Abstract
Objective
To estimate the impact of antiretroviral therapy (ART) on labor productivity and income using detailed employment data from two large tea plantations in western Kenya for HIV-infected tea pluckers who initiated ART.
Design
Longitudinal study using primary data on key employment outcomes for a group of HIV-infected workers receiving anti-retroviral therapy (ART) and workers in the general workforce.
Methods
We used nearest-neighbor matching methods to estimate the impacts of HIV/AIDS and ART among 237 HIV-positive pluckers on ART (index group) over a four year period (2 years pre- and post-ART) on four monthly employment outcomes—days plucking tea, total kilograms harvested, total days working, and total labor income. Outcomes for the index group were compared to those for a matched reference group from the general workforce.
Results
We observed a rapid deterioration in all four outcomes for HIV-infected subjects in the period before ART initiation and then a rapid improvement after treatment initiation. By 18–24 months after treatment initiation, the index group harvested 8% (males) and 19% (females) less tea than reference subjects. The index group earned 6% (males) and 9% (females) less income from labor than reference subjects. Women’s income would have dropped further if they had not been able to offset their decline in tea plucking by spending more time on non-plucking assignments.
Conclusions
HIV-infected workers experienced long-term income reductions before and after initiating ART. The implications of such long-term impacts in low-income countries have not been adequately addressed.
Keywords: HIV, AIDS, antiretroviral therapy, income, labor productivity, Kenya
INTRODUCTION
While the biomedical effectiveness of antiretroviral therapy (ART) for HIV/AIDS is well established [1–5], far less is known about the “social effectiveness” of ART for adults in sub-Saharan Africa. Social effectiveness can be defined as a patient’s contribution to household welfare after initiating ART, as compared to what their contribution would have been in the absence of HIV infection. One primary way that working-aged adults contribute to household welfare is by generating income in either the formal or informal sector. Because HIV/AIDS typically affects adults in their prime working ages [6], if treatment is to be truly socially effective, it must not only keep patients alive, but also allow them to work productively and engage in other normal daily activities.
Unlike biomedical effectiveness, which can readily be determined for individual patients through laboratory monitoring and medical exams, in most settings labor productivity cannot be measured at the individual level. For most work activities, the only individual measures of productivity that can be observed are labor force participation (whether an individual is employed or not) and absenteeism (presence in the workplace on any given day) (see, e.g., [7, 8]). Labor force participation and absenteeism are incomplete measures of productivity, however, because they do not capture what is known as “impaired presenteeism” -- when workers return to work but are not fully productive due to illness or disability [9–12].
In sub-Saharan Africa, agricultural laborers harvesting cash crops by hand are typically paid based on the quantity they harvest (i.e. their own individual level of production). Tea pluckers employed by tea estates, for example, are paid per kilogram of tea harvested. For workers such as these, we can measure directly any changes over time in an individual’s labor productivity, as indicated by the quantity of tea harvested. Tea estates thus present a unique opportunity to observe the impact of ART treatment on individual output and income.
In 2004, before the public rollout of ART in Kenya began, we demonstrated substantial impacts of HIV illness on labor productivity in the year and a half before an untreated worker died or stopped working due to AIDS [13]. In 2008 and 2009, we published preliminary results of an ongoing longitudinal cohort study of HIV-infected tea plantation workers who initiated ART [14, 15] based on samples of 59 and 97 workers during the first year on treatment. With the study completed, we now report full results over four years (two years pre-ART, two years on ART, n=237) for multiple outcomes for tea pluckers on ART and matched comparison groups from the general workforce. Our primary objective is to evaluate if and how quickly HIV-infected workers initiating ART return to a typical pattern of employment found in the general workforce for similar, mainly HIV-negative workers.
METHODS
Study Site
The study was conducted at two large tea company plantations located in Kericho District of the southern Rift Valley Province of Kenya. In 2008–2009, adult HIV prevalence in Rift Valley Province was estimated at 4.3%, although a substantial share of the study population comes from neighboring Nyanza Province, with HIV prevalence of 13.9% [16]. A detailed description of the study site is available elsewhere [13–15]. Each company maintains a central hospital and a group of satellite dispensaries that provide medical care to workers and their dependents free of charge. ART became available at the company hospitals in 2004.
Tea pluckers spend most days harvesting tea leaf. On any given workday, however, tea pluckers can instead be assigned to non-plucking assignments, which are typically field maintenance activities. These non-plucking assignments are called “light duty” and some are relatively easy assignments (weeding, sweeping, transplanting seedlings), though others are much more strenuous (pruning tea plants).
