Abstract
Treatment of mandibular condyle fractures is still controversial, with surgical treatment slowly becoming the preferred option. However, fractures of the condylar head (diacapitular fractures) are still treated conservatively at many institutions. Recently, more and more surgeons have begun to perform open treatment for diacapitular fractures because it allows to restore the anatomical position of the fragments and disc, it allows an immediate functional movement of the jaw, and avoid the ankylosis of the temporomandibular joint induced by the trauma. Several techniques have been proposed to reduce and fix fractures of the condylar head, such as standard bone screws, resorbable screws, resorbable pins, and cannulated lag screws. Therefore, the aim of this article is to review the literature about the surgical treatment of fractures of the condylar head to resume the current knowledge about open treatment of such fractures.
Keywords: mandibular condyle, fracture, condylar head, diacapitular fractures
The condyle is one of the most common sites of mandibular fractures, ranging from 21 to 49% in the literature.1
Treatment of mandibular condyle fractures is still controversial, with surgical treatment slowly becoming the preferred option. However, fractures of the condylar head (diacapitular fractures) are still treated conservatively at many institutions.1 2 3 Previously known as intracapsular fractures, condylar head fractures are more appropriately named diacapitular fractures.3 4
Fractures of the condylar head are usually treated conservatively because of the difficulty in the exposure and fixation and the risk of facial nerve damage. Differently from conservative treatment, open surgery can give early recovery of occlusion and movement of the jaw.5 6 Furthermore, extensive condylar deformation, height reduction of the mandibular ramus, disc displacement, dysfunctional complaints (such as limitation of mandibular mobility, crepitation, lateral deviation during mouth opening), temporomandibular joint (TMJ) ankylosis, and occlusal disturbances have also been described after closed or conservative treatment of diacapitular fractures.7 8
Recently, more and more surgeons have begun to perform open treatment for diacapitular fractures because it allows to restore the anatomical position of the fragments and disc, it allows an immediate functional movement of the jaw, and avoid the ankylosis of the TMJ induced by the trauma.9 10 Several techniques have been proposed to reduce and fix fractures of the condylar head, such as standard bone screws, resorbable screws, resorbable pins, and cannulated lag screws.6
However, a meta-analysis would not be reliable at present because of great inconsistencies in the variables reported and the often little numerosity of the study populations. Therefore, the aim of this article is to review the literature about the surgical treatment of fractures of the condylar head to resume the current knowledge about open treatment of such fractures.
Materials and Methods
A systematic review of published articles using Medline and the MeSH term “mandibular fractures” in combination with the following terms “condylar head,” “intracapsular,” and “diacapitular.” Articles presenting patients surgically treated for condylar head fractures were identified and included as well as animal experimental studies.10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 Data were collected on age, sex, classification, etiology, intervention, management, and complications.
This article was exempted from institutional review board approval as a review study. We followed Helsinki Declaration guidelines.
Classifications
Several classifications have been proposed for diacapitular fractures.
According to the classification of diacapitular fractures of He et al (Fig. 1),10 four types of fractures can be recognized: type A (a fracture line through the lateral third portion of the condylar head with reduction of the ramus height); type B (a fracture line through the central third portion of the condylar head without reduction of the ramus height); type C (a fracture line through the medial third portion of the condylar head without reduction of the ramus height); and type M (a comminuted fracture with multiple fragments, usually more than three, of the condylar head) (Table 1).
Figure 1.
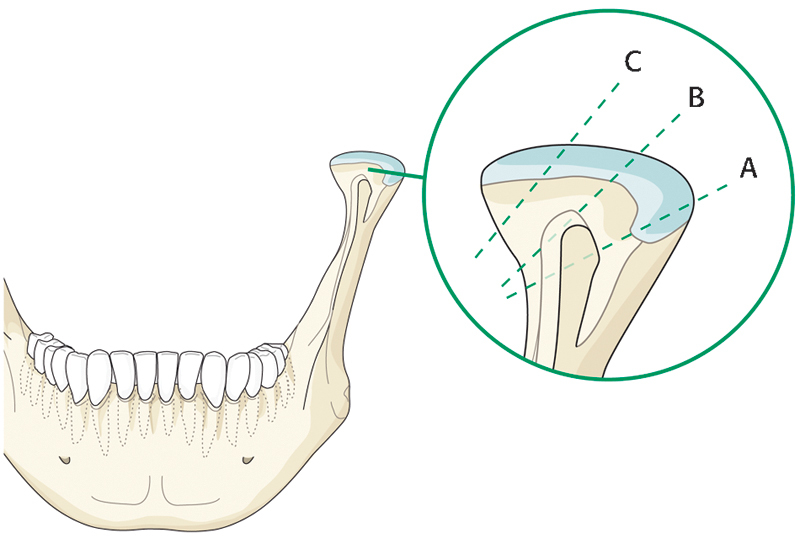
Classification of He et al.
