For M. pneumoniae and Staphylococcus aureus a trend towards respectively lower and higher costs (p: 0.10 and p:0.08, respectively) was observed.
Figure 3 shows median costs of each aetiologic group subdivided into the seven resource categories. Raw numbers of this figure can be found in Additional file 1: Table S4. Overall, costs for general ward nursing, microbiology exams, clinical chemistry laboratory tests, medication drugs, and radiologic exams all differed between the aetiological groups. On an individual pathogen level, CAP caused by C. burnetii was lower in costs for nursing, clinical chemistry tests, and radiological examinations compared to most of the other aetiological groups. Costs of medication were specifically high in patients with L. pneumophila pneumonia. CAP caused by Staphylococcus aureus was higher in costs for nursing and CAP caused by S. pneumoniae was more expensive in radiological examinations. Additional file 1: Table S5A to S5G shows details of this aetiological subgroup analysis.
Figure 3.
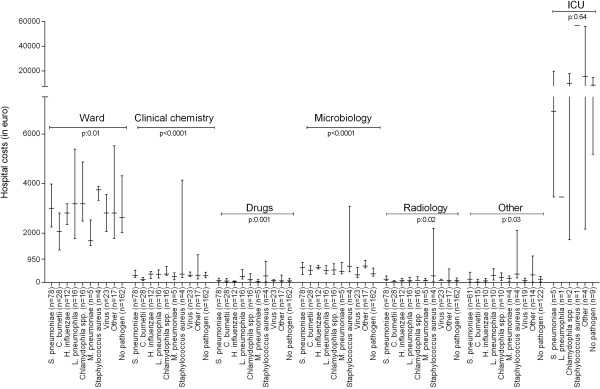
Median hospital costs in euro with interquartile range per aetiology differentiated by resource group. Legend: Abbreviations: C. burnetii, Coxiella burnetii; H. influenzae, Haemophilus influenzae; ICU, intensive care unit; L. pneumophila, Legionella pneumophila; M. pneumoniae, Mycoplasma pneumoniae; n, number; spp, species; S. pneumoniae, Streptococcus pneumoniae.
Costs per S. pneumoniae serotype
As S. pneumoniae is the most frequent identified pathogen in CAP, costs of serotypes were explored grouped per pneumococcal vaccine available in the European Union (results presented in Additional file 1: Table S6). Total costs of hospitalisation were not higher for patients with CAP caused by the serotypes present in the different vaccines compared to patients infected by pneumococcal serotypes not included in these vaccines.
Identification of cost driving factors
To identify cost driving factors, a multivariable linear regression model was constructed. Table 5 lists the variables included in the final model together with their corresponding regression coefficients. Staphylococcus aureus, high PSI score (classes IV and V), and Streptococcus pneumoniae were all independent cost driving factors, increasing total costs of hospitalisation by 98%, 43%, and 18% respectively. Coxiella burnetii decreased total costs of hospitalisation by 35%.
Table 5.