When workers are assigned to plucking tea, baskets of tea are weighed electronically in stations near the fields and pluckers are paid a fixed rate per kilogram (kg) of tea leaf plucked. The payment per kilogram harvested, determined through union contracts, was 9.8 KES/kg in 2011 (USD 0.12 using an average exchange rate of 82.4 KES/USD in 2011). Real pay rates remained relatively constant throughout the study period. When pluckers are assigned to non-plucking tasks, they are paid a flat daily rate equal to the payment for harvesting 32.4 kg of tea (about KES 318.23 in 2011, or $3.86, with minor variation based on length of service and company). A field supervisor can assign non-plucking tasks based on operational need, the worker’s request, or the company hospital’s request.
Because healthy workers can typically harvest more than 32.4 kg of tea per day, this pay structure provides an incentive for healthy workers to prefer plucking tea to performing non-plucking tasks. Sick workers may request non-plucking assignments to maintain their income and mask, at least to some degree, their poorer performance (a form of impaired presenteeism). Each month, individual workers’ incomes depend on the total quantity of tea leaf harvested and the number of days they performed non-plucking tasks.
Data Development and Study Groups
We enrolled in the study HIV-infected adults (called the index group) working for the tea companies during 2006 and 2007 who were permanently employed as tea pluckers, HIV-infected, and either on ART at the time of enrollment or not yet on ART but with a most recent CD4 cell count ≤ 350 cells/mm3. Study enrollment occurred as workers visited the ART clinic for regular appointments. Potentially eligible pluckers were referred for enrollment by clinic staff and then completed the consenting process with the study nurse at each site to allow the study to review their medical and employment records. Workers in the index group initiated ART between April 2004 and May 2007.
Using company payroll records, we extracted daily payroll data for each index subject for 49 months: the 24 months before initiating ART, the month of ART initiation, and the 24 months after initiation. We collapsed daily payroll data (daily job assignment or type of leave and quantities of tea plucked) into monthly units of observation.
As noted above, the companies employ thousands of tea pluckers on permanent contracts (13,178 pluckers as of January 2005). Although the HIV status of these workers is unknown, the relatively low HIV prevalence in the study area suggests that the great majority were HIV-negative. These tea pluckers on permanent contract in the general workforce provided a pool of possible comparison workers (called the potential reference group) for each index subject. For management purposes, the tea companies have organized each plantation into multiple estates that cover a specific geographic area within the overall plantation. All workers in each estate are called here an estate group of workers. We randomly allocated each worker in an estate group to sub-groups, called sub-estate groups. We then allocated one index subject working in the same estate to one of the sub-estate groups (one index subject maximum for each sub-estate group).
For all workers in each sub-estate group, we created a “duration-on-ART” variable as the difference in months between the calendar date of observation and the date of ART initiation for the index subject allocated to the sub-estate group. For example, if the index worker in the sub-estate group began ART in December of 2008, the duration-on-ART variable was 0 for December 2008 for all workers in the sub-estate group. Through this process, all workers in each estate were assigned two types of ‘time variables’: the calendar month and year of observation and a duration-on-ART variable. The pool of workers from the general workforce within each sub-estate group formed the pool of potential reference subjects for each index subject.
Data for workers in the general workforce are not complete panel data over the entire study period. The companies changed data management systems and/or management structures across the plantations at different periods of time, both of which resulted individuals being assigned new employee identification numbers at various times during the study period.
Definitions of Primary Employment Outcomes
We analyzed three primary employment outcomes: days spent plucking tea per month; total days working per month (plucking plus non-plucking days); and total kilograms of tea harvested per month. A fourth outcome is total income from labor per month, which is calculated as total kilograms harvested per month times the price paid per kilogram harvested plus the number of non-plucking days worked in the month times the daily wage for non-plucking activities. The basic pay rates for 2011 presented above are used to aggregate labor income into a constant real value.
Statistical Analysis
With 49 total months of time in the analysis (24 months pre-ART, the month of ART initiation, and 24 months on ART), we grouped the analysis into 8 semi-annual periods (duration-on-ART for months -24 to -19, -18 to -13, -12 to -7, -6 to -1; the month of initiation (month 0), and duration-on-ART for months 1–6, 7–12, 13–18, 19–24). For the index group, the group mean during each semi-annual period shows shows the general trend in employment outcomes before and after initiating ART.
Rather than using the entire pool of potential references for each index subject (all workers in the sub-estate group), we used nearest-neighbor matching methods [17, 18] to identify 4 matched reference workers for each index subject. For each month in each semi-annual period, index subjects were matched to 4 reference subjects from the pool of potential reference subjects based on estate within the plantation, duration on ART, calendar time (month and year), age, and years of experience on the plantation. Matching by estate controlled to some degree for inherent productivity differences across locations within the plantations, such as tea plant age, field terrain, and local rainfall. Matching on age and duration of employment controlled for the effect of these characteristics on individual productivity (e.g. strength and skill). Matching on calendar time and duration-on-ART within the semi-annual period controlled for seasonality and time on treatment for the index subjects. To adjust for imperfect matching on continuous variables (e.g. age, years of experience), a bias-corrected version of the matching estimator with robust standard errors was used (using nnmatch routine in STATA 11, estimating average treatment effects on the treated). Because men and women typically have different work patterns (e.g. men are typically assigned more non-plucking assignments than women), we stratified the analysis by gender.