Table 1. He et al and Yang et al's classification of diacapitular fractures.
| Types | Description |
|---|---|
| A | A fracture line through the lateral third portion of the condylar head with reduction of the ramus height |
| B | A fracture line through the central third portion of the condylar head without reduction of the ramus height |
| C | A fracture line through the medial third portion of the condylar head without reduction of the ramus height |
| M | A comminuted fracture with multiple fragments (usually more than three) of the condylar head |
In this classification, confirmed by Loukota et al,4 the height of the ramus is not reduced in fracture types B and C.
Another classification has been proposed by Neff et al,11 which classified diacapitular fractures as type A fractures (with displacement of the medial parts of the condyle maintaining vertical mandibular dimensions), type B fractures (affecting the lateral condyle with reduction of mandibular height), and type M fractures (fractures that include high extracapsular fracture dislocations) (Table 2).
Table 2. Neff et al's classification of diacapitular fractures.
| Types | Description |
|---|---|
| A | Fractures with displacement of the medial parts of the condyle maintaining vertical mandibular dimensions |
| B | Fractures affecting the lateral condyle with reduction of mandibular height |
| M | Fractures including high extracapsular fracture dislocations |
A further classification of diacapitular fractures (in that study called “sagittal fractures of the mandibular condyle) was recently suggested by Jing et al12 (Fig. 2) that proposed to divide the posterior plane of the condylar head into three vertical sections equally: a medial section, a central section, and a lateral section. Fractures would be distinguished into type M (medial), type C (central), and type L (lateral) according to the location of the fracture line within the sections (Table 3).
Figure 2.
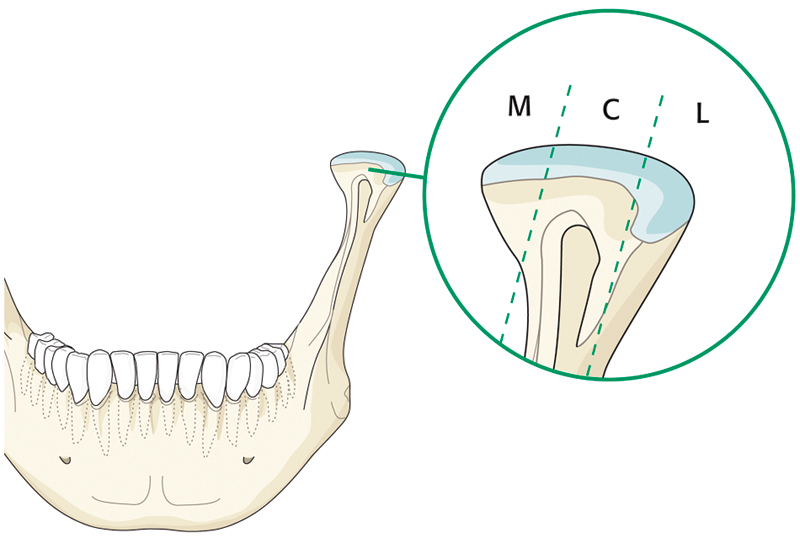
Classification of Jing et al.
Table 3. Jing et al's classification of diacapitular fractures.
| Types | Description |
|---|---|
| M | Fractures involving the medial section of the condylar head |
| C | Fractures involving the central section of the condylar head |
| L | Fractures involving the lateral section of the condylar head |
In the literature, because of these various classifications, it is difficult to obtain a clear picture of the epidemiology of diacapitular fractures types1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 (Table 4). However, the most frequently used classification revealed to be the He et al's system. In all the studies that used such classification, the most frequently observed fractures were type A fractures, followed by type B fractures, and type M fractures, with type C lines resulting as the rarest fractures. Therefore, in most cases, diacapitular fractures are characterized by a fracture line through the lateral third portion of the condylar head with reduction of the ramus height.
Table 4. Review of the literature.