Multivariable linear regression model to predict total costs of hospitalisation in 361 patients with community-acquired pneumonia
| |
Crude analysis |
Multivariable analysis |
||||
|---|---|---|---|---|---|---|
| Independent variables | B | SE | p-value | B | SE | p-value |
| CONSTANT |
|
|
|
3.558 |
0.023 |
<0.001 |
| Male gender |
0.009 |
0.032 |
0.77 |
|
|
|
| Chronic obstructive pulmonary disease |
0.009 |
0.044 |
0.83 |
|
|
|
| Congestive heart failure |
0.083 |
0.045 |
0.06 |
|
|
|
| Chronic renal disease |
0.077 |
0.057 |
0.17 |
|
|
|
| Diabetes mellitus |
0.047 |
0.045 |
0.30 |
|
|
|
| Pneumonia Severity Index classes IV-V |
0.176 |
0.030 |
<0.001 |
0.158 |
0.030 |
<0.001 |
| Hospital ‘Gelderse Vallei’ |
−0.063 |
0.042 |
0.13 |
|
|
|
| Pathogens: |
|
|
|
|
|
|
|
Streptococcus pneumoniae |
0.070 |
0.038 |
0.07 |
0.067 |
0.036 |
0.07 |
|
Coxiella burnetii |
−0.198 |
0.058 |
0.001 |
−0.129 |
0.056 |
0.02 |
|
Haemophilus influenzae |
−0.047 |
0.087 |
0.59 |
|
|
|
|
Legionella pneumophila |
0.060 |
0.076 |
0.43 |
|
|
|
|
Chlamydophila species |
0.087 |
0.076 |
0.25 |
|
|
|
|
Mycoplasma pneumoniae |
−0.179 |
0.134 |
0.18 |
|
|
|
|
Staphylococcus aureus |
0.358 |
0.148 |
0.02 |
0.362 |
0.140 |
0.01 |
| Viral pathogen |
−0.046 |
0.064 |
0.48 |
|
|
|
| Other pathogen |
0.163 |
0.073 |
0.03 |
0.131 |
0.070 |
0.06 |
| No pathogen found | −0.034 | 0.031 | 0.28 | |||
Prices are log-transformed and stated in euro.
Abbreviations: B beta coefficient, SE standard error.
Bold numbers are included in the final model (p < 0.10).
Discussion
In the past years, many studies have been conducted aiming at finding new strategies to lower incidence and improve clinical outcomes of CAP. To determine cost-effectiveness of these strategies, knowledge about causing microorganisms, clinical outcomes, and related costs is needed. To our knowledge, this is the first study that studies the potential associations between costs of hospitalisation for CAP and its microbial aetiology. The main finding in the present study is that costs related to hospitalisation for CAP show great variation between patients, and CAP caused by S. pneumoniae and Staphylococcus aureus is associated with significantly higher costs, mainly due to longer duration of hospital stay.
In this study, S. pneumoniae was confirmed as the most prevalent causative pathogen in CAP (24.6%). Compared to other aetiological groups, median LOS (8.5 days), rate of ICU admission (8%), and one-year mortality (9.7%) were relatively higher for pneumonia caused by S. pneumoniae, despite the relative younger age of patients of this aetiological group (60.4 ± 19.0 years versus 64.4 ± 17.6 years, p:0.033). These findings are in accordance with other CAP studies that also reported higher disease severity and increased need for ICU admission in S. pneumoniae pneumonia [20,21]. In agreement with these findings, we showed S. pneumoniae to be an independent cost-driving factor (on average plus 18% per hospitalisation).
Interestingly, Staphylococcus aureus could also be identified as an independent cost driving factor. CAPs caused by this pathogen were associated with a longer LOS and a higher mortality rate as well. This unfavourable outcome might be explained by the difficulty of treating Staphylococcus aureus pulmonary and systemic infections. Recently, Restrepo et al. have reported that late ICU admission versus early ICU admission is more prevalent in cases of CAP caused by Staphylococcus aureus, which aligns with the higher mortality rate observed in our study [22].
In our study, median total costs of hospitalisation were almost €4,000 per patient. These expenditures are higher compared to similar studies performed in Germany and Spain (median costs of €1,362 [23], €1,683 [24] and €1,553 [25], respectively), but lower than reported in a study from the United Kingdom (£1,700-5,100, depending on length of stay [7]) and a European study (US$6,530 in a secondary-level hospital in the Netherlands and US$8,444 in a teaching hospital) [26]. The most likely explanation for these discrepancies in hospital costs are expected to be differences in registration, and individual resource item prices. Furthermore, diagnostic and treatment standards might differ between countries, leading to other price calculations. The recent study of Ostermann et al., however, showed no large differences in mean total duration of hospital stay for CAP between several EU countries (range 9.6-15.0 days) [26]. Unfortunately, most published studies do not indicate prices of individual resource items, which makes detailed comparisons between studies very difficult. Besides this, none of the available studies in literature included aetiological groups in their analyses, further limiting the possibility of a relative comparison with our study findings at this moment.