In the pre-ART periods, the difference in mean outcomes between the two groups over time represents the impact of untreated HIV on employment outcomes. In the post-ART periods, the difference in mean outcomes between the two groups represents the ability of treated workers to return to a typical pattern of employment as measured by the outcomes used in this analysis (the matched reference group provides the counterfactual for this analysis).
Ethics approvals were obtained from Boston University, the Kenya Medical Research Institute, and the Walter Reed Army Institute for Research.
RESULTS
Among the 295 index subjects originally enrolled in the study, 45 never initiated ART during the study period and are excluded from this analysis. In addition, 8 were excluded because their medical records could not be located at the company hospitals to confirm their dates of ART initiation, and 5 were excluded because they could not be identified in the payroll database. This gave us a total of 237 index subjects for analysis. Table 1 shows the demographic and clinical characteristics of the index group, stratified by gender. Among the 237, 15 (6%) stopped working on the plantations during the 24-month follow up period after initiating ART (died, retired, resigned). For these 15 workers, an average of 15 months of follow up data after initiating ART are available.
Table 1.
Demographic and clinical characteristics among 237 HIV infected tea plantation workers who initiated antiretroviral therapy in western Kenya (measured at the month of initiating ART)
| Variable | Female (N=112) | Male (N=125) |
|---|---|---|
| Mean age (range) | 39.4 (27.4–53) | 39.5 (24.8–54.4) |
| Mean years’ experience (range) | 8.2 (1–24) | 7.7 (0.5–23) |
| Baseline CD4 median (IQR) | 178 (91–243) | 153.5 (85–215) |
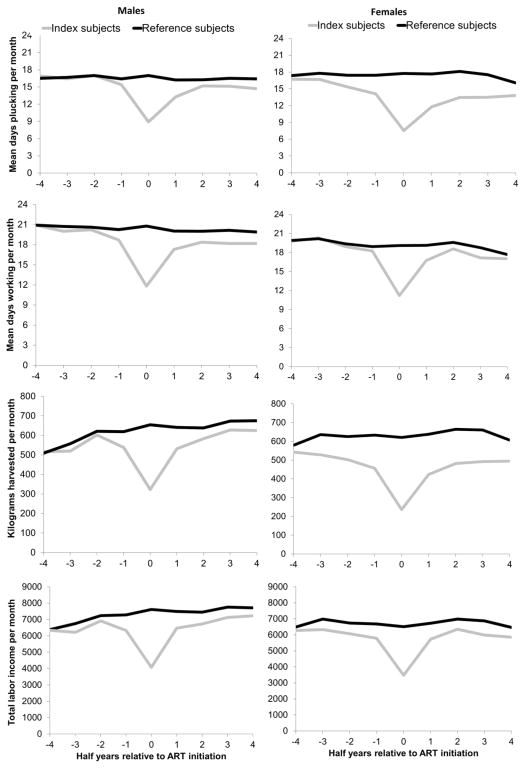
We observed a rapid deterioration in all four outcomes for HIV-infected subjects in the period before ART initiation and then a rapid improvement after treatment initiation. Table 2 for men and Table 3 for women report monthly means and estimated mean differences for index and reference subjects within each semi-annual period for total days working per month, days spent plucking per month, and kilograms harvested per month (based on nearest neighbor matching). Figure 1 displays the results for each outcome over each semi-annual period, stratified by gender. In each figure, the index subjects initiated ART in month 0, semi-annual period -4 covers months -24 to -19 prior to initiating ART, and so on. Table 4 summarizes results for all outcomes by gender. We highlight key results below.
Table 2.