| Authors | Year | Pz | TMJ | Classification | Approach | Fixation | Postoperative management | Complications |
|---|---|---|---|---|---|---|---|---|
| Kermer et al13 | 1998 | 9 | 10 | NA | Preauricular | Lag screw | Soft diet for 6 wk No IMF |
None |
| Hlawitschka et al7 | 2005 | NA | 15 | Neff Type B 15 |
Preauricular | Titanium compression screw: 10 cases Titanium micromesh: 4 cases Absorbable polylactide screw: 1 case |
IMF for 1 d | Temporary FN injury: 1 case |
| Pilling et al14 | 2006 | NA | 5 | Loukota Type-B 5 |
Endaural | Cannulated screw system (Vilex Company, Pittsburgh, PA) | No IMF Early functional exercises |
NA |
| Loukota15 | 2007 | 2 | 2 | NA | Preauricular | Headless bone screw (Martin HBS; KLS Martin, Tuttlingen, Germany) | NA | None |
| Abdel-Galil and Loukota6 | 2008 | 1 | 2 | NA | Preauricular | Custommade ultrasound-activated resorbable pin (KLS Martin SonicWeld Rx) (KLS Martin, Tuttlingen, Germany) | NA | None |
| Vesnaver2 | 2008 | 13 | 16 | NA | Preauricular | Lag screw Whenever possible, 2 lag screws |
No IMF | Mouth opening limitation: 1 case |
| He et al10 | 2009 | 195 | 269 | He &andYang Type A 116 Type B 81 Type C 11 Type M 58 |
Preauricular | Wires, screws, and/or plates | Restricted jaw movement and a soft diet for 1 wk No IMF |
Pain in the TMJ: 1 case FN injury: 1 case |
| He et al8 | 2010 | 151 | 208 | Type A: 110 Type B 60 Type C 9 Type M 25 No displacement 4 |
Preauricular | Wires, screws, and/or plates | No IMF Soft diet for 1 mo |
Facial nerve injury: 1 case Condyle resorption: 4 cases |
| Jing et al12 | 2011 | 24 | 28 | Jing M 2 C 19 L 7 |
Preauricular | 2 microplates (Medicom Instrumente, Tuttingen, Germany) | Elastic IMF for 3–4 wk Liquid diet for 3–4 wk Gape exercises and semiliquid diet for 4 wk after IMF removal |
Temporary FN injury: 5 cases Malocclusion: 2 cases |
| Jones et al3 | 2011 | 5 | 8 | NA | Preauricular 6 Retroauricular 1 |
Lag or position screws, or miniplates | NA | None |
| Müller-Richter et al16 | 2011 | 3 | 4 | NA | Retroauricolar | Custommade ultrasound-activated resorbable pin (KLS Martin SonicWeld Rx) (KLS Martin, Tuttlingen, Germany) | NA | None |
| Benech et al26 | 2011 | 14 | 16 | NA | Retroauricular | Miniplate | Soft diet for 1 month | Temporary FN injury: 2 cases |
| Yang et al17 | 2013 | 11 | 14 | NA | Preauricular | Bicortical screw (AO 2.0 system locked bicortical screw) | NA | 2 temporary FN |
| Chen et al1 | 2010 | 129 | 164 | He and Yang Type A 88 Type B 45 Type C 9 Type M 22 |
Preauricolar | Steel wire and miniplate 87 Miniplate 35 Lag screw and miniplate 12 Lag screw 6 Steel wire 6 Removal of fragment 14 Reconstruction with costochondral graft 4 |
Soft diet for 6 wk No IMF |
Fibrous ankylosis: 1 case Mouth opening limitation: 5 cases Condyle resorption: 3 cases Facial nerve injury: 3 cases Malocclusion:1 case |
Abbreviations: FN, facial nerve; IMF, intermaxillary fixations; Pz, number of patients enrolled in the study; TMJ, number of surgically operated temporomandibular joints.
Imaging and Surgical Planning
In all articles, computed tomography (CT) has been fundamental for an appropriate diagnosis and assessment of condylar head fractures, thus allowing an accurate treatment planning.5 10 12 In fact, CT scans show the precise location of the fracture, size and position of the fragment, and most importantly, the relationship between the ramus stump, fracture segment, and glenoid fossa,2 10 thus being the gold standard method for the diagnosis and classification of diacapitular fractures.10
Furthermore, magnetic resonance imaging (MRI) was used by some authors to complete the evaluation of soft tissue changes in the TMJ after condylar fracture, such as disc displacement, capsular tear, and hemarthrosis.12 Such changes in the soft tissue of the TMJ that accompany condylar head fractures can just be detected by MRI, thus suggesting a role for this imaging method too.18
Finally, the use of computer-assisted preoperative simulation have been proposed to gain more information about the operative site, and simulate the reduction and fixation of the fragment and the stump, thus receiving information about the position and the angle of the hole to be drilled and the length of the screw to be placed.5 9 17 Software such as Mimics (Materialise, Leuven, Belgium) and SimPlantTM (Materialise NV, Leuven, Belgium) have been used to enable computer-assisted preoperative simulation reconstructing the condylar head in three dimensions from Digital Imaging and Communications in Medicine (DICOM) CT data.5 9 17 The condylar segments could be virtually repositioned, adjusted, and made as identical as possible to the image of the residual condyle and the glenoid fossa. After the virtual reduction, the width of the reduced condyle could also be measured to decide preoperatively the length and position of screw for fixation of the fractured condylar head.5 9 17
Indications
The indications for operative treatment of condylar head fractures have been continuously changing in the literature (Table 5). In the past years, absolute indications for surgical treatment included diacapitular fractures in which the stump of the ramus dislocates laterally out of the glenoid fossa.1 8 10 Furthermore, surgery has been increasingly also proposed for significantly displaced or dislocated fractures that make the rehabilitation more difficult and may cause potential TMJ problems.1 8 10 12
Table 5. Indications for open surgical treatment of diacapitular fractures.