A further relevant finding in our study was that 57% of the total costs of hospitalisation is due to general ward nursing. This finding is in accordance with other costs studies [27,28]. The latter is also reflected by C. burnetii, causing a relatively milder course of the disease and a significant shorter duration of hospital stay, being identified as an independent cost limiting factor in the multivariable model.
In the present study, costs of medication represented a very small part of the total costs of hospitalisation (on average 3.2%). This means that policies aiming at an early intravenous to oral switch of antimicrobial treatment will not result in substantial cost-savings by reducing drug-expenses; costs might be reduced if the switch resulted in earlier hospital discharge. Medication costs for pneumonia caused by Legionella pneumophila appeared significantly higher compared to other aetiological groups. This is most likely caused by a higher ICU admission rate for these pneumonias and linked to the use of specific drugs such as fresh frozen plasma and sedatives.
This study has several strengths. First, we were able to identify the causative pathogen in a large number of patients enabling comparisons between aetiological groups. Second, we analysed resource utilization on an individual patient level. Third, data of two hospitals were studied (showing no differences) adding to the external validity of the findings. Besides this, the characteristics of the patients studied resemble data from another large nationwide CAP cohort from the Netherlands further adding to the generalisability of the findings [15].
There are also limitations that need to be addressed. First, due to missing data in some resources categories, not all 505 patients could be included in the overall cost analyses. This was due to being unable to retrieve some resource use from the years 2004 until 2006. We consider, however, that this has no impact on the validity of the findings because the more recent years are fully included , making the total costs of hospitalisation representative for the present standard of care for CAP. A further reassuring factor is that the comparison of patient characteristics and clinical outcomes of the 361 patients included in the analyses with the 144 patients not included, showed no large differences (see Additional file 1: Table S2). However, the lower number of patients available for analysis resulted in some aetiological subgroups becoming rather small.
Another limitation is that patients directly admitted to the ICU were absent in the study cohorts used. In the most recent cohort, 25 of the 817 eligible patients (3%) were not included due to direct ICU admission. This phenomenon could have lead to an underestimation of the absolute costs of hospitalisation for CAP. However, given this low percentage, we expect this effect to be rather small. Furthermore, it is very unlikely to have biased the relative costs per pathogen.
Finally, we cannot rule out that the costs related to microbiology exams are overestimated (9% share of total costs of hospitalisation). We studied patients who had participated in clinical studies in which a large panel of microbiological tests had been performed to maximize pathogen identification. However, presuming this resulted in a 50% increase in microbiology costs, decreasing these costs by 50% influences the total costs by less than 5%. In the present study, 58.2% of the causative pathogens could be identified, which is relatively high as compared to other studies [9].
Conclusions
In conclusion, in the present study we have shown that the total costs of hospitalisation for CAP vary considerably between patients and this variation can be largely explained by differences in length of hospital stay. Increased disease severity, and S. pneumoniae and Staphylococcus aureus as causative pathogens, are independent cost driving factors. This suggests, from a cost perspective, to focus further research on better in-hospital treatment and prevention of CAP caused by these pathogens. As standards of care and individual resource item prices are expected to differ between countries, further study in other countries should be performed to confirm the results of this study.
Consent
From all patients written informed consent was obtained in both studies.
Abbreviations
C. burnetii: Coxiella burnetii; CAP: Community-acquired pneumonia; H. influenzae: Haemophilus influenzae; ICU: Intensive care unit; IQR: Interquartile range; L. pneumophila: Legionella pneumophila; M. pneumoniae: Mycoplasma pneumoniae; PCR: Polymerase chain reaction; PSI: Pneumonia severity index; S. pneumoniae: Streptococcus pneumoniae; SD: Standard deviation.