Differences in days working, days plucking, and kilograms plucked per month for male HIV infected tea pluckers in relation to ART initiation
| Days working
| ||||
|---|---|---|---|---|
| Duration on ART | Index | Reference | Mean Difference (95% CI) | % reduction |
| -24 to -19 months | 20.92 | 20.9 | 0.02 (−0.56 to 0.6) | 0% |
| -18 to -13 months | 20.01 | 20.72 | −0.7 (−1.32 to −0.09) | −3% |
| -12 to -7 months | 20.21 | 20.61 | −0.4 (−1.02 to 0.23) | −2% |
| -6 to -1 months | 18.71 | 20.24 | −1.53 (−2.16 to −0.9) | −8% |
| 0 months | 11.81 | 20.78 | −8.97 (−10.41 to −7.52) | −43% |
| 1 to 6 months | 17.29 | 20.03 | −2.75 (−3.4 to −2.1) | −14% |
| 7 to 12 months | 18.38 | 20.01 | −1.64 (−2.26 to −1.02) | −8% |
| 13 to 18 months | 18.18 | 20.13 | −1.96 (−2.61 to −1.3) | −10% |
| 19 to 24 months | 18.19 | 19.89 | −1.7 (−2.42 to −0.98) | −9% |
| Days plucking
| ||||
|---|---|---|---|---|
| Duration on ART | Index | Reference | Mean Difference (95% CI) | % reduction |
| -24 to -19 months | 16.91 | 16.51 | 0.39 (−0.39 to 1.18) | 2% |
| -18 to -13 months | 16.47 | 16.68 | −0.21 (−1.01 to 0.59) | −1% |
| -12 to -7 months | 17.01 | 16.99 | 0.02 (−0.76 to 0.79) | 0% |
| -6 to -1 months | 15.43 | 16.41 | −0.98 (−1.8 to −0.16) | −6% |
| 0 months | 8.93 | 16.99 | −8.06 (−9.75 to −6.37) | −47% |
| 1 to 6 months | 13.3 | 16.22 | −2.92 (−3.72 to −2.12) | −18% |
| 7 to 12 months | 15.19 | 16.24 | −1.05 (−1.85 to −0.25) | −6% |
| 13 to 18 months | 15.12 | 16.51 | −1.38 (−2.19 to −0.57) | −8% |
| 19 to 24 months | 14.71 | 16.43 | −1.72 (−2.59 to −0.86) | −10% |
| Kilograms plucked
| ||||
|---|---|---|---|---|
| Duration on ART | Index | Reference | Mean Difference (95% CI) | % reduction |
| -24 to -19 months | 516.7 | 508.9 | 7.83 (−32.95 to 48.61) | 2% |
| -18 to -13 months | 519.8 | 557.4 | −37.56 (−77.07 to 1.96) | −7% |
| -12 to -7 months | 601.8 | 621 | −19.15 (−57.34 to 19.03) | −3% |
| -6 to -1 months | 538.9 | 619 | −80.07 (−118.65 to −41.49) | −13% |
| 0 months | 322.9 | 654 | −331.08 (−414.66 to −247.51) | −51% |
| 1 to 6 months | 531.5 | 641 | −109.5 (−149.05 to −69.95) | −17% |
| 7 to 12 months | 583.4 | 637.8 | −54.45 (−95.34 to −13.55) | −9% |
| 13 to 18 months | 627.9 | 673.6 | −45.73 (−89.98 to −1.49) | −7% |
| 19 to 24 months | 624.7 | 675.4 | −50.72 (−97.41 to −4.02) | −8% |
Table 3.
Differences in days working, days plucking, and kilograms plucked per month for female HIV infected tea pluckers in relation to ART initiation
| Days working
| ||||
|---|---|---|---|---|
| Duration on ART | Index | Reference | Mean Difference (95% CI) | % reduction |
| -24 to -19 months | 19.74 | 19.9 | −0.16 (−0.88 to 0.57) | −1% |
| -18 to -13 months | 20.3 | 20.16 | 0.14 (−0.51 to 0.79) | 1% |
| -12 to -7 months | 18.93 | 19.36 | −0.43 (−1.15 to 0.29) | −2% |
| -6 to -1 months | 18.24 | 18.92 | −0.69 (−1.39 to 0.01) | −4% |
| 0 months | 11.21 | 19.08 | −7.88 (−9.52 to −6.24) | −41% |
| 1 to 6 months | 16.75 | 19.12 | −2.38 (−3.09 to −1.66) | −12% |
| 7 to 12 months | 18.57 | 19.59 | −1.02 (−1.68 to −0.35) | −5% |
| 13 to 18 months | 17.16 | 18.77 | −1.61 (−2.36 to −0.85) | −9% |
| 19 to 24 months | 17 | 17.69 | −0.69 (−1.44 to 0.07) | −4% |
| Days plucking
| ||||
|---|---|---|---|---|
| Duration on ART | Index | Reference | Mean Difference (95% CI) | % reduction |
| -24 to -19 months | 16.72 | 17.37 | −0.65 (−1.48 to 0.19) | −4% |
| -18 to -13 months | 16.68 | 17.78 | −1.1 (−1.92 to −0.28) | −6% |
| -12 to -7 months | 15.35 | 17.43 | −2.08 (−2.94 to −1.21) | −12% |
| -6 to -1 months | 14.1 | 17.43 | −3.33 (−4.18 to −2.48) | −19% |
| 0 months | 7.56 | 17.74 | −10.18 (−11.97 to −8.38) | −57% |
| 1 to 6 months | 11.79 | 17.65 | −5.86 (−6.7 to −5.02) | −33% |
| 7 to 12 months | 13.46 | 18.11 | −4.65 (−5.48 to −3.81) | −26% |
| 13 to 18 months | 13.5 | 17.51 | −4.01 (−4.88 to −3.14) | −23% |