| Authors | Year | Indications |
|---|---|---|
| Hlawitschka et al7 | 2005 | Adult patients with displaced, intracapsular mandibular fractures, with a loss of vertical height of the mandibular ramus |
| Vesnaver2 | 2008 | Type B (according to the classification of Neff et al) intra-articular fracture with shortening of the condyle |
| He et al10 | 2009 | Absolute indications: any type of diacapitular fractures in which the stump of the ramus dislocates laterally out of the glenoid fossa, which can cause fibrous or bony ankylosis, especially bilateral intracapsular fractures. |
| He et al8 | 2010 | Relative indications: fracture types A and B (according to the classification of He et al and Yang et al) with fragments significantly displaced or dislocated out of the glenoid fossa, which make rehabilitation more difficult and may cause potential TMJ problems such as mouth-opening restriction, pain, clicking, and crepitations |
| Jing et al12 | 2011 | Displaced or dislocated diacapitular fractures |
| Chen et al1 | 2010 | Absolute indications: any type of diacapitular fractures in which the stump of the ramus dislocates laterally out of the glenoid fossa and which cannot be reduced by closed treatment Relative indications: significantly displaced or dislocated fractures that make the rehabilitation more difficult and may cause potential TMJ problems |
Abbreviation: TMJ, temporomandibular joint.
Instead, most surgeons does not advocate open treatment for any kind of condylar head fractures in children because of their remodeling capacity and good functional adaptative regeneration, though active mobilization of the joint with vigorous mouth-opening exercises has to start early in such cases to avoid development of ankylosis.2 7 19
Several doubts on the advantages of an open treatment have been suggested in cases of undisplaced or comminuted diacapitular fractures too.2 7
Experimental Studies on Animals
Various studies have been performed about condylar head fractures in animals19 20 21 22 23 24 (Table 6). Sheep, pigs, and goats have been used to create diacapitular fractures and to study the development of ankylosis or the outcome of fixation methods.
Table 6. Experimental studies about condylar head fractures in animals.
| Authors | Year | Animals | Fixation | Experiment | Result |
|---|---|---|---|---|---|
| Long and Goss20 | 2007 | 10 sheeps | An animal model was created for the vertical split fracture of the TMJ condylar head similar to a type B intracapsular condylar fracture in humans, and the mandibular function and morphological changes of the TMJ structure were evaluated | Our findings demonstrate that pathological changes of osteonecrosis, osteoarthrosis, and even ankylosis in the TMJ are likely to occur following vertical intracapsular fractures through the lateral condylar pole. This model can be used to evaluate various methods of surgical treatment | |
| Meng et al21 | 2010 | 8 sheeps | Two lateral screws (one lag screw and one position screw) | The aim of the present study was to compare and evaluate the veterinary and radiological outcomes of diacapitular condylar fracture after ORIF and closed treatment in the TMJ of sheep | The animals in the closed group had severely deformed condyles 12 wk after osteotomy. In contrast, animals in the ORIF group showed satisfactory reposition of the fractured fragments immediately after ORIF and well-shaped right condyles at 12 wk, with significantly fewer osteoarthrotic changes and signs of TMJ ankylosis |
| Schneider et al22 | 2011 | 20 pig mandibles | Ultrasound-aided resorbable pins with poly-(d,l)-lactide (SonicWeld Rx, KLS Martin, Tuttlingen, Germany) and titanium screws | The use of resorbable ultrasound-aided pins was compared with titanium screws to assess the biomechanical stability of osteosyntheses of artificially created diacapitular fractures of the condylar head in pigs. Stability of the osteosynthesis was assessed by a shear test using a universal strength-testing machine | An adequate level of clinical stability seems to support the use of pins in lowload-bearing osteosyntheses. The limiting factor is not the bonding between the pin and the host bone, but the strength of the pin itself. For this reason, increasing the number of pins will proportionally increase stability, though the difficulty in placing more than two pins in the narrow lateral pole of the condyle should be considered |
| Feng et al19 | 2012 | 12 Goats | A two-hole, 2-mm plate was attached with one screw to each fragment | Condylar cartilage from one randomly selected side of the condyle was removed while that on the other side was retained | A significant reduction of the ramus height was observed in the group from which the cartilage had been removed, in comparison with the control group in which it had been retained |
| Liu et al23 | 2012 | 20 sheeps | The lateral pterygoid muscle was cut (∼0.5–1.0 cm from each sheep in that group) in a group and a control group in which the muscle had not been cut was used | At 24 wk on CT scan, bone had overgrown the joints in which the muscle had not been cut, and the shape of the joints was less regular than previously. In contrast, the joints in which the muscle had been cut looked almost normal | |
| Schneider et al24 | 2013 | 20 sheeps | 2–3 resorbable SonicWeld pins in 10 animals. 2–3 conventional mini titanium screws in other 10 animals |
The use of resorbable ultrasound-aided pins was compared with titanium screws | The authors found no disadvantages of osteosynthesis with pins compared with titanium screws. Advantages of the resorbable material (ability to degrade and no material to remove) seemed to predominate, thus supporting the use of sonic welding for fractures of the condylar head in humans |
Abbreviation: TMJ, temporomandibular joint.