Competing interests
The department of Pharmacoepidemiology and Clinical Pharmacology, Utrecht Institute for Pharmaceutical Sciences, has received unrestricted research funding from the Netherlands Organisation for Health Research and Development (ZonMW), the Dutch Health Care Insurance Board (CVZ), the Royal Dutch Pharmacists Association (KNMP), the private-public funded Top Institute Pharma (http://www.tipharma.nl, includes co-funding from universities, government, and industry), the EU Innovative Medicines Initiative (IMI), EU 7th Framework Program (FP7), the Dutch Medicines Evaluation Board, the Dutch Ministry of Health and industry (including GlaxoSmithKline, Pfizer, and others).
Authors’ contributions
SMCS performed the data analysis and interpretation and drafted the manuscript. WJWB and GTR were involved in data interpretation and revised the manuscript critically for important intellectual content. RH, GPV and JCG revised the manuscript critically. EMWG designed the study, was involved in data analysis and interpretation and revised the manuscript critically for important intellectual content. All authors had full access to the data and can take responsibility for the integrity of the data and the accuracy of the data analysis. All authors approved the final version of the manuscript. EMWG is the guarantor. All authors read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Web appendix: Table S1. Serotype distribution in 51 patients with Streptococcus pneumoniae pneumonia. Table S2. Patient characteristics of 361 patients included in the pneumonia cost analyses compared to patients not included in the cost analyses. Table S3. Top 5 most frequently used items for each resource group. Table S4. Median hospital costs in euro with interquartile range per aetiology differentiated by resource group. Table S5. P-values of the seven resource categories subdivided by ten aetiologic groups. Table S6. Median total costs of hospitalisation in euro of pneumococcal vaccines serotypes compared with costs of non-vaccine serotypes, with serotyping determined in two manners.
Contributor Information
Simone MC Spoorenberg, Email: s.spoorenberg@antoniusziekenhuis.nl.
Willem Jan W Bos, Email: w.bos@antoniusziekenhuis.nl.
Rik Heijligenberg, Email: HeijligenbergR@zgv.nl.
Paul GP Voorn, Email: p.voorn@antoniusziekenhuis.nl.
Jan C Grutters, Email: j.grutters@antoniusziekenhuis.nl.
Ger T Rijkers, Email: g.rijkers@antoniusziekenhuis.nl.
Ewoudt MW van de Garde, Email: e.van.de.garde@antoniusziekenhuis.nl.
Acknowledgements
We are indebted to Mark Ruitenbeek, Mariette Broekman, and Saskia Linssen (Department of Finances and Information services, St. Antonius Hospital, Nieuwegein) for extracting resource data from the St. Antonius hospital administrative databases. We are also grateful to Rik Eding (Datawarehouse, Gelderse Vallei, Ede) for extracting resource data from the Gelderse Vallei administrative databases and to Mirian Kaal (Department of Hospital Pharmacy, Gelderse Vallei, Ede), who helped us to complete patient’s medication records.
Funding
This study was financially supported by GlaxoSmithKline.
References
- Anderson RN. Deaths: leading causes for 2000. Natl Vital Stat Rep. 2002;14(16):1–85. [PubMed] [Google Scholar]
- Thomas CP, Ryan M, Chapman JD, Stason WB, Tompkins CP, Suaya JA, Polsky D, Mannino DM, Shepard DS. Incidence and Cost of Pneumonia in Medicare Beneficiaries. Chest. 2012;14(4):973–981. doi: 10.1378/chest.11-1160. [DOI] [PubMed] [Google Scholar]
- Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA. 2005;14(21):2712–2719. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- Jackson ML, Neuzil KM, Thompson WW, Shay DK, Yu O, Hanson CA, Jackson LA. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004;14(11):1642–1650. doi: 10.1086/425615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauer TT, Welte T, Ernen C, Schlosser BM, Thate-Waschke I, De Zeeuw J, Schultze-Werninghaus G. Cost analyses of community-acquired pneumonia from the hospital perspective. Chest. 2005;14(4):2238–2246. doi: 10.1378/chest.128.4.2238. [DOI] [PubMed] [Google Scholar]
- Monge V, San-Martin VM, Gonzalez A. The burden of community-acquired pneumonia in Spain. Eur J Public Health. 2001;14(4):362–364. doi: 10.1093/eurpub/11.4.362. [DOI] [PubMed] [Google Scholar]
- Guest JF, Morris A. Community-acquired pneumonia: the annual cost to the National Health Service in the UK. Eur Respir J. 1997;14(7):1530–1534. doi: 10.1183/09031936.97.10071530. [DOI] [PubMed] [Google Scholar]
- Martin LG, Freedman VA, Schoeni RF, Andreski PM. Health and functioning among baby boomers approaching 60. J Gerontol B Psychol Sci Soc Sci. 2009;14(3):369–377. doi: 10.1093/geronb/gbn040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tessmer A, Welte T, Schmidt-Ott R, Eberle S, Barten G, Suttorp N, Schaberg T. CAPNETZ study group. Influenza vaccination is associated with reduced severity of community-acquired pneumonia. Eur Respir J. 2011;14(1):147–153. doi: 10.1183/09031936.00133510. [DOI] [PubMed] [Google Scholar]
- Meijvis SC, Hardeman H, Remmelts HH, Heijligenberg R, Rijkers GT, Van Velzen-Blad H, Voorn GP, van de Garde EM, Endeman H, Grutters JC, Bos WJ, Biesma DH. Dexamethasone and length of hospital stay in patients with community-acquired pneumonia: a randomised, double-blind, placebo-controlled trial. Lancet. 2011;14(9782):2023–2030. doi: 10.1016/S0140-6736(11)60607-7. [DOI] [PubMed] [Google Scholar]
- Maruyama T, Taguchi O, Niederman MS, Morser J, Kobayashi H, Kobayashi T, D’Alessandro-Gabazza C, Nakayama S, Nishikubo K, Noguchi T, Takei Y, Gabazza EC. Efficacy of 23-valent pneumococcal vaccine in preventing pneumonia and improving survival in nursing home residents: double blind, randomised and placebo controlled trial. BMJ. 2010;14:c1004. doi: 10.1136/bmj.c1004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Snedecor SJ, Strutton DR, Ciuryla V, Schwartz EJ, Botteman MF. Transmission-dynamic model to capture the indirect effects of infant vaccination with Prevnar (7-valent pneumococcal conjugate vaccine (PCV7)) in older populations. Vaccine. 2009;14(34):4694–4703. doi: 10.1016/j.vaccine.2009.05.062. [DOI] [PubMed] [Google Scholar]
- Huss A, Scott P, Stuck AE, Trotter C, Egger M. Efficacy of pneumococcal vaccination in adults: a meta-analysis. CMAJ. 2009;14(1):48–58. doi: 10.1503/cmaj.080734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moberley SA, Holden J, Tatham DP, Andrews RM. Vaccines for preventing pneumococcal infection in adults. Cochrane Database Syst Rev. 2008;14:CD000422. doi: 10.1002/14651858.CD000422.pub2. doi(1):CD000422. [DOI] [PubMed] [Google Scholar]
- Remmelts HH, Spoorenberg SM, Oosterheert JJ, Bos WJ, De Groot MC, Van de Garde EM. The role of vitamin D supplementation in the risk of developing pneumonia: three independent case–control studies. Thorax. 2013;14(11):990–996. doi: 10.1136/thoraxjnl-2013-203623. [DOI] [PubMed] [Google Scholar]
- Endeman H, Meijvis SC, Rijkers GT, Van Velzen-Blad H, Van Moorsel CH, Grutters JC, Biesma DH. Systemic cytokine response in patients with community-acquired pneumonia. Eur Respir J. 2011;14(6):1431–1438. doi: 10.1183/09031936.00074410. [DOI] [PubMed] [Google Scholar]
- Van Mens SP, Meijvis SC, Endeman H, Van Velzen-Blad H, Biesma DH, Grutters JC, Vlaminckx BJ, Rijkers GT. Longitudinal analysis of pneumococcal antibodies during community-acquired pneumonia reveals a much higher involvement of Streptococcus pneumoniae than estimated by conventional methods alone. Clin Vaccine Immunol. 2011;14(5):796–801. doi: 10.1128/CVI.00007-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DBC Onderhoud Price Table V20120329. [ http://www.dbconderhoud.nl/index.php?option=com_docman&task=cat_view&gid=725&Itemid=404]