| 19 to 24 months | 13.83 | 16.06 | −2.24 (−3.09 to −1.38) | −14% |
| Kilograms plucked
| ||||
|---|---|---|---|---|
| Duration on ART | Index | Reference | Mean Difference (95% CI) | % reduction |
| -24 to -19 months | 542.3 | 579.8 | −37.46 (−78.93 to 4) | −6% |
| -18 to -13 months | 528.6 | 636.1 | −107.5 (−147.53 to −67.47) | −17% |
| -12 to -7 months | 503.1 | 625.4 | −122.3 (−162.83 to −81.77) | −20% |
| -6 to -1 months | 456.6 | 633.6 | −177.01 (−216.05 to −137.96) | −28% |
| 0 months | 236.1 | 621.3 | −385.2 (−468.98 to −301.41) | −62% |
| 1 to 6 months | 423.8 | 638.2 | −214.48 (−253.23 to −175.73) | −34% |
| 7 to 12 months | 482.2 | 664.5 | −182.3 (−221.99 to −142.62) | −27% |
| 13 to 18 months | 492.5 | 660.8 | −168.31 (−210.72 to −125.9) | −25% |
| 19 to 24 months | 494.6 | 607.2 | −112.55 (−153.93 to −71.18) | −19% |
Figure 1.
Comparison of mean days plucking (row 1), mean days working (row 2), mean kilograms plucked (row 3) per month, and mean income per month from labor (row 4) for HIV infected patients and matched comparison in relation to the month initiating ART for males (column 1) and females (column 2)*
Table 4.
Summary of differences in outcomes over time between index and reference subjects (%), by sex
| Time period | Days working | Days plucking | Kilograms plucked | Labor Income | ||||
|---|---|---|---|---|---|---|---|---|
| Males | Females | Males | Females | Males | Females | Males | Females | |
| Month -24 to -19 | 0 | −1 | 2 | −4 | 2 | −6 | −1 | −3 |
| Month -18 to -13 | −3 | 1 | −1 | −6 | −7 | −17 | −8 | −9 |
| Month -12 to -7 | −2 | −2 | 0 | −12 | −3 | −20 | −4 | −10 |
| Month -6 to -1 | −8 | −4 | −6 | −19 | −13 | −28 | −13 | −13 |
| Month 0 | −43 | −41 | −47 | −57 | −51 | −62 | −46 | −47 |
| Month 1 to 6 | −14 | −12 | −18 | −33 | −17 | −34 | −14 | −15 |
| Month 7 to 12 | −8 | −5 | −6 | −26 | −9 | −27 | −10 | −9 |
| Month 13 to 18 | −10 | −9 | −8 | −23 | −7 | −25 | −8 | −13 |
| Month 19 to 24 | −9 | −4 | −10 | −14 | −8 | −19 | −6 | −9 |
Outcomes for males
Two years before initiating ART, none of the four employment outcomes differed for men in the index and reference groups. Circumstances and/or behaviors may have been different between the groups, which resulted in HIV infection in the index group, but these differences were not reflected in employment outcomes.
Although HIV infected, the index group maintained very similar employment outcomes as the matched reference groups over the three semi-annual periods covering months -24 to -7. The male index group worked the same total number of days monthly as the matched reference group, harvested similar quantities of tea per month, and worked the same number of days plucking tea per month. Because of these similar work patterns, total monthly labor income over this period was also very similar.
HIV began to affect men’s employment outcomes during the six months before initiating ART. Outcomes were worst during the month that treatment began, due both to illness and to time off for initiating ART rather. The differences between index and reference groups observed in month 0 become smaller over the first six months on ART but remain statistically significant. As a result, labor income was about 14% less for the index subjects as compared to the matched reference group over this period.
Over the three semi-annual periods covering months 7 to 24 after ART initiation, both total days working and days plucking for men remained significantly below that of the reference group, but the difference was reduced to less than 2 days per month. Index subjects continued to pluck about 50 kilograms less per month than the reference group. In combination, these differences led to a 6–10% reduction in monthly labor income for male index subjects over this period.