The findings by Long and Goss20 demonstrate that pathological changes of osteonecrosis, osteoarthrosis, and even ankylosis in the TMJ are likely to occur following vertical intracapsular fractures through the lateral condylar pole. Instead, Liu et al23 observed the involvement of lateral pterygoid muscle in the healing process of the condylar head: at 24 weeks after diacapitular osteotomy, on CT scan, bone had overgrown the joints in which the muscle had not been cut, and the shape of the joints was less regular than previously. In contrast, the joints in which the muscle had been cut looked almost normal. Finally, in the study by Feng et al,19 a significant reduction of the ramus height was observed in the group from which the cartilage had been removed, in comparison with the control group in which it had been retained, thus stressing the importance of maintaining the condylar cartilage after diacapitular fractures.
Meng et al21 performed a study to compare and evaluate the veterinary and radiological outcomes of diacapitular condylar fracture after open reduction and internal fixation (ORIF) and closed treatment in the TMJ of sheep. The animals in the closed group had severely deformed condyles 12 weeks after osteotomy. In contrast, animals in the ORIF group showed satisfactory reposition of the fractured fragments immediately after ORIF and well-shaped right condyles at 12 weeks, with significantly fewer osteoarthrotic changes and signs of TMJ ankylosis.
As for fixation methods, both studies by Schneider et al22 24 found no disadvantages of osteosynthesis with resorbable pins compared with titanium screws. In fact, an adequate level of clinical stability seems to support the use of pins in lowload-bearing osteosyntheses. The limiting factor would not be the bonding between the pin and the host bone, but the strength of the pin itself. For this reason, increasing the number of pins would proportionally increase stability, though the difficulty in placing more than two pins in the narrow lateral pole of the condyle should be considered.
Surgical Approaches
Various approaches for diacapitular condylar fractures have been reported in the literature, though the most commonly used were the preauricular (Fig. 3) (with several variations) and retroauricular (Fig. 4) approaches (Table 4).10 26 27
Figure 3.
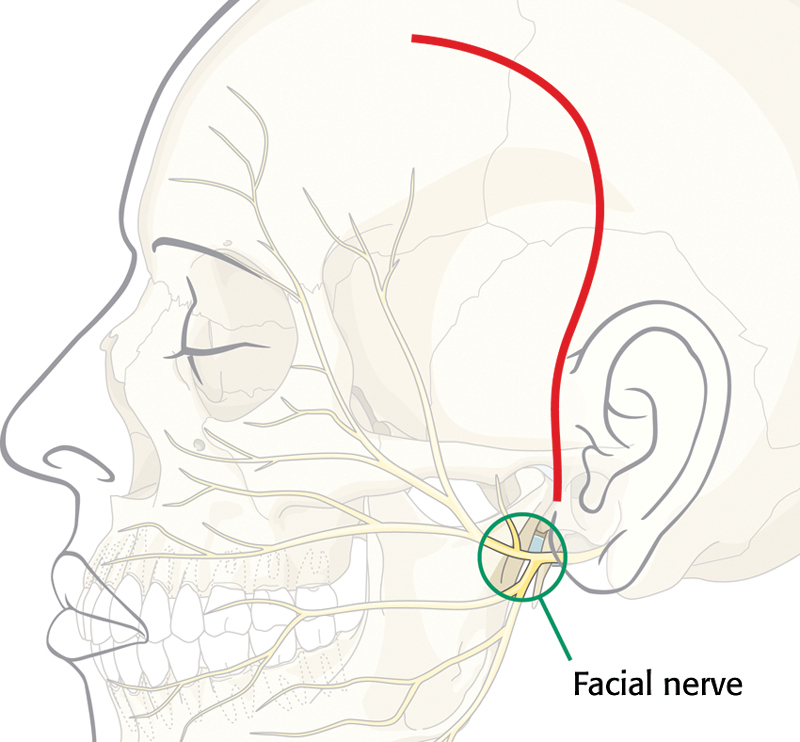
Preauricular approach.
Figure 4.
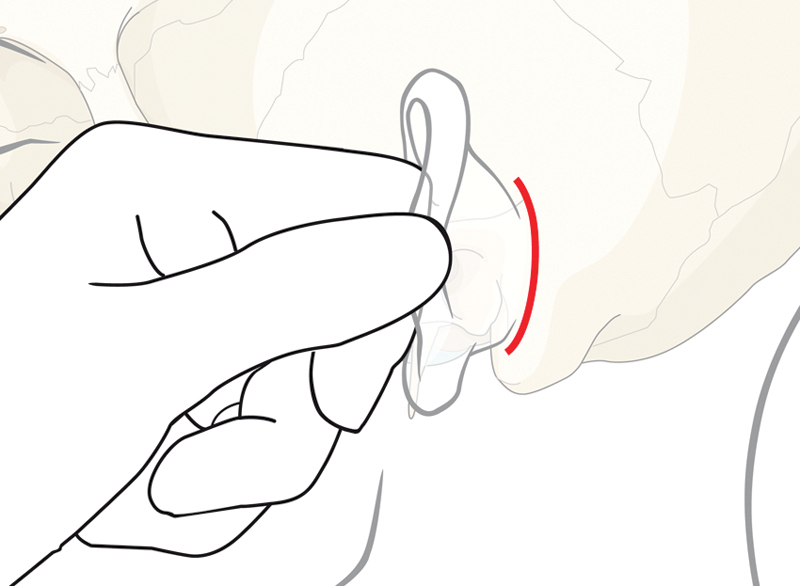
Retroauricular approach.