- Medicine costs Health Care Institute the Netherlands. [ http://www.medicijnkosten.nl/]
- Capelastegui A, Espana PP, Bilbao A, Gamazo J, Medel F, Salgado J, Gorostiaga I, De Goicoechea MJ L, Gorordo I, Esteban C, Altube L, Quintana JM. on behalf of Poblational Study of Pneumonia (PSoP) Group. Etiology of community-acquired pneumonia in a population-based study: Link between etiology and patients characteristics, process-of-care, clinical evolution and outcomes. BMC Infect Dis. 2012;14(1):134. doi: 10.1186/1471-2334-12-134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restrepo MI, Mortensen EM, Velez JA, Frei C, Anzueto A. A comparative study of community-acquired pneumonia patients admitted to the ward and the ICU. Chest. 2008;14(3):610–617. doi: 10.1378/chest.07-1456. [DOI] [PubMed] [Google Scholar]
- Restrepo MI, Mortensen EM, Rello J, Brody J, Anzueto A. Late admission to the ICU in patients with community-acquired pneumonia is associated with higher mortality. Chest. 2010;14(3):552–557. doi: 10.1378/chest.09-1547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ott SR, Hauptmeier BM, Ernen C, Lepper PM, Nuesch E, Pletz MW, Hecht J, Welte T, Bauer TT. Treatment failure in pneumonia: impact of antibiotic treatment and cost analysis. Eur Respir J. 2012;14(3):611–618. doi: 10.1183/09031936.00098411. [DOI] [PubMed] [Google Scholar]
- Reyes S, Martinez R, Valles JM, Cases E, Menendez R. Determinants of hospital costs in community-acquired pneumonia. Eur Respir J. 2008;14(5):1061–1067. doi: 10.1183/09031936.00083107. [DOI] [PubMed] [Google Scholar]
- Bartolome M, Almirall J, Morera J, Pera G, Ortun V, Bassa J, Bolibar I, Balanzo X, Verdaguer A. Maresme Community-Acquired Pneumonia Study Group (GEMPAC): A population-based study of the costs of care for community-acquired pneumonia. Eur Respir J. 2004;14(4):610–616. doi: 10.1183/09031936.04.00076704. [DOI] [PubMed] [Google Scholar]
- Ostermann H, Garau J, Medina J, Pascual E, McBride K, Blasi F. REACH study group. Resource use by patients hospitalized with community-acquired pneumonia in Europe: analysis of the REACH study. BMC Pulm Med. 2014;14(1):36–2466. doi: 10.1186/1471-2466-14-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sun HK, Nicolau DP, Kuti JL. Resource utilization of adults admitted to a large urban hospital with community-acquired pneumonia caused by Streptococcus pneumoniae. Chest. 2006;14(3):807–814. doi: 10.1378/chest.130.3.807. [DOI] [PubMed] [Google Scholar]
- Orrick JJ, Segal R, Johns TE, Russell W, Wang F, Yin DD. Resource use and cost of care for patients hospitalised with community acquired pneumonia: impact of adherence to infectious diseases society of america guidelines. Pharmacoeconomics. 2004;14(11):751–757. doi: 10.2165/00019053-200422110-00005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Web appendix: Table S1. Serotype distribution in 51 patients with Streptococcus pneumoniae pneumonia. Table S2. Patient characteristics of 361 patients included in the pneumonia cost analyses compared to patients not included in the cost analyses. Table S3. Top 5 most frequently used items for each resource group. Table S4. Median hospital costs in euro with interquartile range per aetiology differentiated by resource group. Table S5. P-values of the seven resource categories subdivided by ten aetiologic groups. Table S6. Median total costs of hospitalisation in euro of pneumococcal vaccines serotypes compared with costs of non-vaccine serotypes, with serotyping determined in two manners.