Outcomes for females
Compared to men, the pattern of employment outcomes over time for women shows more pronounced differences from the matched reference group earlier in the pre-ART period. While female index subjects worked fewer days plucking than their reference peers, total days working were not reduced as much because, unlike men, women were more likely to shift to non-plucking assignments that allowed them to partially maintain their income. Women thus experienced the effect of HIV earlier in the pre-ART period than men but were able to mitigate some of the impact through shifting to non-plucking tasks. As with men, women in the index group experienced a sharp decline in all employment outcomes in the month they initiated ART (month 0). Similar to men, these differences persisted over the first 6 months on ART.
In the three semi-annual periods covering months 7 to 24 on ART, females returned to work and showed only small differences in total days worked compared to their counterparts not on ART (1.6 days per month or less). Unlike males on ART, however, female index subjects continued to spend fewer days plucking tea than did reference subjects. Over the same period, these women also harvested substantially fewer kilograms of tea leaf monthly (113 to 182 fewer kilograms monthly or 19–27% less). Total monthly labor income was 9–13% less for the female index group than for the matched reference group (610–884 KES).
DISCUSSION
Understanding the social and economic impact of antiretroviral therapy, and not only its biomedical effectiveness, is essential for evaluating the benefits of treatment programs, justifying ongoing funding support, and promoting life-long adherence to treatment, but there is little evidence describing how ART affects patients’ social and economic lives. A small but growing literature generally identifies positive consequences for employment outcomes after initiating treatment, as well as some spillovers onto others in the household [7, 8, 15, 19–21]. The study described here contributes to this literature with a unique data set containing objective measures of employment outcomes (not self-reported information), outcome data for patients on ART both before and after they initiate therapy, and outcome data for a matched set of reference subjects drawn from a large population of agricultural workers.
The main conclusion of this study is that modest productivity differences persisted between HIV-infected workers on ART and a matched comparison group from the general workforce 18–24 months after initiating therapy. Women’s income would have fallen further if they had not been able to offset their inability to pluck tea by spending more time on non-plucking assignments. Recent results from a study in India showed that men’s income increased substantially more than women’s after initiating ART [21], which probably would have occurred in this Kenyan setting if women had been unable to shift from plucking to non-plucking assignments. Two new studies from South Africa [22, 23], in contrast, found no differences between men and women in the probability of employment after starting ART, suggesting that sex differences in the effect of ART on labor productivity manifest themselves in reduced productivity while working (impaired presenteeism), rather than in the easier-to-measure outcome of labor force participation.
Despite the strengths of the data set, which include objective daily observations of productivity over multiple years for HIV-infected workers before and after initiating ART and a large pool of reference workers to provide comparative data, our study has limitations. The reference workforce contains some workers who are infected with HIV but who have not come forward for HIV care. With recent estimates of HIV prevalence in Kenya far below 10% [16], however, we anticipate that this has little effect on our results. In addition, because many of our index subjects were enrolled in the study after they had initiated treatment, this study addresses employment outcomes for workers who actually initiated ART and remained on treatment at their company hospital over these initial months. Employment outcomes over time for a cohort of workers recruited when they became eligible for treatment would likely be different because some workers would be lost to follow up, die, retire, or resign before initiating treatment, especially those with low CD4 cell counts at or before initiating treatment. We explored the relationship between productivity outcomes and measures of disease progression (e.g. CD4 count and WHO stage) among those in the index group, but found no relationship between the predictors and productivity outcomes.
Another limitation of this study is that we cannot explain why differences persist in the employment outcomes observed between HIV-infected women and men in the post-ART periods (also see [15]). Although existing evidence does not suggest strong gender-related biological differences in the effectiveness of ART [24–26], the differences in employment outcomes are likely to be associated with socioeconomic factors. As compared to men in the study locations, women allocate much of their non-wage earning time to cooking, cleaning, childcare, and care for sick family members, in which case women may experience more fatigue on-the-job than men. As other possibilities, medical staff may recommend that their female patients be assigned to non-plucking days more than their male patients, women on ART might be likely to request non-plucking assignments than men, and/or managers might be more likely to assign women on ART to non-plucking assignments than men. Future research remains needed to explain better why such differences persist and to explore feasible interventions to mitigate such impacts.
In conclusion, we consider our results to tell a “good news/bad news” story about the impact of ART on employment outcomes. As would be expected, HIV-infected workers experienced substantial reductions in productivity and income before and immediately after initiating ART. The good news is that as time on ART increased, these reductions shrank dramatically. By 24 months after ART initiation, male workers on ART were, on average, 90% as productive as men in the rest of the workforce, and female workers on ART were 80% as productive women in the rest of the of the workforce, as measured by kilograms of tea plucked per month. The bad news is, of course, that the reductions we observed did not disappear entirely even after 24 months on treatment. The losses were larger and lasted longer for women than men. Income losses for female workers were avoided to some extent because they were able to shift from plucking to non-plucking assignments. Without this shift, income losses for female workers would likely have been even larger. For poor people living with HIV/AIDS, and for their employers, households, and communities, the long-term challenges of having a chronic disease in terms of employment, earnings, and poverty alleviation need to be quantified across more countries and sectors of the economy. Programs and policies need to be identified and implemented ensure that the economic benefits of ART are maximized and the remaining costs managed and mitigated to the full extent possible.