The incision of preauricular approach can be placed in different regions related to the tragus. With such approach, the exposure of this area may be limited because of the presence of the facial and auriculotemporal nerves in the way. Furthermore, the superficial temporal vessels are often encountered. Therefore, postoperative concerns following preauricular approach are related to facial nerve injury, the possibility of a visible scar, and the risk for Frey syndrome.10 26 27
On the contrary, with the retroauricular approach the frontal branch of the facial nerve and the auriculotemporal nerve have to be located and protected within the substance of the anteriorly retracted flap. A wider exposure of the condylar head may be obtained, thanks to this approach, that is reported to be associated with a low risk for facial nerve injuries, auditory stenosis, aesthetic deformity, vascular injuries, salivary fistulas, and Frey syndrome.26 27
Surgical Techniques
Fractures of the condylar head are usually treated conservatively because of the difficulty in the exposure and fixation and the risk of facial nerve damage. Differently from conservative treatment, open surgery can give early recovery of occlusion and movement of the jaw,5 6 thus lowering the risk for condylar deformation, height reduction of the mandibular ramus, dysfunctional complaints, and TMJ ankylosis.7 8
The most frequently used surgical approach for diacapitular fractures has been the preauricular approach, though retroauricular and endaural approaches have been proposed too (Table 4). The common dissection is behind the superficial temporal vessels to the TMJ area. Because the middle temporal vein, which is a very important branch of the superficial temporal vein, crosses the zygomatic arch, most of the time, it has to be ligated for better exposure.8 The complications associated with these surgical approaches include facial nerve injury, impaired circulation in the ear, bleeding, and scarring.2 16
Several techniques have been proposed to reduce and fix fractures of the condylar head, such as standard bone screws, resorbable screws, resorbable pins, and cannulated lag screws.6
First of all, reduction and stabilization of these fractures before fixation remains a challenge because of the limitation of spaces. The manipulation of the condylar head with two small retractors and additional manipulation with periosteal elevators have been reported.13 The use of a periodontal probe to locate the medial fragment with reduction and stabilization of the fracture using hooks and periodontal elevators has been proposed too.2 Loukota15 and Pilling et al14 described the benefits of stabilizing the fracture with the use of K-wires (Modern Grinding, Port Washington, WI), while Jones et al3 highlighted the retrieval of the proximal fragment with a screw. Finally, Schneider et al proposed the use of a repositioning pin to assist in reduction and fixation of the proximal condylar fragment with only minimal dissection, before the placement of the permanent osteosynthesis screws.25
As for fixation options, lag screw or long screw fixation of the fractured fragment has been one the most frequently used techniques, generally allowing a stable fixation (Table 4). The use of two lag screws has been proposed to obtain a higher stability, though it is not always possible due to the small size of the fractured fragment.2
Some variations of the lag screw technique have been suggested too, thus using headless bone screw or cannulated screw systems.14 15 Some authors used various fixation methods such as wire, screw, and/or plates according to the type of diacapitular fractures.1 8 10
Titanium osteosynthesis with lag screws or long screw osteosynthesis generally showed to be successful in the repositioning of fractured fragments, though titanium plates and screws might cause atrophy of the bone by stress shielding. To overcome these shortcomings, resorbable material has been proposed by some authors that showed that resorbable pins can provide reliable stability for the fixation of mandibular condylar fractures.6 9 16 Other advantages associated with resorbable osteosynthesis materials would be the eliminations of the risk for secondary operations or for dislocation of titanium screws and plates in the joint or at the skull base.16
All authors agree with the lack of need for postoperative intermaxillary fixation after surgical treatment of diacapitular fractures (Table 4). A soft diet for some weeks has been suggested by various authors. Instead, early postoperative functional exercise seems to be controversial.