Acknowledgments
Sponsorship
Funding for the research presented in this paper was provided by the Fogarty International Center of the National Institutes of Health through the International Studies in Health and Economic Development (ISHED) Program (Grant Number 5R01TW7181-3).
We are deeply grateful to the workers who consented to be part of this study. We also extend our sincerest appreciation to the staff and management of the participating companies, and especially the staff at the hospitals, included in this study for their support and generous assistance in accessing and interpreting medical and employment records. Although the authors are solely responsible for this analysis, we also thank Dr. Josephine Maende, Dr. Augustine Kirui, and Dr. Tonui for their advice and support throughout the completion of the study. This paper is published with the permission of the KEMRI Director.
Footnotes
Disclaimer
The views expressed here are the opinions of the authors and are not to be considered as official or reflecting the views of the Walter Reed Army Institute of Research, the US Army, the US Department of Defense, and the Henry M. Jackson Foundation for the Advancement of Military Medicine, Inc.
Authors’ contributions
BAL contributed to study conception and design, acquisition of data, data analysis and interpretation, and drafting and critically revising the manuscript.
MPF contributed to study conception and design, acquisition of data, data analysis and interpretation, and drafting and critically revising the manuscript.
SR contributed to study conception and design, interpretation of results, and drafting and critically revising the manuscript.
MB contributed to study design, acquisition of data, interpretation of results, and critically revising the manuscript.
JR contributed to data management and analysis, interpretation of results, and drafting and critically revising the manuscript.
DS contributed to study design, acquisition of data, interpretation of results, and critically revising the manuscript.
FS contributed to study design, acquisition of data, interpretation of results, and critically revising the manuscript.
MW contributed to study conception and design, acquisition of data, interpretation of results, and critically revising the manuscript.
JLS contributed to study conception and design, acquisition of data, interpretation of results, and critically revising the manuscript.
All authors read and approved the final manuscript.
Contributor Information
Bruce. A. LARSON, Email: blarson@bu.edu.
Matthew P. FOX, Email: mfox@bu.edu.
Margaret BII, Email: mbii@wrp-kch.org.
Sydney ROSEN, Email: sbrosen@bu.edu.
Julia ROHR, Email: jrohr@bu.edu.
Douglas SHAFFER, Email: dshaffer@wrp-kch.org.
Fredrick SAWE, Email: fsawe@wrp-kch.org.
Monique WASUNNA, Email: Africa@dndi.org.
Jonathon L. SIMON, Email: jonsimon@bu.edu.
References
- 1.Akileswaran C, et al. Lessons learned from use of highly active antiretroviral therapy in Africa. Clinical Infectious Diseases. 2005;41(3):376–385. doi: 10.1086/431482. [DOI] [PubMed] [Google Scholar]
- 2.Fairall LR, et al. Effectiveness of antiretroviral treatment in a South African program: a cohort study. Arch Intern Med. 2008;168:86–93. doi: 10.1001/archinternmed.2007.10. [DOI] [PubMed] [Google Scholar]
- 3.Sow PS, et al. Implementation of an Antiretroviral Access Program for HIV-1-Infected Individuals in Resource-Limited Settings: Clinical Results From 4 African Countries. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2007;44(3):262–267. doi: 10.1097/QAI.0b013e31802bf109. [DOI] [PubMed] [Google Scholar]
- 4.Lawn SD, et al. Early mortality among adults accessing antiretroviral treatment programmes in sub-Saharan Africa. AIDS. 2008;22:1897–1908. doi: 10.1097/QAD.0b013e32830007cd. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lawn SD, et al. Changing mortality risk associated with CD4 cell response to antiretroviral therapy in South Africa. AIDS. 2009;23(3):335–342. doi: 10.1097/QAD.0b013e328321823f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yamano T, Jayne T. Measuring the impacts of working-age adult mortality on small-scale farm households in Kenya. World Development. 2004;32:99–119. [Google Scholar]
- 7.Habyarimana J, Mbakile B, Pop-Eleches C. The Impact of HIV/AIDS and ARV Treatment on Worker Absenteeism: Implications for African Firms. J Human Resources. 2010;45(4):809–839. [Google Scholar]
- 8.Thirumurthy H, Graff Zivin J, Goldstein M. The Economic Impact of AIDS Treatment: Labor Supply in Western Kenya. Journal of Human Resources. 2008;43(3):511–552. [PMC free article] [PubMed] [Google Scholar]
- 9.Shamansky SL. Presenteeism … or when being there is not being there. Public Health Nursing. 2002;19(2):79–80. doi: 10.1046/j.1525-1446.2002.19201.x. [DOI] [PubMed] [Google Scholar]
- 10.Dew K, Keefe V, Small K. Choosing to work when sick: workplace presenteeism. Social Science and Medicine. 2005;60:2273–2282. doi: 10.1016/j.socscimed.2004.10.022. [DOI] [PubMed] [Google Scholar]
- 11.Middaugh DJ. Presenteeism: sick and tired at work. Medsurg Nurs. 2006;15(2):103–5. [PubMed] [Google Scholar]
- 12.Zhang W, Bansback N, Anis AH. Measuring and valuing productivity loss due to poor health: A critical review. Social Science & Medicine. 2011;72(2):185–192. doi: 10.1016/j.socscimed.2010.10.026. [DOI] [PubMed] [Google Scholar]
- 13.Fox MP, et al. The impact of HIV/AIDS on labour productivity in Kenya. Tropical Medicine and International Health. 2004;9(3):318–324. doi: 10.1111/j.1365-3156.2004.01207.x. [DOI] [PubMed] [Google Scholar]
- 14.Larson BA, et al. Early effects of antiretroviral therapy on work performance: preliminary results from a cohort study of Kenyan agricultural workers. AIDS. 2008;22(3):421–425. doi: 10.1097/QAD.0b013e3282f3cc0c. [DOI] [PubMed] [Google Scholar]
- 15.Larson B, et al. Do the socioeconomic impacts of antiretroviral therapy vary by gender? A longitudinal study of Kenyan agricultural worker employment outcomes. BMC Public Health. 2009;9(1):240. doi: 10.1186/1471-2458-9-240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kenya National Bureau of Statistics (KNBS) and ICF MacroCalverton. Kenya Demographic and Health Survey 2008–09. Calverton, Maryland: KNBS and ICF Macro; 2010. [Google Scholar]
- 17.Imbens GW. Nonparametric Estimation of Average Treatment Effects under Exogeneity: A Review. Review of Economics and Statistics. 2004;86(1):4–29. [Google Scholar]
- 18.Abadie A, Imbens GW. Large Sample Properties of Matching Estimators for Average Treatment Effects. Econometrica. 2006;74(1):235–267. [Google Scholar]
- 19.Zivin JG, Thirumurthy H, Goldstein M. AIDS treatment and intrahousehold resource allocation: Children’s nutrition and schooling in Kenya. Journal of Public Economics. 2009;93(7–8):1008–1015. doi: 10.1016/j.jpubeco.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Larson BA, et al. Early effects of antiretroviral therapy on work performance: preliminary results from a cohort study of Kenyan agricultural workers. AIDS. 2008;22(3):421–425. doi: 10.1097/QAD.0b013e3282f3cc0c. [DOI] [PubMed] [Google Scholar]
- 21.Thirumurthy H, et al. Two-year impacts on employment and income among adults receiving antiretroviral therapy in Tamil Nadu, India: a cohort study. AIDS. 2011;25(2):239–246. doi: 10.1097/QAD.0b013e328341b928. [DOI] [PubMed] [Google Scholar]
- 22.Bor J, et al. In A Study Of A Population Cohort In South Africa, HIV Patients On Antiretrovirals Had Nearly Full Recovery Of Employment. Health Affairs. 2012;31(7):1459–1469. doi: 10.1377/hlthaff.2012.0407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rosen S, et al. The Impact of Antiretroviral Therapy on Quality of Life and Economic Outcomes for South African Patients: Five-Year Follow-Up. International AIDS Economics Network 7th AIDS & Economics Pre-Conference; 2012; Washington, D.C. [Google Scholar]
- 24.Prins M, Meyer L, Hessol N. Sex and the course of HIV infection in the pre-and highly active antiretroviral therapy eras. AIDS. 2005;19:357–370. doi: 10.1097/01.aids.0000161765.75663.27. [DOI] [PubMed] [Google Scholar]
- 25.Wester CW, et al. Higher-than-expected rates of lactic acidosis among highly active antiretroviral therapy treated women in Botswana. Journal of Acquired Immune Deficiency Syndrome. 2007;46:318–322. doi: 10.1097/QAI.0b013e3181568e3f. [DOI] [PubMed] [Google Scholar]
- 26.Hawkins C, et al. Antiretroviral durability and tolerability in HIV-infected adults living in urban Kenya. Journal of Acquired Immune Deficiency Syndrome. 2007;45:304–310. doi: 10.1097/QAI.0b013e318050d66c. [DOI] [PubMed] [Google Scholar]