As for soft tissue management, several articles state that the lateral pterygoid muscle should never be stripped from the medially displaced fragment, although this would ease reduction.1 2
In fact, disinsertion of this muscle would compromise the vascular supply to the medial bony fragment, which could lead to its ischemic necrosis and resorption.1 2 Finally, it is also necessary to repair the joint's soft tissues, in particular, the intra-articular disc and the joint capsule.2 The disc, that is typically displaced anteriorly and medially following diacapitular fractures, should be replaced in its anatomic position.1 If the posterior attachment is torn, the disc should be sutured with the posterior attachment.1 In addition to anatomic bony reduction, an appropriate management of soft tissues is crucial for a properly functioning TMJ.2
Complications
Complications of open treatment are few, though some cases of facial nerve injury have been reported (Table 4) because of the still challenging nature of the surgical treatment of diacapitular fractures.10 Instead, postoperative malocclusion and mouth opening limitation are rare.
Condylar head resorption has been reported in seven cases, but it is important to remember that an aseptic condylar necrosis can still be the result of the trauma, with an almost complete resorption of the condylar process being observed even following closed functional treatment. Instead serious condylar deformation is rare after open treatment.7
Conclusions
The keys for successful open treatment seem to be a proper preauricular or retroauricular approach with careful dissection to prevent facial nerve injury, a careful repositioning of the condylar head without stripping it from the lateral pterygoid muscle and destroying the condylar cartilage surface is needed, and a stable fixation. There is no consensus about a gold standard fixation technique for open treatment of diacapitular fractures, as this surgery could be still considered experimental in numerous centers.
ORIF of selected diacapitular fractures seem to be successful in a high percentage of cases, improving postoperative function and bony healing.
References
- 1.Chen M, Yang C, He D, Zhang S, Jiang B. Soft tissue reduction during open treatment of intracapsular condylar fracture of the temporomandibular joint: our institution's experience. J Oral Maxillofac Surg. 2010;68(9):2189–2195. doi: 10.1016/j.joms.2009.09.063. [DOI] [PubMed] [Google Scholar]
- 2.Vesnaver A. Open reduction and internal fixation of intra-articular fractures of the mandibular condyle: our first experiences. J Oral Maxillofac Surg. 2008;66(10):2123–2129. doi: 10.1016/j.joms.2008.06.010. [DOI] [PubMed] [Google Scholar]
- 3.Jones S D, Sugar A W, Mommaerts M Y. Retrieval of the displaced condylar fragment with a screw: simple method of reduction and stabilisation of high and intracapsular condylar fractures. Br J Oral Maxillofac Surg. 2011;49(1):58–61. doi: 10.1016/j.bjoms.2010.02.006. [DOI] [PubMed] [Google Scholar]
- 4.Loukota R A, Neff A, Rasse M. Nomenclature/classification of fractures of the mandibular condylar head. Br J Oral Maxillofac Surg. 2010;48(6):477–478. doi: 10.1016/j.bjoms.2009.08.036. [DOI] [PubMed] [Google Scholar]
- 5.Iwai T, Yajima Y, Matsui Y, Tohnai I. Computer-assisted preoperative simulation for screw fixation of fractures of the condylar head. Br J Oral Maxillofac Surg. 2013;51(2):176–177. doi: 10.1016/j.bjoms.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 6.Abdel-Galil K, Loukota R. Fixation of comminuted diacapitular fractures of the mandibular condyle with ultrasound-activated resorbable pins. Br J Oral Maxillofac Surg. 2008;46(6):482–484. doi: 10.1016/j.bjoms.2007.11.025. [DOI] [PubMed] [Google Scholar]
- 7.Hlawitschka M, Loukota R, Eckelt U. Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. Int J Oral Maxillofac Surg. 2005;34(6):597–604. doi: 10.1016/j.ijom.2005.02.004. [DOI] [PubMed] [Google Scholar]
- 8.He D, Yang C, Chen M, Bin J, Zhang X, Qiu Y. Modified preauricular approach and rigid internal fixation for intracapsular condyle fracture of the mandible. J Oral Maxillofac Surg. 2010;68(7):1578–1584. doi: 10.1016/j.joms.2009.07.076. [DOI] [PubMed] [Google Scholar]
- 9.Wang W H, Deng J Y, Zhu J, Li M, Xia B, Xu B. Computer-assisted virtual technology in intracapsular condylar fracture with two resorbable long-screws. Br J Oral Maxillofac Surg. 2013;51(2):138–143. doi: 10.1016/j.bjoms.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 10.He D, Yang C, Chen M, Jiang B, Wang B. Intracapsular condylar fracture of the mandible: our classification and open treatment experience. J Oral Maxillofac Surg. 2009;67(8):1672–1679. doi: 10.1016/j.joms.2009.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Neff A, Kolk A, Deppe H, Horch H H. New aspects for indications of surgical management of intra-articular and high temporomandibular dislocation fractures [in German. ] Mund Kiefer Gesichtschir. 1999;3(1):24–29. doi: 10.1007/s100060050088. [DOI] [PubMed] [Google Scholar]
- 12.Jing J, Han Y, Song Y, Wan Y. Surgical treatment on displaced and dislocated sagittal fractures of the mandibular condyle. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(6):693–699. doi: 10.1016/j.tripleo.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 13.Kermer Ch, Undt G, Rasse M. Surgical reduction and fixation of intracapsular condylar fractures. A follow up study. Int J Oral Maxillofac Surg. 1998;27(3):191–194. doi: 10.1016/s0901-5027(98)80008-8. [DOI] [PubMed] [Google Scholar]
- 14.Pilling E, Schneider M, Mai R, Loukota R A, Eckelt U. Minimally invasive fracture treatment with cannulated lag screws in intracapsular fractures of the condyle. J Oral Maxillofac Surg. 2006;64(5):868–872. doi: 10.1016/j.joms.2005.11.049. [DOI] [PubMed] [Google Scholar]
- 15.Loukota R A. Fixation of dicapitular fractures of the mandibular condyle with a headless bone screw. Br J Oral Maxillofac Surg. 2007;45(5):399–401. doi: 10.1016/j.bjoms.2005.12.002. [DOI] [PubMed] [Google Scholar]
- 16.Müller-Richter U D, Reuther T, Böhm H, Kochel M, Kübler A C. Treatment of intracapsular condylar fractures with resorbable pins. J Oral Maxillofac Surg. 2011;69(12):3019–3025. doi: 10.1016/j.joms.2011.02.013. [DOI] [PubMed] [Google Scholar]
- 17.Yang M L, Zhang B, Zhou Q, Gao X B, Liu Q, Lu L. Minimally-invasive open reduction of intracapsular condylar fractures with preoperative simulation using computer-aided design. Br J Oral Maxillofac Surg. 2013;51(3):e29–e33. doi: 10.1016/j.bjoms.2012.03.005. [DOI] [PubMed] [Google Scholar]
- 18.Yu Y H, Wang M H, Zhang S Y. et al. Magnetic resonance imaging assessment of temporomandibular joint soft tissue injuries of intracapsular condylar fracture. Br J Oral Maxillofac Surg. 2013;51(2):133–137. doi: 10.1016/j.bjoms.2012.03.019. [DOI] [PubMed] [Google Scholar]
- 19.Feng Z, Li L, He D, Yang C, Qiu Y. Role of retention of the condylar cartilage in open treatment of intracapsular condylar fractures in growing goats: three-dimensional computed tomographic analysis. Br J Oral Maxillofac Surg. 2012;50(6):523–527. doi: 10.1016/j.bjoms.2011.09.004. [DOI] [PubMed] [Google Scholar]
- 20.Long X, Goss A N. A sheep model of intracapsular condylar fracture. J Oral Maxillofac Surg. 2007;65(6):1102–1108. doi: 10.1016/j.joms.2006.06.307. [DOI] [PubMed] [Google Scholar]
- 21.Meng F, Hu K, Kong L, Zhao Y, Liu Y, Zhou S. Veterinary and radiological evaluations of open and closed treatment of type B diacapitular (intracapsular) fractures of the mandibular condyle in sheep. Br J Oral Maxillofac Surg. 2010;48(6):448–452. doi: 10.1016/j.bjoms.2009.08.002. [DOI] [PubMed] [Google Scholar]
- 22.Schneider M, Eckelt U, Reitemeier B. et al. Stability of fixation of diacapitular fractures of the mandibular condylar process by ultrasound-aided resorbable pins (SonicWeld Rx® System) in pigs. Br J Oral Maxillofac Surg. 2011;49(4):297–301. doi: 10.1016/j.bjoms.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 23.Liu C K, Liu P, Meng F W. et al. The role of the lateral pterygoid muscle in the sagittal fracture of mandibular condyle (SFMC) healing process. Br J Oral Maxillofac Surg. 2012;50(4):356–360. doi: 10.1016/j.bjoms.2011.05.015. [DOI] [PubMed] [Google Scholar]
- 24.Schneider M, Loukota R, Kuchta A. et al. Treatment of fractures of the condylar head with resorbable pins or titanium screws: an experimental study. Br J Oral Maxillofac Surg. 2013;51(5):421–427. doi: 10.1016/j.bjoms.2012.07.015. [DOI] [PubMed] [Google Scholar]
- 25.Schneider M, Loukota R, Eckelt U. Reduction of diacapitular fractures of the mandibular condyle using a special repositioning pin. Br J Oral Maxillofac Surg. 2009;47(7):558–559. doi: 10.1016/j.bjoms.2008.10.017. [DOI] [PubMed] [Google Scholar]
- 26.Benech A, Arcuri F, Baragiotta N, Nicolotti M, Brucoli M. Retroauricular transmeatal approach to manage mandibular condylar head fractures. J Craniofac Surg. 2011;22(2):641–647. doi: 10.1097/SCS.0b013e318207f495. [DOI] [PubMed] [Google Scholar]
- 27.Arcuri F, Brucoli M, Benech A. Analysis of the retroauricular transmeatal approach: a novel transfacial access to the mandibular skeleton. Br J Oral Maxillofac Surg. 2012;50(2):e22–e26. doi: 10.1016/j.bjoms.2011.08.006. [DOI] [PubMed] [Google Scholar]


